Screening for Referral of Serious Pathology by Physical Examination Tests in Patients with Back or Chest Pain: A Systematic Review
Abstract
1. Background
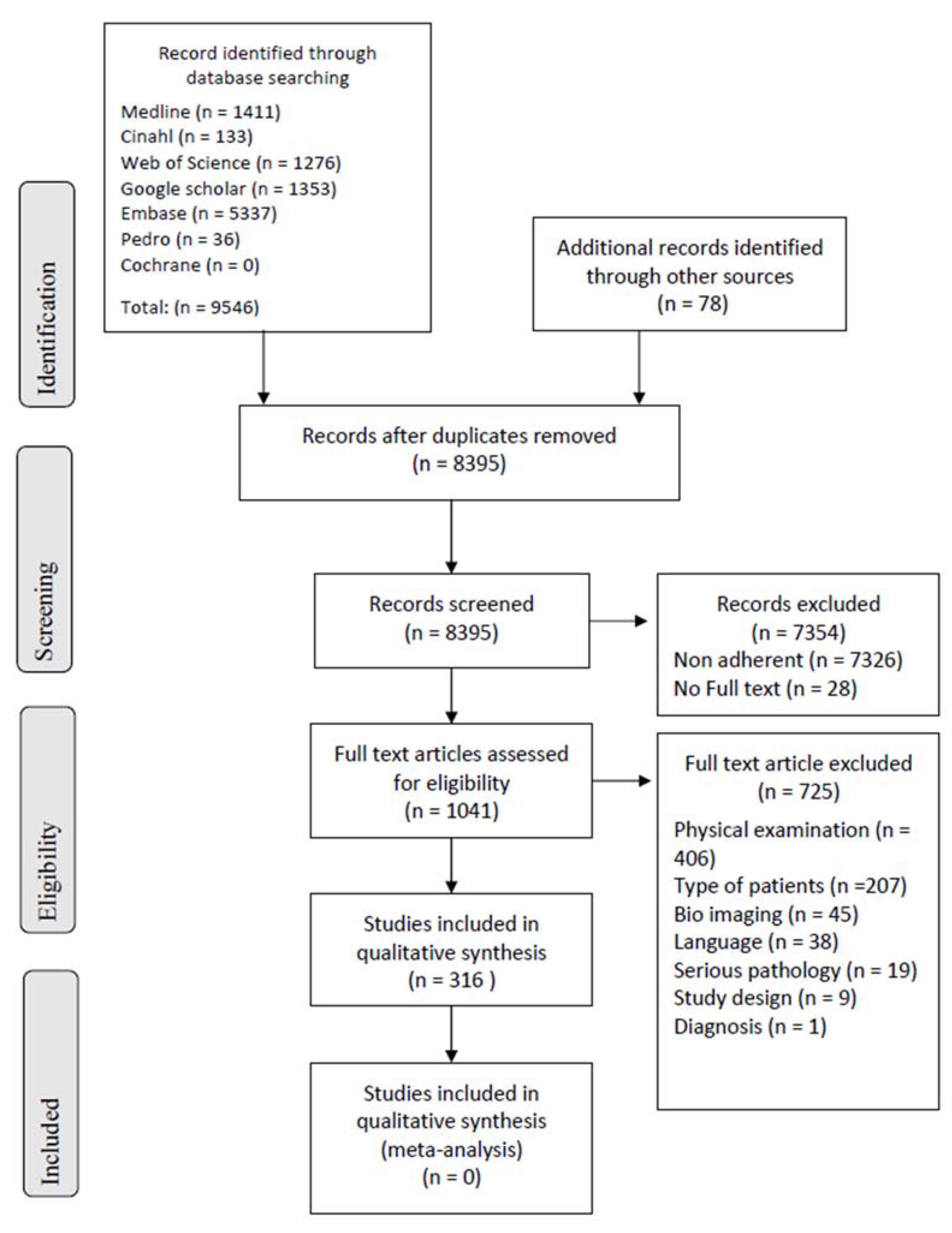
2. Methods
2.1. Eligibility Criteria
2.1.1. Study Designs
2.1.2. Participants
2.1.3. Serious Pathology
2.1.4. Physical Examination Tests (PETs)
2.2. Search Methods for Inclusion of Studies—Search Strategy
2.3. Studies Selection and Data Extraction
- General information (authors, study design, setting, and number of assessments);
- Participants (age, gender, sample size, diagnostic criteria, comorbidities, pain duration, and structures of recruitment);
- Type of PETs;
- PETs values;
- Primary healthcare professional in charge; and
- Serious pathology diagnosed.
2.4. Inter-Rater Agreement
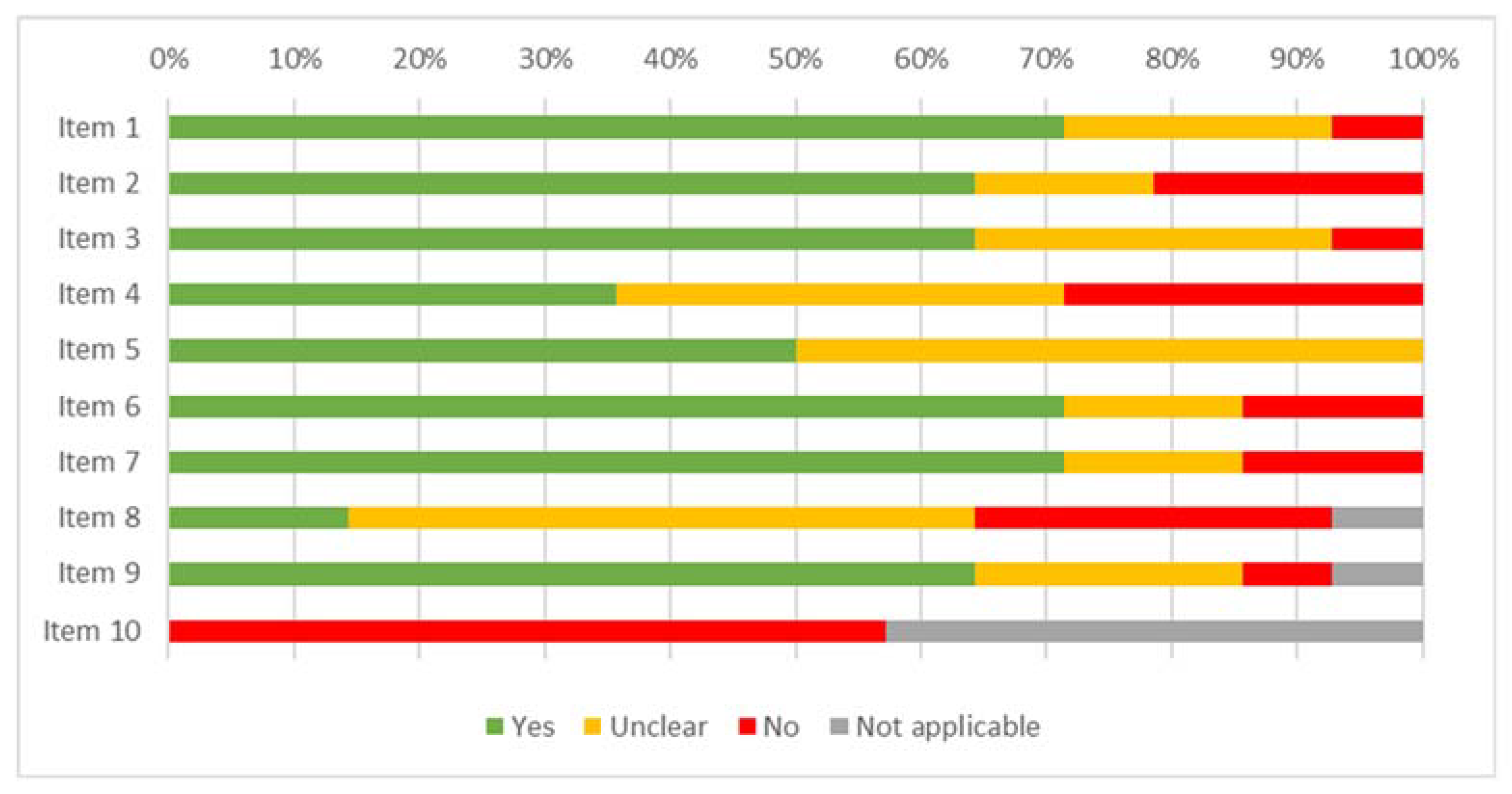
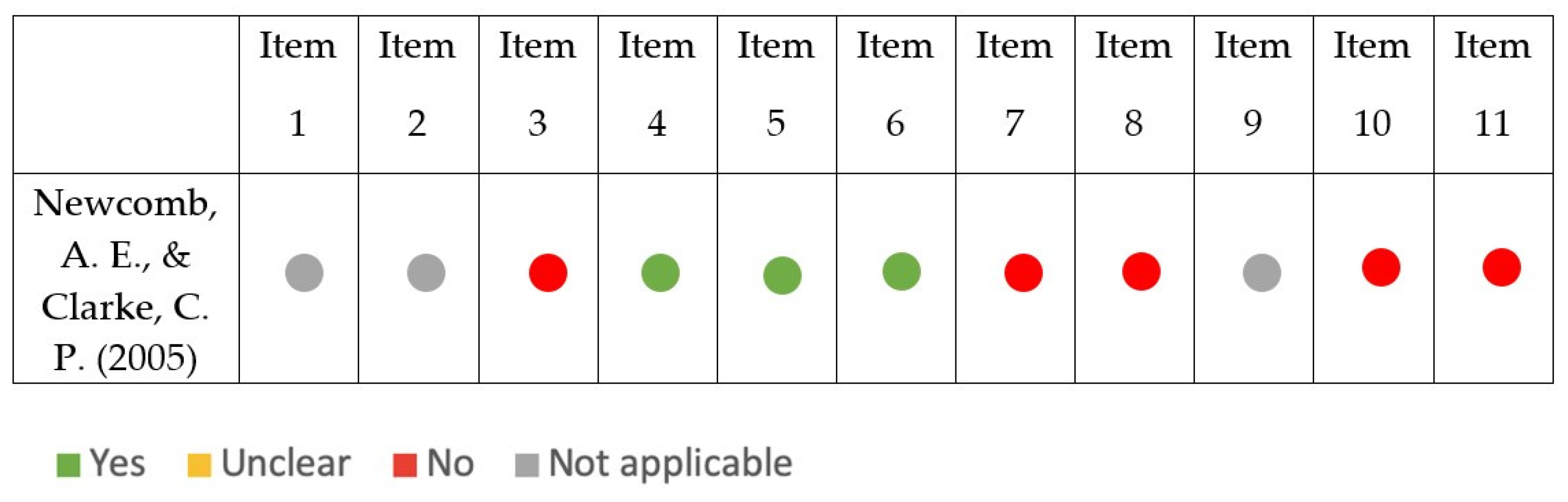
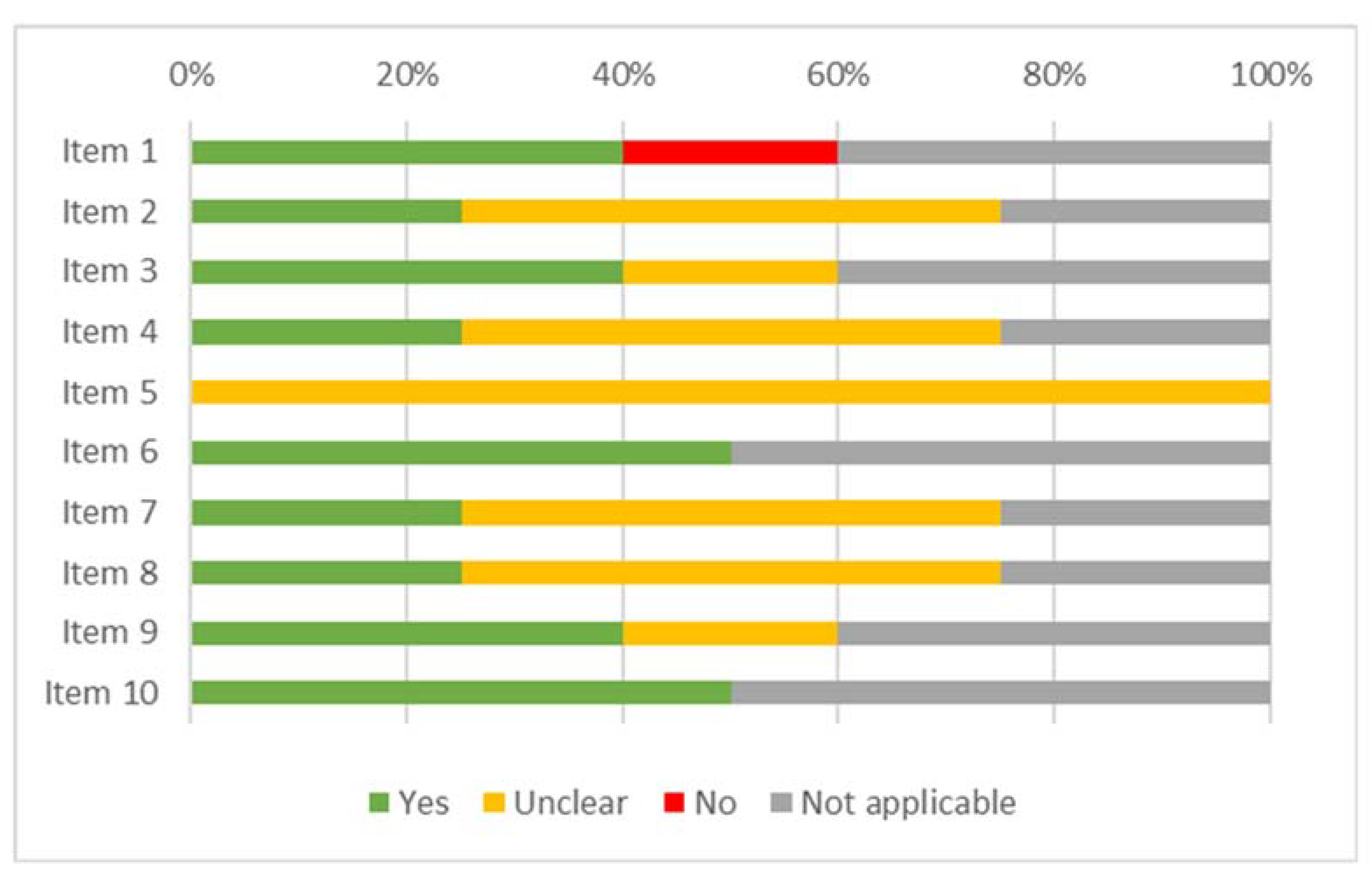
2.5. Risk of Bias
2.6. Data Analysis
3. Results
3.1. Study Characteristics
3.1.1. Study Designs
3.1.2. Sample
3.2. Risk of Bias
3.3. Synthesis of Results
3.3.1. Serious Pathologies
3.3.2. Physical Examination Test
3.3.3. Primary Healthcare Professional in Charge
3.3.4. PET Diagnostic Accuracy
4. Discussion
4.1. Strengths and Limitations
4.2. Directions for the Future
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Enthoven, W.T.; Geuze, J.; Scheele, J.; Bierma-Zeinstra, S.M.; Bueving, H.J.; Bohnen, A.M.; Luijsterburg, P.A. Prevalence and "Red Flags" Regarding Specified Causes of Back Pain in General Practice. Phys. Ther. 2016, 96, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, J.D.; Carroll, L.J.; Côté, P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine 1998, 23, 1860–1866. [Google Scholar] [CrossRef] [PubMed]
- Koes, B.W.; van Tulder, M.W.; Thomas, S. Diagnosis and treatment of low back pain. BMJ 2006, 332, 1430–1434. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.M.; Smith, A.J.; Straker, L.M.; Bragge, P. Thoracic spine pain in the general population: Prevalence, incidence and associated factors in children, adolescents and adults. A systematic review. BMC Musculoskelet. Disord. 2009, 10, 77. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Fu, R.; Carrino, J.A.; Deyo, R.A. Imaging strategies for low-back pain: Systematic review and meta-analysis. Lancet 2009, 373, 463–472. [Google Scholar] [CrossRef]
- Henschke, N.; Maher, C.G.; Refshauge, K.M.; Herbert, R.D.; Cumming, R.G.; Bleasel, J.; York, J.; Das, A.; McAuley, J.H. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009, 60, 3072–3080. [Google Scholar] [CrossRef]
- Bardin, L.D.; King, P.; Maher, C.G. Diagnostic triage for low back pain: A practical approach for primary care. Med. J. Aust. 2017, 206, 268–273. [Google Scholar] [CrossRef]
- Hoorweg, B.B.; Willemsen, R.T.; Cleef, L.E.; Boogaerts, T.; Buntinx, F.; Glatz, J.F.; Dinant, G.J. Frequency of chest pain in primary care, diagnostic tests performed and final diagnoses. Heart 2017, 103, 1727–1732. [Google Scholar] [CrossRef]
- Maselli, F.; Palladino, M.; Barbari, V.; Storari, L.; Rossettini, G.; Testa, M. The diagnostic value of Red Flags in thoracolumbar pain: A systematic review. Disabil. Rehabil. 2020, 44, 1190–1206. [Google Scholar] [CrossRef]
- Geyser, M.; Smith, S. Chest pain prevalence, causes, and disposition in the emergency department of a regional hospital in Pretoria. Afr. J. Prim. Health Care Fam. Med. 2016, 8, e1–e5. [Google Scholar] [CrossRef]
- Haasenritter, J.; Biroga, T.; Keunecke, C.; Becker, A.; Donner-Banzhoff, N.; Dornieden, K.; Stadje, R.; Viniol, A.; Bösner, S. Causes of chest pain in primary care--a systematic review and meta-analysis. Croat. Med J. 2015, 56, 422–430. [Google Scholar] [CrossRef]
- Wertli, M.M.; Dangma, T.D.; Müller, S.E.; Gort, L.M.; Klauser, B.S.; Melzer, L.; Held, U.; Steurer, J.; Hasler, S.; Burgstaller, J.M. Non-cardiac chest pain patients in the emergency department: Do physicians have a plan how to diagnose and treat them? A retrospective study. PLoS ONE 2019, 14, e0211615. [Google Scholar] [CrossRef]
- de Gruchy, A.; Granger, C.; Gorelik, A. Physical Therapists as Primary Practitioners in the Emergency Department: Six-Month Prospective Practice Analysis. Phys. Ther. 2015, 95, 1207–1216. [Google Scholar] [CrossRef]
- Duenas, R.; Carucci, G.M.; Funk, M.F.; Gurney, M.W. Chiropractic-primary care, neuromusculoskeletal care, or musculoskeletal care? Results of a survey of chiropractic college presidents, chiropractic organization leaders, and Connecticut-licensed doctors of chiropractic. J. Manip. Physiol. Ther. 2003, 26, 510–526. [Google Scholar] [CrossRef]
- Garrity, B.; McDonough, C.; Ameli, O.; Rothendler, J.; Carey, K.; Cabral, H.; Stein, M.; Saper, R.; Kazis, L.E. Unrestricted Direct Access to Physical Therapist Services Is Associated With Lower Health Care Utilization and Costs in Patients With New-Onset Low Back Pain. Phys. Ther. 2020, 100, 107–115. [Google Scholar] [CrossRef]
- Kinsella, R.; Collins, T.; Shaw, B.; Sayer, J.; Cary, B.; Walby, A.; Cowan, S. Management of patients brought in by ambulance to the emergency department: Role of the Advanced Musculoskeletal Physiotherapist. Aust. Health Rev. 2018, 42, 309–315. [Google Scholar] [CrossRef]
- Kremer, R.G.; Duenas, R.; McGuckin, B. Defining primary care and the chiropractic physicians’ role in the evolving health care system. J. Chiropr. Med. 2002, 1, 3–8. [Google Scholar] [CrossRef][Green Version]
- Sayer, J.M.; Kinsella, R.M.; Cary, B.A.; Burge, A.T.; Kimmel, L.A.; Harding, P. Advanced musculoskeletal physiotherapists are effective and safe in managing patients with acute low back pain presenting to emergency departments. Aust. Health Rev. 2018, 42, 321–326. [Google Scholar] [CrossRef]
- Leerar, P.J.; Boissonnault, W.; Domholdt, E.; Roddey, T. Documentation of red flags by physical therapists for patients with low back pain. J. Man. Manip. Ther. 2007, 15, 42–49. [Google Scholar] [CrossRef]
- Premkumar, A.; Godfrey, W.; Gottschalk, M.B.; Boden, S.D. Red Flags for Low Back Pain Are Not Always Really Red: A Prospective Evaluation of the Clinical Utility of Commonly Used Screening Questions for Low Back Pain. JBJS 2018, 100, 368–374. [Google Scholar] [CrossRef]
- Verhagen, A.P.; Downie, A.; Maher, C.G.; Koes, B.W. Most red flags for malignancy in low back pain guidelines lack empirical support: A systematic review. Pain 2017, 158, 1860–1868. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.M.; Henschke, N.; Maher, C.G.; Van Tulder, M.W.; Koes, B.W.; Macaskill, P.; Irwig, L. Red flags to screen for vertebral fracture in patients presenting with low-back pain. Cochrane Database Syst. Rev. 2013, 1, CD008643. [Google Scholar] [CrossRef]
- Galliker, G.; Scherer, D.E.; Trippolini, M.A.; Rasmussen-Barr, E.; LoMartire, R.; Wertli, M.M. Low Back Pain in the Emergency Department: Prevalence of Serious Spinal Pathologies and Diagnostic Accuracy of Red Flags. Am. J. Med. 2020, 133, 60–72.e14. [Google Scholar] [CrossRef] [PubMed]
- Goodman, C.C. Screening for gastrointestinal, hepatic/biliary, and renal/urologic disease. J. Hand Ther. 2010, 23, 140–157. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef]
- Sackett, D.L. The Cochrane Collaboration Handbook; The Cochrane Collaboration: Oxford, UK, 1994. [Google Scholar]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Page, M.J.; Shamseer, L.; Tricco, A.C. Registration of systematic reviews in PROSPERO: 30,000 records and counting. Syst. Rev. 2018, 7, 32. [Google Scholar] [CrossRef]
- Altman, D.G. Practical Statistics for Medical Research, 1st ed.; Chapman and Hall: London, UK, 1991. [Google Scholar]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Thompson, M.; Tiwari, A.; Fu, R.; Moe, E.; Buckley, D.I. A Framework To Facilitate the Use of Systematic Reviews and Meta-Analyses in the Design of Primary Research Studies; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2012.
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M.; QUADAS-2 Group. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Boissonnault, W.G.; Ross, M.D. Physical therapists referring patients to physicians: A review of case reports and series. J. Orthop. Sports Phys. Ther. 2012, 42, 446–454. [Google Scholar] [CrossRef]
- Cook, C.E.; George, S.Z.; Reiman, M.P. Red flag screening for low back pain: Nothing to see here, move along: A narrative review. Br. J. Sports Med. 2018, 52, 493–496. [Google Scholar] [CrossRef]
- Henschke, N.; Maher, C.G.; Ostelo, R.W.; De Vet, H.C.; Macaskill, P.; Irwig, L. Red flags to screen for malignancy in patients with low-back pain. Cochrane Database Syst. Rev. 2013, 2, CD008686. [Google Scholar] [CrossRef]
- Finucane, L.M.; Downie, A.; Mercer, C.; Greenhalgh, S.M.; Boissonnault, W.G.; Pool-Goudzwaard, A.L.; Beneciuk, J.M.; Leech, R.L.; Selfe, J. International Framework for Red Flags for Potential Serious Spinal Pathologies. J. Orthop. Sports Phys. Ther. 2020, 50, 350–372. [Google Scholar] [CrossRef]
- Azeredo, T.R.M.; Guedes, H.M.; de Almeida, R.A.R.; Chianca, T.C.M.; Martins, J.C.A. Efficacy of the Manchester Triage System: A systematic review. Int. Emerg. Nurs. 2015, 23, 47–52. [Google Scholar] [CrossRef]
- Graber, M.; Gordon, R.; Franklin, N. Reducing diagnostic errors in medicine: What’s the goal? Acad. Med. 2002, 77, 981–992. [Google Scholar] [CrossRef]
- Dyck, P.; Doyle, J.B. ‘Bicycle test’ of van Gelderen in diagnosis of intermittent cauda equina compression syndrome. J. Neurosurg. 1977, 46, 667–670. [Google Scholar] [CrossRef]
- Kapeller, P.; Fazekas, F.; Krametter, D.; Koch, M.; Roob, G.; Schmidt, R.; Offenbacher, H. Pyogenic infectious spondylitis: Clinical, laboratory and MRI features. Eur. Neurol. 1997, 38, 94–98. [Google Scholar] [CrossRef]
- Negrini, S.; Politano, E.; Carabalona, R.; Mambrini, A. General Practitioners’ Management of Low Back Pain. Spine 2001, 26, 2727–2733. [Google Scholar] [CrossRef]
- Maselli, F.; Testa, M. Superficial peroneal nerve schwannoma presenting as lumbar radicular syndrome in a non-competitive runner. J. Back Musculoskelet Rehabil. 2019, 32, 361–365. [Google Scholar] [CrossRef]
- Feller, D.; Giudice, A.; Faletra, A.; Salomon, M.; Galeno, E.; Rossettini, G.; Brindisino, F.; Maselli, F.; Hutting, N.; Mourad, F. Identifying peripheral arterial diseases or flow limitations of the lower limb: Important aspects for cardiovascular screening for referral in physiotherapy. Musculoskelet. Sci. Pr. 2022, 61, 102611. [Google Scholar] [CrossRef]
- Faletra, A.; Bellin, G.; Dunning, J.; Fernández-De-Las-Peñas, C.; Pellicciari, L.; Brindisino, F.; Galeno, E.; Rossettini, G.; Maselli, F.; Severin, R.; et al. Assessing cardiovascular parameters and risk factors in physical therapy practice: Findings from a cross-sectional national survey and implication for clinical practice. BMC Musculoskelet. Disord. 2022, 23, 749. [Google Scholar] [CrossRef] [PubMed]
- Mourad, F.; Lopez, G.; Cataldi, F.; Maselli, F.; Pellicciari, L.; Salomon, M.; Kranenburg, H.; Kerry, R.; Taylor, A.; Hutting, N. Assessing Cranial Nerves in Physical Therapy Practice: Findings from a Cross-Sectional Survey and Implication for Clinical Practice. Healthcare 2021, 9, 1262. [Google Scholar] [CrossRef] [PubMed]
- Maselli, F.; Rossettini, G.; Viceconti, A.; Testa, M. Importance of screening in physical therapy: Vertebral fracture of thoracolumbar junction in a recreational runner. BMJ Case Rep. 2019, 12, e229987. [Google Scholar] [CrossRef] [PubMed]


| Item | n | % | Mean (SD) |
|---|---|---|---|
| Type of study | |||
| Case report | 298 | 94.3 | |
| Case series | 14 | 4.4 | |
| Diagnostic | 3 | 0.9 | |
| Case control | 1 | 0.3 | |
| N patients | 492 | ||
| Age | 429 | 87.2 | 48.9 y (±17.3) |
| Sex | |||
| M | 235 | 54.8 | |
| F | 169 | 39.4 | |
| Pain region | |||
| LBP | 243 | 49.4 | |
| CP | 117 | 23.8 | |
| UBP | 30 | 6.1 | |
| LBP–CP | 3 | 0.6 | |
| CP–UBP | 9 | 1.8 | |
| LBP–UBP | 90 | 18.3 | |
| Other symptoms | |||
| UL | 83 | 16.9 | |
| LL | 21 | 4.3 | |
| Dyspnea | 56 | 11.4 | |
| Cough | 39 | 7.9 | |
| Others | 147 | 29.9 | |
| Serious pathology | 474 | 96.3 | |
| Cardiovascular | 156 | 32.9 | |
| Pulmonary | 33 | 7.0 | |
| Tumor | 94 | 19.8 | |
| Fracture | 96 | 20.3 | |
| Visceral | 34 | 7.2 | |
| Infection | 32 | 6.8 | |
| Other | 29 | 6.1 | |
| Secondary impairment | |||
| Pathological fracture | 28 | 5.9 | |
| Spinal cord compression | 34 | 7.2 |
| Test | n | POS | n Serious | % Serious | NEG | n Serious | % Serious | HPP. | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | EE | % | PT | % | CH | % | NS | % | |||||||||
| T | 73 | 32 | 32 | 100.0 | 41 | 40 | 97.6 | 3 | 4.11 | 32 | 43.84 | 0 | 0.00 | 0 | 0.00 | 38 | 52.05 |
| Blood pressure | 108 | 57 | 54 | 94.7 | 51 | 48 | 94.1 | 14 | 12.96 | 54 | 50.00 | 1 | 0.93 | 1 | 0.93 | 38 | 35.19 |
| Heartbeat | 101 | 60 | 58 | 96.7 | 41 | 38 | 92.7 | 9 | 8.91 | 53 | 52.48 | 1 | 0.99 | 0 | 0.00 | 38 | 37.62 |
| Respiratory frequency | 55 | 35 | 34 | 97.1 | 20 | 19 | 95.0 | 4 | 7.27 | 27 | 49.09 | 0 | 0.00 | 0 | 0.00 | 23 | 41.82 |
| Saturation | 47 | 24 | 23 | 95.8 | 23 | 22 | 95.7 | 3 | 6.38 | 24 | 51.06 | 0 | 0.00 | 0 | 0.00 | 20 | 42.55 |
| Cardiac auscultation | 149 | 118 | 115 | 97.5 | 31 | 30 | 96.8 | 75 | 50.34 | 47 | 31.54 | 0 | 0.00 | 0 | 0.00 | 27 | 18.12 |
| Pulmonary auscultation | 114 | 84 | 80 | 95.2 | 30 | 30 | 100.0 | 17 | 14.91 | 46 | 40.35 | 0 | 0.00 | 0 | 0.00 | 52 | 45.61 |
| Babinski | 26 | 22 | 22 | 100.0 | 4 | 4 | 100.0 | 4 | 15.38 | 6 | 23.08 | 1 | 3.85 | 0 | 0.00 | 15 | 57.69 |
| Reflex | 50 | 32 | 31 | 96.9 | 18 | 17 | 94.4 | 8 | 16.00 | 9 | 18.00 | 5 | 10.00 | 1 | 2.00 | 27 | 54.00 |
| Sensory | 81 | 49 | 48 | 98.0 | 32 | 31 | 96.9 | 11 | 13.58 | 22 | 27.16 | 7 | 8.64 | 3 | 3.70 | 38 | 46.91 |
| Strength | 56 | 21 | 20 | 95.2 | 35 | 34 | 97.1 | 7 | 12.50 | 14 | 25.00 | 7 | 12.50 | 2 | 3.57 | 26 | 46.43 |
| SLR | 35 | 28 | 24 | 85.7 | 7 | 7 | 100.0 | 6 | 17.14 | 7 | 20.00 | 8 | 22.86 | 2 | 5.71 | 13 | 37.14 |
| SLUMP | 3 | 1 | 1 | 100.0 | 2 | 2 | 100.0 | 0 | 0.00 | 0 | 0.00 | 2 | 66.67 | 1 | 33.33 | 0 | 0.00 |
| Abdominal palpation | 55 | 18 | 17 | 94.4 | 37 | 37 | 100.0 | 10 | 18.18 | 19 | 34.55 | 4 | 7.27 | 2 | 3.64 | 20 | 36.36 |
| Costal/vertebral palpation | 46 | 39 | 37 | 94.9 | 7 | 7 | 100.0 | 14 | 30.43 | 9 | 19.57 | 4 | 8.70 | 1 | 2.17 | 18 | 39.13 |
| Lymph node palpation | 14 | 5 | 5 | 100.0 | 9 | 9 | 100.0 | 2 | 14.29 | 2 | 14.29 | 0 | 0.00 | 0 | 0.00 | 10 | 71.43 |
| Mass | 24 | 24 | 24 | 100.0 | 0 | 0 | 0.0 | 4 | 16.67 | 4 | 16.67 | 0 | 0.00 | 0 | 0.00 | 16 | 66.67 |
| Pulsatile mass | 8 | 8 | 7 | 87.5 | 0 | 0 | 0.0 | 2 | 25.00 | 2 | 25.00 | 1 | 12.50 | 2 | 25.00 | 1 | 12.50 |
| Inspection | 52 | 52 | 51 | 98.1 | 0 | 0 | 0.0 | 2 | 3.85 | 29 | 55.77 | 0 | 0.00 | 1 | 1.92 | 20 | 38.46 |
| Other tests | |||||||||||||||||
| ∆ pressure UL | 3 | 3 | 3 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 3 | 100.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Pulmonary percussion | 11 | 11 | 10 | 90.9 | 0 | 0 | 0.0 | 3 | 27.27 | 3 | 27.27 | 0 | 0.00 | 0 | 0.00 | 5 | 45.45 |
| Anal/rectal examination | 11 | 8 | 8 | 100.0 | 3 | 3 | 100.0 | 0 | 0.00 | 4 | 36.36 | 1 | 9.09 | 0 | 0.00 | 6 | 54.55 |
| Abdominal auscultation | 4 | 4 | 3 | 75.0 | 0 | 0 | 0.0 | 0 | 0.00 | 1 | 25.00 | 0 | 0.00 | 1 | 25.00 | 2 | 50.00 |
| Costovertebral angle | 6 | 6 | 6 | 100.0 | 0 | 0 | 0.0 | 3 | 50.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 3 | 50.00 |
| Peripheral pulses | 17 | 7 | 7 | 100.0 | 10 | 9 | 90.0 | 1 | 5.88 | 10 | 58.82 | 1 | 5.88 | 0 | 0.00 | 5 | 29.41 |
| ROM spine | 11 | 4 | 4 | 100.0 | 7 | 7 | 100.0 | 2 | 18.18 | 0 | 0.00 | 5 | 45.45 | 2 | 18.18 | 2 | 18.18 |
| ROM hip | 9 | 6 | 6 | 100.0 | 3 | 3 | 100.0 | 0 | 0.00 | 1 | 11.11 | 4 | 44.44 | 1 | 11.11 | 3 | 33.33 |
| FABER | 3 | 2 | 2 | 100.0 | 1 | 1 | 100.0 | 0 | 0.00 | 1 | 33.33 | 1 | 33.33 | 0 | 0.00 | 1 | 33.33 |
| Bicycle test | 2 | 2 | 2 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 2 | 100.00 | 0 | 0.00 | 0 | 0.00 |
| Close fist percussion test | 45 | 45 | 42 | 93.3 | 0 | 0 | 0.0 | 42 | 93.33 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 3 | 6.67 |
| Supine sign | 41 | 41 | 39 | 95.1 | 0 | 0 | 0.0 | 30 | 73.17 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Spinal percussion | 4 | 4 | 4 | 100.0 | 0 | 0 | 0.0 | 1 | 25.00 | 1 | 25.00 | 1 | 25.00 | 0 | 0.00 | 1 | 25.00 |
| Psoas test | 3 | 2 | 2 | 100.0 | 1 | 1 | 100.0 | 0 | 0.00 | 1 | 33.33 | 1 | 33.33 | 0 | 0.00 | 1 | 33.33 |
| Subcutaneus emphysema | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 1 | 100.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Pulsus paradoxus | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 |
| PROM of different joints | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 |
| Romberg | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 | 0 | 0.00 | 0 | 0.00 |
| Tinel’s sign (sciatic nerve) | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 1 | 100.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Mennel’s sign | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 1 | 100.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Sacroiliac compression | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 | 0 | 0.00 |
| Lhermitte’s sign | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 |
| Tuning fork test | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 | 0 | 0.00 | 0 | 0.00 |
| Beevor’s sign | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 |
| Altered muscle tone | 1 | 1 | 1 | 100.0 | 0 | 0 | 0.0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 |
| Clonus test | 1 | 0 | 0 | 0 | 1 | 1 | 100.0 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 | 0 | 0.00 | 0 | 0.00 |
| Breast palpation | 1 | 0 | 0 | 0 | 1 | 1 | 100.0 | 0 | 0.00 | 1 | 100.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Item | n | % |
|---|---|---|
| Primary Healthcare Professional | ||
| Physician | 197 | 40.0 |
| Emergency equipped | 126 | 25.6 |
| Physiotherapist | 13 | 2.6 |
| Chiropractor | 4 | 0.8 |
| Not specified | 152 | 30.9 |
| Direct access | ||
| 1° | 337 | 68.5 |
| 2° | 29 | 5.9 |
| 3° | 5 | 1.0 |
| >3° | 6 | 1.2 |
| See and treat | 1 | 0.2 |
| Not specified | 114 | 23.2 |
| Positive Test | n | % |
|---|---|---|
| T | 4 | 12.1 |
| Blood pressure | 5 | 15.2 |
| Heartbeat | 5 | 15.2 |
| Respiratory frequency | 1 | 3.0 |
| Saturation | 1 | 3.0 |
| Cardiac auscultation | 1 | 3.0 |
| Pulmonary auscultation | 5 | 15.2 |
| Babinski | 6 | 18.2 |
| Reflex | 5 | 15.2 |
| Sensory | 5 | 15.2 |
| Strength | 4 | 12.1 |
| SLR | 3 | 9.1 |
| Abdominal palpation | 3 | 9.1 |
| Costal/vertebral palpation | 2 | 6.1 |
| Pulsatile mass | 1 | 3.0 |
| Inspection | 1 | 3.0 |
| Other tests | ||
| Pulmonary percussion | 1 | 3.0 |
| Peripheral pulses | 4 | 12.1 |
| ROM spine | 2 | 6.1 |
| ROM hip | 3 | 9.1 |
| Bicycle test | 2 | 6.1 |
| Psoas test | 1 | 3.0 |
| Tuning fork test | 1 | 3.0 |
| Spinal percussion | 1 | 3.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreoletti, F.; Maselli, F.; Storari, L.; Vongher, A.; Erbesato, M.; Testa, M.; Turolla, A. Screening for Referral of Serious Pathology by Physical Examination Tests in Patients with Back or Chest Pain: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 16418. https://doi.org/10.3390/ijerph192416418
Andreoletti F, Maselli F, Storari L, Vongher A, Erbesato M, Testa M, Turolla A. Screening for Referral of Serious Pathology by Physical Examination Tests in Patients with Back or Chest Pain: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(24):16418. https://doi.org/10.3390/ijerph192416418
Chicago/Turabian StyleAndreoletti, Federico, Filippo Maselli, Lorenzo Storari, Andrea Vongher, Monica Erbesato, Marco Testa, and Andrea Turolla. 2022. "Screening for Referral of Serious Pathology by Physical Examination Tests in Patients with Back or Chest Pain: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 24: 16418. https://doi.org/10.3390/ijerph192416418
APA StyleAndreoletti, F., Maselli, F., Storari, L., Vongher, A., Erbesato, M., Testa, M., & Turolla, A. (2022). Screening for Referral of Serious Pathology by Physical Examination Tests in Patients with Back or Chest Pain: A Systematic Review. International Journal of Environmental Research and Public Health, 19(24), 16418. https://doi.org/10.3390/ijerph192416418








