The Sex and Race/Ethnicity-Specific Relationships of Abdominal Fat Distribution and Anthropometric Indices in US Adults
Abstract
:1. Introduction
2. Method
2.1. Demographics
2.2. Anthropometrics
2.3. Abdominal Fat Distribution
2.4. Data Analysis
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ansari, S.; Haboubi, H.; Haboubi, N. Adult obesity complications: Challenges and clinical impact. Ther. Adv. Endocrinol. Metab. 2020, 11, 2042018820934955. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.S.; Stanforth, P.R.; Gagnon, J.; Rankinen, T.; Leon, A.S.; Rao, D.C.; Skinner, J.S.; Bouchard, C.; Wilmore, J.H. The effect of sex, age and race on estimating percentage body fat from body mass index: The heritage family study. Int. J. Obes. 2002, 26, 789–796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallagher, D.; Visser, M.; Sepulveda, D.; Pierson, R.N.; Harris, T.; Heymsfield, S.B. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am. J. Epidemiol. 1996, 143, 228–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flegal, K.M.; Shepherd, J.A.; Looker, A.C.; Graubard, B.I.; Borrud, L.G.; Ogden, C.L.; Harris, T.B.; Everhart, J.E.; Schenker, N. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am. J. Clin. Nutr. 2009, 89, 500–508. [Google Scholar] [CrossRef] [Green Version]
- Camhi, S.M.; Bray, G.A.; Bouchard, C.; Greenway, F.L.; Johnson, W.D.; Newton, R.L.; Ravussin, E.; Ryan, D.H.; Smith, S.R.; Katzmarzyk, P.T. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: Sex and race differences. Obesity 2011, 19, 402–408. [Google Scholar] [CrossRef]
- Janssen, I.; Heymsfield, S.B.; Allison, D.B.; Kotler, D.P.; Ross, R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am. J. Clin. Nutr. 2002, 75, 683–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fryar, C.D.; Gu, Q.; Ogden, C.L.; Flegal, K.M. Anthropometric Reference Data for Children and Adults: United States, 2011–2014. Vital Health Stat. 2016, 3, 1–46. [Google Scholar]
- Romero-Corral, A.; Somers, V.K.; Sierra-Johnson, J.; Thomas, R.J.; Collazo-Clavell, M.L.; Korinek, J.; Allison, T.G.; Batsis, J.A.; Sert-Kuniyoshi, F.H.; Lopez-Jimenez, F. Accuracy of body mass index in diagnosing obesity in the adult general population. Int. J. Obes. 2008, 32, 959–966. [Google Scholar] [CrossRef] [Green Version]
- Ostchega, Y.; Seu, R.; Sarafrazi, N.; Zhang, G.; Hughes, J.P.; Miller, I. Waist Circumference Measurement Methodology Study: National Health and Nutrition Examination Survey, 2016. Vital Health Stat. 2019, 2, 1–20. [Google Scholar]
- Karelis, A.D.; St-Pierre, D.H.; Conus, F.; Rabasa-Lhoret, R.; Poehlman, E.T. Metabolic and body composition factors in subgroups of obesity: What do we know? J. Clin. Endocrinol. Metab. 2004, 89, 2569–2575. [Google Scholar] [CrossRef]
- Phillips, C.M. Metabolically healthy obesity: Definitions, determinants and clinical implications. Rev. Endocr. Metab. Disord. 2013, 14, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Neeland, I.J.; Turer, A.T.; Vega, G.L. Waist circumference as measure of abdominal fat compartments. J. Obes. 2013, 2013, 454285. [Google Scholar] [CrossRef] [PubMed]
- Vasudev, S.; Mohan, A.; Mohan, D.; Farooq, S.; Raj, D.; Mohan, V. Validation of body fat measurement by skinfolds and two bioelectric impedance methods with DEXA–the Chennai Urban Rural Epidemiology Study [CURES-3]. J. Assoc. Physicians India 2004, 52, 877–881. [Google Scholar] [PubMed]
- Pasanta, D.; Htun, K.T.; Pan, J.; Tungjai, M.; Kaewjaeng, S.; Chancharunee, S.; Tima, S.; Kim, H.J.; Kæwkhao, J.; Kothan, S. Waist Circumference and BMI Are Strongly Correlated with MRI-Derived Fat Compartments in Young Adults. Life 2021, 11, 643. [Google Scholar] [CrossRef] [PubMed]
- Kuk, J.L.; Lee, S.; Heymsfield, S.B.; Ross, R. Waist circumference and abdominal adipose tissue distribution: Influence of age and sex. Am. J. Clin. Nutr. 2005, 81, 1330–1334. [Google Scholar] [CrossRef] [Green Version]
- Gadekar, T.; Dudeja, P.; Basu, I.; Vashisht, S.; Mukherji, S. Correlation of visceral body fat with waist-hip ratio, waist circumference and body mass index in healthy adults: A cross sectional study. Med. J. Armed Forces India 2020, 76, 41–46. [Google Scholar] [CrossRef]
- Hill, J.O.; Sidney, S.; Lewis, C.E.; Tolan, K.; Scherzinger, A.L.; Stamm, E.R. Racial differences in amounts of visceral adipose tissue in young adults: The CARDIA (Coronary Artery Risk Development in Young Adults) study. Am. J. Clin. Nutr. 1999, 69, 381–387. [Google Scholar] [CrossRef] [Green Version]
- Carroll, J.F.; Chiapa, A.L.; Rodriquez, M.; Phelps, D.R.; Cardarelli, K.M.; Vishwanatha, J.K.; Bae, S.; Cardarelli, R. Visceral fat, waist circumference, and BMI: Impact of race/ethnicity. Obesity 2008, 16, 600–607. [Google Scholar] [CrossRef]
- Kaess, B.M.; Pedley, A.; Massaro, J.M.; Murabito, J.; Hoffmann, U.; Fox, C.S. The ratio of visceral to subcutaneous fat, a metric of body fat distribution, is a unique correlate of cardiometabolic risk. Diabetologia 2012, 55, 2622–2630. [Google Scholar] [CrossRef] [Green Version]
- Kwon, S.; Han, A.L. The Correlation between the Ratio of Visceral Fat Area to Subcutaneous Fat Area on Computed Tomography and Lipid Accumulation Product as Indexes of Cardiovascular Risk. J. Obes. Metab. Syndr. 2019, 28, 186–193. [Google Scholar] [CrossRef]
- Fox, C.S.; Massaro, J.M.; Hoffmann, U.; Pou, K.M.; Maurovich-Horvat, P.; Liu, C.Y.; Vasan, R.S.; Murabito, J.M.; Meigs, J.B.; Cupples, L.A.; et al. Abdominal visceral and subcutaneous adipose tissue compartments: Association with metabolic risk factors in the Framingham Heart Study. Circulation 2007, 116, 39–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available online: https://wwwn.cdc.gov/nchs/nhanes (accessed on 2 July 2022).
- National Center for Health Statistics. NHANES Questionnaires, Datasets, and Related Documentation. Available online: https://wwwn.cdc.gov/nchs/nhanes/default.aspx (accessed on 20 January 2022).
- Xu, F.; Earp, J.E.; LoBuono, D.L.; Greene, G.W. The Relationship of Physical Activity and Dietary Quality with Android Fat Composition and Distribution in US Adults. Nutrients 2022, 14, 2804. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. About Adult BMI. Available online: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html (accessed on 18 June 2022).
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.H.; Kang, B.K.; Ahn, B.K. Higher visceral fat area/subcutaneous fat area ratio measured by computed tomography is associated with recurrence and poor survival in patients with mid and low rectal cancers. Int. J. Colorectal Dis. 2018, 33, 1303–1307. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics. NHANES Survey Methods and Analytic Guidelines. Available online: https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx#estimation-and-weighting-procedures (accessed on 20 June 2022).
- Kanaley, J.A.; Giannopoulou, I.; Tillapaugh-Fay, G.; Nappi, J.S.; Ploutz-Snyder, L.L. Racial differences in subcutaneous and visceral fat distribution in postmenopausal black and white women. Metabolism 2003, 52, 186–191. [Google Scholar] [CrossRef]
- Hoffman, D.J.; Wang, Z.; Gallagher, D.; Heymsfield, S.B. Comparison of visceral adipose tissue mass in adult African Americans and whites. Obes. Res. 2005, 13, 66–74. [Google Scholar] [CrossRef]
- Weinsier, R.L.; Hunter, G.R.; Gower, B.A.; Schutz, Y.; Darnell, B.E.; Zuckerman, P.A. Body fat distribution in white and black women: Different patterns of intraabdominal and subcutaneous abdominal adipose tissue utilization with weight loss. Am. J. Clin. Nutr. 2001, 74, 631–636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Despres, J.P.; Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 2006, 444, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Hamdy, O.; Porramatikul, S.; Al-Ozairi, E. Metabolic obesity: The paradox between visceral and subcutaneous fat. Curr. Diabetes Rev. 2006, 2, 367–373. [Google Scholar] [CrossRef]
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and Cardiovascular Disease: Pathophysiology, Evaluation, and Effect of Weight Loss. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 968–976. [Google Scholar] [CrossRef]
- Toth, M.J.; Tchernof, A.; Sites, C.K.; Poehlman, E.T. Menopause-related changes in body fat distribution. Ann. N. Y. Acad. Sci. 2000, 904, 502–506. [Google Scholar] [CrossRef] [PubMed]



| Variables | Total | Male | Female | p Values |
|---|---|---|---|---|
| n = 11,943 | 6049 (51.6%) | 5894 (48.4%) | ||
| Age (years) | 39.69 ± 0.23 | 39.33 ± 0.22 | 40.08 ± 0.30 | <0.001 * |
| Race/ethnicity, n (weighted %) | ||||
| White | 4161 (61.7) | 2144 (61.6) | 2017 (61.8) | 0.768 |
| Black | 2671 (11.8) | 1322 (11.3) | 1349 (12.4) | 0.01 * |
| Hispanic | 2896 (17.0) | 1416 (17.7) | 1480 (16.3) | 0.003 * |
| Asian | 1695 (5.8) | 881 (5.6) | 814 (5.9) | 0.164 |
| Others | 520 (3.8) | 286 (3.9) | 234 (3.6) | 0.589 |
| Education, n (weighted %) | ||||
| High school or less | 4789 (34.7) | 2674 (38.7) | 2115 (30.4) | <0.001 * |
| Some college or more | 7152 (65.3) | 3375 (61.3) | 3777 (69.6) | <0.001 * |
| Ratio of family income to poverty, n (weighted %) | ||||
| <1.0 | 2495 (15.8) | 1189 (14.7) | 1306 (17.1) | <0.001 * |
| ≥1.0 | 8465 (84.2) | 4342 (85.3) | 4123 (82.9) | <0.001 * |
| Body mass index (kg/m2) | 29.01 ± 0.13 | 28.81 ± 0.14 | 29.23 ± 0.18 | <0.001 * |
| Weight status, n (weighted %) | ||||
| Underweight | 214 (1.5) | 93 (1.2) | 121 (1.9) | 0.004 * |
| Normal | 3402 (28.2) | 1654 (25.1) | 1748 (31.6) | <0.001 * |
| Overweight | 3721 (32.0) | 2169 (36.5) | 1552 (27.2) | <0.001 * |
| Obese | 4532 (37.6) | 2095 (36.6) | 2437 (38.7) | 0.11 |
| Waist circumference (cm) | 98.27 ± 0.33 | 100.26 ± 0.37 | 96.14 ± 0.43 | <0.001 * |
| Abdominal obesity, n (weighted %) | 6082 (52.6) | 2327 (42.2) | 3755 (63.8) | <0.001 * |
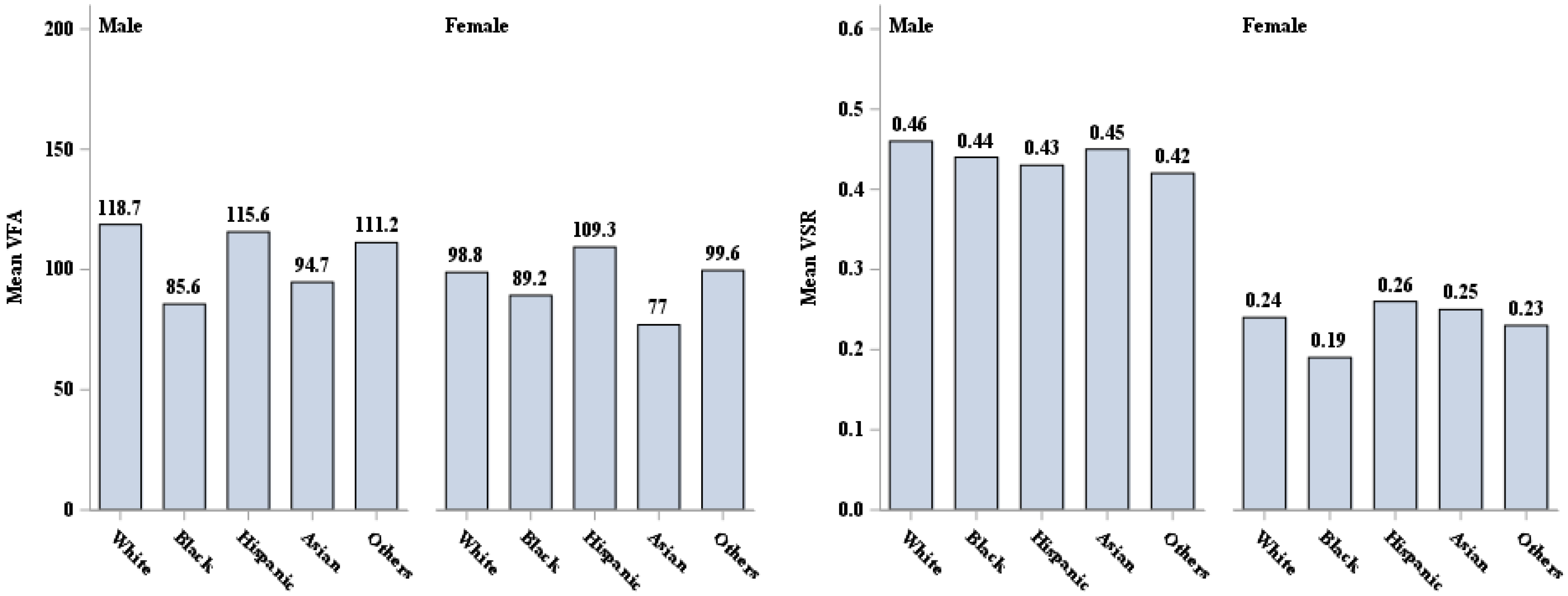
| VFA (cm2) | 105.68 ± 1.19 | 112.79 ± 1.36 | 98.09 ± 1.47 | <0.001 * |
| VSR | 0.35 ± 0.00 | 0.45 ± 0.00 | 0.24 ± 0.00 | <0.001 * |
| Overall | Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Adj. β (95% CI) | p-Value | R-Square | Adj. β (95% CI) | p-Value | R-Square | Adj. β (95% CI) | p-Value | R-Square | |
| BMI | |||||||||
| Total | 5.86 (5.56, 6.15) | <0.001 * | 0.609 | 6.12 (5.74, 6.51) | <0.001 * | 0.598 | 5.67 (5.32, 6.01) | <0.001 * | 0.619 |
| White | 6.40 (6.02, 6.78) abc | <0.001 * | 0.633 | 6.70 (6.14, 7.26) abc | <0.001 * | 0.603 | 6.18 (5.73, 6.63) abc | <0.001 * | 0.654 |
| Black | 3.79 (3.42, 4.16) adef | <0.001 * | 0.508 | 4.24 (3.79, 4.70) adef | <0.001 * | 0.56 | 3.51 (3.09, 3.93) adef | <0.001 * | 0.471 |
| Hispanic | 5.63 (5.19, 6.08) bd | <0.001 * | 0.570 | 5.66 (4.91, 6.41) bd | <0.001 * | 0.549 | 5.62 (5.17, 6.07) bdg | <0.001 * | 0.589 |
| Asian | 6.04 (5.43, 6.64) e | <0.001 * | 0.589 | 5.40 (4.56, 6.25) ce | <0.001 * | 0.495 | 6.59 (5.97, 7.22) egh | <0.001 * | 0.657 |
| Others | 5.51 (5.11, 5.91) cf | <0.001 * | 0.641 | 5.79 (5.13, 6.44) f | <0.001 * | 0.664 | 5.34 (4.70, 5.99) cfh | <0.001 * | 0.628 |
| p-value for interaction term (BMI × race) | <0.001 * | <0.001 * | <0.001 * | ||||||
| WC | |||||||||
| Total | 2.64 (2.53, 2.75) | <0.001 * | 0.684 | 2.60 (2.48, 2.72) | <0.001 * | 0.673 | 2.67 (2.53, 2.80) | <0.001 * | 0.690 |
| White | 2.85 (2.72, 2.99) abcd | <0.001 * | 0.710 | 2.84 (2.67, 3.01) abcd | <0.001 * | 0.684 | 2.85 (2.69, 3.01) a | <0.001 * | 0.723 |
| Black | 1.75 (1.61, 1.89) aefg | <0.001 * | 0.583 | 1.77 (1.61, 1.93) aefg | <0.001 * | 0.633 | 1.73 (1.56, 1.91) bcd | <0.001 * | 0.538 |
| Hispanic | 2.64 (2.50, 2.79) be | <0.001 * | 0.657 | 2.52 (2.29, 2.76) be | <0.001 * | 0.635 | 2.75 (2.58, 2.91) ab | <0.001 * | 0.677 |
| Asian | 2.67 (2.46, 2.87) cf | <0.001 * | 0.678 | 2.41 (2.13, 2.69) cf | <0.001 * | 0.625 | 2.94 (2.69, 3.19) ce | <0.001 * | 0.714 |
| Others | 2.46 (2.25, 2.68) dg | <0.001 * | 0.677 | 2.35 (2.03, 2.67) dg | <0.001 * | 0.696 | 2.60 (2.28, 2.92) de | <0.001 * | 0.661 |
| p-value for interaction term (WC × race) | <0.001 * | <0.001 * | <0.001 * | ||||||
| Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adj. β1 (95% CI) (Linear) | p-Value (Linear) | Adj. β2 (95% CI) (Quadratic) | p-Value (Quadratic) | R-Square | Adj. β1 (95% CI) (Linear) | p-Value (Linear) | Adj. β2 (95% CI) (Quadratic) | p-Value (Quadratic) | R-Square | |
| BMI | ||||||||||
| Total | −0.0469 (−0.0523, −0.0414) | <0.001 * | 0.0006 (0.0005, 0.0006) | <0.001 * | 0.308 | 0.0155 (0.0130, 0.0180) | <0.001 * | −0.0002 (−0.0002, −0.0001) | <0.001 * | 0.290 |
| White | −0.0400 (−0.0484, −0.0316) a | <0.001 * | 0.0005 (0.0003, 0.0006) a | <0.001 * | 0.272 | 0.0152 (0.0113, 0.0191) a | <0.001 * | −0.0002 (−0.0002, −0.0001) a | <0.001 * | 0.289 |
| Black | −0.0899 (−0.1001, −0.0797) abcd | <0.001 * | 0.0011 (0.0009, 0.0012) abcd | <0.001 * | 0.531 | 0.0055 (0.0015, 0.0096) abcd | 0.008 * | −0.0001 (−0.0001, −0.0000) abc | 0.006 * | 0.166 |
| Hispanic | −0.0335 (−0.0455, −0.0215) be | <0.001 * | 0.0004 (0.0002, 0.0005) be | <0.001 * | 0.327 | 0.0200 (0.0155, 0.0246) b | <0.001 * | −0.0003 (−0.0003, −0.0002) b | <0.001 * | 0.286 |
| Asian | −0.0402 (−0.0538, −0.0266) cf | <0.001 * | 0.0005 (0.0003, 0.0007) c | <0.001 * | 0.342 | 0.0201 (0.0093, 0.0309) c | <0.001 * | −0.0003 (−0.0005, −0.0001) c | 0.013 * | 0.331 |
| Others | −0.0643 (−0.0810, −0.0476) def | <0.001 * | 0.0008 (0.0006, 0.0011) de | <0.001 * | 0.453 | 0.0150 (0.0045, 0.0254) d | 0.006 * | −0.0002 (−0.0003, −0.0001) | 0.014 * | 0.244 |
| p-value for interaction term (BMI × race) | <0.001 * | <0.001 * | <0.001 * | <0.001 * | ||||||
| WC | ||||||||||
| Total | −0.0289 (−0.0322, −0.0256) | <0.001 * | 0.0001 (0.0001, 0.0001) | <0.001 * | 0.331 | 0.0087 (0.0073, 0.0101) | <0.001 * | −0.0001 (−0.0001, −0.0000) | <0.001 * | 0.316 |
| White | −0.0254 (−0.0307, −0.0201) a | <0.001 * | 0.0001 (0.0001, 0.0001) a | <0.001 * | 0.286 | 0.0087 (0.0067, 0.0106) a | <0.001 * | −0.0001 (−0.0001, −0.0000) | <0.001 * | 0.326 |
| Black | −0.0456 (−0.0504, −0.0408) abcd | <0.001 * | 0.0002 (0.0002, 0.0002) abcd | <0.001 * | 0.575 | 0.0041 (0.0008, 0.0074) abcd | 0.014 * | −0.0001 (−0.0001, −0.0000) bcd | 0.019 * | 0.167 |
| Hispanic | −0.0192 (−0.0257, −0.0127) be | <0.001 * | 0.0001 (0.0000, 0.0001) be | <0.001 * | 0.330 | 0.0107 (0.0079, 0.0135) b | <0.001 * | −0.0001 (−0.0001, −0.0000) b | <0.001 * | 0.298 |
| Asian | −0.0235 (−0.0322, −0.0149) c | <0.001 * | 0.0001 (0.0001, 0.0001) c | <0.001 * | 0.348 | 0.0126 (0.0081, 0.0171) c | <0.001 * | −0.0001 (−0.0001, −0.0000) c | <0.001 * | 0.359 |
| Others | −0.0332 (−0.0403, −0.0260) de | <0.001 * | 0.0001 (0.0001, 0.0002) de | <0.001 * | 0.482 | 0.0108 (0.0032, 0.0184) b | 0.006 * | −0.0000 (−0.0001, −0.0000) b | 0.013 * | 0.280 |
| p-value for interaction term (WC × race) | <0.001 * | <0.001 * | <0.001 * | <0.001 * | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, F.; Earp, J.E.; Adami, A.; Lofgren, I.E.; Delmonico, M.J.; Greene, G.W.; Riebe, D. The Sex and Race/Ethnicity-Specific Relationships of Abdominal Fat Distribution and Anthropometric Indices in US Adults. Int. J. Environ. Res. Public Health 2022, 19, 15521. https://doi.org/10.3390/ijerph192315521
Xu F, Earp JE, Adami A, Lofgren IE, Delmonico MJ, Greene GW, Riebe D. The Sex and Race/Ethnicity-Specific Relationships of Abdominal Fat Distribution and Anthropometric Indices in US Adults. International Journal of Environmental Research and Public Health. 2022; 19(23):15521. https://doi.org/10.3390/ijerph192315521
Chicago/Turabian StyleXu, Furong, Jacob E. Earp, Alessandra Adami, Ingrid E. Lofgren, Matthew J. Delmonico, Geoffrey W. Greene, and Deborah Riebe. 2022. "The Sex and Race/Ethnicity-Specific Relationships of Abdominal Fat Distribution and Anthropometric Indices in US Adults" International Journal of Environmental Research and Public Health 19, no. 23: 15521. https://doi.org/10.3390/ijerph192315521
APA StyleXu, F., Earp, J. E., Adami, A., Lofgren, I. E., Delmonico, M. J., Greene, G. W., & Riebe, D. (2022). The Sex and Race/Ethnicity-Specific Relationships of Abdominal Fat Distribution and Anthropometric Indices in US Adults. International Journal of Environmental Research and Public Health, 19(23), 15521. https://doi.org/10.3390/ijerph192315521







