Can Medical Devices Help Mitigate Global Environmental Change Effects on Human and Animal Health? A Pilot Study
Abstract
1. Introduction
- (1)
- Health outcomes: injury and mortality from extreme weather events, heat-related diseases, respiratory illness, water-borne diseases and other water-related health impacts, zoonosis, vector-borne diseases, malnutrition and food-borne diseases, non-communicable diseases (NDCs), mental and psychosocial diseases;
- (2)
- Health systems and facilities outcomes: Impacts on healthcare facilities, effects on health systems.
- Eye drops: normally aqueous-based solutions with or without the addition of various substances capable of moistening, soothing burning and redness of the eye (hyaluronic acid, plant extracts, mineral salts, collagen of animal origin, glucans, etc.), in single or multidose packs, usually sold as sterile;
- Nasal sprays, nasal drops, nasal creams: these can have the same composition as eye drops; in the case of creams, they lubricate and keep the nasal mucosa hydrated, favoring the re-epithelialization process, minimizing the formation of crusts. They are usually sold as non-sterile;
- Dry nasal sprays: these are composed of a micronized inert powder (e.g., cellulose), which is nebulized in the nasal cavity forming a protective film that acts as a filter, creating a barrier between allergens (pollen, dust mites, hair and epithelia of animals) and the nasal mucous membranes;
- Throat sprays: the application generates a protective film (barrier) that lines the oral cavity, protecting it from contact with external irritating agents. The ingredients can be the same as the sprays and/or nasal drops, with the addition of any hydro alcoholic plant extracts;
- Creams for eczema: the different types of eczema (atopic, chronic of the hands, contact) are characterized by an altered skin barrier, which increases the risk of reactions (dryness, itching, and irritation) to allergens and irritants. They can be applied on inflammatory lesions alone or in association with dermo-corticosteroids; they are composed of mixtures of “fatty” substances (e.g., glycerine, shea butter, triglycerides) alone or in synergy with others (e.g., urea, hyaluronic acid, mineral salts, plant extracts);
- Creams for erythema: the composition is similar to that of creams for eczema, they may also contain UVA and UVB filters that create an active protective barrier against UV rays. Given the lack or scarcity of knowledge on the topic of GECs and MDs, the Istituto Superiore di Sanità (ISS) has initiated a research project. The purpose of this project was to investigate whether MDs might play a role in mitigating the effects of GECs on human and animal health. The ultimate goal is to link the interactions between the environment and health and activate useful tools for prevention.
2. Materials and Methods
- Primary care physicians commonly named “doctors”;
- Veterinarians;
- Pharmacists;
- MD manufacturers.
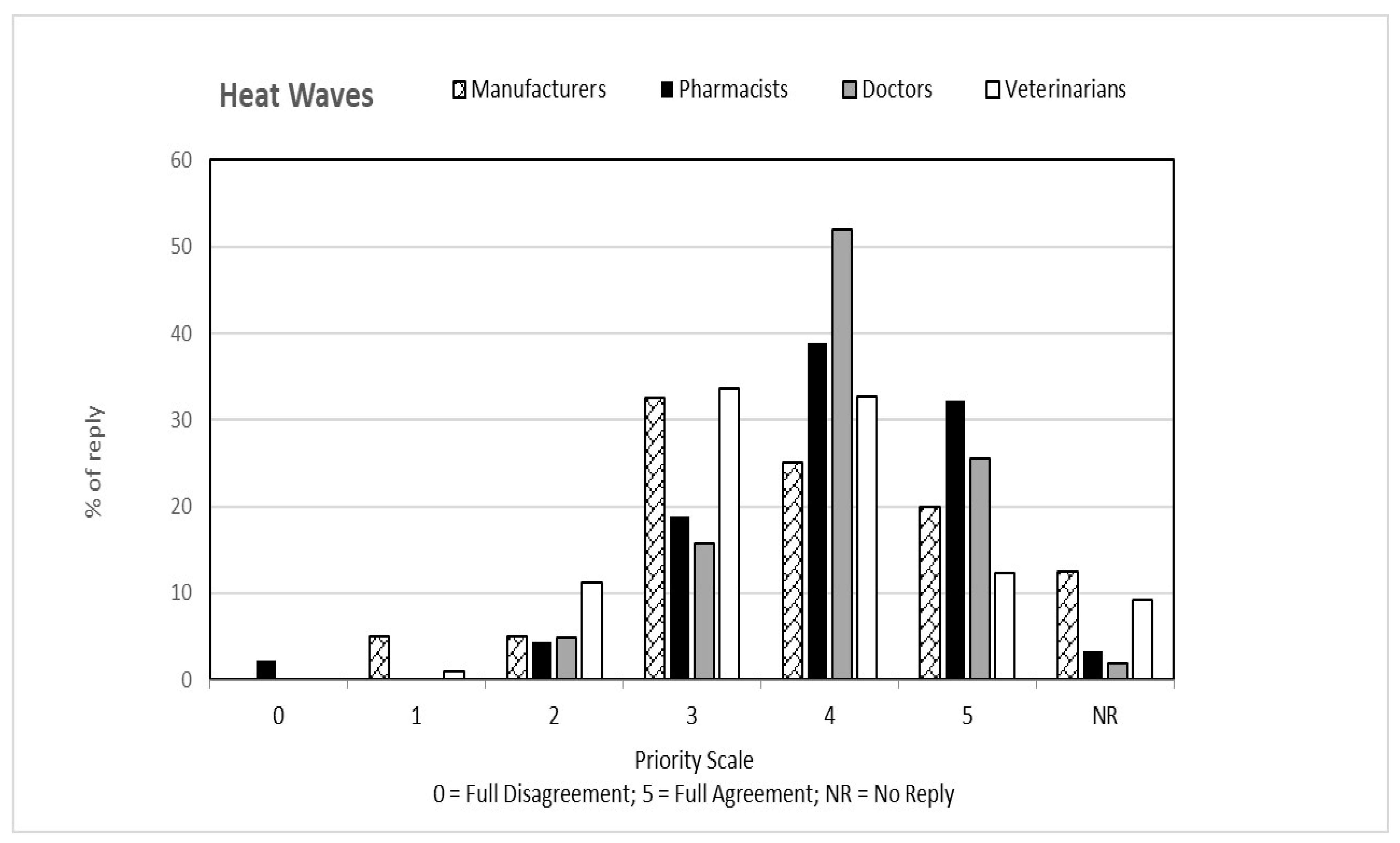
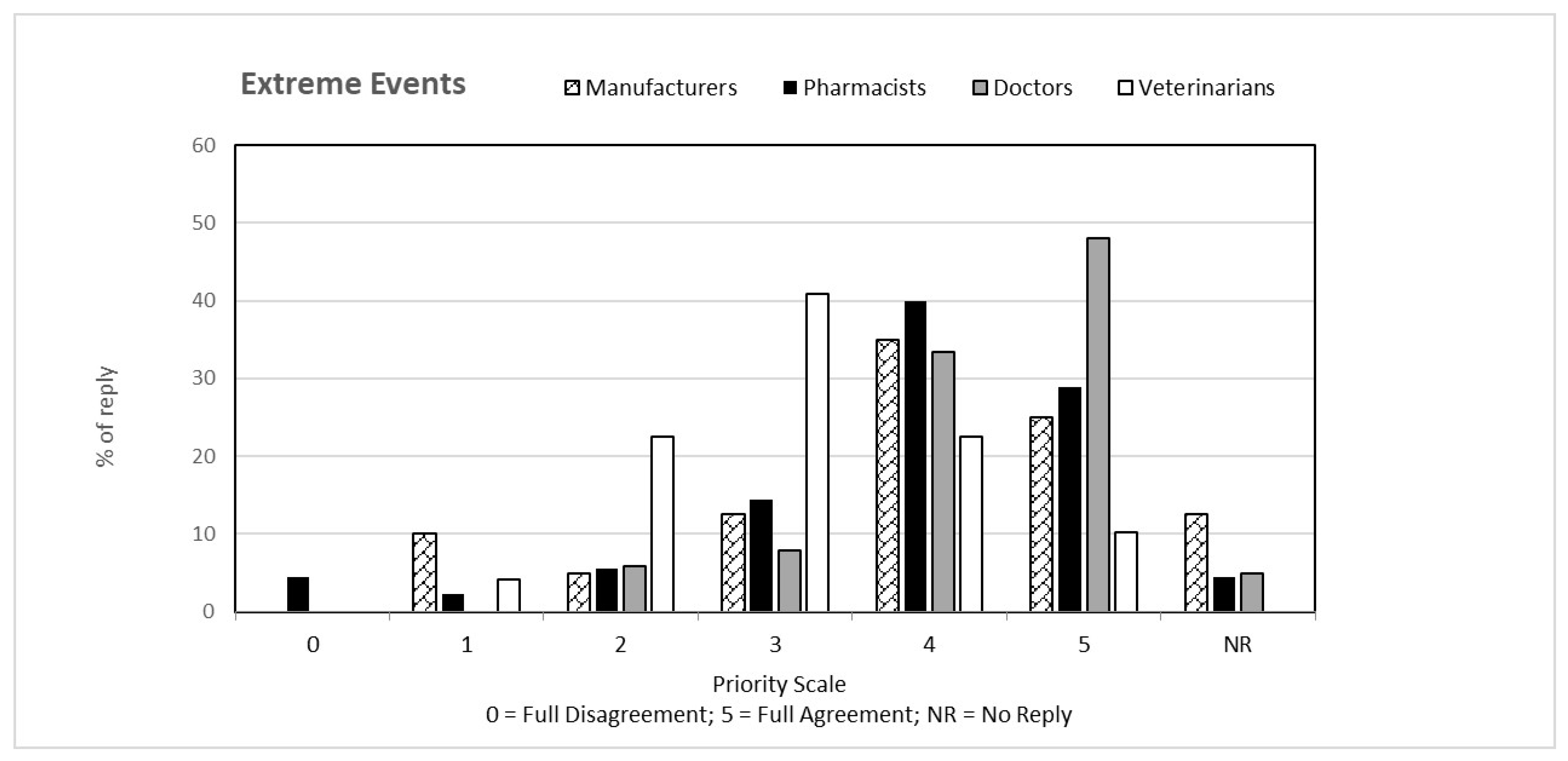
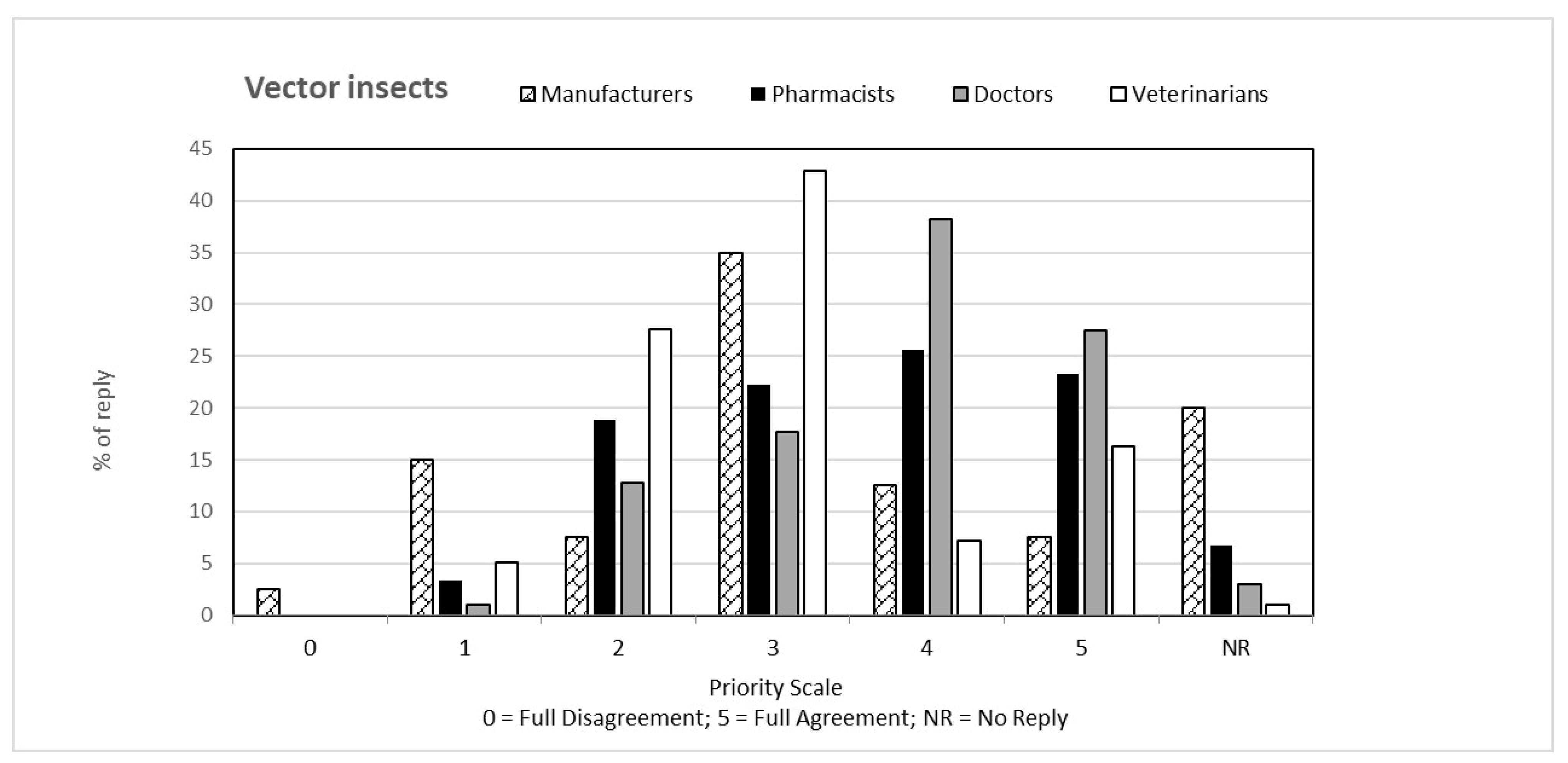
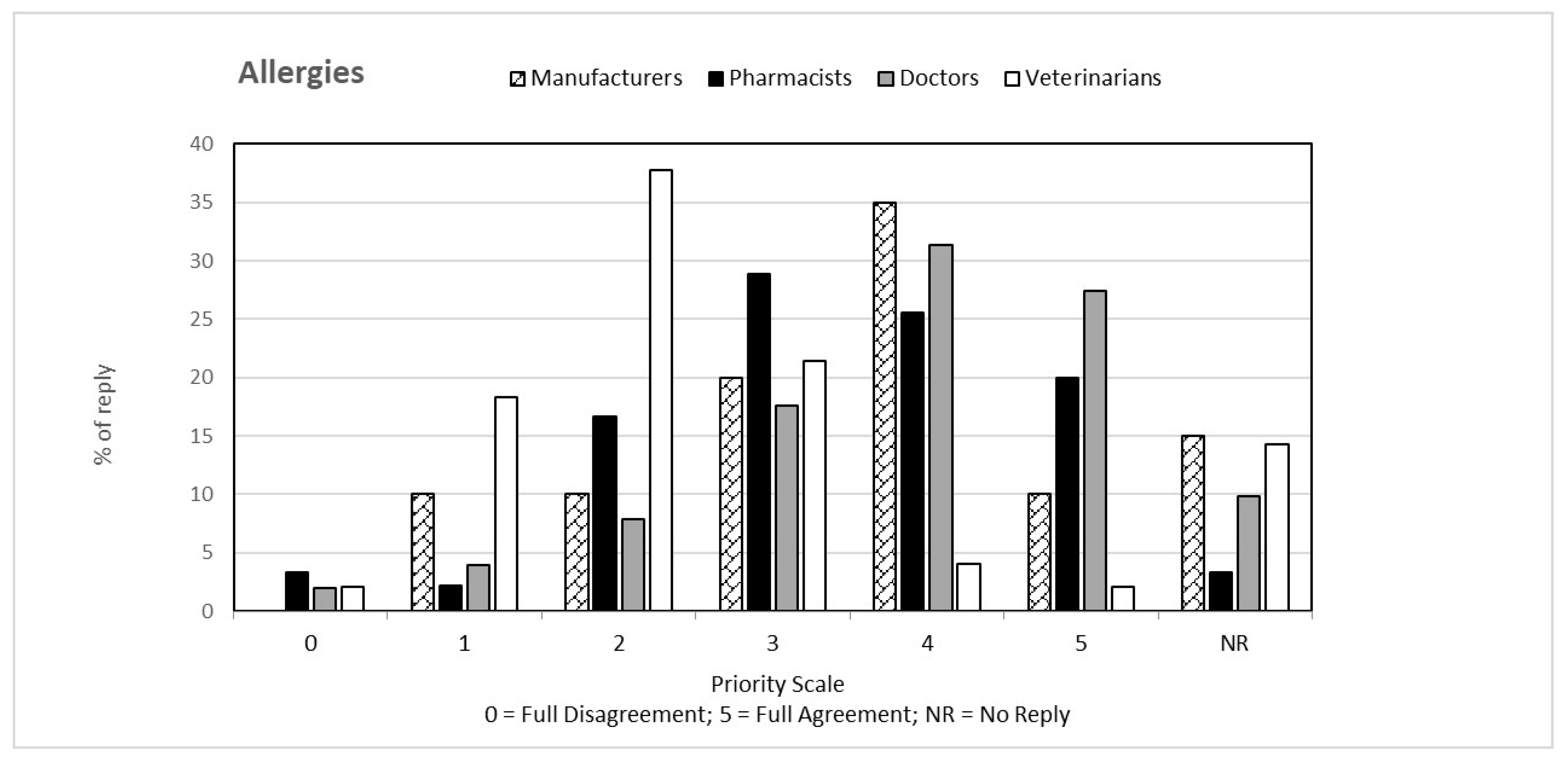
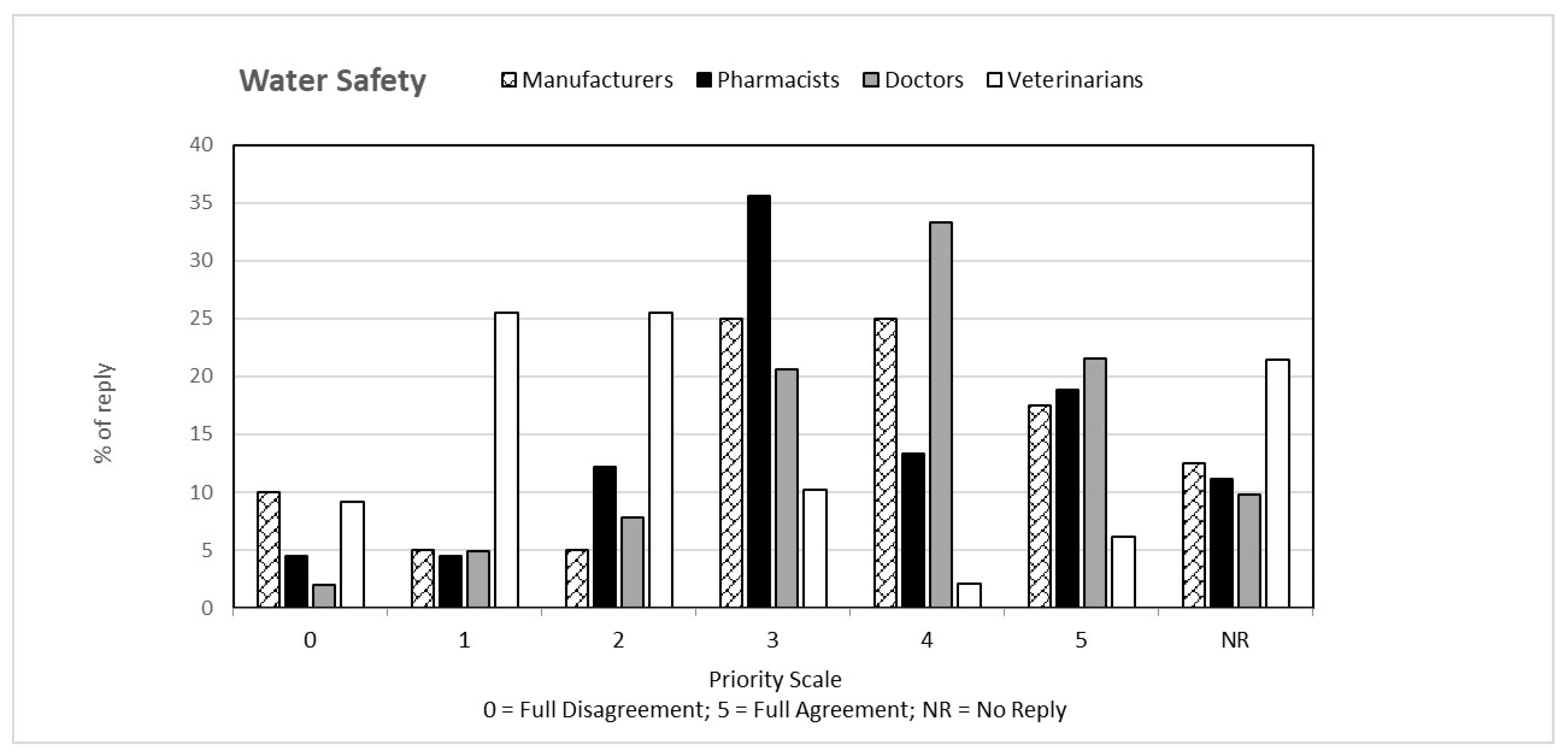
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ricciardi, W.; Marcheggiani, S.; Puccinelli, C.; Carere, M.; Sofia, T.; Giuliano, F.; Dogliotti, E.; Mancini, L.; Agrimi, U.; Alleva, E.; et al. Health and Climate Change: Science calls for global action. Ann. Ist. Super. Sanita 2019, 55, 323–329. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Climate Change and Health. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed on 17 October 2022).
- World Health Organization. Regional Office for Europe. WHO Guidelines for Indoor Air Quality: Dampness and Mould. World Health Organization. Regional Office for Europe. 2009. Available online: https://apps.who.int/iris/handle/10665/164348 (accessed on 17 October 2022).
- Fisher, P.H.; Brunekreef, B.; Lebret, E. Air pollution related deaths during the 2003 heat wave in the Netherlands. Atmos. Environ. 2004, 38, 1083–1085. [Google Scholar] [CrossRef]
- Stedman, R.C. Risk and Climate Change: Perceptions of Key Policy Actors in Canada. Risk Anal. 2004, 24, 1395–1406. [Google Scholar] [CrossRef] [PubMed]
- van Daalen, K.R.; Romanello, M.; Rocklöv, J.; Semenza, J.C.; Tonne, C.; Markandya, A.; Dasandi, N.; Jankin, S.; Achebak, H.; Ballester, J.; et al. The 2022 Europe report of the Lancet Countdown on health and climate change: Towards a climate resilient future. Lancet Public Health 2022, 7, e942–e965, Erratum in Lancet Public Health 2022. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Arias, P.; Bellouin, N.; Coppola, E.; Jones, R.; Krinner, G.; Marotzke, J.; Naik, V.; Palmer, M.; Plattner, G.-K.; Rogelj, J.; et al. Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Masson-Delmotte, V., Zhai, P., Pirani, A., Connors, S.L., Péan, C., Berger, S., Caud, N., Chen, Y., Goldfarb, L., Gomis, M.I., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2021; p. 2391. Available online: https://www.ipcc.ch/report/ar6/wg1/downloads/report/IPCC_AR6_WGI_FullReport.pdf (accessed on 17 October 2022). [CrossRef]
- Lavecchia, C.; Pilati, S.; Turchiarulo, P.; Mancini, L.; Avellis, L.; Ferrari, C. A meteorological monitoring network to investigate climate change in towns: Six mediterranean urban case studio. Fresenius Environ. Bull. 2019, 28, 4990–4997. [Google Scholar]
- Mancini, L.; Gaudi, S.; Figliomeni, M.; Iacobini, V.; Volpi, E.; Marcheggiani, S. Extreme Events and Health: An Italian Pilot Study. Fresenius Environ. Bull. 2019, 28, 4979–4989. [Google Scholar]
- Spano, D.; Mereu, V.; Bacciu, V.; Barbato, G.; Casartelli, V.; Ellena, M.; Lamesso, E.; Ledda, A.; Marras, S.; Mercogliano, P.; et al. Analisi del Rischio. I Cambiamenti Climatici in Sei Città Italiane. 2021. Available online: https://files.cmcc.it/rischio_clima_2021/CLIMA_sei_citta.pdf (accessed on 17 October 2022). [CrossRef]
- Spano, D.; Mereu, V.; Bacciu, V.; Marras, S.; Trabucco, A.; Adinolfi, M.; Barbato, G.; Bosello, F.; Breil, M.; Chiriacò, M.V.; et al. Analisi del Rischio. I Cambiamenti Climatici in Italia. 2020. Available online: https://www.cmcc.it/it/analisi-del-rischio-i-cambiamenti-climatici-in-italia (accessed on 16 October 2022). [CrossRef]
- European Union. Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC. Off. J. Eur. Union 2017, 117, 1–175. [Google Scholar]
- Ministry of Health MDs Database. Available online: https://www.salute.gov.it/interrogazioneDispositivi/RicercaDispositiviServlet?action=ACTION_MASCHERA (accessed on 17 October 2022).
- Neuman, I.; Finkelstein, Y. Narrow-band red light phototherapy in perennial allergic rhinitis and nasal polyposis. Ann Allergy Asthma Immunol. 1997, 78, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Cento, J.V.; Barbaliscia, S.; Perno, C.F. Biotech innovations in the prevention of respiratory infectious diseases. New Microbiol. 2017, 40, 155–160. [Google Scholar] [PubMed]
- Kenney, P.; Hilberg, O.; Sigsgaard, T. Clinical Application of Nasal Filters: An Observational Study on the Usability of Nasal Filters in Managing Seasonal Allergic Rhinitis. J. Allergy Clin. Immunol. Pract. 2016, 4, 445–452.e4. [Google Scholar] [CrossRef] [PubMed]
- Kenney, P.; Hilberg, O.; Laursen, A.C.; Peel, R.G.; Sigsgaard, T. Preventive effect of nasal filters on allergic rhinitis: A randomized, double-blind, placebo-controlled crossover park study. J. Allergy Clin. Immunol. 2015, 136, 1566–1572.e5. [Google Scholar] [CrossRef] [PubMed][Green Version]
- SNLG (Sistema Nazionale per le Linee Guida). Come Produrre, Diffondere e Aggiornare Linee Guida per la Salute Pubblica. Manuale Metodologico. Istituto Superiore di Sanità. 2011. Available online: https://www.tabaccologia.it/filedirectory/PDF/Linee%20Guida%20-%20Ministero%20Salute%2C%20ISS%2C%20CCM_manuale%20metodologico%20per%20la%20salute%20pubblica.pdf (accessed on 17 October 2022).
- Joshi, A.; Kale, S.; Chandel, S.; Pal, D.K. Likert Scale: Explored and Explained. BJAST 2015, 7, 396–403. [Google Scholar] [CrossRef]
- Marcer, G. Le allergie crociate: Gli allergici a pollini o acari devono guardarsi da alcuni alimenti. Rubrica Ambiente Allerg. 2011, 9, 1–5. Available online: http://www.arpa.veneto.it/temi-ambientali/pollini/file-e-allegati/rubrica-ambiente-e-allergie/Rubrica_Ambiente_Allergie_n9.pdf (accessed on 18 October 2022).
- Watts, N.; Adger, W.N.; Agnolucci, P.; Blackstock, J.; Byass, P.; Cai, W.; Chaytor, S.; Colbourn, T.; Collins, M.; Cooper, A.; et al. Health and climate change: Policy responses to protect public health. Lancet 2015, 386, 1861–1914. [Google Scholar] [CrossRef] [PubMed]
- Office of the High Commissioner for Human Rights—OHCHR, Understanding Human Rights and Climate Change. 2015. Available online: https://www.ohchr.org/sites/default/files/Documents/Issues/ClimateChange/COP21.pdf (accessed on 19 October 2022).
| Potential Effects on Human Health | Pharmacists % | Doctors % | Veterinarians % | MD Manufacturers % |
|---|---|---|---|---|
| Skin | 82.2 | 90.2 | 71.4 | 85.0 |
| Ophthalmic | 64.4 | 79.4 | 18.4 | 80.0 |
| Allergies | 86.7 | 86.3 | 69.4 | 85.0 |
| Otorhinolaryngological | 66.7 | 62.7 | 12.2 | 67.5 |
| Infectious diseases | 71.1 | 79.4 | 65.3 | 62.5 |
| Mental Health | 45.6 | 64.7 | 11.2 | 42.5 |
| Priority Scale | ||||||||
|---|---|---|---|---|---|---|---|---|
| Potential Effects on Human Health | Medical Devices | 0 | 1 | 2 | 3 | 4 | 5 | No Reply |
| % | ||||||||
| Skin | Barrier gel | 4.4 | 13.3 | 16.7 | 25.6 | 20.0 | 10.0 | 10.0 |
| Barrier cream | 3.3 | 6.7 | 14.4 | 27.8 | 27.8 | 13.3 | 6.7 | |
| Barrier foam | 6.7 | 14.4 | 18.9 | 25.6 | 13.3 | 7.8 | 13.3 | |
| Erythema products | 2.2 | 2.2 | 8.9 | 24.4 | 21.1 | 27.8 | 13.3 | |
| Eczema products | 2.2 | 2.2 | 10.0 | 20.0 | 36.7 | 13.3 | 15.6 | |
| Ophthalmic | Dry eye products | 3.3 | 10.0 | 12.2 | 27.8 | 20.0 | 15.6 | 11.1 |
| Drops | 2.2 | 6.7 | 21.1 | 32.2 | 14.4 | 8.9 | 14.4 | |
| Ophthalmic solutions | 6.7 | 6.7 | 12.2 | 35.6 | 18.9 | 5.6 | 14.4 | |
| Eye drops | 2.2 | 3.3 | 31.1 | 26.7 | 17.8 | 8.9 | 10.0 | |
| Otorhinolaryngological | Aerosol solutions | 1.1 | 3.3 | 10.0 | 34.4 | 18.9 | 24.4 | 7.8 |
| Products with sea water | 6.7 | 6.7 | 12.2 | 25.6 | 18.9 | 17.8 | 12.2 | |
| Products with aqueous solution | 7.8 | 12.2 | 11.1 | 25.6 | 17.8 | 13.3 | 12.2 | |
| Infectious diseases | Insect bite products | 1.1 | 2.2 | 11.1 | 20.0 | 33.3 | 22.2 | 10.0 |
| Products for pediculosis | 6.7 | 1.1 | 12.2 | 22.2 | 21.1 | 20.0 | 16.7 | |
| Products for onychomycosis | 10.0 | 3.3 | 7.8 | 20.0 | 22.2 | 21.1 | 15.6 | |
| Allergies | Allergy pads | 7.8 | 15.6 | 16.7 | 23.3 | 14.4 | 13.3 | 8.9 |
| Mental health | Stress reduction products (including apps) | 3.3 | 12.2 | 7.8 | 15.6 | 18.9 | 25.6 | 16.7 |
| mean | 4.6 | 7.2 | 13.8 | 25.4 | 20.9 | 15.8 | 12.3 | |
| Priority Scale | ||||||||
|---|---|---|---|---|---|---|---|---|
| Potential Effects on Human Health | Medical Devices | 0 | 1 | 2 | 3 | 4 | 5 | No Reply |
| % | ||||||||
| Skin | Barrier gel | 2.0 | 2.9 | 5.9 | 11.8 | 21.6 | 7.8 | 48.0 |
| Barrier cream | 2.9 | 2.9 | 6.9 | 12.7 | 22.5 | 27.5 | 24.5 | |
| Barrier foam | 2.0 | 6.9 | 4.9 | 7.8 | 18.6 | 6.9 | 52.9 | |
| Erythema products | 2.9 | 2.0 | 6.9 | 11.8 | 25.5 | 31.4 | 19.6 | |
| Eczema products | 1.0 | 2.9 | 3.9 | 11.8 | 29.4 | 32.4 | 18.6 | |
| Ophthalmic | Dry eye products | 2.9 | 4.9 | 5.9 | 6.9 | 13.7 | 6.9 | 58.8 |
| Drops | 1.0 | 3.9 | 4.9 | 12.7 | 23.5 | 27.5 | 26.5 | |
| Ophthalmic solutions | 1.0 | 2.9 | 4.9 | 16.7 | 22.5 | 16.7 | 35.3 | |
| Eye drops | 2.0 | 4.9 | 6.9 | 11.8 | 24.5 | 16.7 | 33.3 | |
| Otorhinolaryngological | Aerosol solutions | 2.9 | 2.9 | 1.0 | 17.6 | 25.5 | 13.7 | 36.3 |
| Products with sea water | 3.9 | 4.9 | 6.9 | 11.8 | 24.5 | 13.7 | 34.3 | |
| Products with aqueous solution | 5.9 | 6.9 | 3.9 | 6.9 | 10.8 | 13.7 | 52.0 | |
| Infectious diseases | Insect bite products | 2.9 | 5.9 | 2.9 | 9.8 | 15.7 | 8.8 | 53.9 |
| Products for pediculosis | 2.0 | 2.0 | 4.9 | 9.8 | 21.6 | 32.4 | 27.5 | |
| Products for onychomycosis | 1.0 | 4.9 | 3.9 | 13.7 | 16.7 | 9.8 | 50.0 | |
| Allergies | Allergy pads | 3.9 | 6.9 | 7.8 | 11.8 | 13.7 | 24.5 | 31.4 |
| Mental health | Stress reduction products (including apps) | 2.9 | 5.9 | 6.9 | 14.7 | 22.5 | 18.6 | 28.4 |
| mean | 2.5 | 4.4 | 5.2 | 11.8 | 20.8 | 18.2 | 37.1 | |
| Priority Scale | ||||||||
|---|---|---|---|---|---|---|---|---|
| Potential Effects on Human Health | Medical Devices | 0 | 1 | 2 | 3 | 4 | 5 | No Reply |
| % | ||||||||
| Skin | Barrier gel | 2.0 | 1.0 | 3.1 | 5.1 | 5.1 | 0.0 | 83.7 |
| Barrier cream | 0.0 | 3.1 | 1.0 | 1.0 | 5.1 | 0.0 | 89.8 | |
| Barrier foam | 0.0 | 1.0 | 1.0 | 3.1 | 4.1 | 0.0 | 90.8 | |
| Erythema products | 0.0 | 3.1 | 3.1 | 3.1 | 7.1 | 1.0 | 82.7 | |
| Eczema products | 0.0 | 1.0 | 1.0 | 0.0 | 0.0 | 1.0 | 96.9 | |
| Ophthalmic | Dry eye products | 0.0 | 4.1 | 3.1 | 1.0 | 1.0 | 0.0 | 90.8 |
| Drops | 0.0 | 2.0 | 2.0 | 2.0 | 3.1 | 0.0 | 90.8 | |
| Ophthalmic solutions | 0.0 | 5.1 | 1.0 | 5.1 | 4.1 | 0.0 | 84.7 | |
| Eye drops | 4.1 | 0.0 | 4.1 | 7.1 | 4.1 | 1.0 | 79.6 | |
| Otorhinolaryngological | Aerosol solutions | 1.0 | 1.0 | 1.0 | 1.0 | 3.1 | 0.0 | 92.9 |
| Products with sea water | 0.0 | 2.0 | 0.0 | 0.0 | 0.0 | 1.0 | 96.9 | |
| Products with aqueous solution | 0.0 | 2.0 | 1.0 | 1.0 | 0.0 | 0.0 | 95.9 | |
| Infectious diseases | Insect bite products | 0.0 | 2.0 | 1.0 | 1.0 | 1.0 | 1.0 | 93.9 |
| Products for pediculosis | 4.1 | 6.1 | 16.3 | 6.1 | 6.1 | 1.0 | 60.2 | |
| Products for onychomycosis | 0.0 | 1.0 | 0.0 | 1.0 | 0.0 | 1.0 | 96.9 | |
| Allergies | Allergy pads | 0.0 | 3.1 | 0.0 | 3.1 | 1.0 | 0.0 | 92.9 |
| Mental health | Stress reduction products (including apps) | 0.0 | 3.1 | 0.0 | 0.0 | 3.1 | 1.0 | 92.9 |
| mean | 0.7 | 2.4 | 2.3 | 2.4 | 2.8 | 0.5 | 89.0 | |
| Priority Scale | ||||||||
|---|---|---|---|---|---|---|---|---|
| Potential Effects on Human Health | Medical Devices | 0 | 1 | 2 | 3 | 4 | 5 | No Reply |
| % | ||||||||
| Skin | Barrier gel | 0.0 | 2.5 | 5.0 | 27.5 | 15.0 | 22.5 | 27.5 |
| Barrier cream | 2.5 | 0.0 | 5.0 | 17.5 | 27.5 | 20.0 | 27.5 | |
| Barrier foam | 0.0 | 0.0 | 10.0 | 25.0 | 20.0 | 12.5 | 32.5 | |
| Erythema products | 0.0 | 2.5 | 2.5 | 5.0 | 25.0 | 22.5 | 42.5 | |
| Eczema products | 0.0 | 0.0 | 2.5 | 15.0 | 25.0 | 12.5 | 45.0 | |
| Ophthalmic | Dry eye products | 2.5 | 0.0 | 7.5 | 10.0 | 17.5 | 22.5 | 40.0 |
| Drops | 0.0 | 5.0 | 0.0 | 17.5 | 37.5 | 15.0 | 25.0 | |
| Ophthalmic solutions | 2.5 | 0.0 | 5.0 | 25.0 | 30.0 | 17.5 | 20.0 | |
| Eye drops | 2.5 | 0.0 | 2.5 | 27.5 | 22.5 | 25.0 | 20.0 | |
| Otorhinolaryngological | Aerosol solutions | 0.0 | 0.0 | 2.5 | 20.0 | 37.5 | 25.0 | 15.0 |
| Products with sea water | 0.0 | 0.0 | 12.5 | 22.5 | 15.0 | 15.0 | 35.0 | |
| Products with aqueous solution | 5.0 | 2.5 | 7.5 | 12.5 | 15.0 | 10.0 | 47.5 | |
| Infectious diseases | Insect bite products | 7.5 | 5.0 | 2.5 | 12.5 | 15.0 | 5.0 | 52.5 |
| Products for pediculosis | 2.5 | 2.5 | 5.0 | 5.0 | 30.0 | 10.0 | 45.0 | |
| Products for onychomycosis | 2.5 | 5.0 | 5.0 | 15.0 | 15.0 | 5.0 | 52.5 | |
| Allergies | Allergy pads | 5.0 | 2.5 | 0.0 | 20.0 | 17.5 | 20.0 | 35.0 |
| Mental health | Stress reduction products (including apps) | 5.0 | 2.5 | 5.0 | 15.0 | 10.0 | 10.0 | 52.5 |
| mean | 2.2 | 1.8 | 4.7 | 17.2 | 22.1 | 15.9 | 36.2 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mancini, L.; Marcheggiani, S.; Figliomeni, M.; Volpi, E.; Avellis, L.; Volpi, F.; D’Angelo, A.M.; Romanelli, C.; Calamea, P.; Tancioni, L.; et al. Can Medical Devices Help Mitigate Global Environmental Change Effects on Human and Animal Health? A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 15936. https://doi.org/10.3390/ijerph192315936
Mancini L, Marcheggiani S, Figliomeni M, Volpi E, Avellis L, Volpi F, D’Angelo AM, Romanelli C, Calamea P, Tancioni L, et al. Can Medical Devices Help Mitigate Global Environmental Change Effects on Human and Animal Health? A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(23):15936. https://doi.org/10.3390/ijerph192315936
Chicago/Turabian StyleMancini, Laura, Stefania Marcheggiani, Mario Figliomeni, Elisabetta Volpi, Luca Avellis, Fabrizio Volpi, Anna Maria D’Angelo, Cristina Romanelli, Pietro Calamea, Lorenzo Tancioni, and et al. 2022. "Can Medical Devices Help Mitigate Global Environmental Change Effects on Human and Animal Health? A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 23: 15936. https://doi.org/10.3390/ijerph192315936
APA StyleMancini, L., Marcheggiani, S., Figliomeni, M., Volpi, E., Avellis, L., Volpi, F., D’Angelo, A. M., Romanelli, C., Calamea, P., Tancioni, L., & Ferrari, C. (2022). Can Medical Devices Help Mitigate Global Environmental Change Effects on Human and Animal Health? A Pilot Study. International Journal of Environmental Research and Public Health, 19(23), 15936. https://doi.org/10.3390/ijerph192315936







