Effectiveness and Cost-Effectiveness of Mental Health Interventions Delivered by Frontline Health Care Workers in Emergency Health Services: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
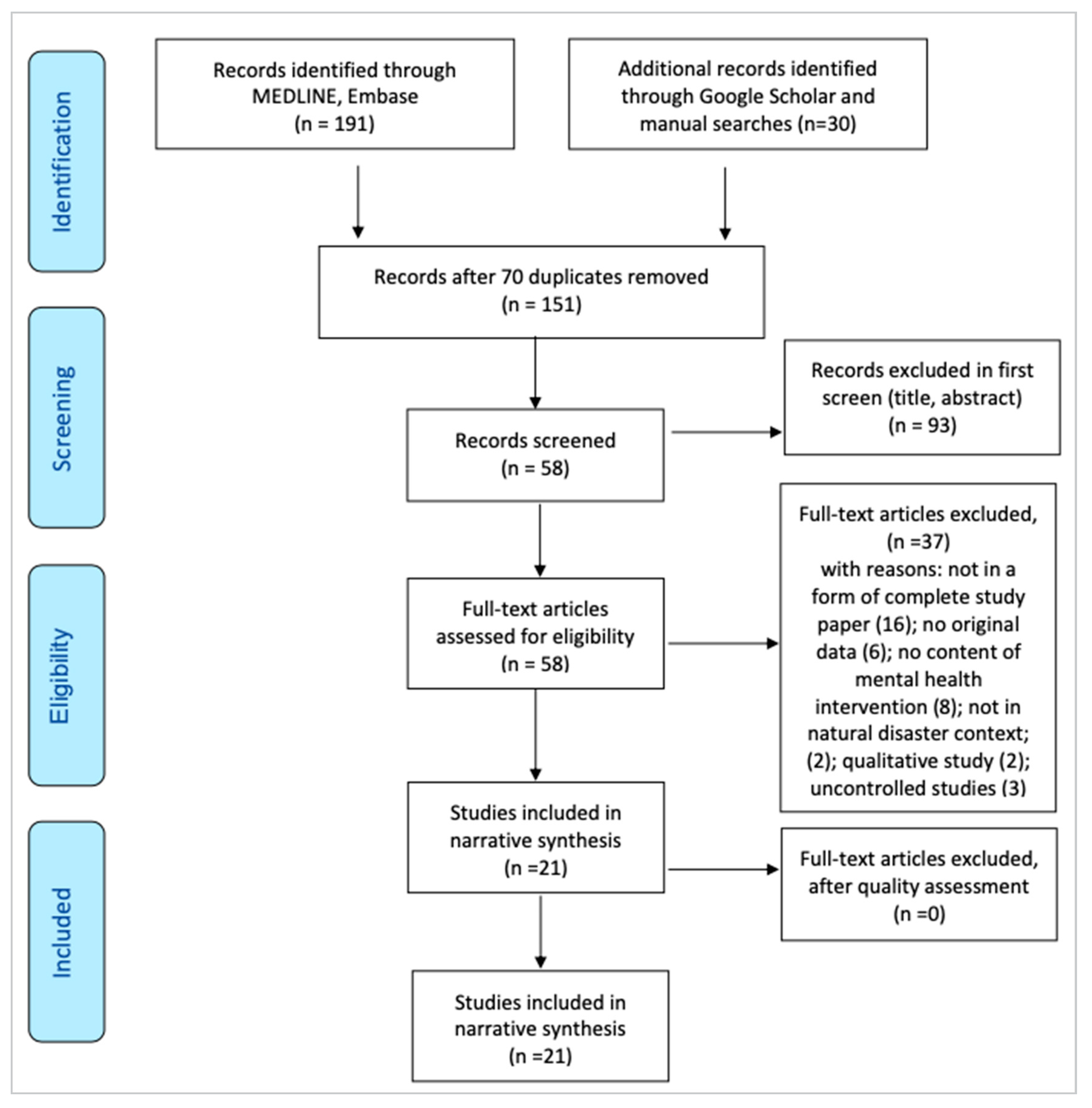
2. Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Selection Process and Data Extraction
| Author and Year | Country of Origin | Disaster and Year | Study Design and Participants | Intervention | Comparators | Primary Outcome Measures |
|---|---|---|---|---|---|---|
| 1. (Başoğlu, 2005) [14] | Turkey | 1999 Earthquake | Study design: Randomised control trial. N = 59. Survivors of earthquake Mean age: 36.3 years (16–65 years) Experimental Group/s: intervention n = 31; waitlist control n = 28 | Brief behavioral treatment | Waitlist control | Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) [26] |
| 2. (Wolmer, 2005) [27] | Turkey | 1999 Earthquake | Study design: Controlled before and after study. N = 287. Students studied in three schools located in the disaster area. Mean age: 11.5 years (Children aged 9–17 years) Experimental Group/s: intervention n = 67; control n = 220. | School reactivation program | No treatment | The Child Post-Traumatic Stress Disorder Reaction Index (CPTSD-RI; Pynoos et al., 1987) [28] |
| 3. (Steinmetz, 2012) [29] | USA | Hurricane | Study design: Randomised control trial. N = 56. Survivors from previous stress study. Mean age: 43 years Experimental Group/s: intervention n = 18; control (UC) n = 19; information only n = 19 | Internet-based psychoeducation | Usual care or Information only | Trauma Screening Questionnaire (Brewin et al., 2002) [30] |
| 4. (Zang, 2013) [31] | China | Earthquake | Study design: Randomised control trial. N = 22. People severely affected by earthquake Mean age: 55.73 years Experimental Group/s: intervention n = 11; waitlist control n = 11 | Narrative Exposure Therapy (NET) | Waitlist control | Impact of Event Scale-Revised (IES-R) (Weiss, 2007) [32]; General Health Questionnaire-28 (Goldberg and Hillier, 1979) [33] |
| 5. (Adams, 2013) [34] | USA | Large-scale community disaster | Study design: Controlled before and after study N = 215. Primary care paediatricians. Mean age: n/a Experimental Group/s: intervention n = 137; control n = 78 | RCI training | N/A | Practice change survey |
| 6. (Zang, 2014) [35] | China | 2008 Earthquake | Study design: Randomised control trial. N = 30. Adults affected by the earthquake Mean age: 53.63 years Experimental Group/s: intervention NET n = 10, NET-R n = 10; waitlist control n = 10 | Narrative Exposure Therapy (NET) | Waitlist control | Impact of Event Scale-Revised (IES-R) (Weiss, 2007) [32] |
| 7. (Jiang, 2014) [36] | China | 2008 Earthquake | Study design: Randomised control trial. N = 49. Mean age: 29.8 years Experimental Group/s: intervention n = 27; treat as usual n = 22 | Interpersonal Psychotherapy (IPT), a 12-week structured psychotherapy | TAU | Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) [26] |
| 8. (Jacob, 2014) [37] | Rwanda | 1994 Rwandan genocide | Study design: Randomised control trial. N = 76. Typical age: 47.55 years (widow); 24.55 years (orphan) Experimental Group/s: intervention n = 38; waitlist control n = 38 | Narrative exposure therapy (NET) treatment | Waitlist control | Clinician-Administered PTSD Scale (CAPS) |
| 9. (Ruggiero, 2015) [38] | USA | Tornadoes | Study design: Randomised control trial N = 2000. Adolescents and parents from communities affected by tornadoes Mean age: 14.55 years (12–17 years) Experimental Group/s: intervention BBN n = 364, BBN + ASH n = 366; control n = 257 | Bounce Back Now (BBN), a modular web-based intervention; BBN plus a 7-module adult self-help (ASH) intervention | No treatment | Adolescent symptoms of post-traumatic stress disorder (PTSD) and depression assessed using the National Survey of Adolescents (NSA) PTSD module (Kilpatrick et al., 2003) [39] |
| 10. (Bass, 2016) [40] | Iraq | Conflict and displacement | Study design: Randomised control trial N = 209. Population in the northern Dohuk region Mean age: 40 years (18–82 years) Experimental Group/s: intervention n = 159; control n = 50 | A 2-week training program that emphasized a social work model of helping and support. | Waitlist control | The Hopkins Symptom Checklist-25 (HSCL-2528,29 (a 25-item version of the HSCL) for symptoms of depression and anxiety (American Psychiatric Association, 1994) [41] |
| 11. (Acarturk, 2016) [11] | Syria | Humanitarian trauma | Study design: Randomised control trial N = 70. Adult refugees located in Kilis Refugee Camp at the Turkish–Syrian border with a PTSD diagnosis Mean age: 33.7 years Experimental Group/s: intervention n = 37; control n = 30 | EMDR | Waitlist control | IES-R (a self-report instrument which rates the severity of PTSD symptoms) (Weiss, 2007) [32] |
| 12. (Cohen, 2017) [42] | USA | Hurricane | Study design: Simulation model. N = 2,642,713 (Model population living in the areas of New York City affected by Hurricane Sandy). Typical age: 33.9% aged 18–34 years, 49.0% aged 35–64 years, and 17.1% aged <65 years) Experimental Group/s: n/a | Stepped care case-finding intervention (stepped care (SC)) | Usual care | The Child Post-Traumatic Stress Disorder Reaction Index (CPTSD-RI) (Frederick et al., 1992) [43] |
| 13. (Dawson, 2018) [44] | Indonesia | Civil conflict | Study design: Randomised control trial. N = 64. Children with post-traumatic stress disorder. Mean age: 10.7 years. (7–14 years) Experimental Group/s: intervention n = 32; comparison n = 32 | Trauma-focused cognitive behavior therapy | Problem-solving therapy provided by lay counselors who were provided with brief training | PTSD measured by the PTSD Child Reaction Index. (Frederick et al., 1992) [43] |
| 14. (Welton-Mitchell, 2018) [45] | Nepal | Earthquake | Study design: Quasi-experimental study. Cluster randomised design. N = 240. People in two earthquake-affected communities Mean age: 38 years. Experimental Group/s: intervention n = 120; control n = 120 | A hybrid mental health and disaster preparedness intervention | Waitlist control | A 7-item investigator developed checklist to measure self-reported disaster preparedness |
| 15. (James, 2020) [46] | Haiti | Earthquake; hurricanes, flooding, and landslides | Study design: Randomised control trial. N = 480. Community members, drawn from three disaster-affected communities Mean age: 37 years (18–78). Experimental Group/s: intervention n = 240; control n = 240 | Community-based mental health-integrated disaster preparedness intervention | Waitlist control | A 12-item Humanitarian Emergency Settings Perceived Needs (HESPER) developed by WHO and King’s College London (Semrau et al., 2012) [47] |
| 16. (Rahman, 2019) [38] | Pakistan | Armed conflict | Study design: Cluster randomised control trial. N = 612. Women in a post-conflict setting. Mean age: 36.32 years. Experimental Group/s: intervention n = 306; control n = 306 | Brief group psychological intervention | Enhanced usual care (EUC) | Hospital Anxiety and Depression Scale (HADS) (Zigmond and Snaith, 1983) [48] |
| 17. (Dhital, 2019) [49] | Nepal | Earthquake | Study design: Cluster randomised control trial. N = 1220. Students from 15 selected schools. Typical age: School-going adolescents from grades six to eight. Experimental Group/s: intervention n = 605; control n = 615 | Psycho-social support provided by trained teachers | No treatment | PTSD symptoms were measured using CPSS, a 17-item measure for children and adolescents (Foa et al., 2001) [50] |
| 18. (Kılıç and Şimşek, 2019) [51] | Turkey | Disaster | Study design: Randomised control trial. N = 76. Nursing students. Typical age: 81.6% 20–23 years; 18.4% 24 years and above. Experimental Group/s: intervention n = 38; control n = 38. | Psychological first-aid training | No treatment | Disaster preparedness perception scale (Özcan, 2013) [52] |
| 19. (Sijbrandij, 2020) [53] | Sierra Leone | Ebola and disasters | Study design: Cluster randomised control trial. N = 408. Primary health workers. Mean age: 39.5 years (intervention); 38.5 years (control). Experimental Group/s: intervention n = 202; waitlist control n = 206. | One-day face-to-face PFA group trainings | Waitlist control | Post-PFA assessment; professional attitude |
| 20. (Hamdani, 2020) [54] | Pakistan | Conflict and displacement | Study design: Randomised control trial. N = 346. Primary care attendees with high levels of psychological distress Typical age: n/a. Experimental Group/s: intervention n = 172; comparison n = 174 | Problem management | Enhanced TAU | Hospital Anxiety and Depression Scale (HADS) (Zigmond and Snaith,1983) [48] Incremental costs per unit change in anxiety, depression, and functioning scores. |
| 21. (Lotzin et al., 2021) [55] | Germany | Traumatic event: life threatening illness or injury, etc. | Study design: Randomised control trial. N = 30. Survivors. Mean age: 42 years (22–63 years). Experimental Group/s: intervention n = 15; waitlist control n = 15 | SOLAR, a 5-session psychosocial intervention | Waitlist control | The Client Satisfaction Questionnaire (CSQ-8) (CSQ-8; Larsen et al., 1979) [56] |
2.4. Risk of Bias and Quality of Evidence Assessment
2.5. Outcome Measures
2.6. Data Synthesis
3. Results
3.1. Study Characteristics
| Author | #1 (0–2) Randomisation | #2 (0–2) Masking (Blinding) | #3 (0–1) Withdrawals and Dropouts (Accountability of Participants) | Quality Score |
|---|---|---|---|---|
| Jacob et al. (2014) [37] | 2 | 2 | 1 | 5 |
| Bass et al. (2016) [40] | 2 | 2 | 1 | 5 |
| Acarturk et al. (2016) [11] | 2 | 2 | 1 | 5 |
| Basoglu et al. (2005) [14] | 2 | 2 | 0 | 4 |
| Jiang et al. (2014) [36] | 2 | 2 | 0 | 4 |
| Dawson et al. (2018) [44] | 2 | 2 | 0 | 4 |
| James et al. (2020) [46] | 2 | 2 | 0 | 4 |
| Steinmetz et al. (2012) [29] | 2 | 1 | 1 | 4 |
| Ruggiero et al. (2015) [38] | 2 | 2 | 0 | 4 |
| Rahman et al. (2019) [38] | 2 | 2 | 0 | 4 |
| Sijbrandij et al. (2019) [53] | 1 | 2 | 1 | 4 |
| Dhital et al. (2019) [49] | 2 | 1 | 1 | 4 |
| Kilic and Şimşek (2019) [51] | 2 | 1 | 1 | 4 |
| Hamdani et al. (2020) [54] | 2 | 1 | 1 | 4 |
| Lotzin et al. (2021) [55] | 2 | 1 | 1 | 4 |
| Zang et al. (2013) [31] | 2 | 1 | 1 | 4 |
| Zang et al. (2014) [35] | 2 | 1 | 1 | 4 |
| Author | #1 Selection | #2 Comparability | #3 Exposure/Outcome | Level of Quality |
|---|---|---|---|---|
| Welton-Mitchell et al. (2018) [45] | 3 | 2 | 3 | Good |
| Wolmer et al. (2005) [27] | 3 | 2 | 2 | Good |
| Wade et al. (2014) [72] | 3 | 2 | 2 | Good |
| McCabe et al. (2011) [73] | 3 | 2 | 2 | Good |
| Powell and Yuma-Guerrero (2016) [74] | 3 | 2 | 2 | Good |
| O’Donnell et al. (2020) [4] | 3 | 2 | 2 | Good |
| Adams et al. (2013) [34] | 2 | 2 | 3 | Good |
| Cohen et al. (2017) [42] | 4 | 2 | 2 | Good |
3.2. Characteristics of the Included Studies
3.3. Overall Findings of RCTs and Controlled Studies
3.3.1. Effectiveness of the Interventions
Psychotherapies
Psychoeducation or Trainings
3.3.2. Cost-Effectiveness of the Interventions
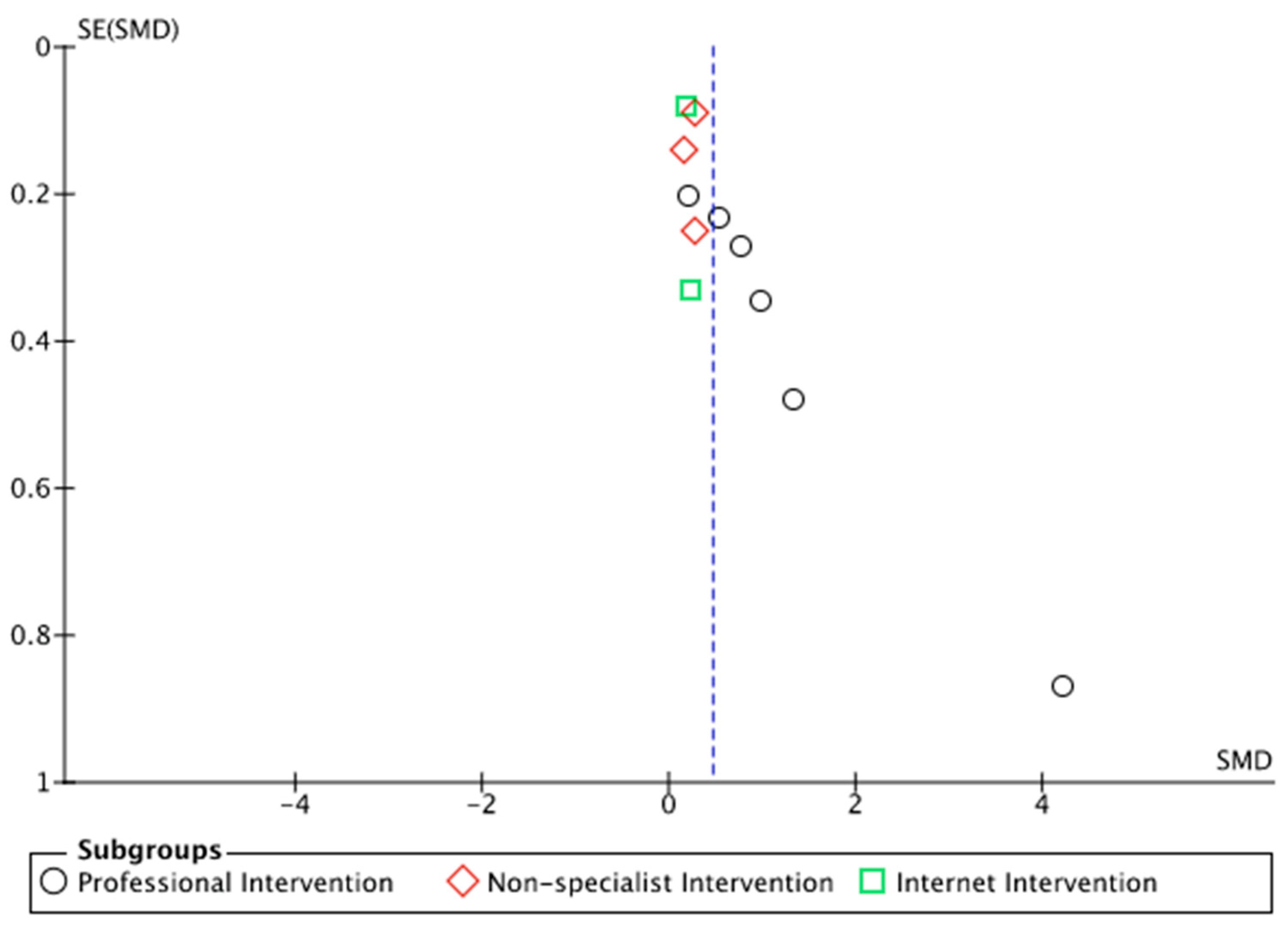
3.3.3. Meta-Analysis
Subgroup: Effect of Mental Health Intervention on PTSD-Related Symptoms
Comparison of Mental-Health-Professional-Delivered Mental Health Interventions versus Control Group
Comparison of Non-Specialists’ Mental Health Interventions versus PTSD Reduction without Mental Health Interventions
Comparison of PTSD-Related Symptoms with Web Mental Health Interventions versus PTSD-Related Symptoms without Mental Health Interventions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TSSC | Traumatic Stress Symptom Checklist |
| MPSS | Modified PTSD Symptoms Scale |
| MDR | My Disaster Recovery |
| IES-R | Impact of Event Scale-Revised |
| DSM-IV | Diagnostic and Statistical Manual of Mental Disorders, fourth edition |
| CAPS | Clinician-Administered PTSD Scale |
| BBN | Bounce Back Now |
| NSA | National Survey of Adolescents PTSD module |
| EMDR | Eye Movement Desensitization and Reprocessing |
| CBT | Cognitive Behavior Therapy |
| PS | Problem-solving |
| PTSD | Post-traumatic Stress Disorder |
| UCLA PTSD-RI | Los Angeles [UCLA] PTSD Reaction Index [RI] |
| CPTSD-RI | Child Post-Traumatic Stress Disorder Reaction Index |
| PCL-C | Post-traumatic Stress Disorder (PTSD) Checklist—Civilian Version |
References
- Wade, D.; Crompton, D.; Howard, A.; Stevens, N.; Metcalf, O.; Brymer, M.; Ruzek, J.; Watson, P.; Bryant, R.; Forbes, D. Skills for Psychological Recovery: Evaluation of a post-disaster mental health training program. Disaster Health 2014, 2, 138–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emergency Event Database. 2021. Available online: www.emdat.be (accessed on 1 April 2022).
- World Health Organization. Mental Health Atlas; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- O’Donnell, M.L.; Lau, W.; Fredrickson, J.; Gibson, K.; Bryant, R.A.; Bisson, J.; Burke, S.; Busuttil, W.; Coghlan, A.; Creamer, M.; et al. Child disaster mental health interventions: Therapy components. Prehosp. Disaster Med. 2014, 29, 494–502. [Google Scholar]
- Farooqui, M.; Quadri, S.A.; Suriya, S.S.; Khan, M.A.; Ovais, M.; Sohail, Z.; Shoaib, S.; Tohid, H.; Hassan, M. Posttraumatic stress disorder: A serious post-earthquake complication. Trends Psychiatry Psychother. 2017, 39, 135–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision (DSM-IV-TR®); American Psychiatric Association: Arlington, VA, USA, 2010. [Google Scholar]
- Math, S.B.; Nirmala, M.C.; Moirangthem, S.; Kumar, N.C. Disaster Management: Mental Health Perspective. Indian J. Psychol. Med. 2015, 37, 261–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charlson, F.; van Ommeren, M.; Flaxman, A.; Cornett, J.; Whiteford, H.; Saxena, S. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet 2019, 394, 240–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kane, J.C.; Ventevogel, P.; Spiegel, P.; Bass, J.K.; van Ommeren, M.; Tol, W.A. Mental, neurological, and substance use problems among refugees in primary health care: Analysis of the Health Information System in 90 refugee camps. BMC Med. 2014, 12, 228. [Google Scholar] [CrossRef] [PubMed]
- Goldmann, E.; Galea, S. Mental health consequences of disasters. Ann. Rev. Public Health 2014, 35, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Acarturk, C.; Konuk, E.; Cetinkaya, M.; Senay, I.; Sijbrandij, M.; Gulen, B.; Cuijpers, P. The efficacy of eye movement desensitization and reprocessing for post-traumatic stress disorder and depression among Syrian refugees: Results of a randomized controlled trial. Psychol. Med. 2016, 46, 2583–2593. [Google Scholar] [CrossRef] [PubMed]
- Castillo, E.G.; Ijadi-Maghsoodi, R.; Shadravan, S.; Moore, E.; Mensah, M.O.; Docherty, M.; Nunez, M.G.A.; Barcelo, N.; Goodsmith, N.; Halpin, L.E.; et al. Community Interventions to Promote Mental Health and Social Equity. Curr. Psychiatry Rep. 2019, 21, 35. [Google Scholar] [CrossRef] [Green Version]
- Chambers, M.; Kantaris, X. Enhancing the therapeutic interaction skills of staff working in acute adult inpatient psychiatric wards: Outcomes of a brief intervention education programme. J. Nurs. Educ. Pract. 2017, 7, 123–132. [Google Scholar] [CrossRef] [Green Version]
- Basoglu, M.; Şalcıoğlu, E.; Livanou, M.; Kalender, D.; Acar, G. Single-Session Behavioral Treatment of Earthquake-Related Posttraumatic Stress Disorder: A Randomized Waiting List Controlled Trial. J. Trauma. Stress 2005, 18, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Bouey, J. Public Mental Health Crisis during COVID-19 Pandemic, China. Emerg. Infect. Dis. 2020, 26, 1616–1618. [Google Scholar] [CrossRef]
- Lipinski, K.; Liu, L.L.; Wong, P.W. The effectiveness of psychosocial interventions implemented after the Indian Ocean Tsunami: A systematic review. Int. J. Soc. Psychiatry 2016, 62, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Lopes, A.P.; Macedo, T.F.; Coutinho, E.S.F.; Figueira, I.; Ventura, P.R. Systematic review of the efficacy of cognitive-behavior therapy related treatments for victims of natural disasters: A worldwide problem. PLoS ONE 2014, 9, e109013. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; Nitiéma, P.; Newman, E.; Patel, A. The Benefit of Interventions to Reduce Posttraumatic Stress in Youth Exposed to Mass Trauma: A Review and Meta-Analysis. Prehosp. Disaster Med. 2019, 34, 540–551. [Google Scholar] [CrossRef] [PubMed]
- Gillies, D.; Taylor, F.; Gray, C.; O’Brien, L.; D’Abrew, N. Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents (Review). Evid. Based Child Health 2013, 8, 1004–1116. [Google Scholar] [CrossRef] [PubMed]
- Kar, N. Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: A review. Neuropsychiatr. Dis. Treat 2011, 7, 167–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mendes, D.D.; Mello, M.; Ventura, P.; Passarela, C.D.M.; Mari, J.D.J. A systematic review on the effectiveness of cognitive behavioral therapy for posttraumatic stress disorder. Int. J. Psychiatry Med. 2008, 38, 241–259. [Google Scholar] [CrossRef]
- Natha, F.; Daiches, A. The effectiveness of EMDR in reducing psychological distress in survivors of natural disasters: A review. J. EMDR Pract. Res. 2014, 8, 157–170. [Google Scholar] [CrossRef]
- Coombe, J.; MacKenzie, L.; Munro, R.; Hazell, T.; Perkins, D.; Reddy, P. Teacher-Mediated Interventions to Support Child Mental Health Following a Disaster: A Systematic Review. PLoS Curr. 2015, 7. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4696867/ (accessed on 1 June 2021). [CrossRef]
- Winders, W.T.; Bustamante, N.D.; Garbern, S.C.; Bills, C.; Coker, A.; Trehan, I.; Osei-Ampofo, M.; Levine, A.C. Establishing the Effectiveness of Interventions Provided to First Responders to Prevent and/or Treat Mental Health Effects of Response to a Disaster: A Systematic Review. Disaster Med. Public Health Prep. 2021, 15, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Doherty, A.; Benedetto, V.; Harris, C.; Boland, P.; Christian, D.L.; Hill, J.; Bhutani, G.; Clegg, A.J. The effectiveness of psychological support interventions for those exposed to mass infectious disease outbreaks: A systematic review. BMC Psychiatry 2021, 21, 592. [Google Scholar] [CrossRef]
- Blake, D.D.; Weathers, F.W.; Nagy, L.M.; Kaloupek, D.G.; Gusman, F.D.; Charney, D.S.; Keane, T.M. The development of a clinician-administered PTSD scale. J. Trauma. Stress 1995, 8, 75–90. [Google Scholar] [CrossRef] [PubMed]
- Wolmer, L.; Laor, N.; Dedeoglu, C.; Siev, J.; Yazgan, Y. Teacher-mediated intervention after disaster: A controlled three-year follow-up of children’s functioning. J. Child Psychol. Psychiatry 2005, 46, 1161–1168. [Google Scholar] [CrossRef] [PubMed]
- Pynoos, R.S.; Frederick, C.; Nader, K.; Arroyo, W.; Steinberg, A.; Eth, S.; Nunez, F.; Fairbanks, L. Life threat and posttraumatic stress in school-age children. Arch. Gen. Psychiatry 1987, 44, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, S.E.; Benight, C.C.; Bishop, S.L.; James, L.E. My Disaster Recovery: A pilot randomized controlled trial of an Internet intervention. Anxiety Stress Coping 2012, 25, 593–600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brewin, C.R.; Rose, S.; Andrews, B.; Green, J.; Tata, P.; McEvedy, C.; Turner, S.; Foa, E.B. Brief screening instrument for post-traumatic stress disorder. Br. J. Psychiatry 2002, 181, 158–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zang, Y.; Hunt, N.; Cox, T. A randomised controlled pilot study: The effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC Psychiatry 2013, 13, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiss, D.S.; Marmar, C.R. Assessing Psychological Trauma and PTSD; Guilford Press: New York, NY, USA, 1997. [Google Scholar]
- Goldberg, D.P.; Hillier, V.F. A scaled version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef]
- Adams, R.E.; Laraque, D.; Chemtob, C.M.; Jensen, P.S.; Boscarino, J.A. Does a one-day educational training session influence primary care pediatricians’ mental health practice procedures in response to a community disaster? Results from the reaching children initiative (RCI). Int. J. Emerg. Ment. Health 2013, 15, 3–14. [Google Scholar]
- Zang, Y.; Hunt, N.; Cox, T. Adapting narrative exposure therapy for Chinese earthquake survivors: A pilot randomised controlled feasibility study. BMC Psychiatry 2014, 14, 262. [Google Scholar] [CrossRef] [PubMed]
- Jiang, R.F.; Tong, H.Q.; Delucchi, K.L.; Neylan, T.C.; Shi, Q.; Meffert, S.M. Interpersonal psychotherapy versus treatment as usual for PTSD and depression among Sichuan earthquake survivors: A randomized clinical trial. Confl. Health 2014, 8, 14. [Google Scholar] [CrossRef]
- Jacob, N.; Neuner, F.; Maedl, A.; Schaal, S.; Elbert, T. Dissemination of psychotherapy for trauma spectrum disorders in postconflict settings: A randomized controlled trial in Rwanda. Psychother. Psychosom. 2014, 83, 354–363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruggiero, K.J.; Price, M.; Adams, Z.; Stauffacher, K.; McCauley, J.; Danielson, C.K.; Knapp, R.; Hanson, R.F.; Davidson, T.M.; Amstadter, A.B.; et al. Web intervention for adolescents affected by disaster: Population-based randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 709–717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kilpatrick, D.G.; Ruggiero, K.J.; Acierno, R.; Saunders, B.E.; Resnick, H.S.; Best, C.L. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. J. Consult. Clin. Psychol. 2003, 71, 692. [Google Scholar] [CrossRef] [PubMed]
- Bass, J.; Murray, S.M.; Mohammed, T.A.; Bunn, M.; Gorman, W.; Ahmed, A.M.A.; Murray, L.; Bolton, P. A randomized controlled trial of a trauma-informed support, skills, and psychoeducation intervention for survivors of torture and related trauma in Kurdistan, Northern Iraq. Glob. Health Sci. Pract. 2016, 4, 452–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Cohen, G.H.; Tamrakar, S.; Lowe, S.; Sampson, L.; Ettman, C.; Linas, B.; Ruggiero, K.; Galea, S. Comparison of simulated treatment and cost-effectiveness of a stepped care case-finding intervention vs usual care for posttraumatic stress disorder after a natural disaster. JAMA Psychiatry 2017, 74, 1251–1258. [Google Scholar] [CrossRef] [PubMed]
- Frederick, C.J.; Pynoos, R.S.; Nader, K. Reaction Index to Psychic Trauma Form C (Child); Department of Psychiatry, University of California at Los Angeles: Los Angeles, CA, USA, 1992. [Google Scholar]
- Dawson, K.; Joscelyne, A.; Meijer, C.; Steel, Z.; Silove, D.; Bryant, R.A. A controlled trial of trauma-focused therapy versus problem-solving in Islamic children affected by civil conflict and disaster in Aceh, Indonesia. Aust. N. Z. J. Psychiatry 2018, 52, 253–261. [Google Scholar] [CrossRef]
- Welton-Mitchell, C.; James, L.E.; Khanal, S.N.; James, A.S. An integrated approach to mental health and disaster preparedness: A cluster comparison with earthquake affected communities in Nepal. BMC Psychiatry 2018, 18, 296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- James, L.E.; Welton-Mitchell, C.; Noel, J.R.; James, A.S. Integrating mental health and disaster preparedness in intervention: A randomized controlled trial with earthquake and flood-affected communities in Haiti. Psychol. Med. 2020, 50, 342–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Semrau, M.; van Ommeren, M.; Blagescu, M.; Griekspoor, A.; Howard, L.M.; Jordans, M.; Lempp, H.; Marini, A.; Pedersen, J.; Pilotte, I.; et al. The development and psychometric properties of the humanitarian emergency settings perceived needs (HESPER) scale. Am. J. Public Health 2012, 102, e55–e63. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Dhital, R.; Shibanuma, A.; Miyaguchi, M.; Kiriya, J.; Jimba, M. Effect of psycho-social support by teachers on improving mental health and hope of adolescents in an earthquake-affected district in Nepal: A cluster randomized controlled trial. PLoS ONE 2019, 14, e0223046. [Google Scholar] [CrossRef] [Green Version]
- Foa, E.B.; Johnson, K.M.; Feeny, N.C.; Treadwell, K.R. The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. J. Clin. Child Psychol. 2001, 30, 376–384. [Google Scholar] [CrossRef]
- Kılıç, N.; Şimşek, N. The effects of psychological first aid training on disaster preparedness perception and self-efficacy. Nurse Educ. Today 2019, 83, 104203. [Google Scholar] [CrossRef] [PubMed]
- Özcan, F. Hemşirelerin Afete Hazır Olma Durumu ve Hazırlık Algısı. Doctoral Dissertation, Marmara Universitesi, Istanbul, Turkey, 2013. [Google Scholar]
- Sijbrandij, M.; Horn, R.; Esliker, R.; O’may, F.; Reiffers, R.; Ruttenberg, L.; Stam, K.; de Jong, J.; Ager, A. The effect of psychological first aid training on knowledge and understanding about psychosocial support principles: A cluster-randomized controlled trial. Int. J. Environ. Res. Public Health 2020, 17, 484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamdani, S.U.; Rahman, A.; Wang, D.; Chen, T.; van Ommeren, M.; Chisholm, D.; Farooq, S. Cost-effectiveness of WHO Problem Management Plus for adults with mood and anxiety disorders in a post-conflict area of Pakistan: Randomised controlled trial. Br. J. Psychiatry 2020, 217, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Lotzin, A.; Hinrichsen, I.; Kenntemich, L.; Freyberg, R.C.; Lau, W.; O’Donnell, M. The SOLAR group program to promote recovery after disaster and trauma—A randomized controlled feasibility trial among German trauma survivors. Psychol. Trauma Theory Res. Pract. Policy 2022, 14, 161. [Google Scholar] [CrossRef] [PubMed]
- Larsen, D.L.; Attkisson, C.C.; Hargreaves, W.A.; Nguyen, T.D. Assessment of client/patient satisfaction: Development of a general scale. Eval. Program Plan. 1979, 2, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jeckinson, C.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Weiss, D.S. The impact of event scale: Revised. In Cross-Cultural Assessment of Psychological Trauma and PTSD; Springer: Boston, MA, USA, 2007; pp. 219–238. [Google Scholar]
- Islam, M.M.; Iqbal, U.; Walther, B.; Atique, S.; Dubey, N.K.; Nguyen, P.-A.; Poly, T.N.; Masud, J.H.B.; Li, Y.-C.; Shabbir, S.-A. Benzodiazepine use and risk of dementia in the elderly population: A systematic review and meta-analysis. Neuroepidemiology 2016, 47, 181–191. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Birleson, P. The validity of depressive disorder in childhood and the development of a self-rating scale: A research report. J. Child Psychol. Psychiatry 1981, 22, 73–88. [Google Scholar] [CrossRef] [PubMed]
- Gollwitzer, P.M.; Bargh, J.A. The Psychology of Action: Linking Cognition and Motivation to Behavior; Guilford Press: New York, NY, USA, 1996. [Google Scholar]
- Chesney, M.A.; Neilands, T.B.; Chambers, D.B.; Taylor, J.M.; Folkman, S. A validity and reliability study of the coping self-efficacy scale. Br. J. Health Psychol. 2006, 11 Pt 3, 421–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef] [Green Version]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- First, M.B.; Gibbon, M. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II); American Psychiatric Press: Washington, DC, USA, 2004. [Google Scholar]
- Lecrubier, Y.; Sheehan, D.V.; Weiller, E.; Amorim, P.; Bonora, I.; Sheehan, K.H.; Janavs, J.; Dunbar, G.C. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur. Psychiatry 1997, 12, 224–231. [Google Scholar] [CrossRef]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychol. Assess. 2016, 28, 1379. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Oxford Press: Oxford, UK, 2000. [Google Scholar]
- UNDRR. The Human Cost of Disasters: An Overview of the Last 20 Years (2000–2019); UN Office for Disaster Risk Reduction: Geneva, Switzerland, 2000. [Google Scholar]
- McCabe, O.L.; Perry, C.; Azur, M.; Taylor, H.G.; Bailey, M.; Links, J.M. Psychological first-aid training for paraprofessionals: A systems-based model for enhancing capacity of rural emergency responses. Prehosp. Disaster Med. 2011, 26, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Powell, T.; Yuma-Guerrero, P. Supporting community health workers after a disaster: Findings from a mixed-methods pilot evaluation study of a psychoeducational intervention. Dis. Med. Public Health Prep. 2016, 10, 754–761. [Google Scholar] [CrossRef] [PubMed]

| Author and Year of Study | Findings Reduced Depression | Reduced Anxiety | PTSD Symptoms | Self-Efficacy | Perceived Support | Other |
|---|---|---|---|---|---|---|
| Steinmetz et al. (2012) [29] | ++ | N/A | N/A | N/A | N/A | Worry ++ |
| Zang et al. (2013) [31] | ++ | ++ | ++ | N/A | N/A | |
| Zang et al. (2014) [31] | ++ | ++ | ++ | N/A | ++ | Post-traumatic growth ++ |
| Jacob et al. (2014) [37] | N/A | N/A | ++ | N/A | N/A | Functional impairment ++ |
| Bass et al. (2016) [40] | ++ | ++ | N/A | N/A | N/A | Dysfunction ++ |
| Acarturk et al. (2016) [11] | N/A | N/A | ++ | N/A | N/A | |
| Basoglu et al. (2005) [14] | ++ | N/A | ++ | N/A | N/A | Fear and avoidance ++ |
| Jiang et al. (2014) [36] | ++ | N/A | ++ | N/A | N/A | |
| Dawson et al. (2018) [44] | + | N/A | ++ | N/A | N/A | Anger ++ |
| James et al. (2019) [46] | ++ | ++ | ++ | N/A | N/A | Disaster preparedness ++ |
| Ruggiero et al. (2015) [38] | + | N/A | ++ | N/A | N/A | Alcohol use + |
| Rahman et al. (2019) [38] | ++ | ++ | N/A | N/A | N/A | |
| Sijbrandij et al. (2019) [53] | N/A | N/A | N/A | N/A | N/A | Knowledge ++ |
| Dhital et al. (2019) [49] | ++ | N/A | ++ | N/A | N/A | |
| Kilic and Şimşek (2019) [51] | N/A | N/A | N/A | ++ | N/A | Disaster preparedness ++ |
| Hamdani et al. (2020) [54] | ++ | ++ | N/A | N/A | N/A | Functional impairment ++ |
| Lotzin et al. (2021) [55] | ++ | ++ | N/A | N/A | N/A | Improved coping with the problem +; social support +; quality of life + |
| Study (Year) | Participants | Mean Age | Intervention | Comparisons | Follow-up (Months) | Outcome Measure |
|---|---|---|---|---|---|---|
| Başoğlu (2005) [14] | N = 59, 84.7% female; 16–65 years; Turkey earthquake survivors, TSSC score higher than 20, literate. | 36.3 | SSBT | Waitlist control | 24 | TSSC |
| Wolmer (2005) [27] | N = 287, 60.6% female; children aged 9–17 years; students in three schools located in the Turkey earthquake disaster area. | 11.5 | School reactivation program | No intervention | 36 | CPTSD-RI |
| Steinmetz (2011) [29] | N = 56, 85.7% female; Hurricane Ike survivors, had access to the Internet, and met distress criteria | 43.0 | MDR | Usual care | 1 | MPSS |
| Zang (2013) [31] | N = 22, 77.3% female; Adult earthquake survivors seeking assistance, and met the DSM-IV criteria of PTSD | 55.73 | NET | Waitlist control | 2 | IES-R |
| Jacob (2014) [37] | N = 76, 81.82% female children; Rwandan widow and orphan genocide survivors | Widow 47.55; Children 24.55 | NET | Waitlist control | 6 | CAPS |
| Jiang (2014) [36] | N = 49, 71.4% female; 18 years or older, able to attend weekly sessions, met criteria for PTSD with heavy exposure to earthquake | 29.8 | IPT | Usual care | 6 | CAPS |
| Zang (2014) [35] | N = 30, 93.3% female; earthquake survivor adults met the DSM-IV criteria of PTSD | 53.63 | NET | Waitlist control | 3 | IES-R |
| Ruggiero (2015) [38] | N = 987, 53.5% female; adolescents from communities affected by devastating tornadoes | 14.55 | BBN | No intervention | 12 | NSA |
| Acarturk (2016) [11] | N = 70, 74% female; adult refugees located in Kilis Refugee Camp at the Turkish–Syrian border with a PTSD diagnosis | 33.7 | EMDR | Waitlist control | 1 | IES-R |
| Dawson (2018) [44] | N = 64, 46.9% female; 7–14 years; children living in the region affected by Aceh’s civil conflict and satisfying criteria for probable PTSD | 10.7 | CBT | Problem-solving intervention | 3 | UCLA PTSD-RI |
| James (2019) [46] | N = 480, 49.8% female; 18–78 years; community members, drawn from three disaster-affected communities | 37 | Mental health integrated disaster preparedness | Waitlist control | 6 | Unstandardised regression coefficients |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peng, M.; Xiao, T.; Carter, B.; Chen, P.; Shearer, J. Effectiveness and Cost-Effectiveness of Mental Health Interventions Delivered by Frontline Health Care Workers in Emergency Health Services: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 15847. https://doi.org/10.3390/ijerph192315847
Peng M, Xiao T, Carter B, Chen P, Shearer J. Effectiveness and Cost-Effectiveness of Mental Health Interventions Delivered by Frontline Health Care Workers in Emergency Health Services: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(23):15847. https://doi.org/10.3390/ijerph192315847
Chicago/Turabian StylePeng, Min, Tao Xiao, Ben Carter, Pan Chen, and James Shearer. 2022. "Effectiveness and Cost-Effectiveness of Mental Health Interventions Delivered by Frontline Health Care Workers in Emergency Health Services: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 23: 15847. https://doi.org/10.3390/ijerph192315847
APA StylePeng, M., Xiao, T., Carter, B., Chen, P., & Shearer, J. (2022). Effectiveness and Cost-Effectiveness of Mental Health Interventions Delivered by Frontline Health Care Workers in Emergency Health Services: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(23), 15847. https://doi.org/10.3390/ijerph192315847








