Awareness and Attitude of Physicians on the Role of Dentists in the Management of Obstructive Sleep Apnea
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Design
2.3. Study Population and Sampling Technique
2.4. Data Collection Methods
- (1)
- Demographic data such as: gender, age, specialty, and years of experience;
- (2)
- Knowledge about OSA and the role of dentists. Using 29 factual statements to be responded by “True, False, or I don’t know” responses, data was collected about the physicians’ knowledge on the followings: (a) General knowledge of craniofacial factors that may cause or aggravate obstructive breathing disorders and general OSA management (statements # 1 to 12), and (b) Specific knowledge about the role of different dental specialties in the management of OSA: orthodontics, oromaxillofacial surgery, and general dentistry (statements # 13 to 29). A scoring system was applied to assess the level of knowledge of each subject: 1 point was given for each correct answer, and 0 points were given for each incorrect or an ‘I don’t know’ answer. Total and percentage mean scores (PMS) were calculated. Participants were grouped into three categories according to their levels of knowledge: poor (<50% PMS), average (50–75% PMS), and good (>75% PMS);
- (3)
- Attitude towards the role of dentists in OSA. Using 12 attitude statements to be responded by a Likert scale of “Never, Rarely, Sometimes, Usually, Always” responses, data was collected on the attitude towards the recognition of craniofacial deformities that may contribute to OSA and their referral response. A scoring system was applied using the Likert 5-point scale; 5 points were assigned to “Always,” and 1 point was assigned to “Never.” Negative attitude statements were scored from 1 (for those who selected always) to 5 (for those who selected never). Total attitude score and PMS were calculated, and participants were grouped into three categories according to their PMS as follows: positive attitude (>75% PMS), neutral attitude (50–75% PMS), and negative attitude (<50% PMS).
2.5. Data Analysis
2.6. Ethical Considerations
3. Results
3.1. Participant Demographic Characteristics
3.2. Knowledge Assessment
3.3. Attitude Assessment
3.4. Predictors of Knowledge and Attitude
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OSA | Obstructive Sleep Apnea |
| PMS | percentage mean score |
| PAP | positive air pressure |
| AHI | apnea-hypopnea index |
| KAMC | King Abdulaziz Medical city |
| MNGHA | Ministry of National Guard-Health Affairs |
| KAIMRC | King Abdullah International Medical Research Center |
| IRB | Institutional Review Board |
References
- Young, T.; Palta, M.; Dempsey, J.; Peppard, P.E.; Nieto, F.J.; Hla, K.M. Burden of sleep apnea: Rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ 2009, 108, 246–249. [Google Scholar]
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef] [PubMed]
- BaHammam, A.S.; Alrajeh, M.S.; Al-Jahdali, H.H.; BinSaeed, A.A. Prevalence of symptoms and risk of sleep apnea in middle-aged Saudi males in primary care. Saudi Med. J. 2008, 29, 423–426. [Google Scholar] [PubMed]
- Bahammam, A.S.; Al-Rajeh, M.S.; Al-Ibrahim, F.S.; Arafah, M.A.; Sharif, M.M. Prevalence of symptoms and risk of sleep apnea in middle-aged Saudi women in primary care. Saudi Med. J. 2009, 30, 1572–1576. [Google Scholar]
- Wali, S.O.; Abalkhail, B.; Krayem, A. Prevalence and risk factors of obstructive sleep apnea syndrome in a Saudi Arabian population. Ann. Thorac. Med. 2017, 12, 88–94. [Google Scholar] [CrossRef]
- Finkel, K.J.; Searleman, A.C.; Tymkew, H.; Tanaka, C.Y.; Saager, L.; Safer-Zadeh, E.; Bottros, M.; Selvidge, J.A.; Jacobsohn, E.; Pulley, D.; et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009, 10, 753–758. [Google Scholar] [CrossRef]
- McNicholas, W.T.; Bonsigore, M.R.; Bonsignore, M.R.; Management Committee of EU COST ACTION B26. Sleep apnoea as an independent risk factor for cardiovascular disease: Current evidence, basic mechanisms and research priorities. Eur. Respir. J. 2007, 29, 156–178. [Google Scholar] [CrossRef]
- Sakakibara, H.; Tong, M.; Matsushita, K.; Hirata, M.; Konishi, Y.; Suetsugu, S. Cephalometric abnormalities in non-obese and obese patients with obstructive sleep apnoea. Eur. Respir. J. 1999, 13, 403–410. [Google Scholar] [CrossRef]
- Bertuzzi, F.; Santagostini, A.; Pollis, M.; Meola, F.; Segù, M. The Interaction of Craniofacial Morphology and Body Mass Index in Obstructive Sleep Apnea. Dent. J. 2022, 10, 136. [Google Scholar] [CrossRef]
- Favero, L.; Arreghini, A.; Cocilovo, F.; Favero, V. Respiratory disorders in paediatric age: Orthodontic diagnosis and treatment in dysmetabolic obese children and allergic slim children. Eur. J. Paediatr. Dent. 2013, 14, 190–194. [Google Scholar] [PubMed]
- Huynh, N.T.; Desplats, E.; Almeida, F.R. Orthodontics treatments for managing obstructive sleep apnea syndrome in children: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Fastuca, R.; Meneghel, M.; Zecca, P.A.; Mangano, F.; Antonello, M.; Nucera, R.; Caprioglio, A. Multimodal airway evaluation in growing patients after rapid maxillary expansion. Eur. J. Paediatr. Dent. 2015, 16, 129–134. [Google Scholar]
- Zaghi, S.; Holty, J.-E.C.; Certal, V.; Abdullatif, J.; Guilleminault, C.; Powell, N.B.; Riley, R.W.; Camacho, M. Maxillomandibular Advancement for Treatment of Obstructive Sleep Apnea: A Meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, K.; Phillips, C.L.; Cistulli, P.A. Efficacy versus Effectiveness in the Treatment of Obstructive Sleep Apnea: CPAP and Oral Appliances. J. Dent. Sleep Med. 2015, 2, 175–181. [Google Scholar] [CrossRef]
- Pavwoski, P.; Shelgikar, A.V. Treatment options for obstructive sleep apnea. Neurol. Clin. Pract. 2017, 7, 77–85. [Google Scholar] [CrossRef]
- Koufatzidou, M.; Koletsi, D.; Basdeki, E.I.; Pandis, N.; Polychronopoulou, A. Pediatricians’ awareness on orthodontic problems and related conditions—A national survey. Prog. Orthod. 2019, 20, 33. [Google Scholar] [CrossRef]
- Sri Meenakshi, R.B.; Senthil Kumar, K.P.; Prabhakar, K. Evaluation of awareness of issues regarding obstructive sleep apnea and the orthodontist role in management: A survey among dental and medical practitioners. J. Indian Acad. Dent. Spec. Res. 2016, 3, 43–46. [Google Scholar] [CrossRef]
- Jauhar, S.; Lyons, M.F.; Banham, S.W.; Orchardson, R.; Livingston, E. The attitudes of general dental practitioners and medical specialists to the provision of intra-oral appliances for the management of snoring and sleep apnoea. Br. Dent. J. 2008, 205, 647–653. [Google Scholar] [CrossRef]
- Simmons, M.; Sayre, J.; Schotland, H.M.; Jeffe, D.B. Obstructive Sleep Apnea Knowledge among Dentists and Physicians. J. Dent. Sleep Med. 2021, 8, 1–12. [Google Scholar] [CrossRef]
- Swapna, L.A.; Alotaibi, N.F.; Falatah, S.A.; Joaithen, M.S.A.; Koppolu, P. Knowledge of Obstructive Sleep Apnea among Dental Fraternity in Riyadh. Open Access Maced. J. Med. Sci. 2019, 7, 2508–2512. [Google Scholar] [CrossRef] [PubMed]
- Bian, H. Knowledge, opinions, and clinical experience of general practice dentists toward obstructive sleep apnea and oral appliances. Sleep Breath. 2004, 8, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Johal, A.; Agha, B. Ready-made versus custom-made mandibular advancement appliances in obstructive sleep apnea: A systematic review and meta-analysis. J. Sleep Res. 2018, 27, e12660. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, M.H.; Alghamdi, A.H.; Alghamdi, S.A.; Alotaibi, R.K. Knowledge and Attitude of Dentists Towards Obstructive Sleep Apnea. Int. Dent. J. 2022, 72, 315–321. [Google Scholar] [CrossRef]

| Characteristics | No. (%) |
|---|---|
| Gender | |
| Male | 198 (55.3) |
| Female | 160 (44.7) |
| Age group (years) | |
| 26–35 | 223 (62.3) |
| >35 | 135 (37.7) |
| Level of training | |
| GPs | 98 (27.4) |
| Residents | 146 (40.8) |
| Specialists | 114 (31.8) |
| Specialty | |
| GP, FM, Int. Med. | 226 (63.1) |
| Pediatr | 64 (17.9) |
| Pulm./Sleep Med. | 35 (9.8) |
| ENT | 33 (9.2) |
| Years of experience | |
| <5 years | 174 (48.7) |
| ≥5 years | 183 (51.3) |
| Statements | Responses | ||
|---|---|---|---|
| True | False | Don’t Know | |
| General Knowledge | No. (%) | No. (%) | No. (%) |
| Mouth breathing may be associated with: | |||
| 280 (78.2) * | 34 (9.5) | 44 (12.3) |
| 197 (55.0) * | 87 (24.3) | 74 (20.7) |
| 215 (60.1) * | 44 (12.3) | 99 (27.7) |
| The following factors may contribute to development of OSA: | |||
| 263 (73.5) * | 28 (7.8) | 67 (18.7) |
| 197 (55.0) * | 71 (19.8) | 90 (25.1) |
| 220 (61.5) * | 59 (16.5) | 79 (22.1) |
| 226 (63.1) * | 45 (12.6) | 87 (24.3) |
| The following is considered one of the management methods of OSA: | |||
| 281 (78.5) * | 43 (12) | 34 (9.5) |
| 242 (67.6) * | 38 (10.6) | 78 (21.8) |
| 243 (67.9) * | 44 (12.3) | 71 (19.8) |
| 208 (58.1) * | 102 (28.5) | 48 (13.4) |
| 245 (68.4) * | 45 (12.6) | 68 (19.0) |
| Specific Knowledge | |||
| 229 (64.0) * | 58 (16.2) | 71 (19.8) |
| 173 (48.3) * | 49 (13.7) | 136 (38.0) |
| 163 (45.5) * | 38 (10.6) | 157 (43.9) |
| 176 (49.2) * | 30 (8.4) | 152 (42.4) |
| Oral appliances to advance the lower jaw (mandible) during sleep for OSA management are best delivered and adjusted by: | |||
| 170 (68.4) | 112 (12.6) * | 76 (19.0) |
| 142 (39.7) * | 140 (39.1) | 76 (21.2) |
| 191 (53.4) | 65 (18.2) * | 102 (28.5) |
| Recommended oral appliance for OSA management should be: | |||
| 122 (34.1) | 94 (26.3) * | 142 (39.7) |
| 197 (55) * | 63 (17.6) | 98 (27.4) |
| 144 (40.2) | 69 (19.3) * | 145 (40.5) |
| Dentists could provide the following: | |||
| 243 (67.9) * | 53 (14.8) | 62 (17.3) |
| 161 (45.0) | 136 (38.0) * | 61 (17.0) |
| 224 (62.6) * | 77 (21.5) | 57 (15.9) |
| 251 (70.1) * | 45 (12.6) | 62 (17.3) |
| 235 (65.6) * | 48 (13.4) | 75 (20.9) |
| 255 (71.2) * | 36 (10.1) | 67 (18.7) |
| 234 (65.4) * | 53 (14.8) | 71 (19.8) |
| Characteristics | Level of Knowledge | PMS (SD) | ||
|---|---|---|---|---|
| Poor No. (%) | Average No. (%) | Good No. (%) | ||
| Overall knowledge (n = 358) | 127 (35.5) | 169 (47.2) | 62 (17.3) | 56.0 (19.4) |
| General knowledge | 74 (20.6) | 157 (43.9) | 127 (35.5) | 65.6 (25.0) |
| Specific knowledge | 167 (46.6) | 170 (47.5) | 21 (5.9) | 49.3 (19.2) |
| χ2# = 143.00, p < 0.001 | t@ = 15.23, p < 0.001 * | |||
| Gender | ||||
| Male | 71 (35.9) | 88 (44.4) | 39 (19.7) | 55.9 (20.1) |
| Female | 56 (35.0) | 81 (50.6) | 23 (14.4) | 56.1 (18.5) |
| χ2 = 2.18, p = 0.34 | t# = 0.12, p = 0.91 | |||
| Age group (years) | ||||
| 26–35 | 85 (38.1) | 106 (47.5) | 32 (14.3) | 54.2 (19.4) |
| >35 | 42 (31.1) | 63 (46.7) | 30 (22.2) | 59.0 (19.1) |
| χ2 = 4.19, p = 0.12 | t# = 2.31, p = 0.025 * | |||
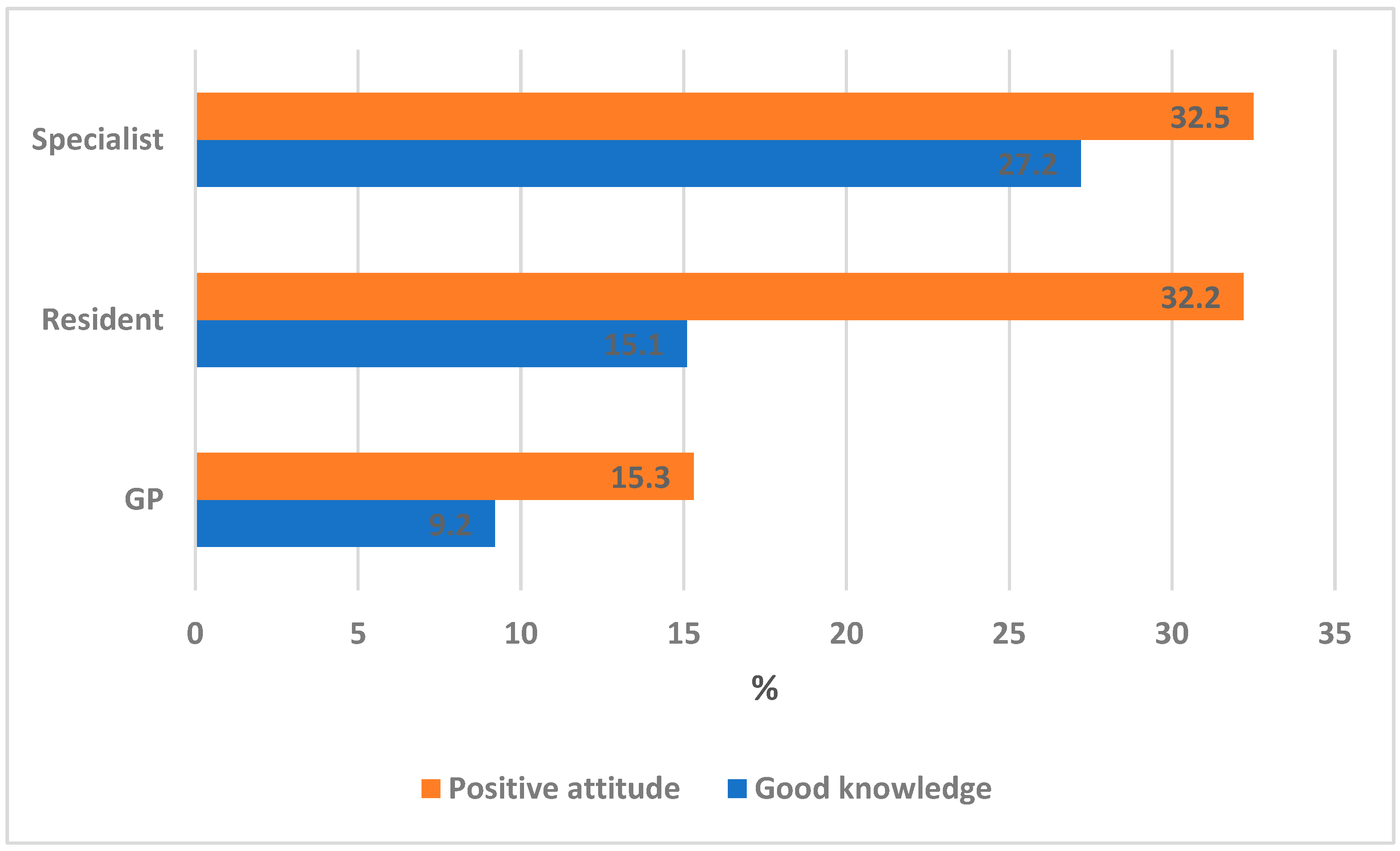
| Level of training | ||||
| GPs | 49 (50.0) | 40 (40.8) | 9 (9.2) | 49.6 (19.3) |
| Residents | 52 (35.6) | 72 (49.3) | 22 (15.1) | 55.2 (19.0) * |
| Specialists | 26 (22.8) | 57 (50.0) | 31 (27.2) | 62.5 (18.0) * |
| χ2LT = 21.88, p < 0.001 * | f = 12.76, p < 0.001 * | |||
| Specialty | ||||
| GP, FM, Int. Med. | 86 (38.1) | 110 (48.7) | 30 (13.3) | 54.7 (19.2) |
| Pediatr | 19 (29.7) | 32 (50.0) | 13 (20.3) | 57.1 (18.9) |
| Pulm./Sleep Med. | 19 (29.7) | 11 (31.4) | 8 (22.9) | 55.1 (20.2) |
| ENT | 6 (18.2) | 16 (48.5) | 11 (33.3) | 64.1 (19.7) * |
| χ2 = 14.88, p = 0.021 * | f = 2.37, 0.071 | |||
| Years of experience | ||||
| <5 years | 72 (41.4) | 81 (46.6) | 21 (12.1) | 52.1 (19.6) |
| ≥5 years | 55 (30.1) | 87 (47.5) | 41 (22.4) | 59.7 (18.5) |
| χ2 = 8.72, p < 0.001 * | t# = 3.76, p < 0.001 * | |||
| Statements | Responses | ||||
|---|---|---|---|---|---|
| Never No. (%) | Rarely No. (%) | Sometime No. (%) | Usually No. (%) | Always No. (%) | |
| I believe I should pay attention to the following in patients with obstructive breathing disorders: | |||||
| 47 (13.1) | 32 (8.9) | 90 (25.1) | 63 (17.6) | 126 (35.2) |
| 57 (15.9) | 46 (12.8) | 99 (27.7) | 75 (20.9) | 81 (22.6) |
| 50 (14.0) | 51 (14.2) | 106 (29.6) | 72 (20.1) | 79 (22.1) |
| 51 (14.2) | 56 (15.6) | 106 (29.6) | 80 (22.3) | 65 (18.2) |
| 55 (15.4) | 43 (12.0) | 84 (23.5) | 90 (25.1) | 86 (24.0) |
| 52 (14.5) | 63 (17.6) | 106 (29.6) | 80 (22.3) | 57 (15.9) |
| I believe I should refer patients with obstructive breathing disorder to a dentist for a more comprehensive assessment when I notice the following: | |||||
| 45 (12.6) | 48 (13.4) | 113 (31.6) | 74 (20.7) | 78 (21.8) |
| 56 (15.6) | 65 (18.2) | 98 (27.4) | 80 (22.3) | 59 (16.5) |
| 41 (11.5%) | 50 (14.0) | 110 (30.7%) | 87 (24.3%) | 70 (19.6%) |
| 48 (13.4) | 51 (14.2) | 104 (29.1%) | 87 (24.3%) | 68 (19%) |
| 67 (18.7) | 56 (15.6) | 139 (38.8%) | 65 (18.2%) | 31 (8.7%) |
| 30 (8.4) | 55 (15.4) | 143 (39.9) | 84 (23.5) | 46 (12.8) |
| Characteristics | Level of Attitude | PMS (SD) | ||
|---|---|---|---|---|
| Negative No. (%) | Neutral No. (%) | Positive No. (%) | ||
| ALL | 84 (23.5) | 175 (48.9) | 99 (27.6) | 64.4 (17.5) |
| Gender | ||||
| Male (n = 198) | 47 (23.7) | 95 (48) | 56 (28.3) | 64.3 (18.2) |
| Female (n = 160) | 37 (23.1) | 80 (50) | 43 (26.9) | 64.5 (16.7) |
| χ2 = 0.15, p = 0.93 | t = 0.13, p = 0.90 | |||
| Age group (years) | ||||
| 26–35 (n = 223) | 46 (20.6) | 119 (53.4) | 58 (26) | 64.4 (18.2) |
| >35 (n = 135) | 38 (28.1) | 56 (41.5) | 41 (30.4) | 64.8 (17.1) |
| χ2 = 5.03, p = 0.0.08 | t = 0.05, p = 0.96 | |||
| Level of training | ||||
| GPs (n = 98) | 34 (34.7) | 49 (50.0) | 15 (15.3) | 58.1 (17.2) |
| Residents (n = 146) | 30 (20.5) | 69 (47.3) | 47 (32.2) | 66.0 (16.8) * |
| Specialists (n = 114) | 20 (17.5) | 57 (50) | 37 (32.5) | 66.7 (17.4) * |
| χ2LT = 11.56, p = 001 * | f = 9.44, p < 0.001 * | |||
| Specialty | ||||
| GP, FM, Int. Med (n = 226) | 51 (22.6) | 123 (54.4) | 52 (23) | 63.3 (16.3) * |
| Pediatr (n = 64) | 9 (14.1) | 28 (43.8) | 27 (42.2) | 70.3 (17.1) * |
| Pulm./Sleep Med. (n = 35) | 16 (45.7) | 13 (37.1) | 6 (17.1) | 56.2 (19.0) |
| ENT (n = 33) | 8 (24.2) | 11 (33.3) | 14 (42.4) | 68.9 (20.3) * |
| χ2 = 24.92, p < 0.001 * | f = 6.29, p < 0.001 * | |||
| Years of experience | ||||
| <5 years (n = 174) | 39 (22.4) | 91 (52.3) | 44 (25.3) | 64.4 (17.9) |
| ≥5 years (n = 183) | 45 (24.6) | 83 (45.4) | 55 (30.1) | 63.3 (17.0) |
| χ2 = 1.79, p = 0.41 | t = 1.14, p = 0.26 | |||
| Knowledge Score | Attitude Score | |||||
|---|---|---|---|---|---|---|
| B (SE) | t-Value | p-Value | B (SE) | t-Value | p-Value | |
| Gender | −0.70(2.0) | −0.35 | 0.73 | −0.06(1.78) | 0.03 | 0.98 |
| Age group | −1.11(2.66) | −0.42 | 0.68 | −2.34(2. 34) | −1.01 | 0.32 |
| Training level | 5.35 (1.48) | 3.60 | <0.001* | 4.16(1.32) | 3.15 | 0.002 * |
| Specialty | 1.11(1.04) | 1.07 | 0.28 | −0.16(0.91) | −0.18 | 0.86 |
| Years of experience | 3.97(2.73) | 1.46 | 0.15 | −1.06 (2.40) | 0.44 | 0.66 |
| Knowledge (score) | 0.21 (0.04) | 5.71 | <0.001 * | |||
| Constant | 41.97(3.24) | 12.94 | <0.001 | 44.03(3.38) | 13.3 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alrejaye, N.S.; Alfayez, K.M.; Al Ali, H.H.; Bushnaq, Y.M.; Bin Zaid, R.S.; Alobaid, F.K.; Abolfotouh, M.A. Awareness and Attitude of Physicians on the Role of Dentists in the Management of Obstructive Sleep Apnea. Int. J. Environ. Res. Public Health 2022, 19, 16126. https://doi.org/10.3390/ijerph192316126
Alrejaye NS, Alfayez KM, Al Ali HH, Bushnaq YM, Bin Zaid RS, Alobaid FK, Abolfotouh MA. Awareness and Attitude of Physicians on the Role of Dentists in the Management of Obstructive Sleep Apnea. International Journal of Environmental Research and Public Health. 2022; 19(23):16126. https://doi.org/10.3390/ijerph192316126
Chicago/Turabian StyleAlrejaye, Najla S., Khalid M. Alfayez, Hafsah H. Al Ali, Yara M. Bushnaq, Reem S. Bin Zaid, Fahad K. Alobaid, and Mostafa A. Abolfotouh. 2022. "Awareness and Attitude of Physicians on the Role of Dentists in the Management of Obstructive Sleep Apnea" International Journal of Environmental Research and Public Health 19, no. 23: 16126. https://doi.org/10.3390/ijerph192316126
APA StyleAlrejaye, N. S., Alfayez, K. M., Al Ali, H. H., Bushnaq, Y. M., Bin Zaid, R. S., Alobaid, F. K., & Abolfotouh, M. A. (2022). Awareness and Attitude of Physicians on the Role of Dentists in the Management of Obstructive Sleep Apnea. International Journal of Environmental Research and Public Health, 19(23), 16126. https://doi.org/10.3390/ijerph192316126






