Effect of Flat Running Shoes on Hip Kinematics in Male Recreational Runners
Abstract
1. Introduction
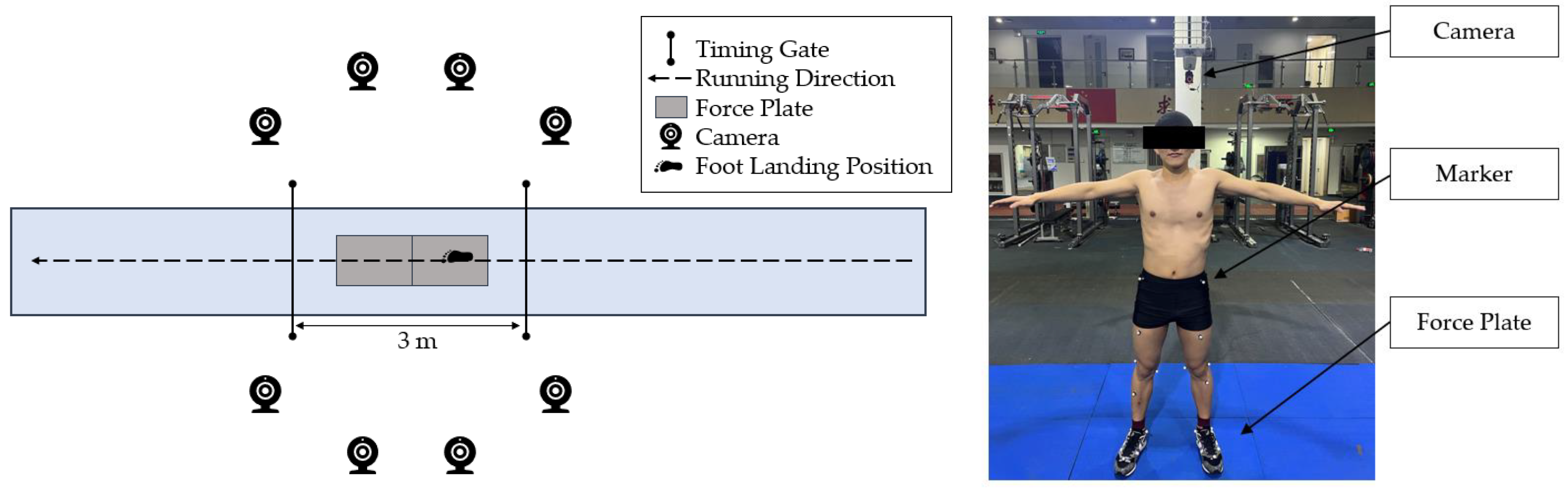
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Data Collection
2.4. Data Reduction
2.5. Statistical Analysis
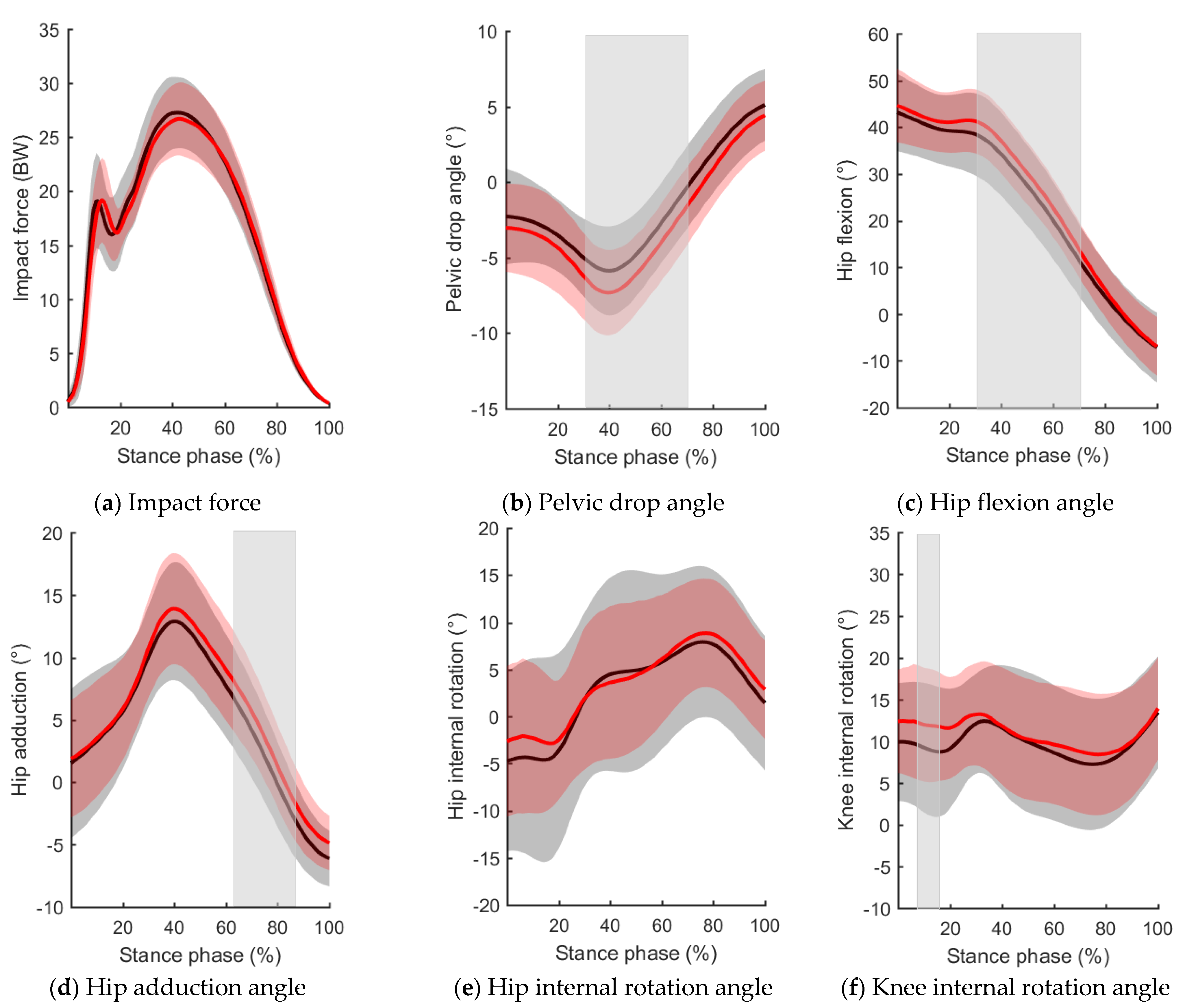
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, D.C.; Pate, R.R.; Lavie, C.J.; Sui, X.; Church, T.S.; Blair, S.N. Leisure−time running reduces all−cause and cardiovascular mortality risk. J. Am. Coll. Cardiol 2014, 64, 472–481. [Google Scholar] [CrossRef]
- Van Gent, R.N.; Siem, D.; Van Middelkoop, M.; Van, A.G.; Bierma−Zeinstra, S.M.A.; Koes, B.W. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br. J. Sports Med. 2007, 41, 469–480. [Google Scholar] [CrossRef]
- Reijnders, L.; Van De Groes, S.A. The quality of life of patients with patellofemoral pain—A systematic review. Acta Orthop. Belg. 2020, 86, 678–687. [Google Scholar]
- Wyndow, N.; Collins, N.; Vicenzino, B.; Tucker, K.; Crossley, K. Is there a biomechanical link between patellofemoral pain and osteoarthritis? A narrative review. Sports Med. 2016, 46, 1797–1808. [Google Scholar] [CrossRef]
- Finnoff, J.T.; Hall, M.M.; Kyle, K.; Krause, D.A.; Lai, J.; Smith, J. Hip strength and knee pain in high school runners: A prospective study. PM&R 2011, 3, 792–801. [Google Scholar]
- Thijs, Y.; Pattyn, E.; Van Tiggelen, D.; Rombaut, L.; Witvrouw, E. Is hip muscle weakness a predisposing factor for patellofemoral pain in female novice runners? A prospective study. Am. J. Sports Med. 2011, 39, 1877–1882. [Google Scholar] [CrossRef]
- Rathleff, M.S.; Rathleff, C.R.; Crossley, K.M.; Barton, C.J. Is hip strength a risk factor for patellofemoral pain? A systematic review and meta−analysis. Br. J. Sports Med. 2014, 48, 1088. [Google Scholar] [CrossRef]
- Boling, M.C.; Padua, D.A.; Marshall, S.W.; Guskiewicz, K.; Pyne, S.; Beutler, A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: The Joint Undertaking to Monitor and Prevent ACL Injury (JUMP−ACL) cohort. Am. J. Sports Med. 2009, 37, 2108–2116. [Google Scholar] [CrossRef]
- Noehren, B.; Hamill, J.; Davis, I. Prospective evidence for a hip etiology in patellofemoral pain. Med. Sci. Sports Exerc. 2013, 45, 1120–1124. [Google Scholar] [CrossRef]
- Neal, B.S.; Barton, C.J.; Gallie, R.; Ohalloran, P.; Morrissey, D. Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: A systematic review and meta−analysis. Gait Posture 2015, 11, 1–10. [Google Scholar] [CrossRef]
- Witvrouw, E.; Callaghan, M.J.; Stefanik, J.J.; Noehren, B.; Bazett−Jones, D.M.; Willson, J.D.; Earl−Boehm, J.E.; Davis, I.S.; Powers, C.M.; Mcconnell, J.; et al. Patellofemoral pain: Consensus statement from the 3rd International Patellofemoral Pain Research Retreat held in Vancouver, September 2013. Br. J. Sports Med. 2014, 48, 411–414. [Google Scholar] [CrossRef]
- Goodfellow, J.; Hungerford, D.S.; Woods, C. Patello−femoral joint mechanics and pathology 2. Chondromalacia patellae. J. Bone Jt. Surg. BR. 1976, 58, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Defrate, L.E.; Zayontz, S.; Park, S.E.; Gill, T.J. The effect of tibiofemoral joint kinematics on patellofemoral contact pressures under simulated muscle loads. J. Orthop. Res. 2004, 22, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Besier, T.F.; Gold, G.E.; Delp, S.L.; Fredericson, M.; Beaupré, G.S. The influence of femoral internal and external rotation on cartilage stresses within the patellofemoral joint. J. Orthop. Res. 2008, 26, 1627–1635. [Google Scholar] [CrossRef] [PubMed]
- Noehren, B.; Scholz, J.; Davis, I. The effect of real−time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br. J. Sports Med. 2011, 45, 691–696. [Google Scholar] [CrossRef]
- Willy, R.W.; Scholz, J.P.; Davis, I.S. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin. Biomech. 2012, 27, 1045–1051. [Google Scholar] [CrossRef]
- Noehren, B.; Davis, I.; Hamill, J. ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin. Biomech. 2007, 22, 951–956. [Google Scholar] [CrossRef]
- Ceyssens, L.; Vanelderen, R.; Barton, C.; Malliaras, P.; Dingenen, B. Biomechanical risk factors associated with running−related injuries: A systematic review. Sports Med. 2019, 49, 1095–1115. [Google Scholar] [CrossRef]
- Ferber, R.; Noehren, B.; Hamill, J.; Davis, I.S. Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J. Orthop. Sports Phys. Ther. 2010, 40, 52–58. [Google Scholar] [CrossRef]
- Noehren, B.; Schmitz, A.; Hempel, R.; Westlake, C.; Black, W. Assessment of strength, flexibility, and running mechanics in men with iliotibial band syndrome. J. Orthop. Sports Phys. Ther. 2014, 44, 217–222. [Google Scholar] [CrossRef]
- Foch, E.; Milner, C.E. Frontal plane running biomechanics in female runners with previous iliotibial band syndrome. J. Appl. Biomech. 2014, 30, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Fredericson, M.; Cookingham, C.L.; Chaudhari, A.M.; Dowdell, B.C.; Oestreicher, N.; Sahrmann, S.A. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin. J. Sport Med. 2000, 10, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Neal, B.S.; Lack, S.D.; Lankhorst, N.E.; Raye, A.; Morrissey, D.; Van Middelkoop, M. Risk factors for patellofemoral pain: A systematic review and meta−analysis. Br. J. Sports Med. 2019, 53, 270–281. [Google Scholar] [CrossRef] [PubMed]
- Meira, E.P.; Brumitt, J. Influence of the hip on patients with patellofemoral pain syndrome: A systematic review. Sports Health 2011, 3, 455–465. [Google Scholar] [CrossRef] [PubMed]
- Davis, I.S.; Tenforde, A.S.; Neal, B.S.; Roper, J.L.; Willy, R.W. Gait retraining as an intervention for patellofemoral pain. Curr. Rev. Musculoske 2020, 13, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Fyock, M.; Cortes, N.; Hulse, A.; Martin, J. Gait retraining with real−time visual feedback to treat patellofemoral pain in adult recreational runners: A critically appraised topic. J. Sport Rehabil. 2020, 29, 675–679. [Google Scholar] [CrossRef]
- Bramah, C.; Preece, S.J.; Gill, N.; Herrington, L. A 10% increase in step rate improves running kinematics and clinical outcomes in runners with patellofemoral pain at 4 weeks and 3 months. Am. J. Sports Med. 2019, 47, 3406–3413. [Google Scholar] [CrossRef]
- Roper, J.L.; Harding, E.M.; Doerfler, D.; Dexter, J.G.; Kravitz, L.; Dufek, J.S.; Mermier, C.M. The effects of gait retraining in runners with patellofemoral pain: A randomized trial. Clin. Biomech. 2016, 35, 14–22. [Google Scholar] [CrossRef]
- Bonacci, J.; Hall, M.; Fox, A.; Saunders, N.; Shipsides, T.; Vicenzino, B. The influence of cadence and shoes on patellofemoral joint kinetics in runners with patellofemoral pain. J. Sci. Med. Sport 2018, 21, 574–578. [Google Scholar] [CrossRef]
- Knorz, S.; Kluge, F.; Gelse, K.; Schulz−Drost, S.; Hotfiel, T.; Lochmann, M.; Eskofier, B.; Krinner, S. Three−dimensional biomechanical analysis of rearfoot and forefoot running. Orthop. J. Sports Med. 2017, 5, 1–7. [Google Scholar] [CrossRef]
- Esculier, J.F.; Dubois, B.; Bouyer, L.J.; Mcfadyen, B.J.; Roy, J.S. Footwear characteristics are related to running mechanics in runners with patellofemoral pain. Gait Posture. 2017, 54, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Shi, H.; Liu, H.; Zhou, X. Biomechanical analysis of running in shoes with different heel−to−toe drops. Appl. Sci. 2021, 11, 12144. [Google Scholar] [CrossRef]
- Bonacci, J.; Vicenzino, B.; Spratford, W.; Collins, P. Take your shoes off to reduce patellofemoral joint stress during running. Br. J. Sports Med. 2014, 48, 425–433. [Google Scholar] [CrossRef]
- Yang, C.; Xiao, S.; Yang, Y.; Zhang, X.; Wang, J.; Fu, W. Patellofemoral joint loads during running immediately changed by shoes with different minimalist indices: A cross−sectional study. Appl. Sci. 2019, 9, 4176. [Google Scholar] [CrossRef]
- Sinclair, J.; Richards, J.; Selfe, J.; Fau−Goodwin, J.; Shore, H. The influence of minimalist and maximalist footwear on patellofemoral kinetics during running. J. Appl. Biomech. 2016, 32, 359–364. [Google Scholar] [CrossRef]
- Besson, T.; Morio, C.; Millet, G.Y.; Rossi, J. Influence of shoe drop on running kinematics and kinetics in female runners. Eur. J. Sport Sci. 2019, 19, 1320–1327. [Google Scholar] [CrossRef]
- Kim, H.K.; Mei, Q.; Gu, Y.; Mirjalili, A.; Fernandez, J. Reduced joint reaction and muscle forces with barefoot running. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 1263–1273. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhou, X.; Zhang, L.; Liu, H.; Yu, B. The effect of heel−to−toe drop of running shoes on patellofemoral joint stress during running. Gait Posture. 2022, 93, 230–234. [Google Scholar] [CrossRef]
- Bonacci, J.; Saunders, P.U.; Hicks, A.; Rantalainen, T.; Vicenzino, B.T.; Spratford, W. Running in a minimalist and lightweight shoe is not the same as running barefoot: A biomechanical study. Br. J. Sports Med. 2013, 47, 387–392. [Google Scholar] [CrossRef]
- Squadrone, R.; Rodano, R.; Hamill, J.; Preatoni, E. Acute effect of different minimalist shoes on foot strike pattern and kinematics in rearfoot strikers during running. J. Sports Sci. 2015, 33, 1196–1204. [Google Scholar] [CrossRef]
- Sinclair, J. Effects of barefoot and barefoot inspired footwear on knee and ankle loading during running. Clin. Biomech. 2014, 29, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Altman, A.R.; Davis, I.S. A kinematic method for footstrike pattern detection in barefoot and shod runners. Gait Posture 2012, 35, 298–300. [Google Scholar] [CrossRef] [PubMed]
- Plaza−Bravo, J.M.; Mateo−March, M.; Sanchis−Sanchis, R.; Pérez−Soriano, P.; Zabala, M.; Encarnación−Martínez, A. Validity and reliability of the leomo motion−tracking device based on inertial measurement unit with an optoelectronic camera system for cycling pedaling evaluation. Int. J. Environ. Res. Public Heal. 2022, 19, 8375. [Google Scholar] [CrossRef] [PubMed]
- Gray, A.D.; Willis, B.W.; Skubic, M.; Huo, Z.; Razu, S.; Sherman, S.L.; Guess, T.M.; Jahandar, A.; Gulbrandsen, T.R.; Miller, S.; et al. Development and validation of a portable and inexpensive tool to measure the drop vertical jump using the Microsoft Kinect V2. Sport. Health 2017, 9, 537–544. [Google Scholar] [CrossRef]
- Vonstad, E.K.; Su, X.; Vereijken, B.; Bach, K.; Nilsen, J.H. Comparison of a deep learning−based pose estimation system to marker−based and kinect systems in exergaming for balance training. Sensors 2020, 20, 6940. [Google Scholar] [CrossRef]
- Wu, G. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion−PartI: Ankle, hip, and spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Pohl, M.B.; Patel, C.; Wiley, J.P.; Ferber, R. Gait biomechanics and hip muscular strength in patients with patellofemoral osteoarthritis. Gait Posture 2013, 37, 440–444. [Google Scholar] [CrossRef]
- Friston, K.J.; Ashburner, J.T.; Kiebel, S.J.; Nichols, T.E.J.N. Statistical Parametric Mapping: The Analysis of Functional Brain Images M; Academic Press: Pittsburgh, PA, USA, 2007. [Google Scholar]
- Mccarthy, C.; Fleming, N.; Donne, B.; Blanksby, B. Barefoot running and hip kinematics: Good news for the knee? Med. Sci. Sports Exerc. 2015, 47, 1009–1016. [Google Scholar] [CrossRef]
- Donnelly, C.J.; Alexander, C.; Pataky, T.C.; Stannage, K.; Reid, S.; Robinson, M.A. Vector−field statistics for the analysis of time varying clinical gait data. Clin. Biomech. 2017, 41, 87–91. [Google Scholar] [CrossRef]
- Lopes, A.D.; Hespanhol, L.C.; Yeung, S.S.; Costa, L.O.P. What are the main running−related musculoskeletal injuries? Sports Med. 2012, 42, 891–905. [Google Scholar] [CrossRef]
- Jiang, X.; Zhou, H.; Quan, W.; Hu, Q.; Baker, J.S.; Gu, Y. Ground reaction force differences between bionic shoes and neutral running shoes in recreational male runners before and after a 5 km run. Int. J. Environ. Res. Public Heal. 2021, 18, 9787. [Google Scholar] [CrossRef] [PubMed]
- Kulmala, J.P.; Avela, J.; Pasanen, K.; Parkkari, J. Forefoot strikers exhibit lower running−induced knee loading than rearfoot strikers. Med. Sci. Sports Exerc. 2013, 45, 2306–2313. [Google Scholar] [CrossRef] [PubMed]
- Boyer, E.R.; Derrick, T.R. Select injury−related variables are affected by stride length and foot strike style during running. Am. J. Sports Med. 2015, 43, 2310–2317. [Google Scholar] [CrossRef] [PubMed]
- Malisoux, L.; Chambon, N.; Urhausen, A.; Theisen, D. Influence of the heel−to−toe drop of standard cushioned running shoes on injury risk in leisure−time runners: A randomized controlled trial with 6−month follow−up. Am. J. Sports Med. 2016, 44, 2933–2940. [Google Scholar] [CrossRef] [PubMed]
- Almonroeder, T.G.; Benson, L.C. Sex differences in lower extremity kinematics and patellofemoral kinetics during running. J. Sports Sci. 2017, 35, 1575–1581. [Google Scholar] [CrossRef]

| Variable | Flat | 10 mm Drop | p−Value | Effect Size |
|---|---|---|---|---|
| Speed (m/s) | 4.0 ± 0.1 | 4.0 ± 0.2 | 0.710 | 0.02 |
| Step length (m) | 1.47 ± 0.10 | 1.50 ± 0.11 | 0.272 | 0.29 |
| Step frequency (steps/min) | 164.1 ± 12.6 | 161.7 ± 9.6 | 0.304 | 0.21 |
| Foot inclination angle at initial contact (°) | 22.6 ± 8.5 | 28.3 ± 7.6 | 0.001 | 0.71 |
| Impact peak (BW) | 2.05 ± 0.40 | 2.03 ± 0.35 | 0.820 | 0.05 |
| Active peak (BW) | 2.75 ± 0.33 | 2.70 ± 0.33 | 0.363 | 0.15 |
| Variable | Flat | 10 mm Drop | p−Value | Effect Size |
|---|---|---|---|---|
| Flexion angle at initial contact (°) | 43.6 ± 8.5 | 44.6 ± 8.1 | 0.270 | 0.18 |
| Adduction angle at initial contact (°) | 1.8 ± 3.1 | 1.9 ± 2.9 | 0.561 | 0.04 |
| Internal rotation angle at initial contact (°) | 4.8 ± 5.8 | 2.6 ± 4.2 | 0.158 | 0.24 |
| Peak contralateral pelvic drop (°) | 6.1 ± 2.7 | 7.5 ± 2.8 | 0.003 | 0.51 |
| Peak flexion angle (°) | 43.4 ± 8.4 | 44.8 ± 8.0 | 0.282 | 0.17 |
| Peak adduction angle (°) | 13.3 ± 4.3 | 14.1 ± 4.7 | 0.161 | 0.18 |
| Peak internal rotation angle (°) | 9.9 ± 8.2 | 10.1 ± 6.5 | 0.837 | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, M.; Cui, J.; Liu, H. Effect of Flat Running Shoes on Hip Kinematics in Male Recreational Runners. Int. J. Environ. Res. Public Health 2022, 19, 16473. https://doi.org/10.3390/ijerph192416473
Zhang M, Cui J, Liu H. Effect of Flat Running Shoes on Hip Kinematics in Male Recreational Runners. International Journal of Environmental Research and Public Health. 2022; 19(24):16473. https://doi.org/10.3390/ijerph192416473
Chicago/Turabian StyleZhang, Masen, Jing Cui, and Hui Liu. 2022. "Effect of Flat Running Shoes on Hip Kinematics in Male Recreational Runners" International Journal of Environmental Research and Public Health 19, no. 24: 16473. https://doi.org/10.3390/ijerph192416473
APA StyleZhang, M., Cui, J., & Liu, H. (2022). Effect of Flat Running Shoes on Hip Kinematics in Male Recreational Runners. International Journal of Environmental Research and Public Health, 19(24), 16473. https://doi.org/10.3390/ijerph192416473





