Early Detection of Refractive Errors by Photorefraction at School Age
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Data Collection
2.3. Analysis
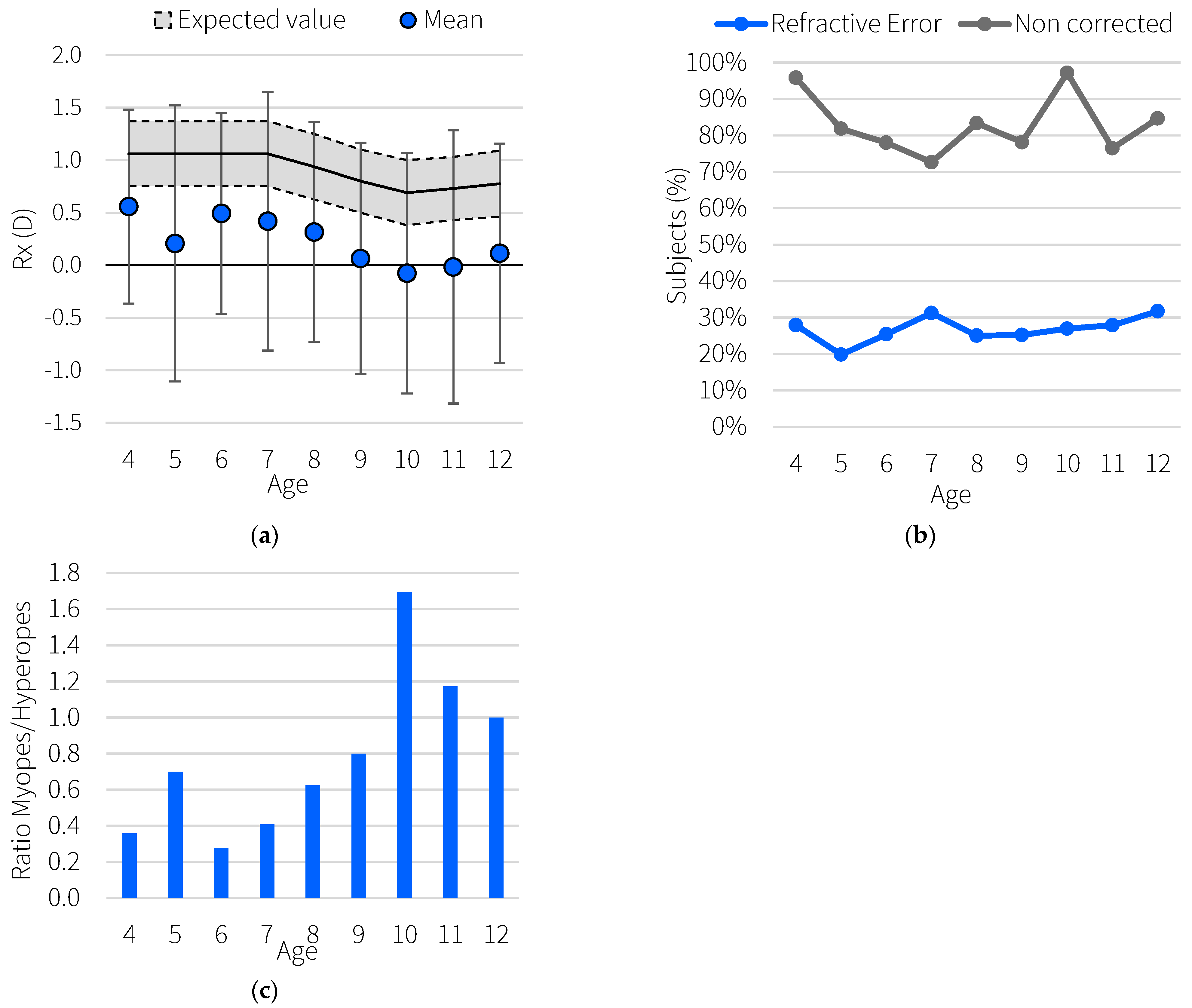
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Data on Visual Impairment 2010; World Health Organization: Geneva, Switzerland, 2010.
- Garzia, R.P.; Borsting, E.J.; Nicholson, S.B.; Press, L.J.; Scheiman, M.M.; Solan, H.A. Care of the Patient with Learning Related Vision Problems; Heath, D.A., Amos, J.F., Miller, S.C., Eds.; American Optometric Association: St. Louis, MO, USA, 2008. [Google Scholar]
- Morgan, I.G.; Ohno-Matsui, K.; Saw, S.-M. Myopia. Lancet 2012, 379, 1739–1748. [Google Scholar] [CrossRef] [PubMed]
- Asakuma, T.; Yasuda, M.; Ninomiya, T.; Noda, Y.; Arakawa, S.; Hashimoto, S.; Ohno-Matsui, K.; Kiyohara, Y.; Ishibashi, T. Prevalence and Risk Factors for Myopic Retinopathy in a Japanese Population: The Hisayama Study. Ophthalmology 2012, 119, 1760–1765. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Guo, Y.; Liao, C.; Chen, Y.; Su, G.; Zhang, G.; Zhang, L.; He, M. Incidence of and Factors Associated with Myopia and High Myopia in Chinese Children, Based on Refraction Without Cycloplegia. JAMA Ophthalmol. 2018, 136, 1017–1024. [Google Scholar] [CrossRef]
- Chua, S.Y.L.; Sabanayagam, C.; Cheung, Y.-B.; Chia, A.; Valenzuela, R.K.; Tan, D.; Wong, T.-Y.; Cheng, C.-Y.; Saw, S.-M. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol. Opt. 2016, 36, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Ding, X.; Guo, X.; Chen, Y.; Zhang, J.; He, M. Association of Age at Myopia Onset with Risk of High Myopia in Adulthood in a 12-Year Follow-up of a Chinese Cohort. JAMA Ophthalmol. 2020, 138, 1129. [Google Scholar] [CrossRef] [PubMed]
- Pai, A.S.-I.; Rose, K.A.; Leone, J.F.; Sharbini, S.; Burlutsky, G.; Varma, R.; Wong, T.Y.; Mitchell, P. Amblyopia Prevalence and Risk Factors in Australian Preschool Children. Ophthalmology 2012, 119, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Chia, A.; Dirani, M.; Chan, Y.-H.; Gazzard, G.; Eong, K.-G.A.; Selvaraj, P.; Ling, Y.; Quah, B.-L.; Young, T.L.; Mitchell, P.; et al. Prevalence of Amblyopia and Strabismus in Young Singaporean Chinese Children. Investig. Opthalmol. Vis. Sci. 2010, 51, 3411–3417. [Google Scholar] [CrossRef]
- Fogel-Levin, M.; Doron, R.; Wygnanski-Jaffe, T.; Ancri, O.; Ben Zion, I. A comparison of plusoptiX A12 measurements with cycloplegic refraction. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2016, 20, 310–314. [Google Scholar] [CrossRef]
- Braverman, R. Diagnosis and treatment of refractive errors in the pediatric population. Curr. Opin. Ophthalmol. 2007, 18, 379–383. [Google Scholar] [CrossRef] [PubMed]
- Rajavi, Z.; Parsafar, H.; Ramezani, A.; Yaseri, M. Is noncycloplegic photorefraction applicable for screening refractive amblyopia risk factors? J. Ophthalmic Vis. Res. 2012, 7, 3–9. [Google Scholar]
- Schaeffel, F.; Brüggemann, G. Noncycloplegic Photorefractive Screening in Pre-School Children with the “PowerRefractor” in a Pediatric Practice. Optom. Vis. Sci. 2007, 84, 630–639. [Google Scholar] [CrossRef] [PubMed]
- Paff, T.; Oudesluys-Murphy, A.M.; Wolterbeek, R.; Berg, M.S.-V.D.; de Nie, J.M.; Tijssen, E.; Schalij-Delfos, N.E. Screening for refractive errors in children: The plusoptiX S08 and the Retinomax K-plus2 performed by a lay screener compared to cycloplegic retinoscopy. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2010, 14, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Weiss, S.; Schaeffel, F.; Seidemann, A.; Howland, H.C.; Wilhelm, B.; Wilhelm, H. Laboratory, Clinical, and Kindergarten Test of a New Eccentric Infrared Photorefractor (PowerRefractor). Optom. Vis. Sci. 2000, 77, 537–548. [Google Scholar] [CrossRef]
- Matta, N.S.; Singman, E.L.; Silbert, D.I. Performance of the Plusoptix vision screener for the detection of amblyopia risk factors in children. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2008, 12, 490–492. [Google Scholar] [CrossRef]
- Howland, H.C.; Howland, B. Photorefraction: A technique for study of refractive state at a distance. J. Opt. Soc. Am. 1974, 64, 240–249. [Google Scholar] [CrossRef]
- Sabbaghi, H.; Rajavi, Z.; Baghini, A.S.; Yaseri, M.; Sheibani, K.; Norouzi, G. Accuracy and repeatability of refractive error measurements by photorefractometry. J. Ophthalmic Vis. Res. 2015, 10, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Kaakinen, K.A.; Kaseva, H.O.; Teir, H.H. Two-flash Photorefraction in Screening of Amblyogenic Refractive Errors. Ophthalmology 1987, 94, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Ayse, Y.K.; Onder, U.; Suheyla, K. Accuracy of Plusoptix SO4 in children and teens. Can. J. Ophthalmol. 2011, 46, 153–157. [Google Scholar] [CrossRef]
- Working Principle of a Transillumination Test. 2019. Available online: https://www.plusoptix.com/fileadmin/Downloads/Anleitungen_manuals/Fact_Sheets/Transillumination/Plusoptix_FactSheet_201904_Working_principle_of_a_transillumination_test.pdf (accessed on 6 May 2022).
- Dahlmann-Noor, A.; Comyn, O.; Kostakis, V.; Misra, A.; Gupta, N.; Heath, J.; Brown, J.; Iron, A.; McGill, S.; Vrotsou, K.; et al. Plusoptix Vision Screener: The accuracy and repeatability of refractive measurements using a new autorefractor. Br. J. Ophthalmol. 2009, 93, 346–349. [Google Scholar] [CrossRef]
- Farbrother, J.E. Spectacle prescribing in childhood: A survey of hospital optometrists. Br. J. Ophthalmol. 2008, 92, 392–395. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McCullough, S.; Adamson, G.; Breslin, K.M.M.; McClelland, J.F.; Doyle, L.; Saunders, K.J. Axial growth and refractive change in white European children and young adults: Predictive factors for myopia. Sci. Rep. 2020, 10, 15189. [Google Scholar] [CrossRef]
- Arnold, R.W. Amblyopia Risk Factor Prevalence. J. Pediatr. Ophthalmol. Strabismus 2013, 50, 213–217. [Google Scholar] [CrossRef]
- Donahue, S.P.; Arthur, B.; Neely, D.E.; Arnold, R.W.; Silbert, D.; Ruben, J.B. Guidelines for automated preschool vision screening: A 10-year, evidence-based update. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2013, 17, 4–8. [Google Scholar] [CrossRef] [PubMed]
- Schimitzek, T.; Lagrèze, W.A. Accuracy of a new photorefractometer in young and adult patients. Graefes Arch. Clin. Exp. Ophthalmol. 2005, 243, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Castagno, V.D.; Fassa, A.G.; Vilela, M.; Meucci, R.D.; Resende, D.P.M. Moderate hyperopia prevalence and associated factors among elementary school students. Cienc. Saude Coletiva 2015, 20, 1449–1458. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef]
- Luong, T.Q.; Shu, Y.-H.; Modjtahedi, B.S.; Fong, D.S.; Choudry, N.; Tanaka, Y.; Nau, C.L. Racial and Ethnic Differences in Myopia Progression in a Large, Diverse Cohort of Pediatric Patients. Investig. Opthalmol. Vis. Sci. 2020, 61, 20. [Google Scholar] [CrossRef]
- Pan, C.-W.; Klein, B.E.; Cotch, M.F.; Shrager, S.; Klein, R.; Folsom, A.; Kronmal, R.; Shea, S.J.; Burke, G.L.; Saw, S.-M.; et al. Racial Variations in the Prevalence of Refractive Errors in the United States: The Multi-Ethnic Study of Atherosclerosis. Am. J. Ophthalmol. 2013, 155, 1129–1138.e1. [Google Scholar] [CrossRef]
- Robinson, B.E. Factors Associated with the Prevalence of Myopia in 6-Year-Olds. Optom. Vis. Sci. 1999, 76, 266–271. [Google Scholar] [CrossRef]
- Jobke, S.; Kasten, E.; Vorwerk, C. The prevalence rates of refractive errors among children, adolescents, and adults in Germany. Clin. Ophthalmol. 2008, 2, 601–607. [Google Scholar] [CrossRef]
- Cummings, G. Vision screening in junior schools. Public Health 1996, 110, 369–372. [Google Scholar] [CrossRef]

| Refractive Error | Criteria | |||||||
|---|---|---|---|---|---|---|---|---|
| Myopia | <−1.0 D [23] High myopia according to Hu et al. [7] | |||||||
| Age (years) | <9 | 9 | 10 | 11 | 12 | 13 | ||
| Myopia (D) | −1 | −2 | −2.75 | −3.5 | −4 | −4.5 | ||
| Future potential myopes: sphere smaller than the minimum expected for their age [24] | ||||||||
| Age (years) | <8 | 8 | 9 | 10 | 11 | 12 | 13 | |
| Min (D) | 0.75 | 0.625 | 0.5 | 0.38 | 0.43 | 0.46 | 0.5 | |
| Hyperopia | Greater than expected spherical equivalent for age [24] | |||||||
| Age (years) | <8 | 8 | 9 | 10 | 11 | 12 | 13 | |
| Min (D) | 1.37 | 1.25 | 1.1 | 1 | 1.03 | 1.09 | 1.12 | |
| Astigmatism | Cylinder > 1.5 D | |||||||
| Amblyopia Risk | Risk factors according to American Association for Pediatric Ophthalmology and Strabismus (AAOPS) [25]: Anisometropia > 1.5 D Hyperopia > 3.5 D Myopia < −3.0 D Astigmatism > 1.5 D @ 90 ± 10° or @ 180 ± 10° Oblique astigmatism > 1.0 D | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alvarez, M.; Benedi-Garcia, C.; Concepcion-Grande, P.; Dotor, P.; Gonzalez, A.; Chamorro, E.; Cleva, J.M. Early Detection of Refractive Errors by Photorefraction at School Age. Int. J. Environ. Res. Public Health 2022, 19, 15880. https://doi.org/10.3390/ijerph192315880
Alvarez M, Benedi-Garcia C, Concepcion-Grande P, Dotor P, Gonzalez A, Chamorro E, Cleva JM. Early Detection of Refractive Errors by Photorefraction at School Age. International Journal of Environmental Research and Public Health. 2022; 19(23):15880. https://doi.org/10.3390/ijerph192315880
Chicago/Turabian StyleAlvarez, Marta, Clara Benedi-Garcia, Pablo Concepcion-Grande, Paulina Dotor, Amelia Gonzalez, Eva Chamorro, and Jose Miguel Cleva. 2022. "Early Detection of Refractive Errors by Photorefraction at School Age" International Journal of Environmental Research and Public Health 19, no. 23: 15880. https://doi.org/10.3390/ijerph192315880
APA StyleAlvarez, M., Benedi-Garcia, C., Concepcion-Grande, P., Dotor, P., Gonzalez, A., Chamorro, E., & Cleva, J. M. (2022). Early Detection of Refractive Errors by Photorefraction at School Age. International Journal of Environmental Research and Public Health, 19(23), 15880. https://doi.org/10.3390/ijerph192315880







