Evaluation of Complexity Measurement Tools for Correlations with Health-Related Outcomes, Health Care Costs and Impacts on Healthcare Providers: A Scoping Review
Abstract
:1. Introduction
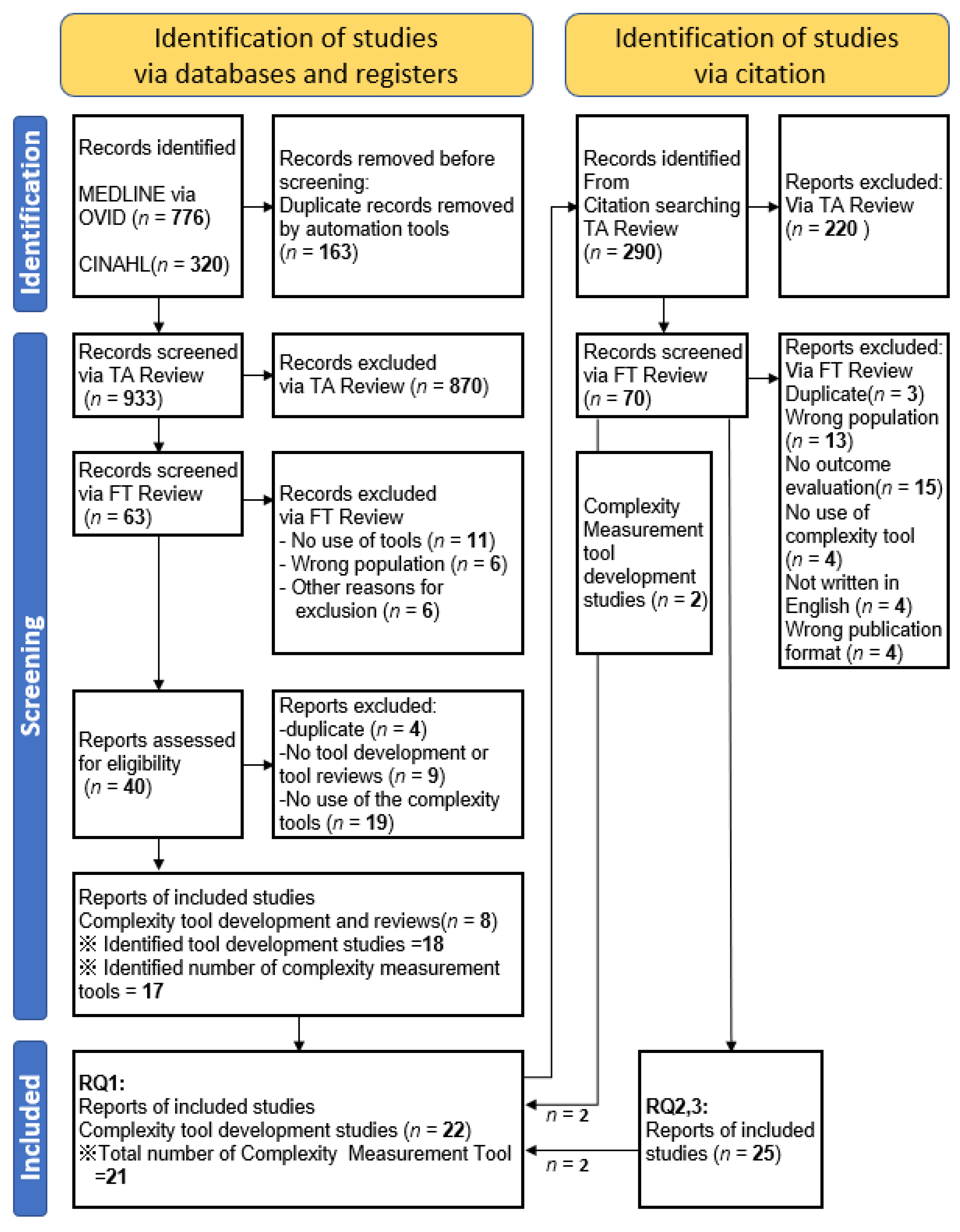
2. Materials and Methods
2.1. Stage 1: Identifying the Research Question
RQ1. What tools to assess patient complexity are available for the general populations or patients?
RQ2. To what extent do health related patient outcomes differ according to the magnitude of the measured indicators?
RQ3. To what extent does the impact on healthcare providers/systems (e.g., healthcare costs, administrative costs, medical staff burnout) differ depending on the magnitude of the measured indicators?
2.2. Stage 2: Identifying Relevant Studies
2.2.1. Participants
2.2.2. Concept
2.2.3. Context
2.3. Stage 3: Study Selection
2.4. Stage 4: Charting the Data
2.5. Stage 5: Collating, Summarizing and Reporting the Results
2.6. Differences between Protocol and Review
3. Results
3.1. Patient Complexity Measurement Tools Used with the General Adult Population or Patients
3.2. Correlations between Patient Complexity and Patients’ Health Related Outcomes
3.3. Correlations between Patient Complexity and Impacts on Healthcare Providers/Systems
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Constitution of the World Health Organization. Chron. World Health Organ. 1947, 1, 29–43. [Google Scholar]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M. The health gap: The challenge of an unequal world. Lancet 2015, 386, 2442–2444. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.B. Managing complexity in chronic care: An overview of the VA state-of-the-art (SOTA) conference. J. Gen. Intern. Med. 2007, 22 (Suppl. 3), 374–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grembowski, D.; Schaefer, J.; Johnson, K.E.; Fischer, H.; Moore, S.L.; Tai-Seale, M.; Ricciardi, R.; Fraser, J.R.; Miller, D.; LeRoy, L. A conceptual model of the role of complexity in the care of patients with multiple chronic conditions. Med. Care 2014, 52 (Suppl. 3), S7–S14. [Google Scholar] [CrossRef]
- Loeb, D.F.; Binswanger, I.A.; Candrian, C.; Bayliss, E.A. Primary care physician insights into a typology of the complex patient in primary care. Ann. Fam. Med. 2015, 13, 451–455. [Google Scholar] [CrossRef] [Green Version]
- Grant, R.W.; Ashburner, J.M.; Hong, C.S.; Chang, Y.; Barry, M.J.; Atlas, S.J. Defining patient complexity from the primary care physician’s perspective: A cohort study. Ann. Fam. Med. 2011, 155, 797–804. [Google Scholar] [CrossRef]
- Schaink, A.K.; Kuluski, K.; Lyons, R.F.; Fortin, M.; Jadad, A.R.; Upshur, R.; Wodchis, W.P. A scoping review and thematic classification of patient complexity: Offering a unifying framework. J. Comorbidity 2012, 2, 1–9. [Google Scholar] [CrossRef]
- Martin, C.M.; Sturmberg, J.P. General practice—Chaos, complexity and innovation. Med. J. Aust. 2005, 183, 106–109. [Google Scholar] [CrossRef]
- Safford, M.M.; Allison, J.J.; Kiefe, C.I. Patient complexity: More than comorbidity. the vector model of complexity. J. Gen. Intern. Med. 2007, 22 (Suppl. 3), 382–390. [Google Scholar] [CrossRef] [Green Version]
- Nicolaus, S.; Crelier, B.; Donzé, J.D.; Aubert, C.E. Definition of patient complexity in adults: A narrative review. J. Multimorb. Comorbidity 2022, 12, 263355652210812. [Google Scholar] [CrossRef] [PubMed]
- Hawker, K.; Barnabe, C.; Barber, C.E.H. A scoping Review of tools used to assess patient Complexity in rheumatic disease. Health Expect 2021, 24, 556–565. [Google Scholar] [CrossRef] [PubMed]
- Marcoux, V.; Chouinard, M.-C.; Diadiou, F.; Dufour, I.; Hudon, C. Screening tools to identify patients with complex health needs at risk of high use of health care services: A scoping review. PLoS ONE 2017, 12, e0188663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Etz, R.; Miller, W.L.; Stange, K.C. Simple Rules That Guide Generalist and Specialist Care. Fam. Med. 2021, 53, 697–700. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid.-Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [Green Version]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- Haddaway, N.R.; Grainger, M.J.; Gray, C.T. citationchaser: A tool for transparent and efficient forward and backward citation chasing in systematic searching. Res. Synth. Methods 2022, 13, 533–545. [Google Scholar] [CrossRef]
- De Jonge, P.; Huyse, F.J.; Stiefel, F.C.; Slaets, J.P.J.; Gans RO, B. INTERMED—A clinical instrument for biopsychosocial assessment. Psychosomatics 2001, 42, 106–109. [Google Scholar] [CrossRef]
- De Jonge, P.; Bauer, I.; Huyse, F.J.; Latou, C.H.M. Medical inpatients at risk of extended hospital stay and poor discharge health status: Detection with COMPRI and INTERMED. Psychosom. Med. 2003, 65, 534–541. [Google Scholar] [CrossRef]
- De Jonge, P.; Latour, C.H.M.; Huyse, F.J. Implementing psychiatric interventions on a medical ward: Effects on patients’ quality of life and length of hospital stay. Psychosom. Med. 2003, 65, 997–1002. [Google Scholar] [CrossRef] [PubMed]
- Lobo, E.; Ventura, T.; Navio, M.; Santabárbara, J.; Kathol, R.; Samaniego, E.; Marco, C.; Lobo, A. Identification of components of health complexity on internal medicine units by means of the INTERMED method. Int. J. Clin. Pract. 2015, 69, 1377–1386. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, C.A.; Weber, B.; Santos, J.L.F.d.; Zucoloto, M.L.; de Camargo, L.L.; Zanetti, A.C.G.; Rzewuska, M.; de Azevedo-Marques, J.M. Health complexity assessment in primary care: A validity and feasibility study of the INTERMED tool. PLoS ONE 2022, 17, e0263702. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, H.S.; Gutierrez, B.A.O. Care complexity in hospitalized elderly according to cognitive performance. Rev. Bras. Enferm. 2019, 72, 134–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wild, B.; Heider, D.; Maatouk, I.; Slaets, J.; König, H.; Niehoff, D.; Saum, K.; Brenner, H.; Söllner, W.; Herzog, W. Significance and costs of complex biopsychosocial health care needs in elderly people: Results of a population-based study. Psychosom. Med. 2014, 76, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Boehlen, F.H.; Herzog, W.; Schellberg, D.; Maatouk, I.; Saum, K.-U.; Brenner, H.; Wild, B. Self-perceived coping resources of middle-aged and older adults—Results of a large population-based study. Aging Ment. Health 2016, 21, 1303–1309. [Google Scholar] [CrossRef] [PubMed]
- Uittenbroek, R.J.; Van Asselt, A.D.I.; Spoorenberg, S.L.W.; Kremer, H.P.H.; Wynia, K.; Reijneveld, S. Integrated and Person-Centered Care for Community-Living Older Adults: A Cost-Effectiveness Study. Health Serv. Res. 2018, 53, 3471–3494. [Google Scholar] [CrossRef]
- Peters, L.L.; Burgerhof, J.G.; Boter, H.; Wild, B.; Buskens, E.; Slaets, J.P. Predictive validity of a frailty measure (GFI) and a case complexity measure (IM-E-SA) on healthcare costs in an elderly population. J. Psychosom. Res. 2015, 79, 404–411. [Google Scholar] [CrossRef]
- Bakker, M.H.; Vissink, A.; Spoorenberg, S.L.W.; Wynia, K.; Visser, A. Self-reported oral health problems and the ability to organize dental care of community-dwelling elderly aged ≥75 years. BMC Oral Health 2020, 20, 185. [Google Scholar] [CrossRef]
- Hoeksema, A.R.; Spoorenberg, S.; Peters, L.; Meijer, H.; Raghoebar, G.; Vissink, A.; Wynia, K.; Visser, A. Elderly with remaining teeth report less frailty and better quality of life than edentulous elderly: A cross-sectional study. Oral Dis. 2017, 23, 526–536. [Google Scholar] [CrossRef]
- Spoorenberg, S.L.; Reijneveld, S.A.; Uittenbroek, R.J.; Kremer, H.P.; Wynia, K. Health-Related Problems and Changes After 1 Year as Assessed With the Geriatric ICF Core Set (GeriatrICS) in Community-Living Older Adults Who Are Frail Receiving Person-Centered and Integrated Care From Embrace. Arch. Phys. Med. Rehabil. 2019, 100, 2334–2345. [Google Scholar] [CrossRef] [PubMed]
- Peters, L.L.; Boter, H.; Slaets, J.P.; Buskens, E. Development and measurement properties of the self assessment version of the INTERMED for the elderly to assess case complexity. J. Psychosom. Res. 2013, 74, 518–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dortland, A.; Peters, L.L.; Boenink, A.D.; Smit, J.H.; Slaets, J.P.; Hoogendoorn, A.W.; Joos, A.; Latour, C.H.; Stiefel, F.; Burrus, C.; et al. Assessment of Biopsychosocial Complexity and Health Care Needs: Measurement Properties of the INTERMED Self-Assessment Version. Psychosom. Med. 2017, 79, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Bakker, M.H.; Vissink, A.; Spoorenberg, S.L.; Jager-Wittenaar, H.; Wynia, K.; Visser, A. Are Edentulousness, Oral Health Problems and Poor Health-Related Quality of Life Associated with Malnutrition in Community-Dwelling Elderly (Aged 75 Years and Over)? A Cross-Sectional Study. Nutrients 2018, 10, 1965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spoorenberg, S.L.W.; Wynia, K.; Uittenbroek, R.J.; Kremer, H.P.H.; Reijneveld, S. Effects of a population-based, person-centred and integrated care service on health, wellbeing and self-management of community-living older adults: A randomised controlled trial on Embrace. PLoS ONE 2018, 13, e0190751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yokokawa, D.; Shikino, K.; Kishi, Y.; Ban, T.; Miyahara, S.; Ohira, Y.; Yanagita, Y.; Yamauchi, Y.; Hayashi, Y.; Ishizuka, K.; et al. Does scoring patient complexity using COMPRI predict the length of hospital stay? A multicentre case–control study in Japan. BMJ Open 2022, 12, e051891. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, S.; Matsushima, M.; Wakabayashi, H.; Mutai, R.; Murayama, S.; Hayashi, T.; Ichikawa, H.; Nakano, Y.; Watanabe, T.; Fujinuma, Y. Validity and reliability of the Patient Centred Assessment Method for patient complexity and relationship with hospital length of stay: A prospective cohort study. BMJ Open 2017, 7, e016175. [Google Scholar] [CrossRef] [Green Version]
- Hewner, S.; Casucci, S.; Sullivan, S.; Mistretta, F.; Xue, Y.; Johnson, B.; Pratt, R.; Lin, L.; Fox, C. Integrating Social Determinants of Health into Primary Care Clinical and Informational Workflow during Care Transitions. EGEMS 2017, 5, 2. [Google Scholar] [CrossRef] [Green Version]
- Yoshida, S.; Matsushima, M.; Wakabayashi, H.; Mutai, R.; Sugiyama, Y.; Yodoshi, T.; Horiguchi, R.; Watanabe, T.; Fujinuma, Y. Correlation of patient complexity with the burden for health-rel ated professions, and differences in the burden between the professions at a Japanese regional hospital: A prospective cohort study. BMJ Open 2019, 9, e025176. [Google Scholar] [CrossRef] [Green Version]
- Sugiyama, Y.; Matsushima, M.; Yoshimoto, H. Association between alcohol consumption/alcohol use disorders and patient complexity: A cross-sectional study. BMJ Open 2020, 10, e034665. [Google Scholar] [CrossRef]
- Hawner, S.; Seo, J.Y.; Gothard, S.E.; Johnson, B.J. Aligning population-based care management with chronic disease complexity. Nurs. Outlook 2014, 62, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Boutin-Foster, C.; Euster, S.; Rolon, Y.; Motal, A.; BeLue, R.; Kline, R.; Charlson, M.E. Social Work Admission Assessment Tool for Identifying Patients in Need of Comprehensive Social Work Evaluation. Health Soc. Work 2005, 30, 117–125. [Google Scholar] [CrossRef]
- Bandini, F.; Guidi, S.; Blaszczyk, S.; Fumarulo, A.; Pierini, M.; Pratesi, P.; Spolveri, S.; Padeletti, M.; Petrone, P.; Zoppi, P.; et al. Complexity in internal medicine wards: A novel screening method and implications for management. J. Eval. Clin. Pract. 2017, 24, 285–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huyse, F.J.; Lyons, J.S.; Stiefel, F.C.; Slaets, J.P.; de Jonge, P.; Fink, P.; Gans, R.O.; Guex, P.; Herzog, T.; Lobo, A.; et al. “INTERMED”: A method to assess health service needs. I. Development and reliability. Gen. Hosp. Psychiatry 1999, 21, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Stiefel, F.C.; de Jonge, P.; Huyse, F.J.; Guex, P.; Slaets, J.P.; Lyons, J.S.; Spagnoli, J.; Vannotti, M. “INTERMED”: A method to assess health service needs. II. Results on its validity and clinical use. Gen. Hosp. Psychiatry 1999, 21, 49–56. [Google Scholar] [CrossRef]
- Wild, B.; Lechner, S.; Herzog, W.; Maatouk, I.; Wesche, D.; Raum, E.; Müller, H.; Brenner, H.; Slaets, J.; Huyse, F.; et al. Reliable integrative assessment of health care needs in elderly persons: The INTERMED for the Elderly (IM-E). J. Psychosom. Res. 2010, 70, 169–178. [Google Scholar] [CrossRef]
- Huyse, F.J.; de Jonge, P.; Slaets, J.P.; Herzog, T.; Lobo, A.; Lyons, J.S.; Opmeer, B.C.; Stein, B.; Arolt, V.; Balogh, N.; et al. COMPRI—An Instrument to Detect Patients With Complex Care Needs: Results From a European Study. J. Psychosom. Res. 2001, 42, 222–228. [Google Scholar] [CrossRef]
- Pratt, R.; Hibberd, C.; Cameron, I.M.; Maxwell, M. The Patient Centered Assessment Method (PCAM): Integrating the Social Dimensions of Health into Primary Care. J. Comorbidity 2015, 5, 110–119. [Google Scholar] [CrossRef]
- Hewner, S.; Wu, Y.W.B.; Castner, J. Comparative Effectiveness of Risk-Stratified Care Management in Reducing Readmissions in Medicaid Adults With Chronic Disease. J. Healthc. Qual. 2016, 38, 3–16. [Google Scholar]
- Hudon, C.; Bisson, M.; Dubois, M.-F.; Chiu, Y.; Chouinard, M.-C.; Dubuc, N.; Elazhary, N.; Sabourin, V.; Vanasse, A. CONECT-6: A case-finding tool to identify patients with complex health needs. BMC Health Serv. Res. 2021, 21, 157. [Google Scholar]
- McDonough, R.P.; McDonough, A.; Doucette, W.R. Use of medication regimen complexity to target services in the community. J. Am. Pharm. Assoc. JAPhA 2021, 62, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Roberson, D.; Connell, M.; Dillis, S.; Gauvreau, K.; Gore, R.; Heagerty, E.; Jenkins, K.; Ma, L.; Maurer, A.; Stephenson, J.; et al. Cognitive Complexity of the Medical Record Is a Risk Factor for Major Adverse Events. Perm. J. 2014, 18, 4–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Groningen, N.V.; Prasad, P.A.; Najafi, N.; Rajkomar, A.; Khanna, R.R.; Fang, M.C. Electronic Order Volume as a Meaningful Component in Estimating Patient Complexity and Resident Physician Workload. J. Hosp. Med. 2018, 13, 829–835. [Google Scholar] [CrossRef]
- Liechti, F.D.; Beck, T.; Ruetsche, A.; Roumet, M.C.; Limacher, A.; Tritschler, T.; Donzé, J.D. Development and validation of a score to assess complexity of general internal medicine patients at hospital discharge: A prospective cohort study. BMJ Open 2021, 11, e041205. [Google Scholar] [CrossRef]
- Mehra, T.; Müller, C.T.B.; Volbracht, J.; Seifert, B.; Moos, R. Predictors of High Profit and High Deficit Outliers under SwissDRG of a Tertiary Care Center. PLoS ONE 2015, 10, e0140874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonizzoni, E.; Gussoni, G.; Agnelli, G.; Incalzi, R.A.; Bonfanti, M.; Mastroianni, F.; Candela, M.; Franchi, C.; Frasson, S.; Greco, A.; et al. The complexity of patients hospitalized in Internal Medicine wards evaluated by FADOI-COMPLIMED score(s). A hypothetical approach. PLoS ONE 2018, 13, e0195805. [Google Scholar] [CrossRef] [Green Version]
- Mount, J.K.; Massanari, R.M.; Teachman, J. Patient care complexity as perceived by primary care physicians. Fam. Syst. Health J. Collab. Fam. Healthc. 2015, 33, 137–145. [Google Scholar] [CrossRef]
- Maxwell, M.; Hibberd, C.; Pratt, R.; Cameron, I.; Mercer, S. Development and Initial Validation of the Minnesota Edinburgh Complexity Assessment Method (MECAM) for Use Within the Keep Well Health Check; NHS Health Scotland: Edinburgh, UK, 2011. [Google Scholar]
- Troigros, O.; Béjot, Y.; Rodriguez, P.M.; Shoaib, F.; Ellis, H.; Wade, D. Measuring complexity in neurological rehabilitation: The Oxford Case Complexity Assessment Measure (OCCAM). Clin. Rehabil. 2013, 28, 499–507. [Google Scholar] [CrossRef]
- Corazza, G.R.; Panel, F.T.C.; Klersy, C.; Formagnana, P.; Lenti, M.V.; Padula, D. A consensus for the development of a vector model to assess clinical complexity. Intern. Emerg. Med. 2017, 12, 1313–1318. [Google Scholar] [CrossRef]
- Salisbury, C.; Lay-Flurrie, S.; Bankhead, C.R.; Fuller, A.; Murphy, M.; Caddick, B.; Ordóñez-Mena, J.M.; Holt, T.; Nicholson, B.D.; Perera, R.; et al. Measuring the complexity of general practice consultations: A Delphi and cross-sectional study in English primary care. Br. J. Gen. Pract. 2020, 71, e423–e431. [Google Scholar] [CrossRef]
| Tool | Author (Year) | Study Design | Setting | n | Location | Outcome Measurement |
|---|---|---|---|---|---|---|
| INTERMED | Jonge (2001) [19] | Cohort study | Consecutively admitted patients on a general internal medicine ward | 89 | Netherlands |
|
| Jonge (2003) [20] | Cohort study | Patients from admission to discharge | 275 | Netherlands |
| |
| Jonge (2003) [21] | Interventional study | Inpatients | 193 | Netherlands |
| |
| Lobo (2015) [22] | Cohort study | Internal medicine inpatients | 626 | Spain |
| |
| C.A. Oliveira [23] | Cohort study | All adults who arrived at the reception of one of the health services | 230 | Brazil |
| |
| H.S. da Silva [24] | Cross sectional and analytical study | Inpatient | 382 | Brazil |
| |
| INTERMED for Elderly | B. Wild (2014) [25] | Cohort Study | General health check-up people | 3121 | Germany |
|
| F.H. Boehlen (2017) [26] | Cohort Study | Health check-up patients | 9949 | Germany |
| |
| R.J. Uittenbroek (2018) [27] | RCT | All adults aged 75 and older, listed with these GP | 1456 | Netherlands |
| |
| IM-E-SA | L.L. Peters (2015) [28] | Population-based cohort | General population | 713 | Netherlands | Healthcare costs |
| M.H. Bakker (2020) [29] | Cohort Study | Community-dwelling elderly | 89 | Netherlands | Oral status and oral health | |
| A.R. Hoeksema (2017) [30] | Crosssectional descriptive study | Community-dwelling elderly | 1026 | Netherlands | Oral status and oral health | |
| R.J. Uittenbroek (2018) [27] | RCT | All adults aged 75 and older, listed with GPs | 1456 | Netherlands |
| |
| S.L. Spoorenberg (2019) [31] | RCT | Community (follow-up) | 136 | Netherlands | Geriatric ICF (International Classification of Functioning) Core Set
| |
| L.L. Peters (2013) [32] | Cross-sectional study | General population | 338 | Netherlands |
| |
| Dortland (2017) [33] | Cohort study | Inpatients and outpatients | 850 | Germany France Italy Netherlands Switzerland |
| |
| M.H. Bakker (2018) [34] | Cross sectional observational study | Community-living elderly | 1325 | Netherlands |
| |
| S.L. Spoorenberg (2018) [35] | RCT | Inpatients and outpatients | 850 | Germany France Italy Netherlands Switzerland |
| |
| COMPRI | Jonge (2003) [20] | Cohort study | Patients from admission to discharge | 275 | Netherlands |
|
| Jonge (2003) [21] | Interventional study | Inpatients | 193 | Netherlands |
| |
| D. Yokokawa (2022) [36] | Case control study | Newly hospitalised patients | 33 | Japan | Length of hospital stays | |
| PCAM | S. Yoshida (2017) [37] | Prospective cohort study | Inpatient | 201 | Japan | Length of hospital stays |
| Hewner (2017) [38] | Interventional study | Patients who were discharged to the community | 419 | USA |
| |
| S. Yoshida (2018) [39] | Cohort study | All inpatients admitted to the acute care unit of Hospital | 201 | Japan | Burden for health-related staff | |
| Y. Sugiyama (2020) [40] | Cross-sectional study | Outpatient practices | 426 | Japan | Alcohol misuse | |
| COMPLEXedex | S. Hawner (2014) [41] | Before-and-after study | Regional health plan in 2009 | 411,407 | USA | Hospital inpatient utilization |
| SWAAT | Boutin-Foster (2005) [42] | Cohort | Newly hospitalised patients | 299 | USA |
|
| Bandini’s tool | Bandini (2018) [43] | Observational study | Inpatients | 240 | Italy |
|
| Complexity Tool | Full Name of Tool | Intended Use of the Tool | Applied Setting | Format of the Tool |
|---|---|---|---|---|
| IM [44,45] | INTERMED | Indication for multidisciplinary care | Inpatients | Face to face interview |
| IMSA Dortland | INTERMED Self-Assessment | Self-assessment version of IM | Inpatients | Self-assessment |
| IM-E [46] | INTERMED for the Elderly | Elderly version of IM | Inpatients, outpatients, community dwelling people | Face to face interview |
| IM-E-SA [32] | INTERMED for the Elderly Self-Assessment | Self-assessment version of IM-E | Inpatients, outpatients, community dwelling people | Self-assessment |
| COMPRI [47] | Complexity Prediction Instrument | Indication for multidimensional assessment and interdisciplinary care coordination | Inpatients | Face to face interview |
| PCAM [48] | Patient Centered Assessment Method | Identify biopsychosocial complexities; make appropriate referrals | Inpatient, Outpatient | Face to face interview |
| COMPLEXedex [49] | Rank individuals with multiple chronic diseases hierarchically into segments | Inpatients, Community dwelling people | Calculated using the amount of data in the medical records | |
| CONECT-6 [50] | COmplex NEeds Case-finding Tool-6 | Identify patients with chronic conditions and complex health needs in emergency Departments | Emergency departments | Self-assessment |
| IMECSs [51] | Iowa Medication Complexity Scores | Describe challenges a patient faces in developing medication regimen | Outpatients | Calculated automatically in real time using clinical documentation system |
| CCMR [52] | Cognitive complexity of the medical record | Use CCMR as a useful surrogate for true patient complexity | Inpatients | Calculated using the amount of data in the medical records |
| Electric order volume [53] | Use electronic order volume a useful surrogate for the workload of residents | Inpatients | Calculated using the data in the medical records | |
| PCA [54] | Patient Complexity Assessment score | Use readily available administrative and clinic data to identify complex inpatients | Inpatients | Calculated using the data in the medical records |
| PCCL [55] | Patient clinical complexity level | Indicate a calculated index of disease burden per patient based on the amount and constellation of secondary diagnoses | Inpatients | Calculated using the data in the medical records |
| FADOI-Complimed [56] | Federation of Associations of Hospital Doctors on Internal Medicine Complimed | Describe the complexity of hospitalized patients as a two-dimensional phenomenon | Inpatients | Face to face interview |
| MCAM [57] | Minnesota Complexity Assessment Method | Identify factors interfering with care; formulate new care plan | Outpatients | Face to face interview |
| MECAM [58] | Minnesota Edinburgh Complexity Assessment Method | Identify factors posing risk to patient well-being | Outpatients | Face to face interview |
| OCCAM [59] | Oxford Case Complexity Assessment Method | Identify factors interfering with care; facilitate care coordination | Inpatients | Face to face interview |
| Corazza’s score [60] | Comprehensive assessment of clinical complexity in which an overall index results from the sum of each vector/domain | Outpatients | Face to face interview | |
| Salisbury’s score [61] | Develop a valid and reliable measure of the complexity of general practice consultations | Outpatients | Face to face interview | |
| SWAAT [42] | Social Work Admission Assessment Tool | SWAAT was developed to identify patients who have complicated discharge planning needs and require early social work evaluation. | Inpatients | Face to face interview |
| Bandini’s tool [43] | To identify patients with clinically complex hospitalization events | Inpatients | Extracted data from the hospital medical records |
| Complexity Measurement Tools | ||||||||
|---|---|---|---|---|---|---|---|---|
| INTERMED | INTERMED for Elderly | IM-E-SA | COMPRI | PCAM | COMPLEXedex | SWAAT | Bandini’s Tool | |
| Patient outcomes | 6 [19,20,21,22,23,24] | 3 [25,26,27] | 8 [27,29,30,31,32,33,34,35] | 3 [20,21,36] | 3 [37,38,40] | 1 [41] | 1 [42] | 1 [43] |
| Health care costs | 1 [25] | 1 [28] | ||||||
| Impacts on health care providers | 1 [39] | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaneko, H.; Hanamoto, A.; Yamamoto-Kataoka, S.; Kataoka, Y.; Aoki, T.; Shirai, K.; Iso, H. Evaluation of Complexity Measurement Tools for Correlations with Health-Related Outcomes, Health Care Costs and Impacts on Healthcare Providers: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 16113. https://doi.org/10.3390/ijerph192316113
Kaneko H, Hanamoto A, Yamamoto-Kataoka S, Kataoka Y, Aoki T, Shirai K, Iso H. Evaluation of Complexity Measurement Tools for Correlations with Health-Related Outcomes, Health Care Costs and Impacts on Healthcare Providers: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(23):16113. https://doi.org/10.3390/ijerph192316113
Chicago/Turabian StyleKaneko, Hiromitsu, Akiko Hanamoto, Sachiko Yamamoto-Kataoka, Yuki Kataoka, Takuya Aoki, Kokoro Shirai, and Hiroyasu Iso. 2022. "Evaluation of Complexity Measurement Tools for Correlations with Health-Related Outcomes, Health Care Costs and Impacts on Healthcare Providers: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 23: 16113. https://doi.org/10.3390/ijerph192316113






