Use of a mHealth System to Improve Antenatal Care in Low and Lower-Middle Income Countries: Report on Patients and Healthcare Workers’ Acceptability in Tanzania
Abstract
:1. Introduction
2. Materials and Methods
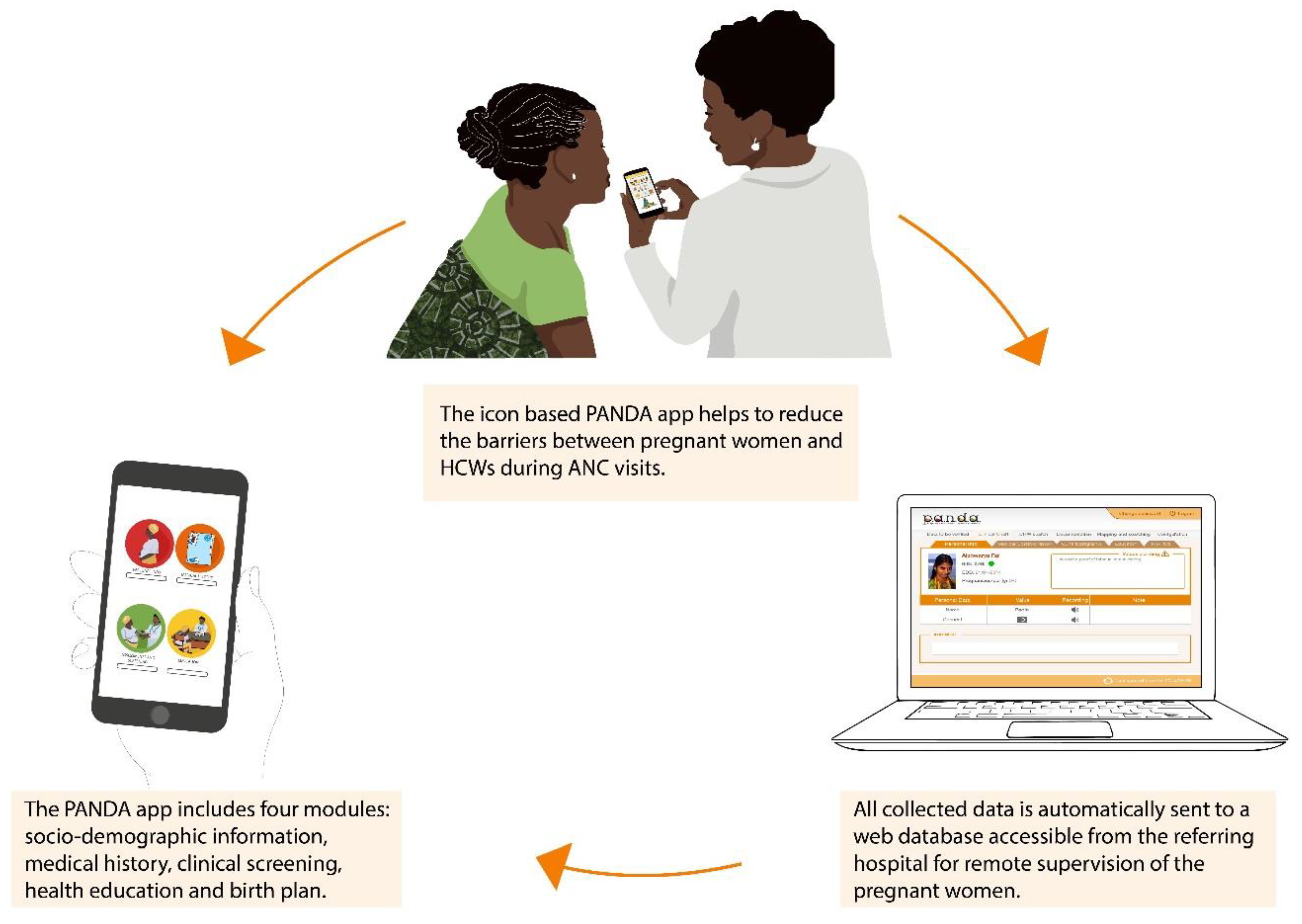
2.1. The PANDA System
2.2. Study Setting and Study Design
2.3. Study Population and Data Collection
2.4. Data Analysis
3. Results
3.1. Women’ Acceptability
3.2. Acceptability of HCWs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO; UNICEF; UNFPA; World Bank Group; United Nations Population Division. Trends in Maternal Mortality: 2000 to 2017; WHO: Geneva, Switzerland, 2019; Available online: https://apps.who.int/iris/handle/10665/327596 (accessed on 16 November 2022).
- UNICEF; WHO; World Bank Group; United Nations Population Division. Levels and Trends in Child Mortality. Report 2020; UNICEF: New York, NY, USA, 2020; Available online: https://www.unicef.org/reports/levels-and-trends-child-mortality-report-2020 (accessed on 16 November 2022).
- USAID. Maternal and Child Health, Tanzania; USAID: Washington, DC, USA, 2018.
- WHO; UNICEF; World Bank Group; United Nations Population Division. A Neglected Tragedy: The Global Burden of Stillbirths. Report of the UN Inter-agency Group for Child Mortality Estimation (IGME); UNICEF: New York, NY, USA, 2020; Available online: https://data.unicef.org/resources/a-neglected-tragedy-stillbirth-estimates-report/ (accessed on 16 November 2022).
- Sankar, M.J.; Natarajan, C.K.; Das, R.R.; Agarwal, R.; Chandrasekaran, A.; Paul, V.K. When do newborns die? A systematic review of timing of overall and cause-specific neonatal deaths in developing countries. J. Perinatol. 2016, 36 (Suppl. S1), S1–S11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience; WHO: Geneva, Switzerland, 2016; Available online: https://apps.who.int/iris/bitstream/handle/10665/259947/WHO-RHR-18.02-eng.pdf (accessed on 16 November 2022).
- WHO. WHO Recommendations on Postnatal Care of the Mother and Newborn 2013; WHO: Geneva, Switzerland, 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK190090/ (accessed on 16 November 2022).
- WHO; United Nations Population Fund; UNICEF. Pregnancy, Childbirth, Postpartum and Newborn Care—A Guide for Essential Practice, 3rd ed.; WHO: Geneva, Switzerland, 2015; Available online: https://apps.who.int/iris/handle/10665/249580 (accessed on 16 November 2022).
- WHO; USAID. Postnatal Care for Mothers and Newborns, Highlights from the World Health Organization 2013 Guidelines; WHO: Geneva, Switzerland, 2015; Available online: https://www.who.int/docs/default-source/mca-documents/nbh/brief-postnatal-care-for-mothers-and-newborns-highlights-from-the-who-2013-guidelines.pdf (accessed on 16 November 2022).
- Benski, A.C.; Stancanelli, G.; Scaringella, S.; Herinainasolo, J.L.; Jinoro, J.; Vassilakos, P.; Petignat, P.; Schmidt, N.C. Usability and feasibility of a mobile health system to provide comprehensive antenatal care in low-income countries: PANDA mHealth pilot study in Madagascar. J. Telemed. Telecare 2017, 23, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Bintabara, D. Addressing the huge poor–rich gap of inequalities in accessing safe childbirth care: A first step to achieving universal maternal health coverage in Tanzania. PLoS ONE 2021, 16, e0246995. [Google Scholar] [CrossRef] [PubMed]
- Mgata, S.; Maluka, S.O. Factors for late initiation of antenatal care in Dar es Salaam, Tanzania: A qualitative study. BMC Pregnancy Childbirth 2019, 19, 415. [Google Scholar] [CrossRef] [PubMed]
- Hulsbergen, M.; van der Kwaak, A. The influence of quality and respectful care on the uptake of skilled birth attendance in Tanzania. BMC Pregnancy Childbirth 2020, 20, 681. [Google Scholar] [CrossRef] [PubMed]
- Obasola, O.I.; Mabawonku, I.; Lagunju, I. A Review of e-Health Interventions for Maternal and Child Health in Sub-Sahara Africa. Matern. Child Health J. 2015, 19, 1813–1824. [Google Scholar] [CrossRef] [PubMed]
- Watterson, J.L.; Walsh, J.; Madeka, I. Using mHealth to Improve Usage of Antenatal Care, Postnatal Care, and Immunization: A Systematic Review of the Literature. Biomed. Res. Int. 2015, 2015, 153402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borsari, L.; Stancanelli, G.; Guarenti, L.; Grandi, T.; Leotta, S.; Barcellini, L.; Borella, P.; Benski, A.C. An Innovative Mobile Health System to Improve and Standardize Antenatal Care among Underserved Communities: A Feasibility Study in an Italian Hosting Center for Asylum Seekers. J. Immigr. Minor. Health 2018, 20, 1128–1136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langer, A.; Villar, J.; Romero, M.; Nigenda, G.; Piaggio, G.; Kuchaisit, C.; Rojas, G.; Al-Osimi, M.; Miguel Belizán, J.; Farnot, U.; et al. Are women and providers satisfied with antenatal care? Views on a standard and a simplified, evidence-based model of care in four developing countries. BMC Womens Health 2002, 2, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jareethum, R.; Titapant, V.; Chantra, T.; Sommai, V.; Chuenwattana, P.; Jirawan, C. Satisfaction of healthy pregnant women receiving short message service via mobile phone for prenatal support: A randomized controlled trial. J. Med. Assoc. Thai 2008, 91, 458–463. [Google Scholar] [PubMed]
- Lund, S.; Nielsen, B.B.; Hemed, M.; Boas, I.M.; Said, A.; Said, K.; Makungu, M.H.; Rasch, V. Mobile phones improve antenatal care attendance in Zanzibar: A cluster randomized controlled trial. BMC Pregnancy Childbirth 2014, 14, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nair, M.; Yoshida, S.; Lambrechts, T.; Boschi-Pinto, C.; Bose, K.; Mason, E.M.; Mathai, M. Facilitators and barriers to quality of care in maternal, newborn and child health: A global situational analysis through metareview. BMJ Open 2014, 4, e004749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rowe, R.E.; Garcia, J.; Macfarlane, A.J.; Davidson, L.L. Improving communication between health professionals and women in maternity care: A structured review. Health Expect. 2002, 5, 63–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Compaoré, R.; Ouédraogo, A.; Baguiya, A.; Dahourou, D.; Somé, A.; Kadari, C.; Tougri, H.; Kouanda, S. Utilisation de la technologie mobile pour l’amelioration des soins prenatals: Faisabilite du systeme PANDA dans le district sanitaire de koupela au Burkina Faso. Burkina Med. 2020, 24, 9–22. [Google Scholar]
- FIGO Committee for the Ethical Aspects of Human Reproduction and Women’s Health. Task-shifting in obstetric care. Int. J. Gynaecol. Obstet. 2013, 120, 206–207. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Recommendations: Optimizing Health Worker Roles to Improve Access to Key Maternal and Newborn Health Interventions Through Task Shifting; WHO: Geneva, Switzerland, 2012; Available online: https://www.who.int/publications/i/item/9789241504843 (accessed on 16 November 2022).

| Items | Questions | Pregnant Women | p-Value | |
|---|---|---|---|---|
| Implementation Site | Control Site | |||
| n (%) * | n (%) * | |||
| Duration of the visit | a lot more time | 2 (3.8) | 0 (0.0) | <0.001 |
| a little more time | 0 (0.0) | 36 (78.3) | ||
| right time | 50 (96.2) | 10 (21.7) | ||
| Health education during the ANC | No | 0 (0.0) | 0 (0.0) | 0.125 |
| sometimes | 0 (0.0) | 2 (4.4) | ||
| yes | 52 (100.0) | 43 (95.6) | ||
| Availability medicines prescribed by HCWs | no | 0 (0.0) | 0 (0.0) | 0.125 |
| sometimes | 0 (0.0) | 2 (4.4) | ||
| yes | 52 (100.0) | 43 (95.6) | ||
| Availability screening tests | no | 0 (0.0) | 0 (0.0) | 0.059 |
| sometimes | 0 (0.0) | 3 (6.7) | ||
| yes | 52 (100.0) | 42 (93.3) | ||
| Information regarding the woman’s health | no information | 0 (0.0) | 0 (0.0) | <0.001 |
| not enough | 0 (0.0) | 0 (0.0) | ||
| as much as they expected | 2 (3.8) | 45 (97.8) | ||
| more than expected | 50 (96.2) | 1 (2.2) | ||
| Information regarding Screening during ANC | no information | 0 (0.0) | 0 (0.0) | <0.001 |
| not enough | 0 (0.0) | 0 (0.0) | ||
| as much as they wanted | 1 (1.9) | 45 (97.8) | ||
| more than expected | 51 (98.1) | 1 (2.2) | ||
| Information regarding danger signs during pregnancy | no information | 0 (0.0) | 0 (0.0) | <0.001 |
| not enough | 0 (0.0) | 0 (0.0) | ||
| as much as they expected | 2 (3.8) | 45 (97.8) | ||
| more than expected | 50 (96.2) | 1 (2.2) | ||
| Information regarding labor | no information | 0 (0.0) | 0 (0.0) | <0.001 |
| not enough | 0 (0.0) | 0 (0.0) | ||
| as much as they expected | 0 (0.0) | 45 (97.8) | ||
| more than expected | 52 (100.0) | 1 (2.2) | ||
| Information regarding labor breastfeeding | no information | 0 (0.0) | 0 (0.0) | <0.001 |
| not enough | 0 (0.0) | 0 (0.0) | ||
| as much as they expected | 0 (0.0) | 46 (100.0) | ||
| more than expected | 52 (100.0) | 0 (0.0) | ||
| Overall satisfaction of the ANC visit | absolutely not satisfied | 0 (0.0) | 0 (0.0) | <0.001 |
| not so satisfied | 0 (0.0) | 0 (0.0) | ||
| quite satisfied | 0 (0.0) | 9 (19.6) | ||
| very satisfied | 52 (100.0) | 37 (80.4) | ||
| If they become pregnant again, will they come back for an ANC visit? | absolutely not | 0 (0.0) | 0 (0.0) | <0.001 |
| probably not | 0 (0.0) | 0 (0.0) | ||
| probably yes | 0 (0.0) | 11 (23.9) | ||
| absolutely yes | 52 (100.0) | 35 (76.1) | ||
| Recommendation to a relative or a friend for ANC | absolutely not | 1 (1.9) | 0 (0.0) | <0.001 |
| probably not | 0 (0.0) | 0 (0.0) | ||
| probably yes | 0 (0.0) | 11 (23.9) | ||
| absolutely yes | 51 (98.1) | 35 (76.1) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paduano, S.; Incerti, F.; Borsari, L.; Benski, A.C.; Ernest, A.; Mwampagatwa, I.; Lilungulu, A.; Masoi, T.; Bargellini, A.; Stornelli, F.; et al. Use of a mHealth System to Improve Antenatal Care in Low and Lower-Middle Income Countries: Report on Patients and Healthcare Workers’ Acceptability in Tanzania. Int. J. Environ. Res. Public Health 2022, 19, 15342. https://doi.org/10.3390/ijerph192215342
Paduano S, Incerti F, Borsari L, Benski AC, Ernest A, Mwampagatwa I, Lilungulu A, Masoi T, Bargellini A, Stornelli F, et al. Use of a mHealth System to Improve Antenatal Care in Low and Lower-Middle Income Countries: Report on Patients and Healthcare Workers’ Acceptability in Tanzania. International Journal of Environmental Research and Public Health. 2022; 19(22):15342. https://doi.org/10.3390/ijerph192215342
Chicago/Turabian StylePaduano, Stefania, Federica Incerti, Lucia Borsari, Anne Caroline Benski, Alex Ernest, Ipyana Mwampagatwa, Athanase Lilungulu, Theresia Masoi, Annalisa Bargellini, Federica Stornelli, and et al. 2022. "Use of a mHealth System to Improve Antenatal Care in Low and Lower-Middle Income Countries: Report on Patients and Healthcare Workers’ Acceptability in Tanzania" International Journal of Environmental Research and Public Health 19, no. 22: 15342. https://doi.org/10.3390/ijerph192215342






