Facilitators and Barriers of Artificial Intelligence Applications in Rehabilitation: A Mixed-Method Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials
2.2.1. Validation of the Questionnaire
2.2.2. Questionnaire Form
- -
- In your opinion, which patients would benefit more from AI applications and why (musculoskeletal, geriatrics, neurologically impaired, etc.)? Please explain your response.
- -
- In your opinion, what are the major challenges or barriers that may limit AI applications?
2.3. Study Design
2.4. Procedure
2.5. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Factors Associated with AI Knowledge
3.2.1. Simple Binary Logistic Regression
3.2.2. Multivariate Logistic Regression Model
3.3. Factors Associated with AI Advantages
3.3.1. Reduce Professional Workload
3.3.2. Ease of Care
3.3.3. Diseases Prevention
3.4. Factors Associated with AI Uses
3.4.1. Predicting Diseases
3.4.2. Goal Setting
3.4.3. Assistive Technologies
3.4.4. Diagnostic Tool
3.5. Factors Associated with AI Impacts
3.5.1. Reducing Human Resource
3.5.2. Increase Productivity
3.5.3. Improve Patient Quality of Life
3.6. Qualitative Data Analysis
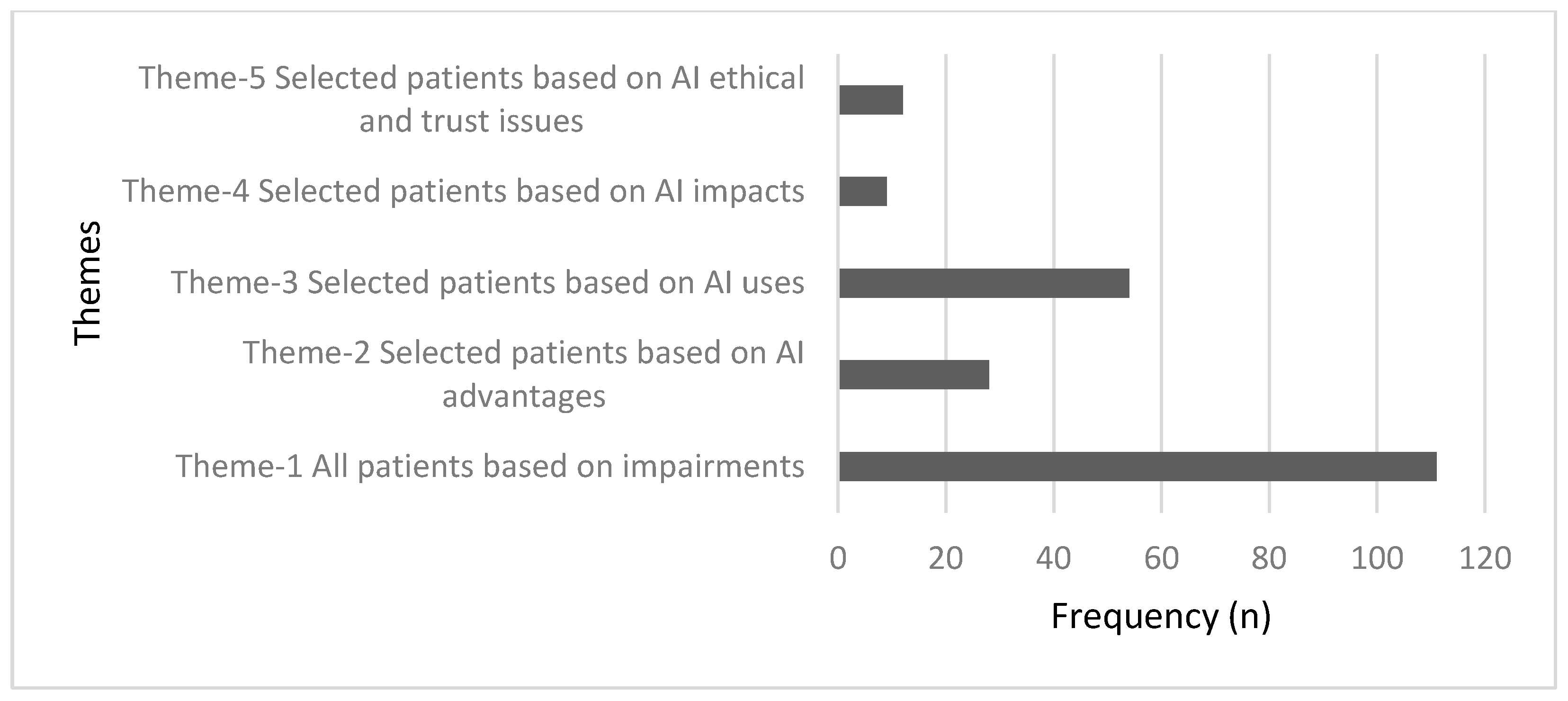
3.6.1. The First Qualitative Question Analysis
- Theme 1. All patients based on the impairments.
“Geriatric, neurologically impaired because it can assist these kinds of cases in their daily activities and predict their response.”—Participant 163.
“Musculoskeletal, as it will be easier for the patient to understand and apply.”—Participant 179.
- Theme 2. Selected patients based on AI advantages.
“I think musculoskeletal and neuro patients would benefit more from AI compared to other areas because, by the application of AI, rehabilitation can be performed more precisely and accurately with a constant rhythm throughout the session when compared to manual techniques.”—Participant 126.
“Geriatrics and neurological impaired because they will be guided by AI to do things correctly even in the absence of a Physiotherapist.”—Participant 14.
- Theme 3. Selected patients based on AI uses.
“Neurological impairments as most therapies targeting neurological disorders are feedback based… so the more accurate feedback the more accurate outcome.”—Participant 30.
“Definitely it will support clinicians’ effort to treat a neurologically impaired patient like visual or audible feedback is necessary to retrain the least amount of response from the patient.”—Participant 192.
- Theme 4. Selected patients based on AI impacts.
“Mostly all of the above mentioned will be benefited as would help them to work more efficiently, effectively and consistent way.”—Participant 189.
“It can help to those staying in remote areas where availability of medical facilities is less. As well it can help even a Physiotherapist to track record and keep data for analysis of progress.”
- Theme 5. Selected patients based on AI ethical and trust issues.
“As I haven’t experienced the applications of AI in all sectors, I am not sure. Still, I think musculoskeletal patients may be benefitted as in Neurological cases are more complicated the judgement of therapist matters more.”—Participant 96.
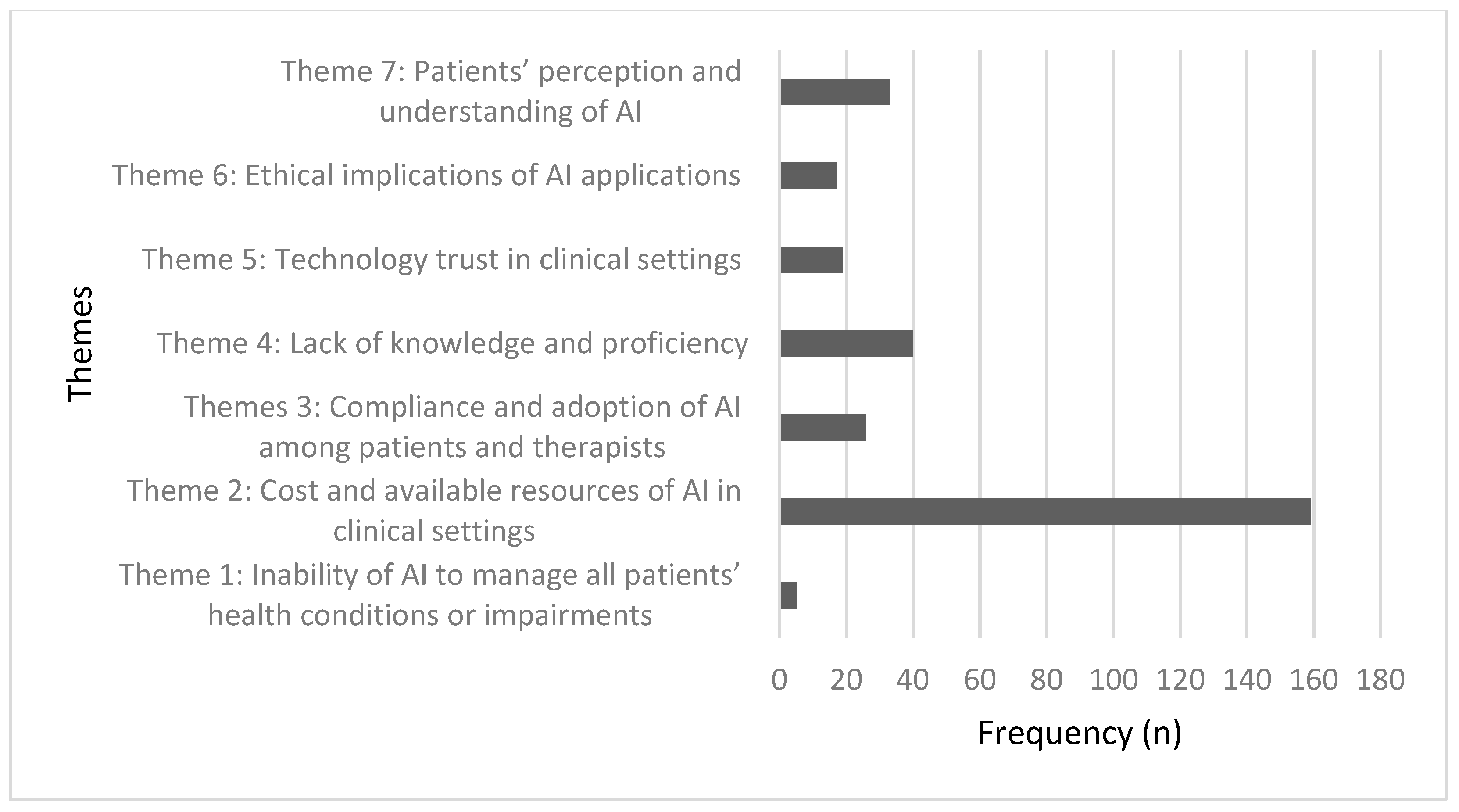
3.6.2. The Second Qualitative Question Analysis
- Theme 1. Inability of AI to manage all patients’ health conditions or impairments.
- Theme 2. Cost and available resources of AI in clinical settings.
- Theme 3. Compliance and adoption of AI among patients and therapists.
- Theme 4. Lack of knowledge and proficiency.
“Cost will obviously go towards higher side. And other limitation will be from developer side as they need to have the knowledge about medical profession, so in turn they will require to couple up with the medical professionals as whole team and need to careful design the script for its successful functionality and will need to set a perfect paradigm for its use.”—Participant 54.
- Theme 5. Technology trust in clinical settings.
- Theme 6. Ethical implications of AI applications.
- Theme 7. Patients’ perception and understanding of AI.
4. Discussion
Study Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Questions of the Survey Questionnaire with the Option Types
| Questionnaire Questions | Option Types |
|---|---|
| 1-What is your age? | Short answer (numerical) |
| 2-What is your gender? | Multiple choice |
| 3-Are you a physical therapy professional? | Multiple choice |
| 4-In which country do you work? | Multiple choice |
| 5-What is your employment sector? | Multiple choice |
| 6-What is your subspecialty? | Multiple choice |
| 7-How many years of experience do you have in the Physical Therapy field? | Multiple choice |
| 8-What is your highest educational qualification? | Multiple choice |
| Knowledge | |
| 9-Have you ever heard about Artificial Intelligence (AI)? | Multiple choice |
| 10-Have you ever heard about any AI technologies used in healthcare? | Multiple choice |
| 11-Have you ever heard about any AI technologies used in rehabilitation? | Multiple choice |
| 12-If you have prior information about AI, can you specify from where you have received it? Select all that apply. | Multiple choice |
| 13-If you came across any AI applications at work, how many were they? | Multiple choice |
| Advantages | |
| 14-The following questions are asking about your opinion regarding the ADVANTAGES of Artificial Intelligence (AI) in rehabilitation: | 5-point Likert scale |
| |
| Uses | |
| 15-Please indicate your level of agreement or disagreement regarding each of the following USES of AI in rehabilitation: | 5-point Likert scale |
| |
| Impact | |
| 16-The following questions are asking about your opinion regarding the IMPACTS of Artificial Intelligence (AI) on the FUTURE of rehabilitation: | 5-point Likert scale |
| |
| 17-Which of the following would be your primary concern regarding the implementation of AI in healthcare? | |
| 18-If Clinician’s judgment and AI’s judgment clashed, which opinion should be trusted? | |
| 19-Do you think AI applications should be taught in rehabilitation curriculums? | Multiple choice |
| 20-In your opinion, which patients would benefit more from AI applications and why? (musculoskeletal, geriatrics, neurologically impaired etc.) Please explain your response | Open-ended |
| 21-In your opinion, what are the major challenges or barriers that may limit AI application in rehabilitation and why? (cost, patient’s perceptions etc.) Please explain your response | Open-ended |
| 22-Would you be willing to receive more information on AI? | Multiple choice |
References
- Buldt, A.K.; Murley, G.S.; Butterworth, P.; Levinger, P.; Menz, H.B.; Landorf, K.B. The relationship between foot posture and lower limb kinematics during walking: A systematic review. Gait Posture 2013, 38, 363–372. [Google Scholar] [CrossRef]
- Gait Deviations of Patients with Ruptured Anterior Cruciate Ligament: A Cross-Sectional Gait Analysis Study on Male Patients|Knee Surgery & Related Research|Full Text. Available online: https://kneesurgrelatres.biomedcentral.com/articles/10.1186/s43019-021-00128-w (accessed on 19 September 2022).
- Lee, M.H.; Siewiorek, D.P.; Smailagic, A.; Bernardino, A. Opportunities of a Machine Learning-based Decision Support System for Stroke Rehabilitation Assessment. arXiv 2020, arXiv:2002.12261. Available online: http://arxiv.org/abs/2002.12261 (accessed on 13 May 2022).
- Wu, H.; Chan, N.-K.; Zhang, C.J.P.; Ming, W.-K. The Role of the Sharing Economy and Artificial Intelligence in Health Care: Opportunities and Challenges. J. Med. Internet Res. 2019, 21, e13469. [Google Scholar] [CrossRef]
- Tack, C. Artificial intelligence and machine learning | applications in musculoskeletal physiotherapy. Musculoskelet. Sci. Pract. 2018, 39, 164–169. [Google Scholar] [CrossRef]
- Romero-Brufau, S.; Wyatt, K.D.; Boyum, P.; Mickelson, M.; Moore, M.; Cognetta-Rieke, C. A lesson in implementation: A pre-post study of providers’ experience with artificial intelligence-based clinical decision support. Int. J. Med. Inform. 2019, 137, 104072. [Google Scholar] [CrossRef]
- Deep learning|Nature. Available online: https://www.nature.com/articles/nature14539 (accessed on 19 September 2022).
- Ravali, R.S.; Vijayakumar, T.M.; Lakshmi, K.S.; Mavaluru, D.; Reddy, L.V.; Retnadhas, M.; Thomas, T. A systematic review of artificial intelligence for pediatric physiotherapy practice: Past, present, and future. Neurosci. Inform. 2022, 2, 100045. [Google Scholar] [CrossRef]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef] [Green Version]
- Scheetz, J.; Rothschild, P.; McGuinness, M.; Hadoux, X.; Soyer, H.P.; Janda, M.; Condon, J.J.; Oakden-Rayner, L.; Palmer, L.J.; Keel, S.; et al. A survey of clinicians on the use of artificial intelligence in ophthalmology, dermatology, radiology and radiation oncology. Sci. Rep. 2021, 11, 5193. [Google Scholar] [CrossRef]
- Abdullah, R.; Fakieh, B. Health Care Employees’ Perceptions of the Use of Artificial Intelligence Applications: Survey Study. J. Med. Internet Res. 2020, 22, e17620. [Google Scholar] [CrossRef]
- Castagno, S.; Khalifa, M. Perceptions of Artificial Intelligence Among Healthcare Staff: A Qualitative Survey Study. Front. Artif. Intell. 2020, 3, 578983. [Google Scholar] [CrossRef]
- Laï, M.-C.; Brian, M.; Mamzer, M.-F. Perceptions of artificial intelligence in healthcare: Findings from a qualitative survey study among actors in France. J. Transl. Med. 2020, 18, 14. [Google Scholar] [CrossRef] [PubMed]
- De Simone, B.; Abu-Zidan, F.M.; Gumbs, A.A.; Chouillard, E.; Di Saverio, S.; Sartelli, M.; Coccolini, F.; Ansaloni, L.; Collins, T.; Kluger, Y.; et al. Knowledge, attitude, and practice of artificial intelligence in emergency and trauma surgery, the ARIES project: An international web-based survey. World J. Emerg. Surg. 2022, 17, 10. [Google Scholar] [CrossRef]
- Al-Khaled, T.; Valikodath, N.; Cole, E.; Hallak, J.; Campbell, J.P.; Chiang, M.F.; Chan, R.V.P. Evaluation of physician perspectives of artificial intelligence in ophthalmology: A pilot study. Investig. Ophthalmol. Vis. Sci. 2020, 61, 2023. [Google Scholar]
- Reddy, S.; Allan, S.; Coghlan, S.; Cooper, P. A governance model for the application of AI in health care. J. Am. Med. Inform. Assoc. 2019, 27, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Tizhoosh, H.R.; Pantanowitz, L. Artificial Intelligence and Digital Pathology: Challenges and Opportunities. J. Pathol. Inform. 2018, 9, 38. [Google Scholar] [CrossRef] [PubMed]
- Beregi, J.-P.; Zins, M.; Masson, J.-P.; Cart, P.; Bartoli, J.-M.; Silberman, B.; Boudghene, F.; Meder, J.-F. Radiology and artificial intelligence: An opportunity for our specialty. Diagn. Interv. Imaging 2018, 99, 677–678. [Google Scholar] [CrossRef] [PubMed]
- Haenssle, H.A.; Fink, C.; Schneiderbauer, R.; Toberer, F.; Buhl, T.; Blum, A.; Kalloo, A.; Hassen, A.B.H.; Thomas, L.; Enk, A.; et al. Man against machine: Diagnostic performance of a deep learning convolutional neural network for dermoscopic melanoma recognition in comparison to 58 dermatologists. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2018, 29, 1836–1842. [Google Scholar] [CrossRef] [PubMed]
- Houssami, N.; Turner, R.M.; Morrow, M. Meta-analysis of pre-operative magnetic resonance imaging (MRI) and surgical treatment for breast cancer. Breast Cancer Res. Treat. 2017, 165, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, Y.K.; Hughes, L.; Ismagilova, E.; Aarts, G.; Coombs, C.; Crick, T.; Duan, Y.; Dwivedi, R.; Edwards, J.; Eirug, A.; et al. Artificial Intelligence (AI): Multidisciplinary perspectives on emerging challenges, opportunities, and agenda for research, practice and policy. Int. J. Inf. Manag. 2019, 57, 101994. [Google Scholar] [CrossRef]
- Anderson, D. Artificial Intelligence and Applications in PM&R. Am. J. Phys. Med. Rehabil. 2019, 98, e128–e129. [Google Scholar]
- Wei, W.; McElroy, C.; Dey, S. Towards On-Demand Virtual Physical Therapist: Machine Learning-Based Patient Action Understanding, Assessment and Task Recommendation. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 1824–1835. [Google Scholar] [CrossRef] [PubMed]
- Lo, W.L.A.; Lei, D.; Li, L.; Huang, D.F.; Tong, K.-F. The Perceived Benefits of an Artificial Intelligence–Embedded Mobile App Implementing Evidence-Based Guidelines for the Self-Management of Chronic Neck and Back Pain: Observational Study. JMIR Mhealth Uhealth 2018, 6, e198. [Google Scholar] [CrossRef] [PubMed]
- Burns, D.M.; Leung, N.E.; Hardisty, M.; Whyne, C.M.; Henry, P.; McLachlin, S. Shoulder physiotherapy exercise recognition: Machine learning the inertial signals from a smartwatch. Physiol. Meas. 2018, 39, 075007. [Google Scholar] [CrossRef] [PubMed]
- Correia, F.D.; Nogueira, A.; Magalhães, I.; Guimarães, J.; Moreira, M.; Barradas, I.; Molinos, M.; Teixeira, L.; Tulha, J.; Seabra, R.; et al. Medium-Term Outcomes of Digital Versus Conventional Home-Based Rehabilitation After Total Knee Arthroplasty: Prospective, Parallel-Group Feasibility Study. JMIR Rehabil. Assist. Technol. 2019, 6, e13111. Available online: https://pubmed.ncbi.nlm.nih.gov/30816849/ (accessed on 23 November 2022). [CrossRef] [PubMed]
- Helm, J.M.; Swiergosz, A.M.; Haeberle, H.S.; Karnuta, J.M.; Schaffer, J.L.; Krebs, V.E.; Spitzer, A.I.; Ramkumar, P.N. Machine Learning and Artificial Intelligence: Definitions, Applications, and Future Directions. Curr. Rev. Musculoskelet. Med. 2020, 13, 69–76. [Google Scholar] [CrossRef]
- Kiger, M.E.; Varpio, L. Thematic analysis of qualitative data: AMEE Guide No. 131. Med. Teach. 2020, 42, 846–854. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Creswell, J.W.; Clark, V.L.P. Designing and Conducting Mixed Methods Research; SAGE: Thousand Oaks, CA, USA, 2011; 489p. [Google Scholar]
- O’Connor, C.; Joffe, H. Intercoder Reliability in Qualitative Research: Debates and Practical Guidelines. Int. J. Qual. Methods 2020, 19, 1609406919899220. [Google Scholar] [CrossRef]
- Bohr, A.; Memarzadeh, K. The rise of artificial intelligence in healthcare applications. In Artificial Intelligence in Healthcare; Academic Press: Cambridge, MA, USA, 2020; pp. 25–60. [Google Scholar] [CrossRef]
- Lambercy, O.; Lehner, R.; Chua, K.; Wee, S.K.; Rajeswaran, D.K.; Kuah, C.W.K.; Ang, W.T.; Liang, P.; Campolo, D.; Hussain, A.; et al. Neurorehabilitation From a Distance: Can Intelligent Technology Support Decentralized Access to Quality Therapy? Front. Robot. AI 2021, 8, 612415. [Google Scholar] [CrossRef]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Futur. Health J. 2019, 6, 94–98. [Google Scholar] [CrossRef] [Green Version]
- Ye, C.; Li, J.; Hao, S.; Liu, M.; Jin, H.; Zheng, L.; Xia, M.; Jin, B.; Zhu, C.; Alfreds, S.T.; et al. Identification of elders at higher risk for fall with statewide electronic health records and a machine learning algorithm. Int. J. Med. Inform. 2020, 137, 104105. [Google Scholar] [CrossRef] [PubMed]
- Popenici, S.A.D.; Kerr, S. Exploring the impact of artificial intelligence on teaching and learning in higher education. Res. Pract. Technol. Enhanc. Learn. 2017, 12, 22. [Google Scholar] [CrossRef] [PubMed]
- Phan, G.H.; Solanki, V.K.; Quang, N.H. Artificial Intelligence in Rehabilitation Evaluation-Based Robotic Exoskeletons: A Review. In Bio-Inspired Motor Control Strategies for Redundant and Flexible Manipulator with Application to Tooling Tasks; Springer: Singapore, 2022; pp. 79–91. [Google Scholar] [CrossRef]
- Victor Mugabe, K. Barriers and facilitators to the adoption of artificial intelligence in radiation oncology: A New Zealand study. Tech. Innov. Patient Support Radiat. Oncol. 2021, 18, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, A.; Bester, M.; Bolton, L. Employees’ Perceptions of the Implementation of Robotics, Artificial Intelligence, and Automation (RAIA) on Job Satisfaction, Job Security, and Employability. J. Technol. Behave. Sci. 2021, 6, 106–113. [Google Scholar] [CrossRef]
- Rowe, M.; Nicholls, D.A.; Shaw, J. How to replace a physiotherapist: Artificial intelligence and the redistribution of expertise. Physiother. Theory Pract. 2021, 38, 2275–2283. [Google Scholar] [CrossRef]
- Sun, T.Q.; Medaglia, R. Mapping the challenges of Artificial Intelligence in the public sector: Evidence from public healthcare. Gov. Inf. Q. 2018, 36, 368–383. [Google Scholar] [CrossRef]
- Wang, C.; Zhu, X.; Hong, J.C.; Zheng, D. Artificial Intelligence in Radiotherapy Treatment Planning: Present and Future. Technol. Cancer Res. Treat. 2019, 18, 1533033819873922. [Google Scholar] [CrossRef]
- Pinto Dos Santos, D.; Giese, D.; Brodehl, S.; Chon, S.H.; Staab, W.; Kleinert, R.; Maintz, D.; Baeßler, B. Medical students’ attitude towards artificial intelligence: A multicentre survey. Eur. Radiol. 2019, 29, 1640–1646. [Google Scholar] [CrossRef]
- Alsobhi, M.; Khan, F.; Chevidikunnan, M.; Basuodan, R.; Shawli, L.; Neamatallah, Z. Physical Therapists’ Knowledge and Attitudes Regarding Artificial Intelligence Applications in Health Care and Rehabilitation: Cross-sectional Study. J. Med. Internet Res. 2022, 24, e39565. [Google Scholar] [CrossRef]
- Yang, Y.; Yuan, Y.; Zhang, G.; Wang, H.; Chen, Y.-C.; Liu, Y.; Tarolli, C.G.; Crepeau, D.; Bukartyk, J.; Junna, M.R.; et al. Artificial intelligence-enabled detection and assessment of Parkinson’s disease using nocturnal breathing signals. Nat. Med. 2022, 28, 2207–2215. [Google Scholar] [CrossRef]
- Vayena, E.; Blasimme, A.; Cohen, I.G. Machine learning in medicine: Addressing ethical challenges. PLoS Med. 2018, 15, e1002689. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, A.; Sharkey, N. Granny and the robots: Ethical issues in robot care for the elderly. Ethic. Inf. Technol. 2010, 14, 27–40. [Google Scholar] [CrossRef]

| Variable | ± SD | (min–max) | |
|---|---|---|---|
| Age (Years) | 35.20 ± 6.97 | 35.50 (22–56) | |
| Frequency (n) | Percentage (%) | ||
| Gender | Male | 143 | (59.6) |
| Female | 93 | (38.8) | |
| Work setting | Academic | 88 | (36.7) |
| Non-academic | 148 | (61.7) | |
| Educational qualification | Undergraduate | 69 | (28.7) |
| Postgraduate | 167 | (69.6) | |
| Subspecialty | Cardiopulmonary | 18 | (7.5) |
| General | 43 | (17.9) | |
| Geriatrics | 2 | (0.8) | |
| Musculoskeletal | 67 | (27.9) | |
| Neurorehabilitation | 89 | (37.1) | |
| Pediatrics rehabilitation | 12 | (5.0) | |
| Workplace AI applications | 0 | 152 | (63.3) |
| 1 | 35 | (14.6) | |
| 2 to 4 | 37 | (15.4) | |
| More than 4 | 12 | (5.0) | |
| AI ethical implications | Technology trust | 92 | (40.1) |
| Empathy | 83 | (35.2) | |
| Users’ proficiency | 61 | (25.8) | |
| AI curriculum implementation | Yes | 186 | (78.8) |
| No | 50 | (21.2) | |
| AI knowledge | General | 211 | (89.4) |
| Healthcare | 150 | (75.4) | |
| Rehabilitation | 178 | (63.6) | |
| Variable | B | 95% CI for B | SE B | β | p Value | ||
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Knowledge about AI in rehabilitation | |||||||
| Gender | Constant | 0.50 | 0.21 | ||||
| Male | 0.08 | 0.63 | 1.87 | 0.28 | 1.09 | 0.76 | |
| Female | Reference | ||||||
| Employment Sector | Constant | 0.36 | 0.17 | ||||
| Non academic | 0.57 | 1.01 | 3.12 | 0.29 | 1.77 | 0.04 | |
| Academic | Reference | ||||||
| Experience | Constant | 0.16 | 0.18 | ||||
| >10 years | 0.89 | 1.40 | 4.22 | 0.28 | 2.44 | 0.002 | |
| <10 years | Reference | ||||||
| Qualification | Constant | 0.09 | 0.24 | ||||
| Postgraduate | 0.68 | 1.11 | 3.50 | 0.29 | 1.97 | 0.02 | |
| Undergraduate | Reference | ||||||
| AI in work place | Constant | 0.13 | 0.16 | ||||
| 1 or more AI in workplace | 1.39 | 2.12 | 7.67 | 0.33 | 4.03 | ≤0.0001 | |
| No AI in workplace | Reference | ||||||
| Specialty | Constant | 1.11 | 0.25 | ||||
| Musculoskeletal | −0.66 | 0.26 | 1.03 | 0.35 | 0.52. | 0.06 | |
| General | −1.01 | 0.19 | 0.70 | 0.33 | 0.36 | 0.002 | |
| Neurorehabilitation | Reference | ||||||
| Variable | B | 95%CI for B | SE B | β | % Predictability | |
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Step 1 | 63.6 | |||||
| Constant | 0.13 | 0.16 | ||||
| AI in workplace | ||||||
| 1 or more AI in workplace | 1.39 | 2.12 | 7.67 | 0.33 | 4.03 *** | |
| No AI in workplace | Reference | |||||
| Step 2 | 67.4 | |||||
| Constant | −0.23 | 0.21 | ||||
| AI in workplace | ||||||
| 1 or more AI in workplace | 1.36 | 2.04 | 7.51 | 0.33 | 3.91 *** | |
| No AI in workplace | Reference | |||||
| Years of experience | ||||||
| <10 years | 0.85 | 1.32 | 4.14 | 0.29 | 2.34 ** | |
| >10 Years | Reference | |||||
| Step 3 | 72.0 | |||||
| Constant | −0.44 | 0.32 | ||||
| AI in workplace | ||||||
| 1 or more AI in workplace | 1.34 | 1.95 | 7.44 | 0.34 | 3.81 *** | |
| No AI in workplace | Reference | |||||
| Years of experience | ||||||
| <10 years | 0.97 | 1.46 | 4.79 | 0.30 | 2.64 *** | |
| >10 Years | Reference | |||||
| Specialty | ||||||
| General | −0.28 | 0.37 | 1.54 | 0.36 | 0.76 | |
| Neurorehabilitation | 0.77 | 1.03 | 4.45 | 0.38 | 2.16 * | |
| Musculoskeletal | Reference | |||||
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | Total | ||
|---|---|---|---|---|---|---|---|
| Reducing therapist workload | |||||||
| Gender | Male | 38 (16.1) | 71 (30.1) | 31 (13.1) | 2 (0.8) | 1 (0.4) | 143 (60.6) |
| Female | 29 (12.3) | 42 (17.8) | 21 (8.9) | 1 (0.4) | 0 (0) | 93 (39.4) | |
| Employment sector | Academic | 25 (10.6) | 46 (19.5) | 17 (7.2) | 0 (0) | 0 (0) | 88 (37.3) |
| Non academic | 42 (17.8) | 67 (28.4) | 35 (14.8) | 3 (1.3) | 1 (0.4) | 148 (62.7) | |
| Experience | >10 years | 26 (11.0) | 60 (25.4) | 25 (10.6) | 1 (0.4) | 0 (0) | 112 (47.5) |
| <10 years | 41 (17.4) | 53 (22.5) | 27 (11.4) | 2 (0.8) | 1 (0.4) | 124 (52.5) | |
| Qualification | Postgraduate | 50 (21.2) | 80 (33.9) | 35 (14.8) | 1 (0.4) | 1 (0.4) | 167 (70.8) |
| Undergraduate | 17 (7.2) | 33 (14.0) | 17 (7.2) | 2 (0.8) | 0 (0) | 96 (29.2) | |
| Easing the patient care | |||||||
| Gender | Male | 41 (17.4) | 72 (30.5) | 25 (10.6) | 4 (1.7) | 1 (0.4) | 143 (60.6) |
| Female | 25 (10.6) | 53 (22.5) | 14 (5.9) | 0 (0) | 1 (0.4) | 93 (39.4) | |
| Employment sector | Academic | 23 (9.7) | 50 (21.2) | 15 (6.4) | 0 (0) | 0 (0) | 88 (37.3) |
| Non academic | 43 (18.2) | 75 (31.8) | 24 (10.2) | 4 (1.7) | 2 (0.8) | 148 (62.7) | |
| Experience | >10 years | 29 (12.3) | 66 (28.0) | 13 (5.5) | 3 (1.3) | 1 (0.4) | 112 (47.5) |
| <10 years | 37 (15.7) | 59 (25.0) | 26 (11.0) | 1 (0.4) | 1 (0.4) | 124 (52.5) | |
| Qualification | Postgraduate | 47 (19.9) | 91 (38.6) | 25 (10.6) | 3 (1.3) | 1 (0.4) | 167 (70.8) |
| Undergraduate | 19 (8.1) | 34 (14.4) | 14 (5.9) | 1 (0.4) | 1 (0.4) | 69 (29.2) | |
| Prevention of diseases | |||||||
| Gender | Male | 29 (12.3) | 34 (14.4) | 51 (21.6) | 24 (10.2) | 5 (2.1) | 143 (60.6) |
| Female | 14 (5.9) | 30 (12.7) | 32 (13.6) | 16 (6.8) | 1 (0.4) | 93 (39.4) | |
| Employment sector | Academic | 13 (5.5) | 26 (11.0) | 39 (16.5) | 10 (4.2) | 0 (0) | 88 (37.3) |
| Non academic | 30 (12.7) | 38 (16.1) | 44 (18.6) | 30 (12.7) | 6 (2.5) | 148 (62.7) | |
| Experience | >10 years | 16 (6.8) | 36 (15.3) | 42 (17.8) | 16 (6.8) | 2 (0.8) | 112 (47.5) |
| <10 years | 27 (11.4) | 28 (11.9) | 41 (17.4) | 24 (10.2) | 4 (1.7) | 124 (52.5) | |
| Qualification | Postgraduate | 26 (11.0) | 50 (21.2) | 63 (26.7) | 24 (10.2) | 4 (1.7) | 167 (70.8) |
| Undergraduate | 17 (7.2) | 14 (5.9) | 20 (8.5) | 16 (6.8) | 2 (0.8) | 69 (29.2) | |
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | Total | ||
|---|---|---|---|---|---|---|---|
| Disease prediction | |||||||
| Gender | Male | 26 (11.0) | 59 (25.0) | 47 (19.9) | 10 (4.2) | 1 (0.4) | 143 (60.6) |
| Female | 14 (5.9) | 45 (19.1) | 25 (10.6) | 8 (3.4) | 1 (0.4) | 93 (39.4) | |
| Employment sector | Academic | 18 (7.6) | 37 (15.7) | 26 (11.0) | 6 (2.5) | 1 (0.4) | 88 (37.3) |
| Non academic | 22 (9.3) | 67 (28.4) | 46 (19.5) | 12 (5.1) | 1 (0.4) | 148 (62.7) | |
| Experience | >10 years | 20 (8.5) | 57 (24.2) | 25 (10.6) | 10 (4.2) | 0 (0) | 112 (47.5) |
| <10 years | 20 (8.5) | 47 (19.9) | 47 (19.9) | 8 (3.4) | 2 (0.8) | 124 (52.5) | |
| Qualification | Postgraduate | 28 (11.9) | 73 (30.9) | 50 (21.2) | 15 (6.4) | 1 (0.4) | 167 (70.8) |
| Undergraduate | 12 (5.1) | 31 (13.1) | 22 (9.3) | 3 (1.3) | 1 (0.4) | 69 (29.2) | |
| Goal setting | |||||||
| Gender | Male | 40 (16.9) | 66 (28.0) | 29 (12.3) | 5 (2.1) | 3 (1.3) | 143 (60.6) |
| Female | 20 (8.5) | 50 (21.2) | 17 (7.2) | 6 (2.5) | 0 (0) | 93 (39.4) | |
| Employment sector | Academic | 18 (7.6) | 42 (17.8) | 26 (11.0) | 2 (0.8) | 0 (0) | 88 (37.3) |
| Non academic | 42 (17.8) | 74 (31.4) | 20 (8.5) | 9 (3.8) | 3 (1.3) | 148 (62.7) | |
| Experience | >10 years | 27 (11.4) | 62 (26.3) | 22 (9.3) | 1 (0.4) | 0 (0) | 112 (47.5) |
| <10 years | 33 (14.0) | 54 (22.9) | 24 (10.2) | 10 (4.2) | 3 (1.3) | 124 (52.5) | |
| Qualification | Postgraduate | 40 (16.9) | 79 (33.5) | 38 (16.1) | 8 (3.4) | 2 (0.8) | 167 (70.8) |
| Undergraduate | 20 (8.5) | 37 (15.7) | 8 (3.4) | 3 (1.3) | 1 (0.4) | 69 (29.2) | |
| Assistive technologies | |||||||
| Gender | Male | 50 (21.2) | 76 (32.2) | 15 (6.4) | 2 (0.8) | 0 (0) | 143 (60.6) |
| Female | 38 (16.1) | 44 (18.6) | 11 (4.7) | 0 (0) | 0 (0) | 93 (39.4) | |
| Employment sector | Academic | 30 (12.7) | 49 (20.8) | 9 (3.8) | 0 (0) | 0 (0) | 88 (37.3) |
| Non academic | 58 (24.6) | 71 (30.1) | 17 (7.2) | 2 (0.8) | 0 (0) | 148 (62.7) | |
| Experience | >10 years | 44 (18.6) | 62 (26.3) | 6 (2.5) | 0 (0) | 0 (0) | 112 (47.5) |
| <10 years | 4 (18.6) | 58 (24.6) | 20 (8.5) | 2 (0.8) | 0 (0) | 124 (52.5) | |
| Qualification | Postgraduate | 70 (29.7) | 83 (35.2) | 13 (5.5) | 1 (0.4) | 0 (0) | 167 (70.8) |
| Undergraduate | 18 (7.7) | 37 (15.7) | 13 (5.5) | 1 (0.4) | 0 (0) | 69 (29.2) | |
| Diagnostic tool | |||||||
| Gender | Male | 43 (18.2) | 56 (23.7) | 36 (15.3) | 4 (1.7) | 4 (1.7) | 143 (60.6) |
| Female | 26 (11.0) | 42 (18.2) | 20 (8.5) | 4 (1.7) | 0 (0) | 93 (39.4) | |
| Employment sector | Academic | 24 (10.2) | 37 (15.7) | 23 (9.7) | 4 (1.7) | 0 (0) | 88 (37.3) |
| Non academic | 45 (19.1) | 62 (26.3) | 33 (14.0) | 4 (1.7) | 4 (1.7) | 148 (62.7) | |
| Experience | >10 years | 39 (16.5) | 46 (19.7) | 25 (10.6) | 2 (0.8) | 0 (0) | 112 (47.5) |
| <10 years | 30 (12.7) | 53 (22.5) | 31 (13.1) | 6 (2.5) | 4 (1.7) | 124 (52.5) | |
| Qualification | Postgraduate | 49 (20.8) | 73 (30.9) | 37(15.7) | 6 (2.5) | 2 (0.8) | 167 (70.8) |
| Undergraduate | 20 (8.5) | 26 (11.0) | 19 (8.1) | 2 (0.8) | 2 (0.8) | 69 (29.2) | |
| Education enhancement | |||||||
| Gender | Male | 52 (22.0) | 63 (26.7) | 23 (9.7) | 1 (1.3) | 2 (0.8) | 143 (60.6) |
| Female | 29 (12.3) | 51 (21.6) | 10 (4.2) | 3 (1.3) | 0 (0) | 93 (39.4) | |
| Employment sector | Academic | 27 (11.4) | 48 (20.3) | 9 (3.8) | 4 (1.7) | 0 (0) | 88 (37.3) |
| Non academic | 54 (22.9) | 66 (28.0) | 24 (10.2) | 2 (0.8) | 2 (0.8) | 148 (62.7) | |
| Experience | >10 years | 37 (15.7) | 58 (24.6) | 16 (6.8) | 1 (0.4) | 0 (0) | 112 (47.5) |
| <10 years | 44 (18.6) | 56 (23.7) | 17 (7.2) | 5 (2.1) | 2 (0.8) | 124 (52.5) | |
| Qualification | Postgraduate | 57 (24.2) | 78 (33.1) | 26 (11.0) | 6 (2.5) | 0 (0) | 167 (70.8) |
| Undergraduate | 24 (10.2) | 36 (15.3) | 7 (3.0) | 0 (0) | 2 (0.8) | 69 (29.2) | |
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | Total | ||
|---|---|---|---|---|---|---|---|
| Reducing human resource | |||||||
| Gender | Male | 26 (11.0) | 64 (27.1) | 37 (15.7) | 12 (5.1) | 4 (1.7) | 143 (60.6) |
| Female | 33 (14.0) | 48 (20.3) | 8 (3.4) | 3 (1.3) | 1 (0.4) | 93 (39.4) | |
| Employment sector | Academic | 27 (11.4) | 44 (18.6) | 13 (5.5) | 4 (1.7) | 0 (0) | 88 (37.7) |
| Non academic | 32 (13.6) | 68 (28.8) | 32 (13.6) | 11 (4.7) | 5 (2.1) | 148 (62.7) | |
| Experience | >10 years | 22 (9.3) | 59 (25.0) | 22 (9.3) | 7 (3.0) | 2 (0.8) | 112 (47.5) |
| <10 years | 37 (15.7) | 53 (22.5) | 23 (9.7) | 8 (3.4) | 3 (1.3) | 124 (52.5) | |
| Qualification | Postgraduate | 45 (19.1) | 80 (33.9) | 29 (12.3) | 10 (4.9) | 3 (1.3) | 167 (70.8) |
| Undergraduate | 14 (5.9) | 32 (13.6) | 16 (6.8) | 5 (2.1) | 2 (0.8) | 69 (29.2) | |
| Increase productivity | |||||||
| Gender | Male | 49 (20.8) | 60 (25.4) | 29 (12.3) | 4 (1.7) | 1 (0.4) | 143 (60.6) |
| Female | 25 (10.6) | 55 (23.3) | 12 (5.1) | 1 (0.6) | 0 (0) | 93 (39.4) | |
| Employment sector | Academic | 26 (11.0) | 48 (20.3) | 14 (5.9) | 0 (0) | 0 (0) | 88 (37.3) |
| Non academic | 48 (20.3) | 67 (28.4) | 27 (11.4) | 5 (2.1) | 1 (0.4) | 148 (62.7) | |
| Experience | >10 years | 35 (14.8) | 64 (27.1) | 12 (5.1) | 1 (0.4) | 0 (0) | 112 (47.5) |
| <10 years | 39 (16.5) | 51 (21.6) | 29 (12.3) | 4 (1.7) | 1 (0.4) | 124 (52.5) | |
| Qualification | Postgraduate | 54 (22.9) | 83 (35.2) | 28 (11.9) | 2 (0.8) | 0 (0) | 167 (70.8) |
| Undergraduate | 20 (8.5) | 32 (13.6) | 13 (5.5) | 3 (1.3) | 1 (0.4) | 69 (29.2) | |
| Improve patient quality of life | |||||||
| Gender | Male | 55 (23.3) | 50 (21.2) | 29 (12.3) | 7 (3.0) | 2 (0.8) | 143 (60.6) |
| Female | 29 (12.3) | 40 (16.9) | 22 (9.3) | 2 (0.8) | 0 (0) | 93 (39.4) | |
| Employment sector | Academic | 23 (9.7) | 37 (15.7) | 26 (11.0) | 2 (0.8) | 0 (0) | 88 (37.3) |
| Non academic | 61 (25.8) | 53 (22.5) | 25 (10.6) | 7 (3.0) | 2 (0.8) | 148 (62.7) | |
| Experience | >10 years | 35 (14.8) | 50 (21.2) | 24 (10.2) | 3 (1.3) | 0 (0) | 112 (47.5) |
| <10 years | 49 (20.8) | 40 (16.9) | 27 (11.4) | 6 (2.5) | 2 (0.8) | 124 (52.5) | |
| Qualification | Postgraduate | 59 (25.0) | 67 (28.4) | 36 (15.3) | 4 (1.7) | 1 (0.4) | 167 (70.8) |
| Undergraduate | 25 (10.6) | 23 (9.7) | 15 (6.4) | 5 (2.1) | 1 (0.4) | 69 (29.2) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsobhi, M.; Sachdev, H.S.; Chevidikunnan, M.F.; Basuodan, R.; K U, D.K.; Khan, F. Facilitators and Barriers of Artificial Intelligence Applications in Rehabilitation: A Mixed-Method Approach. Int. J. Environ. Res. Public Health 2022, 19, 15919. https://doi.org/10.3390/ijerph192315919
Alsobhi M, Sachdev HS, Chevidikunnan MF, Basuodan R, K U DK, Khan F. Facilitators and Barriers of Artificial Intelligence Applications in Rehabilitation: A Mixed-Method Approach. International Journal of Environmental Research and Public Health. 2022; 19(23):15919. https://doi.org/10.3390/ijerph192315919
Chicago/Turabian StyleAlsobhi, Mashael, Harpreet Singh Sachdev, Mohamed Faisal Chevidikunnan, Reem Basuodan, Dhanesh Kumar K U, and Fayaz Khan. 2022. "Facilitators and Barriers of Artificial Intelligence Applications in Rehabilitation: A Mixed-Method Approach" International Journal of Environmental Research and Public Health 19, no. 23: 15919. https://doi.org/10.3390/ijerph192315919





