The Direct and Indirect Costs of Breast Cancer in Poland: Estimates for 2017–2019
Abstract
1. Introduction
- low public awareness of the causes of carcinogenesis;
- poor organization of the health care system (lack of basic preventive examinations, deteriorating access to services, no reference centers, an inefficient information flow system that does not guarantee the physician access to information about the patient’s health, lack of treatment coordination);
- limited and inadequately deployed resources of the health care system, in particular medical staff, as well as specialized equipment [8].
2. Materials and Methods
- BC screening program—the first step was the basic diagnostic in the form of mammography, after which patients with abnormal results were referred for extended diagnostics (enhanced diagnosis stage), which could include clinical examination of the breast, fine-needle or core needle breast biopsy;
- Oncological package—also called the Rapid oncological therapy package for which the main goal was to efficiently and quickly guide the patient through the next stages of diagnosis and oncological treatment. Initially, the patient was diagnosed, and then the treatment method was determined on the Concilium. The BC Concilium was a type of medical consultation with several clinical specialists: a breast tumor surgery specialist, a clinical oncology specialist in BC, a specialist in x-ray diagnostics or radiology, and a specialist in radiotherapy. During the entire treatment process, the patient was under the constant care of the coordinator. Only costs of basic diagnostic and enhanced diagnosis under this package were included in the calculations. Other costs are taken into account at different stages of treatment, e.g., radiotherapy and outpatient treatment.
- Surgical treatment—breast-conserving surgery (BCS), mastectomy, and breast reconstruction. The expenses of the indicated types of surgical procedures were estimated based on the Polish Diagnosis-Related Group (DRG) system. DRG related to BC were: J01 Radical breast removal with reconstruction, J02 Complex breast surgeries, J03E Major breast surgeries >65 years of age, J03F Major breast surgeries <65 years of age, J04 Breast reconstruction treatments, and J05 Medium breast surgery. BCS was realized with groups J01, J02, J03E, and J03F; mastectomy with groups J01, J02, J03E, J03F, and J05; and breast reconstruction with group J04.
- Hospitalization—conservative treatment (DRG: J08. Malignant breast diseases) and mammotomic biopsy (DRG: J10. Mammotomic biopsy);
- Drug program (also called Therapeutic program)—B.09 Treatment of patients with breast cancer (ICD-10: C50). Drug program costs included costs of drugs (trastuzumab, pertuzumab, lapatinib, palbociclib (refund has started in 2019) and ribociclib (2019)), hospitalization or outpatients visit related to the patient treatment in the drug program, and diagnostic tests which have determined the efficacy and safety of the drugs in the program;
- Chemotherapy (CHT)—treatment provided to patients with diagnosis ICD-10: C50.X, including the cost of chemotherapeutic agents and the cost of CHT administration (e.g., hospitalization, outpatient consultations);
- Radiotherapy—costs of teleradiotherapy, brachytherapy, and radioisotope therapy in patients with diagnosis ICD-10: C50.X. This category also included the costs of accommodation, hospitalization, and treatment of adverse events related to radiotherapy in patients with BC;
- Outpatient care—all outpatient visits and medical services provided to patients with diagnosis ICD-10: C50.X. In particular, these were diagnostic tests on an outpatient basis (e.g., nuclear medicine tests, computed tomography, magnetic resonance imaging), outpatient visits, or outpatient surgical services.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- ECIS—European Cancer Information System. Available online: https://ecis.jrc.ec.europa.eu/index.php (accessed on 11 August 2022).
- Sun, Y.-S.; Zhao, Z.; Yang, Z.-N.; Xu, F.; Lu, H.-J.; Zhu, Z.-Y.; Shi, W.; Jiang, J.; Yao, P.-P.; Zhu, H.-P. Risk Factors and Preventions of Breast Cancer. Int. J. Biol. Sci. 2017, 13, 1387–1397. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rubio, I.T.; Zackrisson, S.; Senkus, E.; ESMO Guidelines Committee. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1194–1220. [Google Scholar] [CrossRef] [PubMed]
- WHO. International Agency for Research on Cancer. Available online: https://gco.iarc.fr/tomorrow/en/dataviz/isotype (accessed on 11 August 2022).
- Piechocki, M.; Koziołek, W.; Sroka, D.; Matrejek, A.; Miziołek, P.; Saiuk, N.; Sledzik, M.; Jaworska, A.; Bereza, K.; Pluta, E.; et al. Trends in Incidence and Mortality of Gynecological and Breast Cancers in Poland (1980–2018). Clin. Epidemiol. 2022, 14, 95–114. [Google Scholar] [CrossRef] [PubMed]
- Banas, T.; Juszczyk, G.; Pitynski, K.; Nieweglowska, D.; Ludwin, A.; Czerw, A. Incidence and mortality rates in breast, corpus uteri, and ovarian cancers in Poland (1980–2013): An analysis of population-based data in relation to socioeconomic changes. OncoTargets Ther. 2016, 9, 5521–5530. [Google Scholar] [CrossRef]
- Eurostat. Preventable and Treatable Mortality Statistics. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Preventable_and_treatable_mortality_statistics (accessed on 1 August 2022).
- Supreme Audit Office in Poland. Availability and Effects of Cancer Treatment. Available online: https://www.nik.gov.pl/plik/id,16371,vp,18897.pdf (accessed on 24 May 2022).
- Oncology Expenditure—Report. Available online: https://www.nfz.gov.pl/aktualnosci/aktualnosci-centrali/coraz-wiecej-pieniedzy-przeznaczamy-na-leczenie-nowotworow-i-leki-onkologiczne,7590.html (accessed on 14 July 2022).
- Cancer Trends Progress Report 2020 Update. Available online: http://progressreport.cancer.gov (accessed on 24 May 2022).
- Australian Institute of Health and Welfare 2021. Health System Expenditure on Cancer and Other Neoplasms in Australia, 2015–2016. Cancer Series No. 131. Cat. No. CAN 142. Canberra: AIHW. Available online: https://www.aihw.gov.au/getmedia/6bff10f3-3ec8-43d7-a967-55c5168da174/aihw-can-142.pdf.aspx?inline=true (accessed on 24 May 2022).
- Sousa, R.; Fiorentino, F.; Alarcão, J.; Lopes Pereira, C.; Jesus, G.; Costa, J.; Gouveia, M.; Borges, M. Cost and Burden of Female Breast Cancer in Portugal. Value Health 2016, 19, A724. [Google Scholar] [CrossRef]
- Mennini, F.S.; Aurilio, M.T.; Gazzillo, S.; Nardone, C.; Sciattella, P.; Marcellusi, A.; Migliorini, R.; Sciannamea, V.; Piccioni, A.; Bolcato, M.; et al. An Analysis of the Social and Economic Costs of Breast Cancer in Italy. Int. J. Environ. Res. Public Health 2021, 18, 9005. [Google Scholar] [CrossRef] [PubMed]
- The Cost and Burden of Breast Cancer in Romania. Investment in a Screening Programme for Breast Cancer. Analysis Report Made for Roche Romania. Available online: https://assets.cwp.roche.com/f/172042/x/90ca10d469/the_cost_and_burden_of_breast_cancer_in_romania.pdf (accessed on 11 July 2022).
- Luchowska, K.; Rutkiewicz, I.; Ząbek, K. Exceptions from Standard form of Data Collection Connected with Specificity of Health Care Benefit and Different Approach to cost Calculation. AOTMiT. Warsaw. 2019. Available online: https://power.aotm.gov.pl/static/Materialy/26.%20Odst%C4%99pstwa%20od%20standardowej%20formy%20zbierania%20danych%20wynikaj%C4%85ce%20ze%20specyfiki%20%C5%9Bwiadczenia%20i%20odmiennego%20podej%C5%9Bcia%20do%20kalkulacji%20koszt%C3%B3w.pdf (accessed on 11 July 2022).
- National Health Fund Statistics. Available online: https://statystyki.nfz.gov.pl/Benefits/1a (accessed on 17 August 2020).
- Resolutions of the NHF Council on the Adoption of the Periodic Report on the Activities of the National Health Fund for the Fourth Quarter of 2017/2018/2019. Available online: https://www.nfz.gov.pl/zarzadzenia-prezesa/uchwaly-rady-nfz/ (accessed on 16 September 2020).
- “Healthy Data” Portal. Available online: www.ezdrowie.gov.pl (accessed on 21 July 2020).
- Statistic Poland. Poland—Macroeconomic Indicators. Available online: https://stat.gov.pl/wskazniki-makroekonomiczne/ (accessed on 11 August 2022).
- Sickness Absenteeism due to Own Illness of Persons Insured in Social Insurance Institution. Available online: https://psz.zus.pl/kategorie/absencja-chorobowa/absencja-chorobowa-z-tytulu-choroby-wlasnej-osob-ubezpieczonych-w-zus (accessed on 24 May 2022).
- EY. Methodology of Estimating Indirect Costs in Polish Health Care System. Warsaw. 2013. Available online: https://www.infarma.pl/assets/files/raporty/Raport_Metodyka_pomiaru_kosztow_posrednich_2013.pdf (accessed on 10 July 2020).
- National Bank of Poland. Exchange Rates. Available online: https://www.nbp.pl/home.aspx?f=/kursy/arch_a.html (accessed on 23 September 2022).
- Ministry of Health. Announcements of the Minister of Health—List of Reimbursed Drugs. Available online: https://www.gov.pl/web/zdrowie/obwieszczenia-ministra-zdrowia-lista-lekow-refundowanych (accessed on 11 July 2022).
- Ministry of Health. List of Reimbursed Drugs—Announcements of the Minister of Health. Archival Page. Available online: http://www.archiwum.mz.gov.pl/leki/refundacja/lista-lekow-refundowanych-obwieszczenia-ministra-zdrowia/ (accessed on 11 July 2022).
- Statistics Poland. Expenditures on Health Care in 2018–2020. Available online: https://stat.gov.pl/files/gfx/portalinformacyjny/pl/defaultaktualnosci/5513/27/1/1/wydatki_na_ochrone_zdrowia_w_latach_2018-2020.pdf (accessed on 7 June 2022).
- A Short Guide to Cancer Screening. Increase Effectiveness, Maximize Benefits and Minimize Harm; WHO Regional Office for Europe: Copenhagen, Denmark, 2022; Available online: https://apps.who.int/iris/bitstream/handle/10665/351396/9789289057561-eng.pdf (accessed on 14 July 2022).
- National Health Fund. Data on the Implementation of the Programs. Available online: https://www.nfz.gov.pl/dla-pacjenta/programy-profilaktyczne/dane-o-realizacji-programow/ (accessed on 13 July 2022).
- Łyszczarz, B.; Nojszewska, E. Productivity losses and public finance burden attributable to breast cancer in Poland, 2010–2014. BMC Cancer 2017, 17, 676. [Google Scholar] [CrossRef] [PubMed]



| Treatment Method | Resource Utilization, Healthcare Services Number | Expenditures of the Public Payer (in Thousand EUR) | ||||
|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | |
| Direct costs | ||||||
| BC screening program 1 | 20,654.0 | 20,280.4 | 21,483.6 | |||
| Basic diagnostic stage: screening mammography | 1,048,151 | 1,017,165 | 1,043,743 | 19,522.0 | 19,221.1 | 20,357.1 |
| Enhanced diagnosis stage | 34,269 | 31,894 | 33,241 | 1132.0 | 1059.3 | 1126.5 |
| Oncological package (only diagnostic) 2 | 3538.5 | 4013.1 | 4010.9 | |||
| Basic diagnostic | 6374 | 10,828 | 14,589 | 554.2 | 919.6 | 1238.0 |
| Enhanced diagnostics | 14,682 | 15,417 | 15,569 | 2984.3 | 3093.5 | 2773.0 |
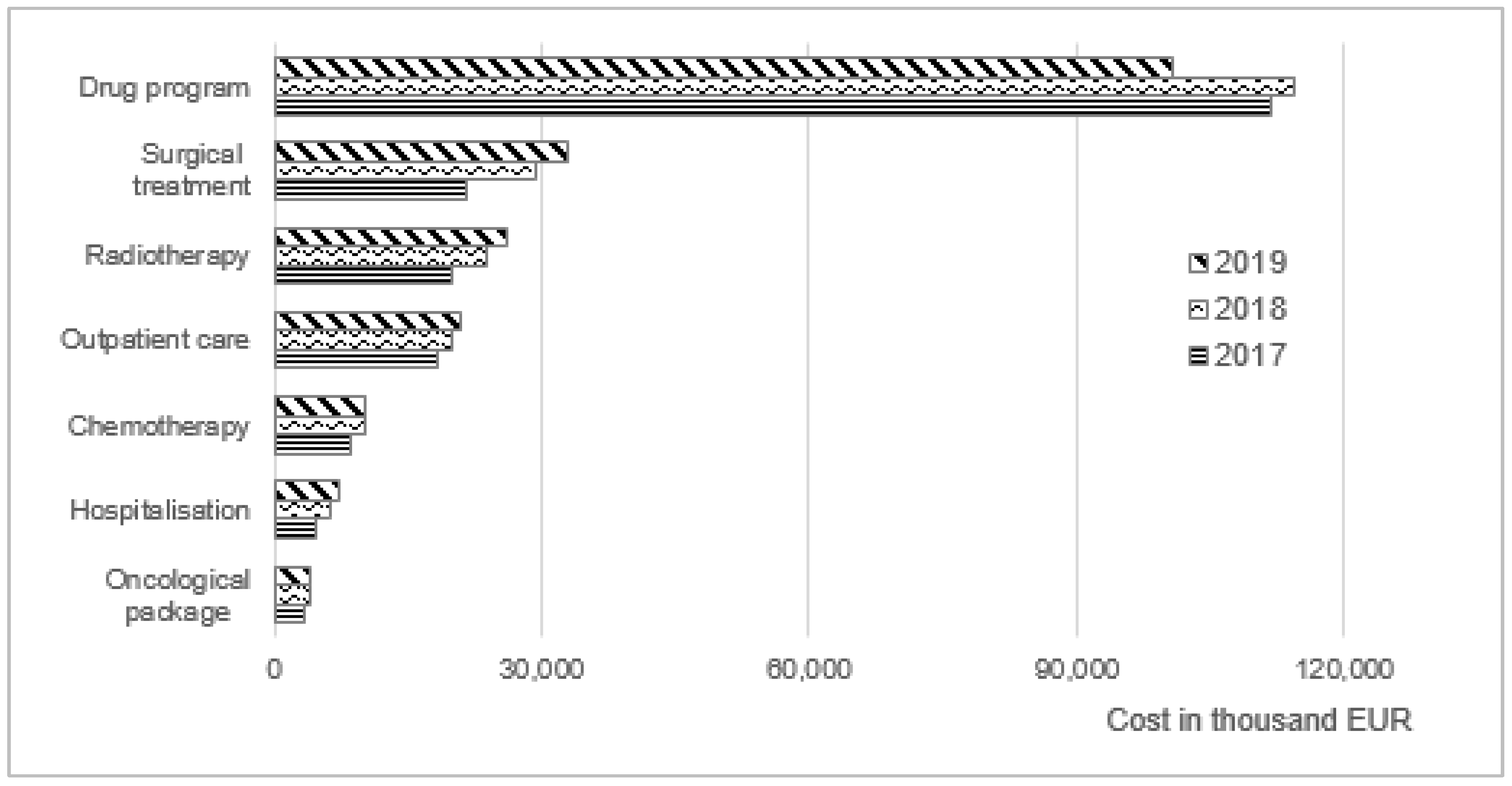
| Surgical treatment 2 | 21,713.2 | 29,482.6 | 32,994.8 | |||
| Breast-conserving surgery (BCS) | 12,610 | 15,108 | 12,843 | 11,211.9 | 15,324.7 | 15,374.1 |
| Mastectomy | 7997 | 8856 | 9070 | 8733.9 | 11,837.3 | 14,993.4 |
| Breast reconstruction 3 | 2152 | 2410 | 2341 | 1767.4 | 2320.5 | 2627.3 |
| Hospitalization 2 | 4761.3 | 6453.7 | 7318.9 | |||
| Conservative treatment | 7503 | 7747 | 7990 | 2499.0 | 3011.6 | 4185.5 |
| Mammotomic biopsy 4 | 6257 | 6825 | 5838 | 2262.4 | 3442.1 | 3133.5 |
| Drug program B.09 2 | 111,851.5 | 114,357.8 | 100,831.1 | |||
| Drugs (number of patients) | 6883 | 7341 | 8077 | 104,529.0 | 106,551.8 | 93,148.0 |
| Hospitalization and outpatients visit | 60,747 | 63,542 | 62,301 | 5979.2 | 6095.9 | 5803.5 |
| Diagnostics tests | 2933 | 3215 | 3250 | 1343.3 | 1710.1 | 1879.6 |
| Chemotherapy 1,5 | na | na | na | 8685.8 | 10,105.7 | 10,337.7 |
| Radiotherapy 1,5 | 20,016.9 | 23,914.3 | ||||
| Teleradiotherapy | 33,790 | 39,135 | 43,795 | 18,272.7 | 22,136.3 | 24,153.9 |
| Brachytherapy and radioisotope therapy | 913 | 941 | 1067 | 1744.1 | 1778.0 | 2075.3 |
| Outpatient care 1,5 | 756,992 | 772,353 | 806,582 | 18,306.1 | 19,790.8 | 21,078.0 |
| Total medical care cost | 209,527.3 | 228,398.4 | 224,284.3 | |||
| Year-to-year change | - | 9% | −2% | |||
| Indirect costs | ||||||
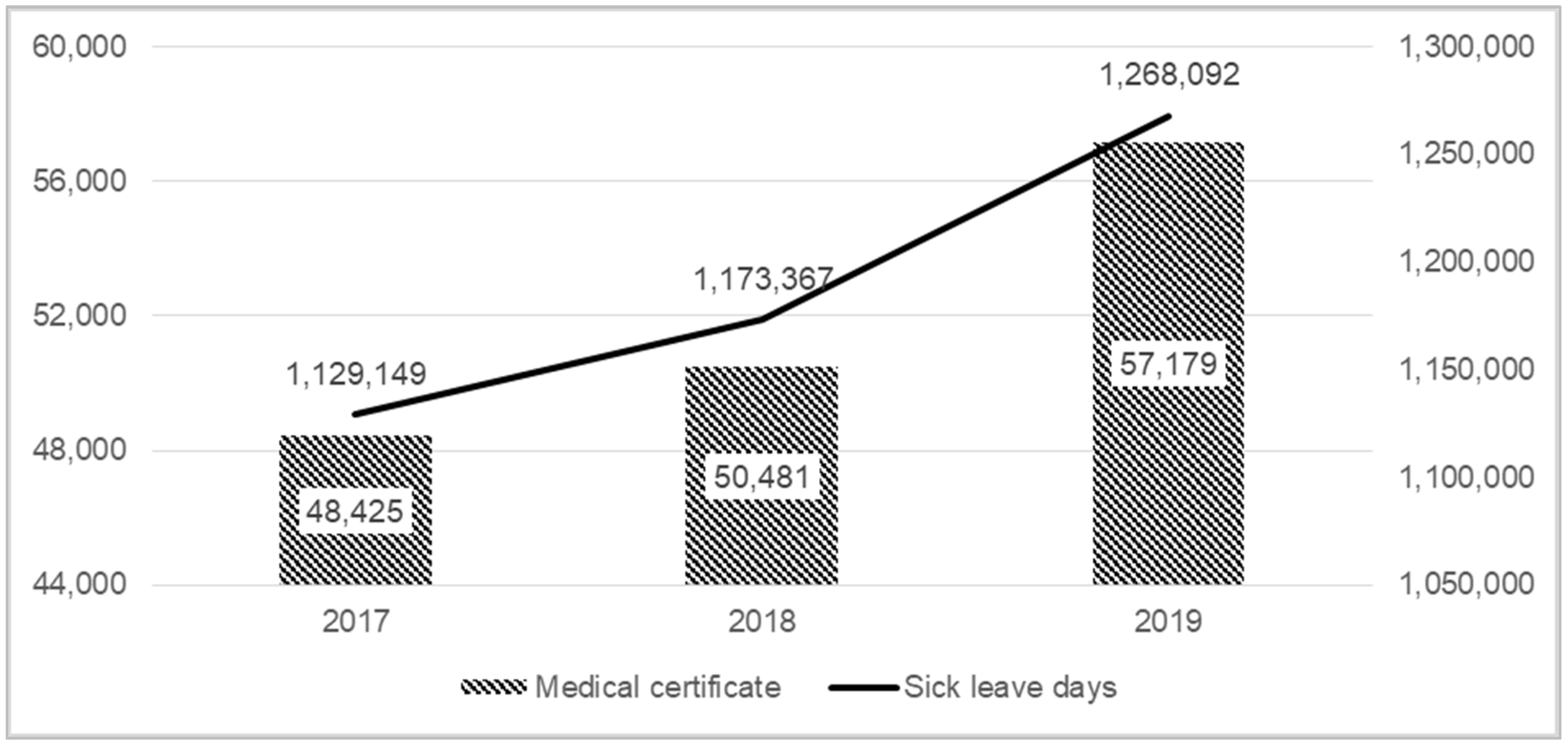
| Number of sick leave days/Number of medical certificate | 1,129,149/ 48,425 | 1,173,367/50,481 | 1,268,092/57,179 | - | ||
| Value of productivity loss due to BC (social cost) | 95,844.1 | 104,599.8 | 120,364.3 | |||
| Year-to-year change | - | 9% | 15% | |||
| Total expenditures for BC | 305,371.4 | 332,998.2 | 344,648.5 | |||
| Percentage of medical care cost in total expenditures | 69% | 69% | 65% | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seweryn, M.; Banas, T.; Augustynska, J.; Lorenc, O.; Kopel, J.; Pluta, E.; Skora, T. The Direct and Indirect Costs of Breast Cancer in Poland: Estimates for 2017–2019. Int. J. Environ. Res. Public Health 2022, 19, 16384. https://doi.org/10.3390/ijerph192416384
Seweryn M, Banas T, Augustynska J, Lorenc O, Kopel J, Pluta E, Skora T. The Direct and Indirect Costs of Breast Cancer in Poland: Estimates for 2017–2019. International Journal of Environmental Research and Public Health. 2022; 19(24):16384. https://doi.org/10.3390/ijerph192416384
Chicago/Turabian StyleSeweryn, Michal, Tomasz Banas, Joanna Augustynska, Ola Lorenc, Justyna Kopel, Elzbieta Pluta, and Tomasz Skora. 2022. "The Direct and Indirect Costs of Breast Cancer in Poland: Estimates for 2017–2019" International Journal of Environmental Research and Public Health 19, no. 24: 16384. https://doi.org/10.3390/ijerph192416384
APA StyleSeweryn, M., Banas, T., Augustynska, J., Lorenc, O., Kopel, J., Pluta, E., & Skora, T. (2022). The Direct and Indirect Costs of Breast Cancer in Poland: Estimates for 2017–2019. International Journal of Environmental Research and Public Health, 19(24), 16384. https://doi.org/10.3390/ijerph192416384






