The Impact of COVID-19 on the Health-Related Behaviours, Mental Well-Being, and Academic Engagement of a Cohort of Undergraduate Students in an Irish University Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Survey Implementation and Data Collection Procedure
2.3. Questionnaire Instrument
2.4. Statistical Analysis
3. Results
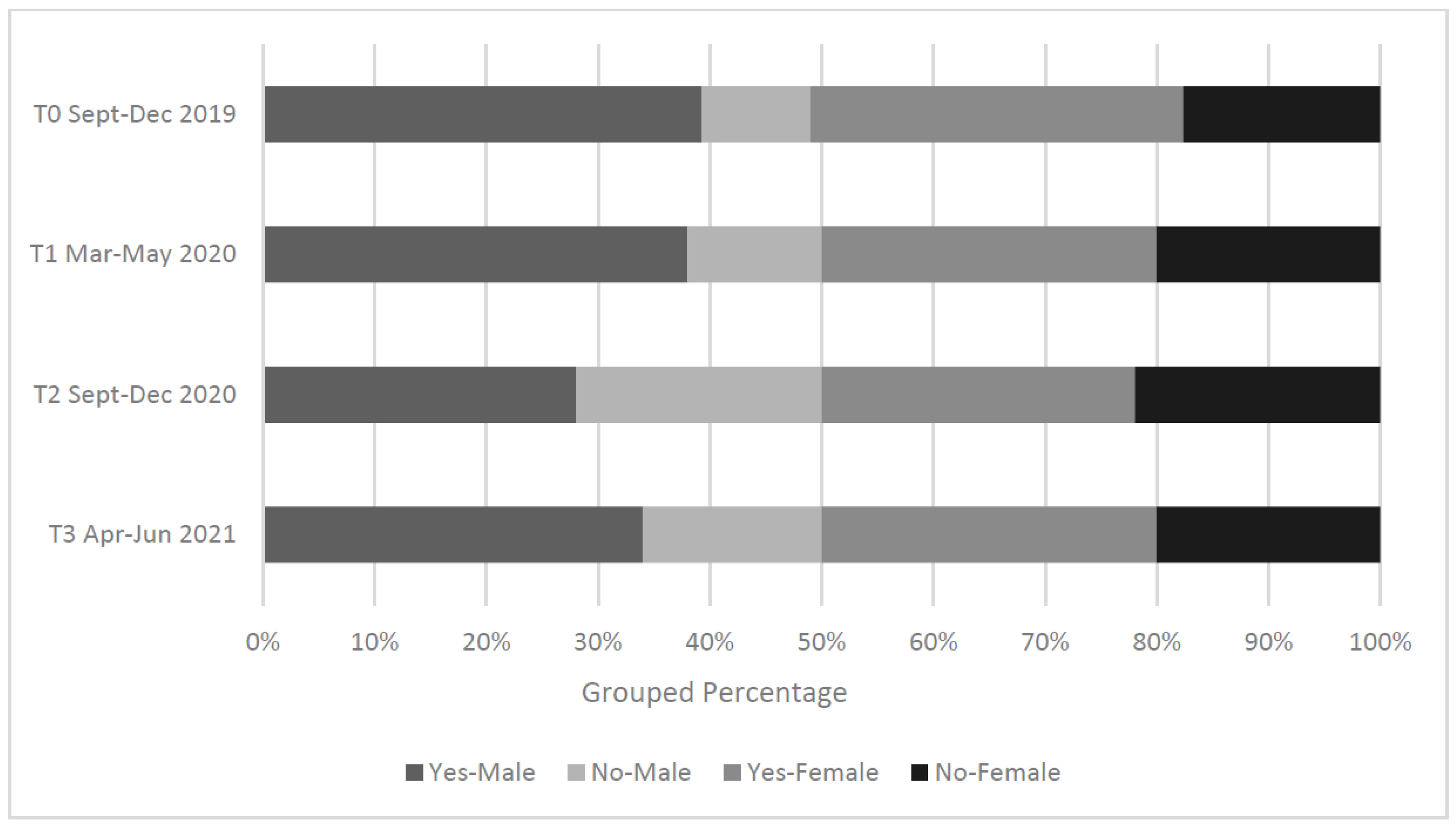
3.1. Participant Demographics
3.2. Health-Related Behaviours
3.2.1. General Health
3.2.2. Physical Activity
3.2.3. Body Mass Index
3.2.4. Nutrition & Alcohol
3.2.5. Sleep
3.3. Mental Well-Being
3.4. Educational Experience & Academic Engagement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Who.int. Coronavirus Disease-Answers. 2022. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/coronavirus-disease-answers?query=What+is+COVID19%3F&referrerPageUrl=https%3A%2F%2Fwww.who.int%2Femergencies%2Fdiseases%2Fnovel-coronavirus-2019%2Fcoronavirus-disease-answers (accessed on 6 January 2022).
- Islam, A.; Barna, S.D.; Raihan, H.; Alam Khan, N.; Hossain, T. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. PLoS ONE 2020, 15, e0238162. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. Coronavirus Pandemic (COVID-19). Our World in Data. 2022. Available online: https://ourworldindata.org/covid-vaccinations?country=OWID_WRL (accessed on 16 February 2022).
- Evans, S.; Alkan, E.; Bhangoo, J.K.; Tenenbaum, H.; Ng-Knight, T. Effects of the COVID-19 lockdown on mental health, wellbeing, sleep, and alcohol use in a UK student sample. Psychiatry Res. 2021, 298, 113819. [Google Scholar] [CrossRef] [PubMed]
- Gloster, A.T.; Lamnisos, D.; Lubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; Aydın, G.; Chong, Y.Y.; et al. Impact of COVID-19 pandemic on mental health: An international study. PLoS ONE 2020, 15, e0244809. [Google Scholar] [CrossRef] [PubMed]
- Bakaloudi, D.R.; Jeyakumar, D.T.; Jayawardena, R.; Chourdakis, M. The impact of COVID-19 lockdown on snacking habits, fast-food and alcohol consumption: A systematic review of the evidence. Clin. Nutr. 2021. [Google Scholar] [CrossRef]
- Batra, K.; Sharma, M.; Batra, R.; Singh, T.; Schvaneveldt, N. Assessing the Psychological Impact of COVID-19 among College Students: An Evidence of 15 Countries. Healthcare 2021, 9, 222. [Google Scholar] [CrossRef]
- Ammar, A.; Trabelsi, K.; Brach, M.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of home con-finement on mental health and lifestyle behaviours during the COVID-19 outbreak: Insights from the ECLB-COVID19 multi-centre study. Biol. Sport 2021, 38, 9. [Google Scholar] [CrossRef]
- Jia, P.; Liu, L.; Xie, X.; Yuan, C.; Chen, H.; Guo, B.; Zhou, J.; Yang, S. Changes in dietary patterns among youths in China during COVID-19 epidemic: The COVID-19 impact on lifestyle change survey (COINLICS). Appetite 2020, 158, 105015. [Google Scholar] [CrossRef]
- Villanti, A.C.; LePine, S.E.; Peasley-Miklus, C.; West, J.C.; Roemhildt, M.; Williams, R.; Copeland, W.E. COVID-related distress, mental health, and substance use in adolescents and young adults. Child Adolesc. Ment. Health 2022, 27, 138–145. [Google Scholar] [CrossRef]
- Palmer, K.; Bschaden, A.; Stroebele-Benschop, N. Changes in lifestyle, diet, and body weight during the first COVID 19 ‘lockdown’ in a student sample. Appetite 2021, 167, 105638. [Google Scholar] [CrossRef]
- Sidebottom, C.; Ullevig, S.; Cheever, K.; Zhang, T. Effects of COVID-19 pandemic and quarantine period on physical activity and dietary habits of college-aged students. Sports Med. Health Sci. 2021, 3, 228–235. [Google Scholar] [CrossRef]
- Schepis, T.S.; De Nadai, A.S.; Bravo, A.J.; Looby, A.; Villarosa-Hurlocker, M.C.; Earleywine, M.; Norms, S. Alcohol use, cannabis use, and psychopathology symptoms among college students before and after COVID-19. J. Psychiatr. Res. 2021, 142, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Healthy Ireland Survey 2021 Summary Report. 2021. Available online: https://www.hse.ie/eng/about/who/healthwellbeing/healthy-ireland/publications/healthy-ireland-survey-2019-summary-report.pdf (accessed on 12 April 2022).
- Bickerdike, A.; Dinneen, J.; O’Neill, C. ‘A Healthy CIT’: An investigation into student health metrics, lifestyle behaviours and the predictors of positive mental health in an Irish higher education setting. Int. J. Environ. Res. 2019, 16, 4318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higher Education Authority. Students|Higher Education Authority. 2022. Available online: https://hea.ie/statistics/data-for-download-and-visualisations/access-our-data/access-our-data-students/ (accessed on 30 June 2022).
- Zhou, J.; Zhang, Q. A Survey Study on U.S. College Students’ Learning Experience in COVID-19. Educ. Sci. 2021, 11, 248. [Google Scholar] [CrossRef]
- Keane, E.; Evans, K.; Morris-Downes, M.; Dee, A.; Fitzgerald, R.; Mannix, M. COVID-19 in the Mid-West—The response from the Department of Public Health, HSE Mid-West between January and September 2020. Health Service Executive (HSE), Department of Public Health. 2020, pp. 13–16. Available online: https://www.lenus.ie/bitstream/handle/10147/628421/Mid-West%20COVID-19%20report_19Oct2020_FINAL.PDF?sequence=1&isAllowed=y (accessed on 14 April 2022).
- Atlam, E.-S.; Ewis, A.; El-Raouf, M.A.; Ghoneim, O.; Gad, I. A new approach in identifying the psychological impact of COVID-19 on university student’s academic performance. Alex. Eng. J. 2021, 61, 5223–5233. [Google Scholar] [CrossRef]
- Meeter, M.; Bele, T.; den Hartogh, C.; Bakker, T.; de Vries, R.E.; Plak, S. College students’ motivation and study results after COVID-19 stay-at-home orders. PsyArXiv 2020. preprint. [Google Scholar] [CrossRef]
- Strayhorn, T.L. Student Development Theory in Higher Education: A Social Psychological Approach; Routledge: London, UK, 2015. [Google Scholar] [CrossRef]
- Ha, E.-J.; Caine-Bish, N. Effect of Nutrition Intervention Using a General Nutrition Course for Promoting Fruit and Vegetable Consumption among College Students. J. Nutr. Educ. Behav. 2009, 41, 103–109. [Google Scholar] [CrossRef]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Babor, T.F.; Higgins-Biddle, J.C.; Saunders, J.B.; Monteiro, M.G. The Alcohol Use Disorders Identification Test; World Health Organization: Geneva, Switzerland, 2001; pp. 1–37. [Google Scholar]
- Lawford, B.R.; Barnes, M.; Connor, J.P.; Heslop, K.; Nyst, P.; Young, R.M. Alcohol Use Disorders Identification Test (AUDIT) scores are elevated in antipsychotic-induced hyperprolactinaemia. J. Psychopharmacol. 2011, 26, 324–329. [Google Scholar] [CrossRef]
- Davoren, M.P.; Shiely, F.; Byrne, M.; Perry, I.J. Hazardous alcohol consumption among university students in Ire-land: A cross-sectional study. BMJ Open 2015, 5, e006045. [Google Scholar] [CrossRef]
- Who.int. Obesity and Overweight. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 13 July 2022).
- Tahara, M.; Mashizume, Y.; Takahashi, K. Mental Health Crisis and Stress Coping among Healthcare College Students Momentarily Displaced from Their Campus Community Because of COVID-19 Restrictions in Japan. Int. J. Environ. Res. Public Health 2021, 18, 7245. [Google Scholar] [CrossRef] [PubMed]
- Rafael, R.D.M.R.; Correia, L.M.; de Mello, A.S.; Prata, J.A.; Depret, D.G.; Santo, T.B.D.E.; e Silva, F.V.C.; Acioli, S. Psychological distress in the COVID-19 pandemic: Prevalence and associated factors at a nursing college. Rev. Bras. Enferm. 2021, 74, e20210023. [Google Scholar] [CrossRef] [PubMed]
- Hamrik, Z.; Sigmundova, D.; Kalman, M.; Pavelka, J.; Sigmund, E. Physical activity and sedentary behaviour in Czech adults: Results from the GPAQ study. Eur. J. Sport Sci. 2012, 14, 193–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawkins, M.S.; Storti, K.L.; Richardson, C.R.; King, W.C.; Strath, S.J.; Holleman, R.G.; Kriska, A.M. Objectively measured physical activity of USA adults by sex, age, and racial/ethnic groups: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 31–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pauline, J. Physical activity behaviors, motivation, and self-efficacy among college students. Coll. Stud. J. 2013, 47, 64–74. [Google Scholar]
- López-Valenciano, A.; Suárez-Iglesias, D.; Sanchez-Lastra, M.A.; Ayán, C. Impact of COVID-19 Pandemic on University Students’ Physical Activity Levels: An Early Systematic Review. Front. Psychol. 2021, 11, 624567. [Google Scholar] [CrossRef] [PubMed]
- Jalal, S.M.; Beth, M.R.M.; Al-Hassan, H.J.M.; Alshealah, N.M.J. Body Mass Index, Practice of Physical Activity and Lifestyle of Students During COVID-19 Lockdown. J. Multidiscip. Health 2021, 14, 1901–1910. [Google Scholar] [CrossRef]
- Food Safety Authority of Ireland. Scientific Recommendations for Healthy Eating Guidelines in Ireland; FSAI: Dublin, Ireland, 2011. [Google Scholar]
- Fruehwirth, J.C.; Gorman, B.L.; Perreira, K.M. The Effect of Social and Stress-Related Factors on Alcohol Use Among College Students during the COVID-19 Pandemic. J. Adolesc. Health 2021, 69, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Bollen, Z.; Pabst, A.; Creupelandt, C.; Fontesse, S.; Lannoy, S.; Pinon, N.; Maurage, P. Prior drinking motives predict alcohol consumption during the COVID-19 lockdown: A cross-sectional online survey among Belgian college students. Addict. Behav. 2020, 115, 106772. [Google Scholar] [CrossRef]
- Lieber, C.S. Relationships between nutrition, alcohol use, and liver disease. Alcohol Res. Health 2003, 27, 220. [Google Scholar]
- Zheng, D.; Yuan, X.; Ma, C.; Liu, Y.; VanEvery, H.; Sun, Y.; Wu, S.; Gao, X. Alcohol consumption and sleep quality: A community-based study. Public Health Nutr. 2020, 24, 1–8. [Google Scholar] [CrossRef]
- Martínez-De-Quel, Ó.; Suárez-Iglesias, D.; López-Flores, M.; Pérez, C.A. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: A longitudinal study. Appetite 2020, 158, 105019. [Google Scholar] [CrossRef]
- Hayley, A.C.; Downey, L.; Stough, C.; Sivertsen, B.; Knapstad, M.; Øverland, S. Social and emotional loneliness and self-reported difficulty initiating and maintaining sleep (DIMS) in a sample of Norwegian university students. Scand. J. Psychol. 2016, 58, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Önder, I.; Beşoluk, Ş.; Iskender, M.; Masal, E.; Demirhan, E. Circadian Preferences, Sleep Quality and Sleep Patterns, Personality, Academic Motivation and Academic Achievement of university students. Learn. Individ. Differ. 2014, 32, 184–192. [Google Scholar] [CrossRef]
- Flueckiger, L.; Lieb, R.; Meyer, A.H.; Mata, J. How Health Behaviors Relate to Academic Performance via Affect: An Intensive Longitudinal Study. PLoS ONE 2014, 9, e111080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahrberg, K.; Dresler, M.; Niedermaier, S.; Steiger, A.; Genzel, L. The interaction between sleep quality and academic performance. J. Psychiatr. Res. 2012, 46, 1618–1622. [Google Scholar] [CrossRef]
- Abdulghani, H.M.; Alrowais, N.A.; Bin-Saad, N.S.; Al-Subaie, N.M.; Haji, A.M.A.; Alhaqwi, A.I. Sleep disorder among medical students: Relationship to their academic performance. Med. Teach. 2012, 34, S37–S41. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, S.P.; Weaver, C.C. Sleep Quality and Academic Performance in University Students: A Wake-Up Call for College Psychologists. J. Coll. Stud. Psychother. 2010, 24, 295–306. [Google Scholar] [CrossRef]
- Rosekind, M.R.; Gregory, K.B.; Mallis, M.M.; Brandt, S.L.; Seal, B.; Lerner, D. The Cost of Poor Sleep: Workplace Productivity Loss and Associated Costs. J. Occup. Environ. Med. 2010, 52, 91–98. [Google Scholar] [CrossRef] [Green Version]
- Kline, C.E.; Chasens, E.R.; Bizhanova, Z.; Sereika, S.M.; Buysse, D.J.; Imes, C.C.; Kariuki, J.K.; Mendez, D.D.; Cajita, M.I.; Rathbun, S.L.; et al. The association between sleep health and weight change during a 12-month behavioral weight loss intervention. Int. J. Obes. 2021, 45, 639–649. [Google Scholar] [CrossRef]
- Ross, K.M.; Thomas, J.G.; Wing, R.R. Successful weight loss maintenance associated with morning chronotype and better sleep quality. J. Behav. Med. 2015, 39, 465–471. [Google Scholar] [CrossRef] [Green Version]
- Thomson, C.A.; Morrow, K.L.; Flatt, S.W.; Wertheim, B.C.; Perfect, M.M.; Ravia, J.J.; Sherwood, N.E.; Karanja, N.; Rock, C.L. Relationship Between Sleep Quality and Quantity and Weight Loss in Women Participating in a Weight-Loss Intervention Trial. Obesity 2012, 20, 1419–1425. [Google Scholar] [CrossRef] [PubMed]
- Pedrelli, P.; Nyer, M.; Yeung, A.; Zulauf, C.; Wilens, T. College Students: Mental Health Problems and Treatment Considerations. Acad. Psychiatry 2014, 39, 503–511. [Google Scholar] [CrossRef] [PubMed]






| Timepoint | COVID-19 Timeline | Corresponding Months & Cohort Academic Year | COVID-19 Status |
|---|---|---|---|
| Baseline (T0) | Prior to the onset of COVID-19 | September–December 2019, Year 1 Semester 1 | No restrictions in place |
| Timepoint 1 (T1) | The onset of COVID-19 | March–May 2020, Year 1 Semester 2 | Emergency transition to remote delivery |
| Timepoint (T2) | During COVID-19 | September–December 2020, Year 2 Semester 2 | Blended model with second transition to remote delivery in October |
| Timepoint (T3) | The time of data collection | April–June 2021 | Remote or blended model, dependent on the academic Dept./discipline |
| Thematic Area | Questionnaire Item | Adapted from (Where Relevant) | Questionnaire Item Structure |
|---|---|---|---|
| Demographic information | Gender/Age (self-reported in years) | ‘Male’, ‘Female’, ‘Prefer not to say’, ‘Other’/Continuous | |
| Academic grade achieved in semester 1 of year 2 (T2) | [15] | ‘Less than 40%’, ‘40–59%’, ‘60–69%’, ‘70% or above’, ‘Do not know’, ‘I would rather not provide this information’ and ‘Other’ | |
| Health-related behaviours | |||
| General Health | Overall general health rating (5-point Likert Scale) | ‘Very good’, ‘Good’, ‘Neither good nor poor’, ‘Poor’, ‘Very poor’ | |
| Physical Activity | Impact of COVID-19 on PA levels | ‘Yes’, ‘No’ | |
| Impact of COVID-19 on PA/sedentary levels, frequency and duration during (T0–T3) | ‘Increased’, ‘Decreased’, ‘Stayed the same’ | ||
| BMI | Self-reported body mass & height measurements/Perceived BMI category | Students could answer in imperial or metric values. Options available: ‘underweight’, ‘normal weight’, ‘overweight’ or ‘obese’ | |
| Change in body mass/Gained or lost body mass/Feelings towards body mass | Have you noticed a change in your body mass during COVID-19? ‘yes’, ‘no- I have stayed the same’, ‘do not know’, ‘gained body mass’, ‘lost body mass’, ‘stayed the same’/ ‘Very good’, ‘Good’, ‘Neither good nor poor’, ‘Poor’, ‘Very poor’ | ||
| Nutrition | Eleven newly devised lockdown dietary habits statements such as: ‘I have more time to prepare meals’, ‘I have more set mealtimes’, ‘I don’t eat as many takeaways’, ‘I sometimes eat because I am bored’ | Likert scale reporting level of agreement: ‘Strongly Agree’, ‘Agree’, ‘Neither Agree nor Disagree’, ‘Disagree’, ‘Strongly Disagree’, ‘Not Applicable’ | |
| Daily fruit & veg intake across timepoints | Self-reported sliding scale to indicate habitual daily portions (range 0–10) across timepoints T0–T3 | ||
| Alcohol | AUDIT-C scale | [23] | ‘How often do you have a drink containing alcohol?’ ‘How many units of alcohol do you drink on a typical day when you are drinking?’ ‘How often have you had 6 or more units if female, or 8 or more if male, on a single occasion in the last year?’ Scores are calculated using a scoring scale with answers equivalent to a number. Calculated score thresholds of 5 or more for females and 6 or more for males to constitute hazardous drinking (Davoren et al., 2015). |
| Impact of COVID-19 on drinking habits/did habits change during level-5 lockdowns | ‘Yes’, ‘No’ If yes: Did your drinking volumes and/or frequency Nominal: ‘Increased’, ‘Decreased’ | ||
| Sleep | Sleep quality across (T0–T3) (5-point Likert Scale) | ‘Very good’, ‘Good’, ‘Neither good nor poor’, ‘Poor’, ‘Very poor’, ‘I would rather not say’ | |
| Sleep duration at the time of data collection | [15] | ‘Less than 4 hours’, ‘4 h’, ‘5 h’, ‘6 h’, ‘7 h’, ‘8 h’, ‘9 h or more’ | |
| Changes in sleep duration across (T0–T3) | ‘More sleep’, ‘Less sleep’, ‘Stayed the same’, ‘I don’t know’ | ||
| Mental Well-being | |||
| Perceived mental well-being/WHO-5 | Personal rating of mental well-being (5-point Likert Scale) | [15] | ‘Very good’, ‘Good’, ‘Neither good nor poor’, ‘Poor’, ‘Very poor’, ‘I would rather not say’ |
| Current and/or past receipt of mental well-being supports | ‘Yes’, ‘No’, ‘I would rather not say’ | ||
| Source, type, and time period of support received | ‘Ongoing’, ‘Within the last month’, ‘Within the last 6 months’, ‘Within the last year’, ‘More than 1 year ago’ | ||
| WHO-5 well-being index | [24] | ||
| Academic Engagement | |||
| Educational experience & academic engagement | Experience when entering university, ‘socially’, ‘academically’/student’s ‘sense of belonging’ perceived university experience across timepoints: (T0-T3)/Rating of remote learning experience during applicable timepoints (T1, T2, T3)/‘Communication with lecturers’, ‘Using online learning management’, ‘Communication with classmates’, ‘Accessing supports’, ‘Attending online lectures/webinars’ | ‘Very good’, ‘Good’, ‘Neither good nor poor’, ‘Poor’, ‘Very poor’, ‘Not Applicable’ | |
| Daily technology use—weekday (Mon-Fri), weekend (Sat-Sun) | ‘Less than 1 h’, ‘1–3 h’, ‘3–5 h’, ‘5–7 h’, ‘7–9 h’, ‘9–11 h’, ‘More than 11 h’ | ||
| Total | Males | Females | Other * | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Age (years) | 18–20 | 149 | 56.0 | 42 | 55.3 | 104 | 56.2 | 3 | 60.0 |
| 21–23 | 70 | 26.3 | 21 | 27.6 | 48 | 25.9 | 1 | 20.0 | |
| 24+ | 47 | 17.7 | 13 | 17.1 | 33 | 17.8 | 1 | 20.0 | |
| Total | 266 | 76 | 185 | 5 | |||||
| Self-reported academic grade category Year 1 Semester 1 (pre-COVID) | Less than 40% | 3 | 1.1 | 1 | 1.3 | 2 | 1.1 | 0 | 0.0 |
| 40–59% | 33 | 12.4 | 15 | 19.7 | 17 | 9.2 | 1 | 20.0 | |
| 60–69% | 109 | 41.0 | 29 | 38.2 | 78 | 42.2 | 2 | 40.0 | |
| 70% or above | 90 | 33.8 | 22 | 29.0 | 67 | 36.2 | 1 | 20.0 | |
| Do not know | 25 | 9.4 | 7 | 9.2 | 18 | 9.7 | 0 | 0.0 | |
| I would rather not provide this information | 6 | 2.3 | 2 | 2.6 | 3 | 1.6 | 1 | 20.0 | |
| Total | 266 | 76 | 185 | 5 | |||||
| Lifestyle Factor | Category | Total | Males | Female | Other | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| In general, would you say your health is? | Good or very good | 193 | 72.6 | 58 | 76.3 | 131 | 70.8 | 4 | 80.0 |
| Higher-grade category | 142 | 71.4 | 37 | 72.5 | 102 | 70.3 | 3 | 100.0 | |
| Lower-grade category | 29 | 80.6 | 15 | 93.8 | 14 | 73.7 | 0 | 0.0 | |
| BMI Category | Overweight or obese | 96 | 40.5 | 23 | 32.9 | 71 | 43.8 | 2 | 40.0 |
| Higher-grade category | 75 | 42.9 | 17 | 36.9 | 57 | 45.3 | 1 | 33.3 | |
| Lower-grade category | 11 | 32.3 | 3 | 20.0 | 7 | 38.9 | 1 | 100.0 | |
| Have you noticed a change in your body mass during COVID-19? | Yes | 194 | 72.9 | 51 | 67.1 | 139 | 75.1 | 4 | 80.0 |
| Do you feel you have gained body mass? | 152 | 78.4 | 39 | 76.5 | 110 | 79.1 | 3 | 75.0 | |
| Higher-grade category | 114 | 80.9 | 27 | 81.8 | 86 | 81.8 | 1 | 50.0 | |
| Lower-grade category | 21 | 70.0 | 7 | 63.6 | 13 | 72.2 | 1 | 100.0 | |
| Generally, did you get more or less sleep during the stay-at-home periods? | More sleep | 111 | 41.7 | 29 | 38.2 | 80 | 43.2 | 2 | 40.0 |
| Higher-grade category | 83 | 41.7 | 19 | 37.3 | 64 | 44.1 | 0 | 0.0 | |
| Lower-grade category | 19 | 52.8 | 7 | 43.8 | 11 | 57.9 | 1 | 100 | |
| AUDIT-C Categorised Drinking Risk | Higher risk drinking: Score of 5+ for females, 6+ for males. | 107 | 48.9 | 39 | 63.9 | 65 | 42.2 | 3 | 75.0 |
| Higher-grade category | 76 | 46.9 | 26 | 34.2 | 48 | 63.2 | 2 | 66.7 | |
| Lower-grade category | 19 | 63.3 | 7 | 36.8 | 12 | 63.2 | 0 | 0.0 | |
| How would you rate your current mental well-being? | Good or very good | 112 | 42.1 | 38 | 50.0 | 73 | 39.5 | 1 | 20.0 |
| Higher-grade category | 92 | 46.2 | 29 | 56.9 | 62 | 42.8 | 1 | 33.3 | |
| Lower-grade category | 11 | 30.6 | 8 | 50.0 | 3 | 15.8 | 0 | 0.0 | |
| Can you estimate how long you spend on your phone in a typical day? | 5+ h | 101 | 38.0 | 24 | 31.5 | 77 | 41.6 | 0 | 0.0 |
| Higher-grade category | 79 | 39.7 | 16 | 27.1 | 60 | 41.4 | 0 | 0.0 | |
| Lower-grade category | 36 | 44.4 | 5 | 31.3 | 11 | 57.9 | 1 | 100.0 | |
| Independent Variable | B | Sig | OR | 95% CI− | 95% CI+ |
|---|---|---|---|---|---|
| Gender Female Male | −0.07 | 0.90 | 1.00 0.94 | 0.33 | 2.64 |
| Age group 18–20 21–23 ≥24 | −0.22 2.09 | 0.12 | 1.00 0.81 8.10 | 0.26 1.83 | 2.54 35.84 |
| Feelings about body mass Good/very good Neither good nor poor Poor/very poor | −1.00 1.59 | 0.00 | 1.00 0.367 4.88 | 0.11 1.15 | 1.22 20.68 |
| Perceived BMI Category Underweight/normal weight Overweight/Obese | 1.74 | 0.03 | 1.00 5.73 | 1.25 | 26.21 |
| Dietary Statement ‘I sometimes eat because I am bored’ Strongly agree Agree Neither agree nor disagree Strongly disagree/disagree | −1.50 −2.04 −3.75 | 0.00 | 1.00 0.22 0.13 0.02 | 0.07 0.02 0.00 | 0.74 0.83 0.16 |
| Changes in sleep during stay-at-home period Stayed the same or don’t know More sleep Less sleep | 1.86 0.97 | 0.01 | 1.00 6.43 2.63 | 1.97 0.61 | 20.99 11.39 |
| Sleep quality during stay-at-home period Good/very good Neither good nor poor Poor/very poor | −0.23 −1.49 | 0.08 | 1.00 0.80 0.23 | 0.21 0.06 | 3.05 0.85 |
| Constant | 1.25 | 0.43 | 3.49 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheedy O’Sullivan, E.; McCarthy, K.-M.; O’Neill, C.; Walton, J.; Bolger, L.; Bickerdike, A. The Impact of COVID-19 on the Health-Related Behaviours, Mental Well-Being, and Academic Engagement of a Cohort of Undergraduate Students in an Irish University Setting. Int. J. Environ. Res. Public Health 2022, 19, 16096. https://doi.org/10.3390/ijerph192316096
Sheedy O’Sullivan E, McCarthy K-M, O’Neill C, Walton J, Bolger L, Bickerdike A. The Impact of COVID-19 on the Health-Related Behaviours, Mental Well-Being, and Academic Engagement of a Cohort of Undergraduate Students in an Irish University Setting. International Journal of Environmental Research and Public Health. 2022; 19(23):16096. https://doi.org/10.3390/ijerph192316096
Chicago/Turabian StyleSheedy O’Sullivan, Elaine, Karrie-Marie McCarthy, Cian O’Neill, Janette Walton, Lisa Bolger, and Andrea Bickerdike. 2022. "The Impact of COVID-19 on the Health-Related Behaviours, Mental Well-Being, and Academic Engagement of a Cohort of Undergraduate Students in an Irish University Setting" International Journal of Environmental Research and Public Health 19, no. 23: 16096. https://doi.org/10.3390/ijerph192316096






