Expanding the Focus of Occupational Safety and Health: Lessons from a Series of Linked Scientific Meetings
Abstract
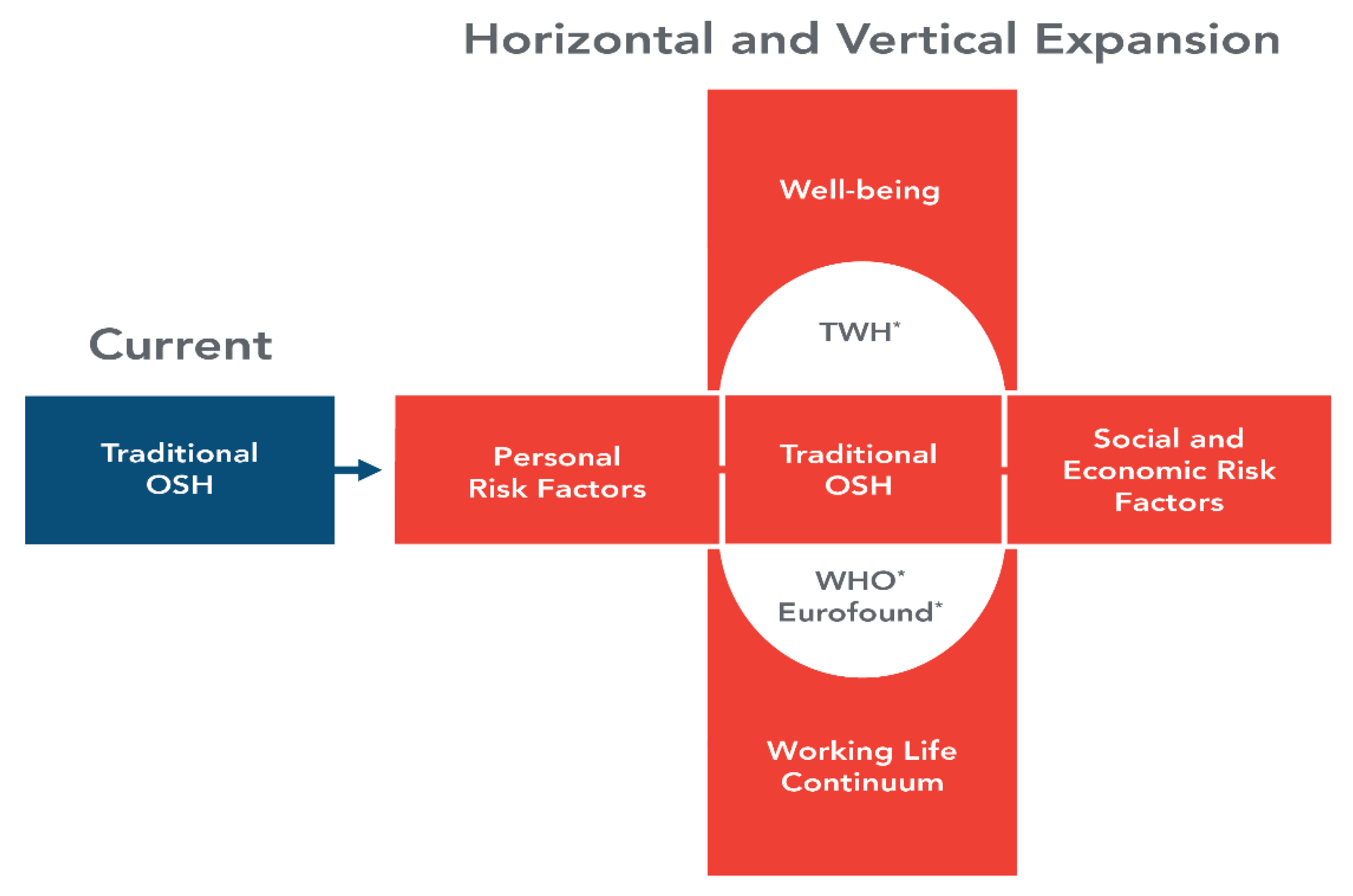
:1. Introduction
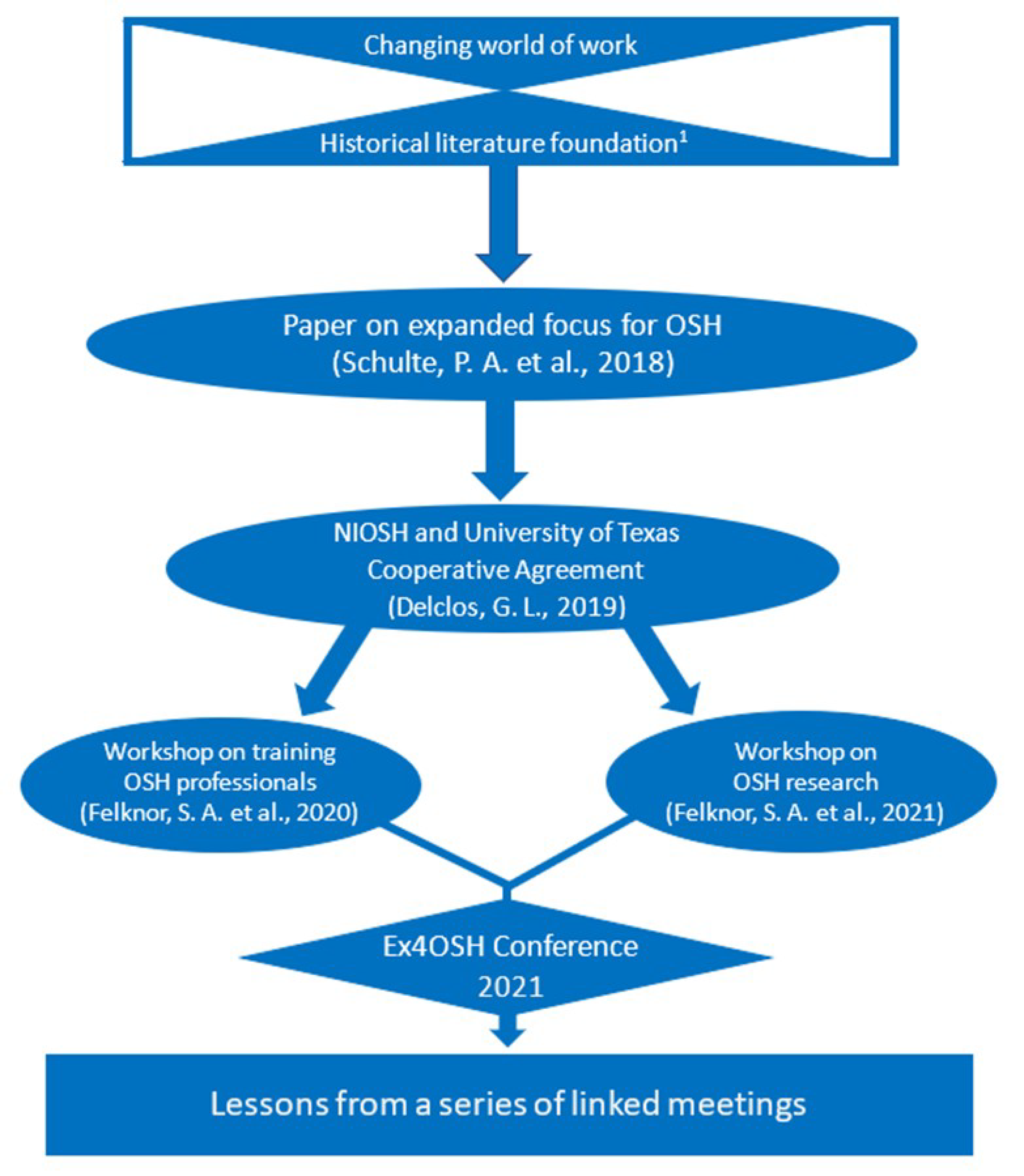
2. Materials and Methods
3. Significant Emergent Themes from the Workshops and Ex4OSH Conference
3.1. Worker Health Inequalities
3.2. Training New OSH Professionals
3.3. Future OSH Research and Practice
3.4. Tools to Measure Well-Being of Workers
3.4.1. Thriving from Work Questionnaire
3.4.2. NIOSH Worker Well-Being Questionnaire
3.5. Psychosocial Hazards and Adverse Mental Health Effects
3.6. Skilling, Upskilling and Improving Job Quality
3.7. Soceioeconomic Influences
3.8. Climate Change
3.9. COVID-19 Pandemic Influences on OSH
3.10. Strategic Foresight
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Daheim, C.; Winterman, O. 2050: The Future of Work. Findings of an International Study of the Millennium Project; Bertelmann Stiffung: Gutersloh, Germany, 2016. [Google Scholar]
- Peckham, T.K.; Bker, M.G.; Camp, J.E.; Kaufman, J.D.; Seixas, N.S. Creating the future for occupational health. Ann. Work. Expo. Health 2017, 61, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Schulte, P.A.; Streit, J.M.K.; Sheriff, F.; Delclos, G.; Felknor, S.A.; Tamers, S.L.; Fendinger, D.; Grosch, J.; Sala, R. Potential scenarios and hazards in the work of the future: A systemic review of the peer-reviewed literature and gray literature. Ann. Work. Expo. Health 2020, 64, 786–816. [Google Scholar] [CrossRef] [PubMed]
- The World Bank. The World Development Report (WDR) 2019. The Changing Nature of Work. Available online: https://www.worldbank.org/en/publication/wdr2019 (accessed on 12 May 2020).
- Balliester, T.; Elsheikhia, A. The Future of Work: A Literature Review; Working Paper No. 29; International Labour Organization: Geneva, Switzerland, 2018; pp. 1–54. Available online: https://www.ilo.org/global/research/publications/working-papers/WCMS_625866/lang--en/index.htm (accessed on 10 October 2019).
- Manyika, J.; Lund, S.; Jacques, C.; Bughin, J.; Woetzel, J.; Batra, P.; Ko, R.; Sanghvi, S. What the Future of Work Will Mean for Jobs, Skills and Wages: Jobs Lost, Jobs Gained; McKinsey Global Institute: Washington, DC, USA, 2017; Available online: https://www.mckinsey.com/featured-insights/future-of-work/jobs-lost-jobs-gained-what-the-future-of-work-will-mean-for-jobs-skills-and-wages (accessed on 11 April 2022).
- Howard, J. Nonstandard work arrangements and worker health and safety. Am. J. Ind. Med. 2017, 60, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cox, T.; Griffiths, A.; Rial-Gonzalez, E. Research on Work Related Stress; Office of Official Publications of the European Communities: Luxembourg, 2000. [Google Scholar]
- Coggon, D. Occupational medicine at a turning point. Occup. Environ. Med. 2005, 65, 281–283. [Google Scholar] [CrossRef] [Green Version]
- Leka, S.; Jain, A. Health Impact of Psychosocial Hazards at Work: An Overview; World Health Organization: Geneva, Switzerland, 2010; Available online: https://apps.who.int/iris/handle/10665/44428 (accessed on 11 April 2022).
- Goetzel, R.Z.; Roemer, E.C.; Holingue, C.; Fallin, M.D.; McCleary, K.; Eaton, W.; Agnew, J.; Azocar, F.; Ballard, D.; Bartlett, J.; et al. Mental health in the workplace: A call to action; proceedings from the mental health in the workplace. Public health summit. J. Occup. Environ. Med. 2018, 60, 311–330. [Google Scholar] [CrossRef] [Green Version]
- Roehring, C. Mental disorder top the list of most costly conditions in the United States: $201 Billion. Health Aff. 2016, 35, 1113–1135. [Google Scholar] [CrossRef]
- Leka, S.; Jain, A.; Lerouge, L. Work-related Psychosocial risks: Key definitions and an overview of the policy context in Europe. In Psychosocial Risks in Labour and Social Security Law: A Comparative Legal Overview from Europe, North America, Australia and Japan; Lerouge, L., Ed.; Springer International Publishing AG: Cham, Switzerland, 2017. [Google Scholar]
- Mykletun, A.; Harvey, S.B. Prevention of mental disorders: A new era for workplace mental health. Occup. Environ. Med. 2012, 69, 868–869. [Google Scholar] [CrossRef]
- Trautmann, S.; Rehm, J.; Wittchen, H.-U. The economic costs of mental disorders. EMBO Rep. 2016, 17, 1245–1249. [Google Scholar] [CrossRef]
- Jespersen, A.H.; Hasle, P.; Nielsen, K.T. The wicked character of psychosocial risks: Implications for regulation. Nord. J. Work. Life Stud. 2016, 6, 23–42. [Google Scholar] [CrossRef] [Green Version]
- Sigahi, T.F.A.C.; Kawasaki, B.C.; Bolis, I.; Morioka, S.N. A systematic review of the impacts of Covid-19 on work: Contributions and a path forward from the perspectives of ergonomics and psychodynamics of work. Hum. Factors. Ergon. Manuf. 2021, 31, 375–388. [Google Scholar] [CrossRef]
- Schulte, P.A.; Delclos, G.; Felknor, S.A.; Chosewood, L.C. Toward an expanded focus for occupational safety and health: A commentary. Int. J. Environ. Res. Public Health 2019, 16, 4946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Felknor, S.A.; Streit, J.M.H.; McDaniel, M.; Schulte, P.A.; Chosewood, L.C.; Delclos, G.L. How will the future of work shape OSH research and practice? A workshop summary. Int. J. Environ. Res. Public Health 2021, 18, 5896. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, D. The psychologist and occupational health. In Proceedings of the Annual Conference, Ergonomics Society of Australia and New Zealand; Brebner, J., Ed.; Department of Psychology, University of Adelaide: Adelaide, Australia, 1977; pp. 41–50. [Google Scholar]
- Karasek, R.A., Jr. Job Demands, Job Decision Latitude, and Mental Strain: Implications for Job Redesign. Admin. Sci. Q. 1979, 24, 285–308. [Google Scholar] [CrossRef]
- El Batawi, M.A. Work-related diseases: A new program of the World Health Organization. Scand. J. Work Environ. Health 1984, 10, 341–346. [Google Scholar] [CrossRef]
- Samuels, S.W. (Ed.) The Environment of the Workplace and Human Values; Alan R Liss: New York, NY, USA, 1986; 118p. [Google Scholar]
- Antonovsky, A. Health promoting factors at work: The sense of coherence. In Psychosocial Factors at Work and Their Relation to Health; Cooper, C.C., Kalima, R., El-Batauri, M., Eds.; WHO: Geneva, Switzerland, 1987; pp. 153–167. [Google Scholar]
- Sauter, S.L.; Murphy, L.R.; Hurrell, J.J. Prevention of work-related psychological disorders: A national strategy proposed by the National Institute for Occupational Safety and Health (NIOSH). Am. Psychol. 1990, 45, 1146–1158. [Google Scholar] [CrossRef]
- Ilmarinen, J.; Tuomi, K.; Eskelinen, L.; Nygard, C.H.; Huuhtanen, P.; Klockars, M. Background and objectives of the Finnish research project on aging workers in municipal occupations. Scand. J. Work Environ. Health 1991, 17 (Suppl. S1), 7–11. [Google Scholar]
- Amick, B.C.; McDonough, P.; Chang, H.; Rogers, W.; Pieper, C.; Duncan, G. Relationship between all-cause mortality and cumulative life course psychosocial and physical exposure, in the United States labor market 1968 to 1992. Psychosom. Med. 2002, 64, 370–381. [Google Scholar] [CrossRef]
- Israel, B.A.; Schurman, S.J.; Hugentobler, M.K. Conducting Action Research: Relationships between Organization Members and Researchers. J. Appl. Behav. Sci. 1992, 28, 74–101. [Google Scholar] [CrossRef]
- Heaney, C.A.; Price, R.H.; Rafferty, J. Increasing coping resources at work: A field experiment to increase social support, improve work team functioning, and enhance employee mental health. J. Organ. Behav. 1995, 16, 335–353. [Google Scholar] [CrossRef]
- Sorensen, G.; Himmelstein, J.S.; Hunt, M.K.; Youngstrom, R.; Hebert, J.R.; Hammond, S.K.; Palombo, R.; Stoddard, A.; Ockene, J.K. A Model for Worksite Cancer Prevention: Integration of Health Protection and Health Promotion in the WellWorks Project. Am. J. Heal. Promot. 1995, 10, 55–62. [Google Scholar] [CrossRef]
- Quick, J.C. Editorial. J. Occup. Health. Psychol. 1996, 1, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, J. Adverse health effects of high-effort/low reward conditions. J. Occup. Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Adkins, J.A. Promoting organizational health: The evolving practices of occupational health psychology. Prof. Psychol. Res. Pract. 1999, 30, 129–137. [Google Scholar] [CrossRef]
- Dembe, A. Social inequalities in occupational health and health-care for work-related injuries and illnesses. Int. J. Law Psychiatry 1999, 22, 567–579. [Google Scholar] [CrossRef]
- Rantanen, J. Challenges for occupational health from work in the information society. Am. J. Ind. Med. Suppl. 1999, 1, 1–6. [Google Scholar] [CrossRef]
- London, L.; Kisting, S. Ethical concerns in international occupational health. Occup. Med. 2002, 17, 587–600. [Google Scholar]
- U.S. EPA. Framework for Cumulative Risk Assessment; EPA/600/P-02/001F; U.S. Environmental Protection Agency Office of Research and Development, National Center for Environmental Assessment: Washington, DC, USA, 2003. Available online: https://www.epa.gov/risk/framework-cumulative-risk-assessment (accessed on 11 April 2022).
- Lavis, J.N.; Robertson, D.; Woodside, J.M.; McLeod, C.B.; Abelson, J. How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q. 2003, 81, 221–248. [Google Scholar] [CrossRef] [Green Version]
- Quinn, M. Occupational health, public health, worker health. Am. J. Public Health 2003, 93, 526. [Google Scholar] [CrossRef]
- Putnam, K.; McKibbin, L.; Wachs, J.E. Managing workplace depression: An untapped opportunity for occupational health professionals. AAOHN J. 2004, 52, 122–129. [Google Scholar] [CrossRef] [Green Version]
- Caruso, C.C.; Bushnell, T.; Eggerth, D.; Heitmann, A.; Kojola, B.; Newman, K.; Rosa, R.R.; Sauter, S.L.; Vila, B. Long working hours safety and health: Toward a national research agenda. Am. J. Ind. Med. 2006, 49, 930–942. [Google Scholar] [CrossRef]
- Schulte, P.A. Emerging issues in occupational safety and health. Int. J. Occup. Environ. Health 2006, 12, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Bakker, A.B.; Demerouti, E. The Job Demands-Resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–322. [Google Scholar] [CrossRef]
- Westerholm, P. Professional ethics in occupational health. West. Eur. Perspect. Ind. Health 2007, 45, 19–25. [Google Scholar] [CrossRef] [Green Version]
- Black, C. Working for A Healthier Tomorrow; The Stationary Office: London, UK, 2008. Available online: https://www.gov.uk/government/publications/working-for-a-healthier-tomorrow-work-and-health-in-britain (accessed on 11 April 2022).
- Cummings, K.J.; Kreiss, K. Contingent workers and contingent health: Risks of a modern economy. JAMA 2008, 299, 448–450. [Google Scholar] [CrossRef] [PubMed]
- ILO/ISSA/KOSHA. Seoul Declaration on Safety and Health at Work. Safety and Health Summit, XVIII World Congress on Safety and Health at Work: International Labour Organization, International Social Security Association, and Korean Occupational Safety and Health Agency. Ind. Health. 2008, 46, 513–518. [Google Scholar] [CrossRef] [Green Version]
- Anttonen, H.; Räsänen, T. (Eds.) Well-Being at Work: New Innovations and Good Practices; EU Progress Booklet. Progress/application for programme VP/2007/005/371; Finnish Institute of Occupational Health: Helsinki, Finland, 2008. [Google Scholar]
- Punnett, L.; Warren, N.; Henning, R.; Nobrega, S.; Cherniack, M. CPH-New Research Team. Participatory ergonomics as a model for integrated programs to prevent chronic disease. J. Occup. Environ. Med. 2015, 51 (Suppl. S12), 519–524. [Google Scholar] [CrossRef]
- Schulte, P.A.; Chun, H. Climate change and occupational safety and health: Establishing a preliminary framework. J. Occup. Environ. Hyg. 2009, 6, 542–554. [Google Scholar] [CrossRef]
- Virtanen, M.; Singh-Manoux, A.; Ferria, J.E.; Gimeno, D.; Marmot, M.G.; Eloveinio, M.; Joketa, M.; Vantera, J.; Kivimäki, M. Long working hours and cognitive function: The whitehall II study. Am. J. Epidemiol. 2009, 16, 169, 596–605. [Google Scholar] [CrossRef]
- Johns, G. Presenteeism in the workplace: A review and research agenda. J. Organ Behav. 2010, 31, 519–542. [Google Scholar] [CrossRef]
- Bambra, C. Work, worklessness and the political economy of health inequalities. J. Epidemiol. Commun. Health 2011, 65, 746–750. [Google Scholar] [CrossRef] [Green Version]
- Dollard, M.F.; McTernan, W. Psychosocial safety climates: A multilevel theory of work stress in the health and community service sector. Epidemiol. Psychiatr. Sci. 2011, 23, 287–295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asfaw, A.; Pana-Cryan, R.; Rosa, R. Paid sick leave and non-fatal occupational injuries. Am. J. Public Health 2012, 102, e59–e64. [Google Scholar] [CrossRef] [PubMed]
- Schulte, P.A.; Pandalai, S.; Wilson, V.; Chun, H. Interaction of occupational and personal risk factors in workforce health and safety. Am. J. Public Health. 2012, 102, 43448. [Google Scholar] [CrossRef] [PubMed]
- Kranika-Murray, M.; Weyman, A.K. Optimising workplace interventions for health and well-being. A commentary on the limitations of the public health approach within the workplace health arena. IJWHM 2013, 6, 104–117. [Google Scholar] [CrossRef] [Green Version]
- Zwetsloot, G.I.; van Scheppingen, A.R.; Bos, E.H.; Dijkman, A.; Starren, A. The core values that support health safety, and well-being at work. Saf. Health Work. 2013, 4, 181–196. [Google Scholar] [CrossRef] [Green Version]
- Bauer, G.F.; Hämmig, O. Bridging Ocupational, Organizational and Public Health: A Transdisciplinary Approach; Springer: Dordrecht, The Netherlands, 2014. [Google Scholar]
- Weil, D. The Fissured Workplace: Why Work Became So Bad for So Many and What Can be Done to Improve It; Harvard University Press: Cambridge, MA, USA, 2014. [Google Scholar]
- Kang, S.-K. New concepts for occupational health development: 3 phrases. Saf. Health Work. 2015, 53, 109–111. [Google Scholar] [CrossRef] [Green Version]
- Lentz, T.J.; Dotson, S.; Williams, P.R.D.; Maier, A.; Gadagbui, B.; Pandalai, S.P.; Lamba, A.; Hearl, F.; Mamtaz, M. Aggregate exposure and cumulative rich assessment and non-occupation risk factors. JOEH 2015, 12, 5112–5126. [Google Scholar] [CrossRef] [Green Version]
- Schulte, P.A.; Guerin, R.J.; Schill, A.L.; Bhattacharya, A.; Cunningham, T.R.; Pandalai, S.P.; Eggerth, D.; Stephenson, C.M. Considerations of incorporating well-being in public policy for workers and workplaces. Am. J. Public Health 2015, 105, e31–e44. [Google Scholar] [CrossRef]
- Blustein, D.L.; Olle, C.; Connors-Kellgren, A.; Diamonti, A.J. Decent work: A psychological perspective. Front. Psychol. 2016, 7, 407. [Google Scholar] [CrossRef] [Green Version]
- DeBord, D.G.; Carreon, T.; Lentz, T.J.; Middendorf, P.J.; Hoover, M.D.; Schulte, P.A. The use of the “exposome” in the practice of epidemiology: A primer on omic-technologies. Am. J. Epidemiol. 2016, 184, 304–314. [Google Scholar] [CrossRef] [Green Version]
- Harrison, J.; Dawson, L. Occupational health: Meeting the challenges in the next 20 years. Saf. Health Work. 2016, 7, 143–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dugan, A.G.; Punnett, L. Dissemination and Implementation research for occupational safety and heats. Occup. Health Sci. 2017, 1, 29–45. [Google Scholar] [CrossRef] [PubMed]
- Ganzleben, C.; Antignac, J.-P.; Barouki, R.; Castaño, A.; Fiddicke, U.; Klánová, J.K.; Lebret, E.; Olea, N.; Sarigiannis, D.; Schoeters, G.R.; et al. Human biomonitoring as a tool to support chemicals regulation in the European Union. Int. J. Environ. Res. Public Health 2017, 220, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Oeij, P.R.A.; Rus, D.; Pot, F.D. (Eds.) Workplace Innovation: Theory, Research and Practice; Volume in a Series: Aligning Perspectives on Health, Safety and Well-Being; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Sauter, S.; Hurrell, J.J. Occupational heath contributions to the development and promise of occupational health psychology. J. Occup. Health Psychol. 2017, 22, 251–258. [Google Scholar] [CrossRef]
- Iavicoli, S.; Valenti, A.; Gagliardi, D.; Cantanen, J. Ethics and occupational health in the contemporary world and work. Int. J. Environ. Res. Public Health 2018, 15, 1713. [Google Scholar] [CrossRef] [Green Version]
- Pfeffer, J. Dying for a Paycheck; Harpers Business: New York, NY, USA, 2018. [Google Scholar]
- DeJoy, D.M.; Wilson, M.G. Total Worker Health: Evolution of the concept. In Total Worker Health®; Hudson, H.L., Nigam, J.A.S., Sauter, S.L., Chosewood, L.C., Schill, A.L., Howard, J., Eds.; American Psychological Association: Washington, DC, USA, 2019; pp. 11–28. [Google Scholar]
- Hudson, H.L.; Nigam, J.A.S.; Sauter, S.L.; Chosewood, L.C.; Schiff, A.L.; Howard, J. Total Worker Health®; American Public Health Association: Washington, DC, USA, 2019. [Google Scholar]
- ILO. Sustainable Development Goals (SDG): Goal 8. Promote Inclusive and Sustainable Growth, Employment, and Decent Work for All; International Labour Organization: Geneva, Switzerland, 2019; Available online: https://www.ilo.org/global/topics/dw4sd/theme-by-sdg-targets/WCMS_556964/lang--en/index.htm (accessed on 11 April 2022).
- Felknor, S.A.; Streit, J.M.K.; Chosewood, L.C.; McDaniel, M.; Schulte, P.A.; Delclos, G.L. How will the future of work shape the OSH professional of the future? A workshop summary. Int. J Environ. Res. Public Health 2020, 17, 7154. [Google Scholar] [CrossRef]
- Newman, L.S.; Scott, J.S.; Childness, A.; Linnan, L.; Newhall, W.J.; McLellan, D.L.; Campo, S.; Freewynn, S.; Hammer, L.B.; Leff, M.; et al. Education and training to build capacity in Total Worker Health. JOEM 2020, 62, e384–e391. [Google Scholar] [CrossRef]
- Way, K. Psychosocial hazards. In The core body of knowledge for generalist OHS professionals, 2nd ed.; Australian Institute of Health and Safety: Tullamarine, VIC, Australia, 2020. [Google Scholar]
- Guerin, R.J.; Harden, S.M.; Rabin, B.A.; Rohlman, D.S.; Cunningham, T.R.; TePoel, M.R.; Parish, M.; Glasgow, R.E. Dissemination and Implementation Science Approaches for Occupational Safety and Health Research: Implications for Advancing Total Worker Health. Int. J. Environ. Res. Public Heal. 2021, 18, 11050. [Google Scholar] [CrossRef]
- Lovejoy, M.; Kelly, E.; Kubzansky, L.; Berkman, L.F. Work redesign for the 21st century: Promising strategies for enhancing worker well-being. Am. J. Public Health 2021, 11, 1787–1795. [Google Scholar] [CrossRef]
- Pratap, P.; Dickson, A.; Love, M.; Zanoni, J.; Donato, C.; Flynn, M.; Schulte, P.A. Public health impacts of underemployment and unemployment in the United States: Exploring perceptions, gaps, and opportunities. Int. J. Environ. Res. Public Health 2021, 18, 10021. [Google Scholar] [CrossRef]
- Tamers, S.; Pana-Cryan, R.; Ruff, T.; Streit, J.; Flynn, M.; Childress, A.; Chang, C.C.; Novicki, E.; Ray, T.; Fosbroke, D.; et al. The NIOSH Future of Work Initiative Research Agenda; DHHS (NIOSH) Publication No 2022-105. NIOSH: Cincinnnati, OH, USA, 2022. Available online: www.cdc.gov/niosh/docs/2022-105/pdf/2022-105.pdf (accessed on 11 April 2022).
- Rogers, B.; Schill, A.L. Ethics and Total Worker Health®: Constructs for ethical decision-making and competencies for professional practice. Int. J. Env. Res. Public Health 2021, 18, 10030. [Google Scholar] [CrossRef] [PubMed]
- Samuels, S.W.; Ringen, K.; Rom, W.N.; Frank, A. Ethical thinking in occupational and environmental medicine: Commentaries from the Selikoff Fund for Occupational and Environmental Cancer Research. Am. J. Ind. Med. 2022, 65, 286–320. [Google Scholar] [CrossRef] [PubMed]
- Fujishiro, K.; Ahonen, E.Q.; de Porras, D.G.R.; Chen, I.-C.; Benavides, F.G. Sociopolitical values and social institutions: Study in work and health equity through the lens of the political economy. Popul. Health 2021, 14, 100787. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.A.; Check, P.; Steege, A.L.; Siven, J.M.; Syron, L.N. Health equity and a paradigm shift in occupational safety and health. Int. J. Environ. Res. Public Health 2022, 19, 349. [Google Scholar] [CrossRef] [PubMed]
- Ilmarinen, J.; Tuomi, K.; Klockars, M. Changes in the work ability of active employees over a 11-year period. Scand. J. Work Environ. Health. 1997, 23, 49–57. [Google Scholar] [PubMed]
- Chosewood, L.C.; Kirby, E. Total Worker Health Program readies NIOSH for the next 50 years. In NIOSH Science Blog; CDC: Atlanta, GA, USA, 2022. Available online: https://blogs.cdc.gov/niosh-science-blog/2022/01/18/twh-50th/ (accessed on 11 April 2022).
- Punnett, L.; Cavallari, J.M.; Henning, R.A.; Nobrega, S.; Dugan, A.G.; Cherniak, M.G. Defining ‘integration’ for Total Worker Health: A new proposal. Ann. Work. Expo. Health 2020, 64, 223–225. [Google Scholar] [CrossRef] [Green Version]
- Lovelock, K. Psychosocial Hazards in Work Environments and Effective Approaches for Managing Them; Worksafe New Zealand. April 2019. Available online: https://www.worksafe.govt.nz/research/psychosocial-hazards-in-work-environments-and-effective-approaches-for-managing-them/ (accessed on 11 April 2022).
- Wild, C. Complementing the genome with an “exposome”: The outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol. Biomarkers Prev. 2005, 14, 1847–1850. [Google Scholar] [CrossRef] [Green Version]
- NIOSH. Exposome and Exposomics; CDC: Atlanta, GA, USA. Available online: https://www.cdc.gov/niosh/topics/exposome/default.html (accessed on 11 April 2022).
- Gilles, L.; Govarts, E.; Martin, L.R.; Andersson, A.-M.; Appenzeller, B.M.R.; Barbone, F.; Castaño, A.; Coertjens, D.; Hond, E.D.; Dzhedzheia, V.; et al. Harmonization of human biomonitoring studies in Europe: Characteristics of HBM4EU-aligned studies participants. Int. J. Environ. Res. Public Health 2022, 19, 6787. [Google Scholar] [CrossRef]
- Scheepers, P.T.J.; Duca, R.C.; Galea, K.S.; Godderis, L.; Hardy, E.; Knudsen, L.E.; Leese, E.; Louro, H.; Mahiout, S.; Ndaw, S.; et al. HBM4EU Occupational biomonitoring study on e-waste—Study, protocol. Int. J. Environv. Res. Public Health 2021, 18, 12987. [Google Scholar] [CrossRef]
- Pandalai, S.P.; Schulte, P.A.; Miller, D.B. Conceptual models of the interrelationship between obesity and the occupational environment. Scand. J. Environ. Health 2013, 39, 221–232. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Healthy Workplaces: A Model for Action for Employers, Workers, Policy Makers and Practitioners; World Health Organization: Geneva, Switzerland, 2010; Available online: https://www.who.int/publications-detail-redirect/healthy-workplaces-a-model-for-action (accessed on 11 April 2022).
- DGUV. New Forms of Work, New Forms of Prevention; Deutsche-Gesetliche Unfallversicherung: Berlin, Germany, 2016; Available online: https://publikationen.dguv.de/praevention/allgemeine-informationen/3114/new-forms-of-work.-new-forms-of-prevention.-work-4.0-opportunities-and-challenges (accessed on 11 April 2022).
- Eeckelaert, L.; Dhondt, S.; Oeij, P.; Pot, F.; Nicolescu, G.I.; Webster, J.; Eisler, D. Review of Workplace Innovation and Its Relation with Occupational Safety and Health; European Agency for Safety and Health at Work: Bilbao, Spain, 2012; Available online: https://osha.europa.eu/en/publications/review-workplace-innovation-and-its-relation-occupational-safety-and-health (accessed on 11 April 2022).
- Karasek, R.A.; Theorell, T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life; Basic Books: New York, NY, USA, 1990. [Google Scholar]
- Pot, F.; Dhondt, S. Workplace innovation. In Co-Creating Humane and Innovative Organizations. Evolutions in the Practice of Socio-Technical System Design; Mohr, B.J., Van Amelsvoort, P., Eds.; Global STS-D Network Press: New York, NY, USA, 2016; pp. 201–222. ISBN 978-0692510032. [Google Scholar]
- International Labour Organisation. Istanbul Declaration on Safety and Health at Work; International Labour Organization: Geneva, Switzerland; Available online: https://www.ilo.org/safework/info/WCMS_1637//lang-en/index.htm (accessed on 11 April 2022).
- Finnish Institute of Occupational Health. Vision Zero 2019; Finnish Institute of Occupational Health: Helsinki, Finland, 2019; Available online: https://visionzero.global/vision-zero-2019-summit (accessed on 11 April 2022).
- Geisler, E. An integrated cost-performance model of public sector research evaluation. Scientometrics 1996, 36, 379–395. [Google Scholar] [CrossRef]
- Van Eerd, D.; Cole, D.; Keown, E.; Irvin, E.; Kramer, D.; Brennenman-Gibson, J.; Kazman, M.; Mahood, Q.; Slack, T.; Amick, B., III; et al. Report on Knowledge Transfer and Exchange Practices: A Systematic Review of the Quality and Types of Instruments Used to Assess KTE Implementation and Impact; Institute for Work and Health: Toronto, ON, Canada, 2011; Available online: https://www.iwh.on.ca/scientific-reports/systematic-review-of-instruments-used-to-assess-kte (accessed on 11 April 2022).
- Estabrooks, C.A.; Derksen, L.; Winther, C.; Lavis, J.N.; Scott, S.D.; Wallin, L.; Profetlo, M.; Grath, J. The intellectual structure and substance of the knowledge utilization field: A longitudinal author co-citation analysis, 1945–2004. Implement. Sci. 2008, 3, 49. [Google Scholar] [CrossRef] [PubMed]
- Rabin, B.A.; Brownson, R.C.; Haire-Joshu, D.; Kreuter, M.W.; Weaver, N.L. A glossary for dissemination and implementation research in health. J. Public Health Manag. Pract. 2008, 14, 117–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulte, P.A.; Cunningham, T.R.; Nickels, L.; Felknor, S.; Guerin, R.; Blosser, F.; Chang, C.-C.; Check, P.; Eggerth, D.; Flynn, M.; et al. Translation research in occupational safety and health: A proposed framework. Am. J. Ind. Med. 2017, 12, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- Schulte, P.; Okun, A.; Stephenson, C.; Colligan, M.; Ahlers, H.; Gjessing, C.; Loos, G.; Niemeier, R.; Sweeney, M. Information dissemination and use: Critical components in occupational safety and health. Am. J. Ind. Med. 2003, 44, 515–531. [Google Scholar] [CrossRef]
- Cunningham, T.R.; Tinc, P.J.; Guerin, R.J.; Schulte, P.A. Translation research in occupational health and safety settings: Common ground and future directions. J. Saf. Res. 2020, 14, 161–167. [Google Scholar] [CrossRef]
- Gewirth, A. Human rights and the workplace. Am. J. Industr. Med. 1986, 9, 31–40. [Google Scholar] [CrossRef]
- Yeh, M.-J.; Liu, H.-C. Comment on Iavicoli et al., Ethics and occupational health in the contemporary world of work. Int. J. Environ. Res. Public Health 2018, 15, 1713. [Google Scholar] [CrossRef] [Green Version]
- Schulte, P.A.; Sauter, S.L. Work and Well-Being: The Changing Face of Occupational Safety and Health. NIOSH Science Blog. 7 June 2021. Available online: https://blogs.cdc.gov/niosh-science-blog/2021/06/07/work-and-well-being/ (accessed on 11 April 2022).
- Stacey, N.; Ellwood, P.; Bradbrook, S.; Reynolds, J.; Williams, H.; Lye, D. Foresight on New and Emerging Occupational Safety and Health Risks Associated with Digitalization by 2025. Available online: https://osha.europa.eu/en/publications/foresightnew-and-emerging-occupational-safety-and-health-risks-associated/view (accessed on 6 November 2019).
- Delclos, G.L. Principal Investigator. U13 Cooperative Agreement: Shaping the Future to Ensure Worker Health and Well-Being: Shifting Paradigms for Research, Training and Policy; University of Texas School of Public Health/National Institute for Occupational Safety and Health: Houston, TX, USA, 2019. [Google Scholar]
- Schulte, P.A.; Vainio, H. Well-being at work: Overview and perspective. Scand. J. Work Environ. Health 2010, 36, 422–429. [Google Scholar] [CrossRef] [Green Version]
- Pratap, P. Horizontal expansion: Socioeconomic factors [Panelist]. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 11 December 2021. [Google Scholar]
- Hammer, L.B.; Brady, J.M.; Brossoit, R.M.; Mohr, C.D.; Bodner, T.E.; Crain, T.L.; Brockwood, K.J. Effects of Total Worker Health leadership intervention on employee well-being and functional impairment. J. Occup. Health. Psychol. 2021, 26, 582–598. [Google Scholar] [CrossRef] [PubMed]
- Cengiz, D.; Dube, A.; Linder, A.; Zipperer, B. The effect of minimum wages on low-wage jobs. Q. J. Econ. 2019, 134, 1405–1454. [Google Scholar] [CrossRef] [Green Version]
- Chari, R.; Sauter, S.L.; Petrun Sayers, E.L.; Huang, W.; Fisher, G.G.; Chang, C.C. Development of the National Institute for Occupational Safety and Health Worker Well-being Questionnaire. J. Occup. Environ. Med. 2022, 65, 707–717. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, L.A.; Härenstam, A.; Warren, N.A.; Punnett, L. Incorporating work organization into occupational health research: An invitation for dialogue. Occup. Environ. Med. 2008, 65, 1–3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miranda, H.; Gore, R.J.; Boyer, J.; Nobreya, S.; Punnett, L. Health behaviors and overweight in nursing home employees: Contribution of workplace stressor and implications for worksite health promotion. Sci. World J. 2015, 2015, 91539. [Google Scholar] [CrossRef] [Green Version]
- Peters, S.E.; Denerlein, J.T.; Wagner, G.R.; Sorensen, G. Work and worker health in the post pandemic world: Public health perspectives. Lancet. 2022, 7e, 188–194. [Google Scholar] [CrossRef]
- Chandola, T.; Britton, A.; Brunner, E.; Hemingway, H.; Malik, M.; Kumari, M.; Badrick, E.; Kivimaki, M.; Marmot, M. Work stress and coronary heart disease: What are the mechanisms? Eur. Heart, J. 2008, 29, 640–648. [Google Scholar] [CrossRef] [Green Version]
- Ishizaki, M.; Nakagawa, H.; Morikawa, Y.; Honda, R.; Yamada, Y.; Kawakami, N. Japan work stress and health cohort study group. Influences of job strain on changes in bay mass index and waist circumference—6 year longitudinal study. Scan J. Work. Environ. Health 2008, 34, 288–290. [Google Scholar] [CrossRef] [Green Version]
- Nobrega, S.; Kernan, L.; Plaku-Alakbarora, B.; Robertson, M.; Warren, N.; Henning, R. CPH-NEW Research Team. Field tests of a participatory ergonomics toolkit for Total Worker Health. Appl. Ergon. 2017, 60, 366–379. [Google Scholar] [CrossRef] [Green Version]
- Cherniack, M.; Berger, S.; Namazi, S.; Henning, P.; Punnett, L. A particaptory action research approach to mental health interventions among corrections officers: Standardizing priorities and maintaining design autonomy. Occup Health Sci 2019, 3, 387–409. [Google Scholar] [CrossRef]
- El Ghazari, M.; Jaegers, L.A.; Monteiro, C.E.; Grubb, P.L.; Cherniac, K. Progress in corrections worker health: The national corrections collaborative utilizing a Total Worker Health® strategy. Occup. Environ. Med. 2020, 62, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Punnett, L. Expanding our focus: From what to what. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 9 December 2021. [Google Scholar]
- Greenwood, K.; Anas, J. It’s a new era for mental health at work. Harvard Business Review. 2021. Available online: https://hbr.org/2021/10/its-a-new-era-for-mental-health-at-work (accessed on 11 April 2022).
- Bakker, A.B.; Cost, P.L. Chronic job burnout and daily functioning: A theoretical analysis. Burn. Res. 2014, 1, 112–119. [Google Scholar] [CrossRef] [Green Version]
- Schulte, P.A.; Pana-Cryan, R.; Schnorr, T.; Schill, A.L.; Guerin, R.; Felknor, S.; Wagner, G.R. An approach to assess the burden of work-related injury, disease, and distress. Am. J. Public. Health 2017, 107, 1051–1057. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Jenny, G.J.; Bauer, G.F.; Vinje, H.F.; Vogt, K.; Torp, S.; Lindstrom, B.; Espnes, G.A.; Torp, S.; Mittlemarch, M.B.; Sagy, S.; et al. The Application of Salutogenesis to Work. In The Handbook of Salutogenesis; Mittelmark, M.B., Sagy, S., Eriksson, M., Bauer, G.F., Pelikan, J.M., Lindström, B., Espnes, G.A., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; Available online: https://link.springer.com/book/10.1007/978-3-319-04600-6 (accessed on 5 October 2022).
- Bauer, G.F.; Roy, M.; Bakibinga, P.; Contu, P.; Downe, S.; Eriksson, M.; Espnes, G.A.; Jensen, B.B.; Juvinya Canal, D.; Lindstrom, B.; et al. Future directions for the concept of salutogenesis: A position article. Health Promo. Intl. 2020, 35, 187–195. [Google Scholar] [CrossRef]
- Walsh, M. Day 2 opening address. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 10 December 2021. [Google Scholar]
- Goldin, I.; Muggah, R. COVID-19 is Increasing Multiple Kinds of Inequality. Here’s What We Can Do About It.; World Economic Forum: Geneva, Switzerland, 2020; Available online: https://www.weforum.org/agenda/2020/10/covid-19-is-increasing-multiple-kinds-of-inequalities-heres-what-we-can-do-about-it/ (accessed on 11 April 2022).
- Baron, S.L.; Beard, S.; Davis, L.K.; Delp, L.; Forst, L.; Kidd-Taylor, A.; Liebman, A.K.; Linnan, L.; Punnett, L.; Welch, L.S. Promoting integrated approaches to reducing health inequities among low-income workers: Applying a social ecological framework. Am. J. Ind. Med. 2014, 57, 539–556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Do, D.P.; Frank, R.U.S. frontline workers and COVID-19 inequities. Prev. Med. 2021, 153, 106833. [Google Scholar] [CrossRef]
- Piketty, T. Capital in the Twenty-First Century; The Belknap Press of Harvard University Press: Cambridge, MA, USA, 2014. [Google Scholar]
- Leonhardt, D. Our broken economy, in one simple chat. New York Times, 7 August 2017. Available online: https://www.nytimes.com/interactive/2017/08/07/opinion/leonhardt-income-inequality.html (accessed on 11 April 2022).
- Chancel, L.; Piketty, T.; Saez, E.; Zucman, G. (Eds.) World Inequality Report 2022; World Inequality Lab: Paris, France, 2021; Available online: https://wid.world/news-article/world-inequality-report-2022/ (accessed on 11 April 2022).
- Picketty, T.; Saez, E.; Zucman, G. Distributional National Accounts; Methods and Estimates for the United States; NBER Working Paper 2294T; National Bureau of Economic Research: Cambridge, MA, USA, 2016; Available online: https://www.nber.org/papers/w22945 (accessed on 11 April 2022).
- Bryson, A.; Forth, J.; Stokes, L. The performance pay premium and wage dispersion in Britain. The Manchester School. City Res. Online 2018, 86, 139–154. [Google Scholar] [CrossRef]
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2010; Available online: https://www.who.int/publications/i/item/9789241500852 (accessed on 11 April 2022).
- Flynn, M. Work, mental health, and well-being: A biopsychosocial approach to health. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 11 December 2021. [Google Scholar]
- Pateman, C. Participation and Democratic Theory; Cambridge University Press: Cambridge, UK, 1970. [Google Scholar]
- Eldor, L.; Harpaz, I.; Westman, M. The Work/Nonwork Spillover: The Enrichment Role of Work Engagement. J Lead. Org Stud. 2020, 27, 21–34. [Google Scholar] [CrossRef]
- Meadows, D.H. Thinking in Systems; Earthscan: London, UK, 2008. [Google Scholar]
- Carey, G.; Malbon, E.; Carey, N.; Joyce, A.; Crammond, B.; Carey, A. Systems science and systems thinking for public health: A systematic review of the field. BMJ Open 2015, 5, e009002. [Google Scholar] [CrossRef]
- Nicolson, C.R.; Starfield, A.m.; Kofinas, G.P.; Kruse, J.A. 2002. Ten heuristics for interdisciplinary modeling projects. Ecosystems 2002, 5, 376–384. [Google Scholar] [CrossRef]
- Streit, J.M.K.; Felknor, S.A.; Edwards, N.T.; Howard, J. Leveraging strategic foresight to advance worker safety, health, and well-being. Int. J. Environ. Res. Public Health 2021, 18, 8477. [Google Scholar] [CrossRef] [PubMed]
- Streit, J.; Felknor, S.A.; Edwards, N.T.; Howard, J. Advancing worker safety, health, and well-being with strategic foresight. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 9 December 2021. [Google Scholar]
- Shaw, W.S.; Roelofs, C.; Punnett, L. Work environment factors and presentation of opioid-related deaths. Am. J. Public Health. 2020, 110, 1235–1241. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, D.; Davis, L.; Punnett, L.; Kriebel, D. Disparities in the deaths of despair by occupation, Massachusetts, 2005 to 2015. J. Occup. Environ. Med. 2020, 62, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Henning, R.; Wallen, N.; Robertson, M.; Faghri, P.; Chorniack, M.; The CPH-New Research Team. Workplace health protection and promotion through participatory ergonomics: An integrated approach. Public Health Rep. 2009, 24 (Suppl. S1), 26–35. [Google Scholar] [CrossRef] [Green Version]
- Haines, M.; Wilson, J.R.; Vink, P.; Koningsueld, E. Validating a framework for participatory ergonomics (the PEF). Ergonomics 2002, 45, 309–327. [Google Scholar] [CrossRef]
- Green, L.; George, A.M.; Marek, D.; Frankish, J.C.; Herbert, C.P.; Bowle, W. Guidelines to participatory research in health promotion. In Community-Based Participatory Research for Health; Minkler, M., Wellerstein, N., Eds.; Jossey-Bass: San Francisco, CA, USA, 2003; pp. 419–488. [Google Scholar]
- Loewenson, R.; Laurell, A.C.; Hogstedt, C. Participatory approaches in occupational health research: A review. Med. Lav. 1995, 86, 263–271. [Google Scholar] [CrossRef]
- Mergler, D. Worker participation in occupational health research: Theory and practice. Int. J. Health Serv. 1987, 17, 151–167. [Google Scholar] [CrossRef]
- Lacouture, A.; Breton, E.; Guichara, A.; Riddle, S. The concept of mechanism from a realist approach: A scoping review to facilitate its operationalization in public health program evaluation. Implement. Sci. 2015, 10, 153. [Google Scholar] [CrossRef] [Green Version]
- Nurjono, M.; Shrestha, P.; Lee, A.; Lim, X.Y.; Shiraz, F.; Tan, S.; Wong, S.H.; Foo, K.M.; Wee, T.; Toh, S.-A.; et al. Realist evaluation of a complex integrated care programme: Protocol for a mixed methods study. BMJ Open 2018, 8, e017111. [Google Scholar] [CrossRef] [Green Version]
- Eurofound and Cedefop. European Company Survey 2019: Workplace Practices Unlocking Employee Potential; European Company Survey 2019 series; Publications Office of the European Union: Luxembourg, 2020; Available online: https://www.eurofound.europa.eu/publications/flagship-report/2020/european-company-survey-2019-workplace-practices-unlocking-employee-potential (accessed on 11 April 2022).
- Eurofound, Cedefop. Innovation in EU Companies: Do Workplace Practices Matter? European Company Survey 2019 series; Publications Office of the European Union: Luxembourg, 2021; Available online: https://www.eurofound.europa.eu/publications/policy-brief/2021/innovation-in-eu-companies-do-workplace-practices-matter (accessed on 11 April 2022).
- Schnall, P.; Dobson, M.; Rosskam, E. (Eds.) Unhealthy Work: Causes, Consequences, Cures; Baywood Publishing: New York, NY, USA, 2009. [Google Scholar]
- Rodrik, D.; Sabel, C.F. Building a Good Jobs Economy; HKS Faculty Research Working Paper Series RWP20-001; Harvard Kennedy School: Cambridge, MA, USA, 2020; Available online: https://www.hks.harvard.edu/publications/building-good-jobs-economy (accessed on 11 April 2022).
- Evanoff, B.A.; Bohrf, K.; Wolf, L.D. Effects of a participatory ergonomics team among hospital orderlies. Am. J. Ind. Med. 1999, 35, 358–365. [Google Scholar] [CrossRef]
- Sinclair, R.C.; Cunningham, T.R.; Schulte, P.A. A model for occupational safety and health intervention diffusion to small businesses. Am. J. Ind. Med. 2015, 56, 1742–1751. [Google Scholar] [CrossRef] [PubMed]
- Jaegers, L.; Dale, A.M.; Weaver, N.; Buckholz, B.; Welch, L.; Evanoff, B. Development of a program logic model and evaluation plan for a participatory ergonomics intenention in construction. Am. J. Ind. Med. 2014, 87, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Roelofs, C.; Sugerman-Brozan, J.; Kurowski, A.; Russell, L.; Punnett, L. Promoting opioid awareness through a union-based peer training model. New Solut. 2021, 31, 286–297. [Google Scholar] [CrossRef] [PubMed]
- Warr, P.B. Decision latitude, job demands, and employee well-being. Work. Stress 1990, 4, 285–294. [Google Scholar] [CrossRef]
- Weziak-Baialowolska, D.; Bialowolski, P.; Sacco, P.L.; Wanderweele, T.J.; McNeely, E. Well-being in life and well-being at work: Which comes first? Evidence from a longitudinal study. Front. Public Health 2020, 8, 103. [Google Scholar] [CrossRef] [Green Version]
- Peters, S.E.; Sorensen, G.; Katz, J.N.; Gunderson, D.A.; Wagner, G.R. Thriving from work: Conceptualization and measurement. Int. J. Environ. Res. Public Health 2021, 18, 7196. [Google Scholar] [CrossRef]
- Chirico, F.; Heponiemi, T.; Parlou, M.; Zaffing, S.; Magnavita, N. Psychosocial risk prevention in a global health perspective. A descriptive analysis. Int. J. Environ. Res. Public Health. 2019, 16, 2470. [Google Scholar] [CrossRef] [Green Version]
- Schnall, P.L.; Landsbergis, P.A.; Baker, D. Job strain and cardiovascular disease. Ann. Rev. Public Health 1994, 15, 381–411. [Google Scholar] [CrossRef]
- Niedhammer, I.; Bertrais, S.; Witt, K. Psychosocial work exposures and health outcomes: A meta-review of 72 literature reviews with meta-analysis. Scand. J. Work. Environ. Health 2018, 47, 489–508. [Google Scholar] [CrossRef]
- Thiede, I.; Thiede, M. Quantifying the costs and benefits of occupational health and safety interventions at a Bangladesh shipbuilding company. Int. J. Occup. Environ. Med. 2015, 213, 127–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, A.; Leka, S.; Zwetsloot, G. Managing Health Safety and Well-Being. Ethics, Responsibility and Sustainability; Springer: Dordrecht, The Netherlands, 2021. [Google Scholar]
- Oakman, J.; Kinsman, N.; Stucheg, R.; Graham, M.; Woale, V. A rapid review of mental and physical health effects of working at home: How do we optimise health? BMC Public Health 2020, 20, 1825. [Google Scholar] [CrossRef] [PubMed]
- Strecher, V. Life on Purpose: How Living for What Matters Most Changes Everything; Harper: New York, NY, USA, 2016. [Google Scholar]
- Cocker, F.; Sanderson, R.; La Montagne, A.D. Estimating the economic benefits of eliminating job strain as a risk factor for depression. J. Occup. Environ. Med. 2017, 59, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Bremen, J.M.; Levanat, A.D.; Stretcher, V.; Zimmerman, E. Building Dignity and Purpose to Create Greater Performance During the Pandemic. 2020. Available online: https://www.wtwco.com/en-US/Insights/2020/10/building-dignity-and-purpose-to-create-greater-performance-and-wellbeing (accessed on 11 April 2022).
- Strecher, V. Employee Mental Health, Work Engagement, and Retention in a New Era: A New Model, New Interventions. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 11 December 2021. [Google Scholar]
- Stahl, A. What the Future of Work Means for Our Mental Health. Forbes 2020. Available online: https://www.forbes.com/sites/ashleystahl/2020/10/09/what-the-future-of-work-means-for-our-mental-health/ (accessed on 11 April 2022).
- Schaufeli, W.B.; Peeters, M.C. Job stress and burnout among correctional officers. A literature review. Int. J. Stress Mgmt. 2000, 2, 19–48. [Google Scholar] [CrossRef]
- Parker, S.K.; Morgeson, F.P.; Johns, G. One hundred years of work design research: Looking back and looking forward. J Appl. Psychol 2017, 102, 403–420. [Google Scholar] [CrossRef]
- Rössler, W. Stress, burnout, and job dissatisfaction in mental health workers. Eur. Arch. Psychiatry Clin. Neuro. Sci. 2012, 262, 65–67. [Google Scholar] [CrossRef] [Green Version]
- Hola, B.; Nowobilski, T. Analysis of the influence of socio-economic factors on occupational safety in the construction industry. Sustainability 2019, 11, 4460. [Google Scholar] [CrossRef] [Green Version]
- CSA Group. Stand-Alone Guidance: Psychological Health in the Workplace; CAN/CSA–Z1002–13/BNQ4700-803/2013; Canadian Standards Association: Toronto, ON, Canada, 2013; Available online: https://www.csagroup.org/standards/ (accessed on 11 April 2022).
- International Standards Organization. ISO 45003: Occupational Health and Safety Management—Psychological Health and Safety at Work—Guidelines for Managing Psychosocial Risks; International Standards Organization: Geneva, Switzerland, 2021; Available online: https://www.iso.org/standard/64283.html (accessed on 11 April 2022).
- Dollard, M.F.; Bailey, T. Building a psychosocial safety climate in turbulent times: The case of COVID-19. J. Appl. Psych. 2021, 106, 951–964. [Google Scholar] [CrossRef]
- Dollard, M.F.; Tuckey, M.R.; Dormann, C. Psychological safety climate moderates the job demand resource interaction in predicting work group distress. Accid. Anal. Prev. 2012, 45, 694–704. [Google Scholar] [CrossRef]
- Miller, M. Social, economic, and political forces affecting the future of occupational health nursing. AAOHN J. 1989, 37, 361–366. [Google Scholar] [CrossRef]
- Brynjolfsson, E.; McAfee, A. The Second Machine Age: Work, Proper Prosperity in a Time of Brilliant Technologies; W.W. Norton and Co.: New York, NY, USA, 2014. [Google Scholar]
- Cain, C. Future of work: Partnerships, perspectives, policy, and practice. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 10 December 2021. [Google Scholar]
- Lauer, M. The Future of Work Requires a Return to Apprenticeships; World Economic Forum: Geneva, Switzerland, 16 December 2014; Available online: https://www.weforum.org/agenda/2019/apprenticeships-future-of-work-4ir-for-training-reskilling/ (accessed on 11 April 2022).
- Osterman, P. Employment and Training for Mature Adults: The Current System and Moving Forward; Brookings Economic Studies: Washington, DC, USA, 2019; Available online: https://www.brooking.edu (accessed on 11 April 2022).
- Lagerlöf, E. Research dissemination: Proceedings of a workshop in Brussels 24th November 1998. Arb. Och Hälsa 2000, 16, 1–6. Available online: https://gupea.ub.gu.se/handle/2077/4238 (accessed on 11 April 2022).
- Choi, S.L.; Heo, W.; Cho, S.H.; Lee, P. The links between job insecurity, financial well-being and financial stress: A moderated mediation model. Int. J. Consum. Study 2020, 44, 353–360. [Google Scholar] [CrossRef]
- Main, C.J.; Shaw, W.S.; Nicholas, M.K.; Linton, S.J. System-level efforts to address pain-related workplace challenges. Pain 2022, 163, 1425–1431. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, C.E.; Gaydos, M.; Monforton, C.; Slatin, C.; Borkowski, L.; Dooley, P.; Liebman, A.; Rosenberg, E.; Shor, G.; Keifer, M. Effects of social, economic, and labor policies on occupational health disparities. Am. J. Ind. Med. 2014, 57, 557–572. [Google Scholar] [CrossRef] [PubMed]
- Piha, K.; Laaksonen, M.; Martikainen, P.; Rahkonen, O.; Lahelma, E. Socio-economic and occupational determinants of work injury absence. Eur. J. Public Health 2012, 23, 693–698. [Google Scholar] [CrossRef]
- Bushnell, T. Economic factors in safety, health and well-being and the roles of public policy. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 11 December 2021. [Google Scholar]
- Pot, F. Monotonous and Repetitive Work—Some People are more unequal Than Others; Sustainable Work in Europe. Concepts, Conditions, Challenge; Abrahamsson, K., Ennals, R., Eds.; Peter Lang: Bern, Switzerland, 2022; pp. 77–96. [Google Scholar]
- Barth, A.; Winker, R.; Ponocny-Seliger, E.; Sögner, L. Economic growth and the incidence of occupational injuries in Austria. Wien. Klin. Wochenschr. 2007, 119, 158–163. [Google Scholar] [CrossRef]
- Silver, S.R.; Li, J.; Quay, B. Employment status, unemployment duration, and health-related metrics among US adults of prime working age: Behavioral Risk Factor Surveillance System, 2018–2019. Am. J. Ind. Med. 2022, 65, 59–71. [Google Scholar] [CrossRef]
- Waring, A. The five pilars of occupational safety & health in a context of authoritarian soci-politcal climate. Saf. Sci. 2019, 117, 152–163. [Google Scholar] [CrossRef]
- The Lancet. A commission on climate change. Lancet 2009, 373, 1659. [Google Scholar] [CrossRef]
- Applebaum, K.M.; Graham, J.; Gray, G.M.; LaPumu, P.; McCormick, S.A.; Northcross, A.; Perry, M.J. An overview of occupational risks from climate change. Curr. Environ. Health Rep. 2016, 3, 13–22. [Google Scholar] [CrossRef]
- Schulte, P.A.; Battacharya, A.; Butter, C.R.; Chun, H.H.; Jacklitsch, B.; Jacobs, T.; Kiefer, M.; Lincoln, J.; Pendergrass, S.; Shire, J.; et al. Advancing the framework for considering the effects of climate change on worker safety and health. J. Occup. Environ. Hyg. 2016, 13, 847–865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kjellsrom, T.; Maitre, N.; Saget, C.; Otto, M.; Karimova, T. Working on a Warmer Planet: The Impact of Heat Stress on Labour Productivity and Decent Work; International Labor Organization: Geneva, Switzerland, 2019; Available online: https://www.ilo.org/global/publications/books/WCMS_711919/lang--en/index.htm (accessed on 11 April 2022).
- Roelofs, C.; Wegman, D. Workers: The climate canaries. Am. J. Public Health 2014, 104, 1799–1801. [Google Scholar] [CrossRef] [PubMed]
- Charlson, F.; Ali, S.; Bermarhnia, T.; Pearl, M.; Massozza, A.; Augustinavicius, J.; Scott, J. Climate change and mental health: A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 4484. [Google Scholar] [CrossRef] [PubMed]
- Azzi, M. Managing work-related psychosocial risks during the pandemic and beyond. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 10 December 2021. [Google Scholar]
- International Labour Organisation. Managing Work-Related Psychosocial Risks During the COVID-19 Pandemic; International Labour Organization: Geneva, Switzerland, 2020; Available online: https://www.ilo.org/global/topics/safety-and-health-at-work/resources-library/publications/WCMS_748638/lang--en/index.htm (accessed on 11 April 2022).
- de Jong, T.; Wiezer, N.; De Weerd, M.; Nielsen, K.; Mattila-Holappa, P.; Mockallo, Z. The impact of restructuring on employee well-being: A systematic review of longitudinal studies. Work. Stress 2016, 30, 91–114. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B.; Van Rhenen, W. How changes in job demands and resources predict burnout, work engagement, and sickness absenteeism. J. Organ. Behav. 2007, 30, 893–917. [Google Scholar] [CrossRef] [Green Version]
- Van der Weele, T.J.; Fulks, J.; Plake, J.F.; Lee, M.T. National well-being measures before and during the COVID-19 pandemic in online samples. J. Gen. Intern. Med. 2021, 36, 248–250. [Google Scholar] [CrossRef]
- Dennerlein, J. Improving COVID-19 policies and practices using total worker ealth approaches for essential workplaces: A case study in the energy supply sector. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 9 December 2021. [Google Scholar]
- Leff, M. Assessing the impact of COVID-19 on small and medium sized businesses: The Carolina PROSPER worksite impact survey. In Proceedings of the Expanded Focus for Occupational Safety and Health (Ex4OSH) International Conference, Houston, TX, USA, 11 December 2021. [Google Scholar]
- Hines, A.; Bishop, P. Thinking about the Future; Guidelines for Strategic Foresight, 2nd ed.; Hinesight: Houston, TX, USA, 2015. [Google Scholar]
- Bishop, P.; Hines, A. Teaching about the Future; Palgrave Macmillan: New York, NY, USA, 2012. [Google Scholar]
- NIOSH. Strategic Foresight at NIOSH; NIOSH: Washington, DC, USA. Available online: https://www.cdc.gov/niosh/topics/foresight/ (accessed on 11 April 2022).
- Lax, M.B. The perils of integrating wellness and safety and health and possibility of a worker-oriented alternative. New Solut. 2016, 26, 11–39. [Google Scholar] [CrossRef]
| Work | Workforce | Workplace |
|---|---|---|
| Mosaic of old and new hazards Shift from physical to mental work More service work Work intensification Many jobs in a working lifetime Emotional labor | Greater distribution of older workers More immigrants More women Less unionization Increased chronic disease burden | New work arrangements More telecommuting Contractors and temporary workers More small businesses Decrease in social protection Pandemics Increased climate-related hazards |
| Theme | Key Issues | Recommendations |
|---|---|---|
| Worker health inequalities |
|
|
| Training new OSH professionals |
|
|
| Future of OSH research and practice |
|
|
| Tools to measure well-being of workers |
|
|
| Psychosocial hazards and adverse mental health effects |
|
|
| Skilling, upskilling and improving job quality |
|
|
| Socioeconomic influences |
|
|
| Climate change |
|
|
| COVID-19 pandemic influences on OSH |
|
|
| Content Area | Examples |
|---|---|
| New Investigation Strategies | Biopsychosocial model of OSH Systems thinking Futures thinking |
| Technology | Digitalization Societal reliance on technology Human-machine interface |
| Organizational Development | Organizational change Change management |
| Data Techniques | Data collection Data management Data analysis Data interpretation |
| Interpersonal skills | Social skills Communication Emotional intelligence Transdisciplinary teamwork |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schulte, P.A.; Delclos, G.L.; Felknor, S.A.; Streit, J.M.K.; McDaniel, M.; Chosewood, L.C.; Newman, L.S.; Bhojani, F.A.; Pana-Cryan, R.; Swanson, N.G. Expanding the Focus of Occupational Safety and Health: Lessons from a Series of Linked Scientific Meetings. Int. J. Environ. Res. Public Health 2022, 19, 15381. https://doi.org/10.3390/ijerph192215381
Schulte PA, Delclos GL, Felknor SA, Streit JMK, McDaniel M, Chosewood LC, Newman LS, Bhojani FA, Pana-Cryan R, Swanson NG. Expanding the Focus of Occupational Safety and Health: Lessons from a Series of Linked Scientific Meetings. International Journal of Environmental Research and Public Health. 2022; 19(22):15381. https://doi.org/10.3390/ijerph192215381
Chicago/Turabian StyleSchulte, Paul A., George L. Delclos, Sarah A. Felknor, Jessica M. K. Streit, Michelle McDaniel, L. Casey Chosewood, Lee S. Newman, Faiyaz A. Bhojani, Rene Pana-Cryan, and Naomi G. Swanson. 2022. "Expanding the Focus of Occupational Safety and Health: Lessons from a Series of Linked Scientific Meetings" International Journal of Environmental Research and Public Health 19, no. 22: 15381. https://doi.org/10.3390/ijerph192215381