Childhood Obesity and Incorrect Body Posture: Impact on Physical Activity and the Therapeutic Role of Exercise
Abstract
1. Introduction
2. Materials and Methods
3. Childhood Obesity
3.1. Risk Factors
3.2. Complications
3.3. Treatment
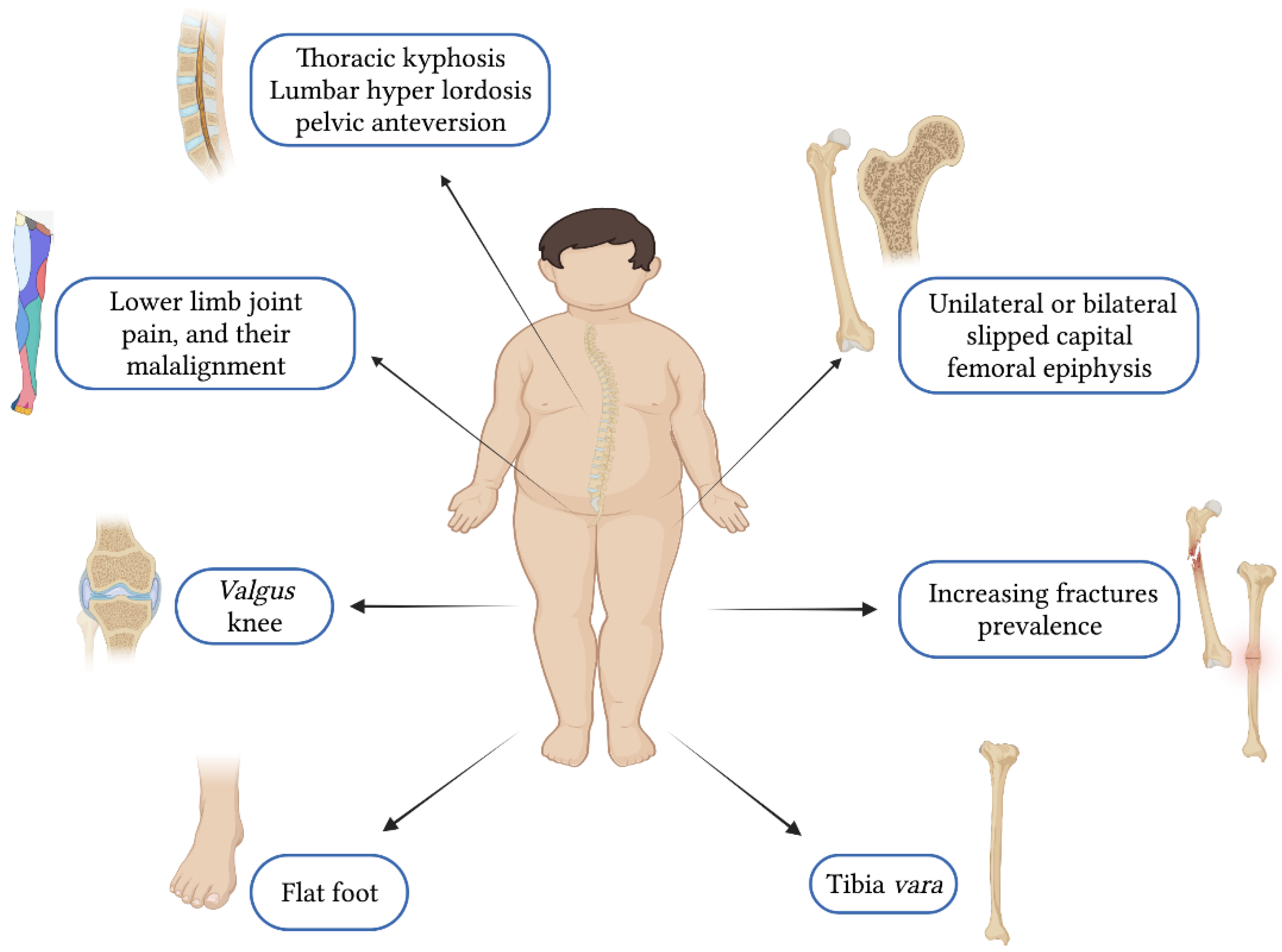
4. Incorrect Body Posture in Children and Adolescents with Obesity
5. Impact of Body Posture on Physical Activity in Childhood Obesity
6. Therapeutic Exercise Benefits for Incorrect Body Posture
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization WHO Obesity. Available online: https://www.who.int/health-topics/obesity (accessed on 25 November 2022).
- Kumar, S.; Kelly, A.S. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin. Proc. 2017, 92, 251–265. [Google Scholar] [CrossRef]
- Sahoo, K.; Sahoo, B.; Choudhury, A.; Sofi, N.; Kumar, R.; Bhadoria, A. Childhood Obesity: Causes and Consequences. J. Fam. Med. Prim. Care 2015, 4, 187. [Google Scholar] [CrossRef]
- Wijnhoven, T.M.A.; van Raaij, J.M.A.; Spinelli, A.; Starc, G.; Hassapidou, M.; Spiroski, I.; Rutter, H.; Martos, É.; Rito, A.I.; Hovengen, R.; et al. WHO European Childhood Obesity Surveillance Initiative: Body Mass Index and Level of Overweight among 6-9-Year-Old Children from School Year 2007/2008 to School Year 2009/2010. BMC Public Health 2014, 14, 806. [Google Scholar] [CrossRef]
- Rito, A.I.; Buoncristiano, M.; Spinelli, A.; Salanave, B.; Kunešová, M.; Hejgaard, T.; García Solano, M.; Fijałkowska, A.; Sturua, L.; Hyska, J.; et al. Association between Characteristics at Birth, Breastfeeding and Obesity in 22 Countries: The WHO European Childhood Obesity Surveillance Initiative—COSI 2015/2017. Obes. Facts 2019, 12, 226–243. [Google Scholar] [CrossRef]
- Wyszyńska, J.; Podgórska-Bednarz, J.; Drzał-Grabiec, J.; Rachwał, M.; Baran, J.; Czenczek-Lewandowska, E.; Leszczak, J.; Mazur, A. Analysis of Relationship between the Body Mass Composition and Physical Activity with Body Posture in Children. BioMed Res. Int. 2016, 2016, 1851670. [Google Scholar] [CrossRef]
- Maciałczyk-Paprocka, K.; Stawińska-Witoszyńska, B.; Kotwicki, T.; Sowińska, A.; Krzyżaniak, A.; Walkowiak, J.; Krzywińska-Wiewiorowska, M. Prevalence of Incorrect Body Posture in Children and Adolescents with Overweight and Obesity. Eur. J. Pediatr. 2017, 176, 563–572. [Google Scholar] [CrossRef]
- Calcaterra, V.; Zuccotti, G. Physical Exercise as a Non-Pharmacological Intervention for Attenuating Obesity-Related Complications in Children and Adolescents. Int. J. Environ. Res. Public. Health 2022, 19, 5046. [Google Scholar] [CrossRef]
- Herman, R.; Mixon, J.; Fisher, A.; Maulucci, R.; Stuyck, J. Idiopathic Scoliosis and the Central Nervous System: A Motor Control Problem. The Harrington Lecture, 1983. Scoliosis Research Society. Spine 1985, 10, 1–14. [Google Scholar] [CrossRef]
- Marin, L.; Kawczyński, A.; Carnevale Pellino, V.; Febbi, M.; Silvestri, D.; Pedrotti, L.; Lovecchio, N.; Vandoni, M. Displacement of Centre of Pressure during Rehabilitation Exercise in Adolescent Idiopathic Scoliosis Patients. J. Clin. Med. 2021, 10, 2837. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Fakhouri, T.H.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of Obesity Among Youths by Household Income and Education Level of Head of Household—United States 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 186–189. [Google Scholar] [CrossRef]
- Bryan, S.; Afful, J.; Carroll, M.; Te-Ching, C.; Orlando, D.; Fink, S.; Fryar, C. NHSR 158. National Health and Nutrition Examination Survey 2017–March 2020 Pre-Pandemic Data Files; National Center for Health Statistics (U.S.): Hyattsville, MD, USA, 2021. [Google Scholar]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- McGuire, S. World Health Organization. Comprehensive Implementation Plan on Maternal, Infant, and Young Child Nutrition. Geneva, Switzerland, 2014. Adv. Nutr. 2015, 6, 134–135. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Regional Office for Europe Gaining Health: The European Strategy for the Prevention and Control of Noncommunicable Diseases; World Health Organization, Regional Office for Europe: Geneva, Switzerland, 2006; ISBN 978-92-890-2179-1.
- Purnell, J.Q. Definitions, Classification, and Epidemiology of Obesity. In Endotext; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Hershman, J.M., Hofland, J., Kalra, S., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Ogden, C.L. Defining Overweight in Children Using Growth Charts. Md. Med. MM Publ. MEDCHI Md. State Med. Soc. 2004, 5, 19–21. [Google Scholar]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 23 August 2022).
- Lolmède, K.; Duffaut, C.; Zakaroff-Girard, A.; Bouloumié, A. Immune Cells in Adipose Tissue: Key Players in Metabolic Disorders. Diabetes Metab. 2011, 37, 283–290. [Google Scholar] [CrossRef]
- Chatzigeorgiou, A.; Karalis, K.P.; Bornstein, S.R.; Chavakis, T. Lymphocytes in Obesity-Related Adipose Tissue Inflammation. Diabetologia 2012, 55, 2583–2592. [Google Scholar] [CrossRef]
- Murano, I.; Barbatelli, G.; Parisani, V.; Latini, C.; Muzzonigro, G.; Castellucci, M.; Cinti, S. Dead Adipocytes, Detected as Crown-like Structures, Are Prevalent in Visceral Fat Depots of Genetically Obese Mice. J. Lipid Res. 2008, 49, 1562–1568. [Google Scholar] [CrossRef]
- Mărginean, C.O.; Meliţ, L.E.; Ghiga, D.V.; Mărginean, M.O. Early Inflammatory Status Related to Pediatric Obesity. Front. Pediatr. 2019, 7, 241. [Google Scholar] [CrossRef]
- Eckersall, P.D. Acute Phase Proteins as Markers of Inflammatory Lesions. Comp. Haematol. Int. 1995, 5, 93–97. [Google Scholar] [CrossRef]
- Sommer, A.; Twig, G. The Impact of Childhood and Adolescent Obesity on Cardiovascular Risk in Adulthood: A Systematic Review. Curr. Diabetes Rep. 2018, 18, 91. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Pascuzzi, M.C.; Magenes, V.C.; Fiore, G.; Di Profio, E.; Tenuta, E.; Bosetti, A.; Todisco, C.F.; D’Auria, E.; et al. Metabolic Derangement in Pediatric Patient with Obesity: The Role of Ketogenic Diet as Therapeutic Tool. Nutrients 2021, 13, 2805. [Google Scholar] [CrossRef]
- Calcaterra, V.; Regalbuto, C.; Porri, D.; Pelizzo, G.; Mazzon, E.; Vinci, F.; Zuccotti, G.; Fabiano, V.; Cena, H. Inflammation in Obesity-Related Complications in Children: The Protective Effect of Diet and Its Potential Role as a Therapeutic Agent. Biomolecules 2020, 10, 1324. [Google Scholar] [CrossRef] [PubMed]
- Bradwisch, S.A.; Smith, E.M.; Mooney, C.; Scaccia, D. Obesity in Children and Adolescents: An Overview. Nursing 2020, 50, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Corica, D.; Oreto, L.; Pepe, G.; Calabrò, M.P.; Longobardo, L.; Morabito, L.; Pajno, G.B.; Alibrandi, A.; Aversa, T.; Wasniewska, M. Precocious Preclinical Cardiovascular Sonographic Markers in Metabolically Healthy and Unhealthy Childhood Obesity. Front. Endocrinol. 2020, 11, 56. [Google Scholar] [CrossRef]
- Di Bonito, P.; Licenziati, M.R.; Corica, D.; Wasniewska, M.G.; Di Sessa, A.; del Giudice, E.M.; Morandi, A.; Maffeis, C.; Faienza, M.F.; Mozzillo, E.; et al. Phenotypes of Prediabetes and Metabolic Risk in Caucasian Youths with Overweight or Obesity. J. Endocrinol. Investig. 2022, 45, 1719–1727. [Google Scholar] [CrossRef] [PubMed]
- Di Bonito, P.; Licenziati, M.R.; Morandi, A.; Maffeis, C.; Miraglia del Giudice, E.; Di Sessa, A.; Campana, G.; Wasniewska, M.; Corica, D.; Valerio, G. Screening for Hypertension in Young People with Obesity: Feasibility in the Real Life. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 1301–1307. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Klersy, C.; Muratori, T.; Telli, S.; Caramagna, C.; Scaglia, F.; Cisternino, M.; Larizza, D. Prevalence of Metabolic Syndrome (MS) in Children and Adolescents with Varying Degrees of Obesity. Clin. Endocrinol. 2008, 68, 868–872. [Google Scholar] [CrossRef]
- Jiménez-Cebrián, A.; Roman-Bravo, P.; Morente-Bernal, M.; Alonso-Ríos, J.; De-la-Cruz-Torres, B.; Romero-Morales, C.; Navarro-Flores, E.; Montiel-Luque, A. Influence of Childhood Overweight and Obesity on Foot and Lower Limb Pain in a Population of Primary School Children. Arch. Med. Sci. 2020. [Google Scholar] [CrossRef]
- Martin, R.M. Breastfeeding in Infancy and Blood Pressure in Later Life: Systematic Review and Meta-Analysis. Am. J. Epidemiol. 2005, 161, 15–26. [Google Scholar] [CrossRef] [PubMed]
- de Onis, M.; Garza, C.; Onyango, A.W.; Borghi, E. Comparison of the WHO Child Growth Standards and the CDC 2000 Growth Charts. J. Nutr. 2007, 137, 144–148. [Google Scholar] [CrossRef]
- Chan, G.; Chen, C.T. Musculoskeletal Effects of Obesity. Curr. Opin. Pediatr. 2009, 21, 65–70. [Google Scholar] [CrossRef]
- Bhatia, N.N.; Pirpiris, M.; Otsuka, N.Y. Body Mass Index in Patients with Slipped Capital Femoral Epiphysis. J. Pediatr. Orthop. 2006, 26, 197–199. [Google Scholar] [CrossRef] [PubMed]
- Valerio, G.; Maffeis, C.; Saggese, G.; Ambruzzi, M.A.; Balsamo, A.; Bellone, S.; Bergamini, M.; Bernasconi, S.; Bona, G.; Calcaterra, V.; et al. Diagnosis, Treatment and Prevention of Pediatric Obesity: Consensus Position Statement of the Italian Society for Pediatric Endocrinology and Diabetology and the Italian Society of Pediatrics. Ital. J. Pediatr. 2018, 44, 88. [Google Scholar] [CrossRef] [PubMed]
- Isasi, C.R.; Parrinello, C.M.; Jung, M.M.; Carnethon, M.R.; Birnbaum-Weitzman, O.; Espinoza, R.A.; Penedo, F.J.; Perreira, K.M.; Schneiderman, N.; Sotres-Alvarez, D.; et al. Psychosocial Stress Is Associated with Obesity and Diet Quality in Hispanic/Latino Adults. Ann. Epidemiol. 2015, 25, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Kluge, H.H.P.; WHO. WHO European Regional Obesity Report 2022; WHO: Geneva, Switzerland, 2022; ISBN 978-92-890-5773-8. [Google Scholar]
- Garnett, S.P.; Cowell, C.T.; Baur, L.A.; Shrewsbury, V.A.; Chan, A.; Crawford, D.; Salmon, J.; Campbell, K.; Boulton, T.J. Increasing Central Adiposity: The Nepean Longitudinal Study of Young People Aged 7–8 to 12–13 y. Int. J. Obes. 2005, 29, 1353–1360. [Google Scholar] [CrossRef]
- Baker, J.L.; Farpour-Lambert, N.J.; Nowicka, P.; Pietrobelli, A.; Weiss, R. Childhood Obesity Task Force of the European Association for the Study of Obesity Evaluation of the Overweight/Obese Child--Practical Tips for the Primary Health Care Provider: Recommendations from the Childhood Obesity Task Force of the European Association for the Study of Obesity. Obes. Facts 2010, 3, 131–137. [Google Scholar] [CrossRef]
- Stabouli, S.; Erdine, S.; Suurorg, L.; Jankauskienė, A.; Lurbe, E. Obesity and Eating Disorders in Children and Adolescents: The Bidirectional Link. Nutrients 2021, 13, 4321. [Google Scholar] [CrossRef]
- Rancourt, D.; McCullough, M.B. Overlap in Eating Disorders and Obesity in Adolescence. Curr. Diabetes Rep. 2015, 15, 78. [Google Scholar] [CrossRef]
- Saviñon, C.; Taylor, J.S.; Canty-Mitchell, J.; Blood-Siegfried, J. Childhood Obesity: Can Electronic Medical Records Customized with Clinical Practice Guidelines Improve Screening and Diagnosis?: Clinical Practice Guidelines for Childhood Obesity. J. Am. Acad. Nurse Pract. 2012, 24, 463–471. [Google Scholar] [CrossRef]
- Thompson, N.M. Sleep and Association With Obesity. J. Pediatr. Surg. Nurs. 2018, 7, 109–111. [Google Scholar] [CrossRef]
- Sutaria, S.; Devakumar, D.; Yasuda, S.S.; Das, S.; Saxena, S. Is Obesity Associated with Depression in Children? Systematic Review and Meta-Analysis. Arch. Dis. Child. 2019, 104, 64–74. [Google Scholar] [CrossRef]
- Fox, C.K.; Gross, A.C.; Rudser, K.D.; Foy, A.M.H.; Kelly, A.S. Depression, Anxiety, and Severity of Obesity in Adolescents: Is Emotional Eating the Link? Clin. Pediatr. 2016, 55, 1120–1125. [Google Scholar] [CrossRef] [PubMed]
- Rao, W.-W.; Zong, Q.-Q.; Zhang, J.-W.; An, F.-R.; Jackson, T.; Ungvari, G.S.; Xiang, Y.; Su, Y.-Y.; D’Arcy, C.; Xiang, Y.-T. Obesity Increases the Risk of Depression in Children and Adolescents: Results from a Systematic Review and Meta-Analysis. J. Affect. Disord. 2020, 267, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Kang, N.R.; Kwack, Y.S. An Update on Mental Health Problems and Cognitive Behavioral Therapy in Pediatric Obesity. Pediatr. Gastroenterol. Hepatol. Nutr. 2020, 23, 15. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.L.; Rhie, Y.-J. Severe Obesity in Children and Adolescents: Metabolic Effects, Assessment, and Treatment. J. Obes. Metab. Syndr. 2021, 30, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Danielsson, P.; Kowalski, J.; Ekblom, Ö.; Marcus, C. Response of Severely Obese Children and Adolescents to Behavioral Treatment. Arch. Pediatr. Adolesc. Med. 2012, 166, 1103. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, G.; Fox, C.K.; Kelly, A.S.; Jastreboff, A.M.; Browne, A.F.; Browne, N.T.; Pratt, J.S.A.; Bolling, C.; Michalsky, M.P.; Cook, S.; et al. Clinical Considerations Regarding the Use of Obesity Pharmacotherapy in Adolescents with Obesity. Obesity 2019, 27, 190–204. [Google Scholar] [CrossRef] [PubMed]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric Obesity—Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef]
- Pratt, J.S.A.; Browne, A.; Browne, N.T.; Bruzoni, M.; Cohen, M.; Desai, A.; Inge, T.; Linden, B.C.; Mattar, S.G.; Michalsky, M.; et al. ASMBS Pediatric Metabolic and Bariatric Surgery Guidelines, 2018. Surg. Obes. Relat. Dis. 2018, 14, 882–901. [Google Scholar] [CrossRef]
- Rusek, W.; Leszczak, J.; Baran, J.; Adamczyk, M.; Weres, A.; Baran, R.; Inglot, G.; Czenczek-Lewandowska, E.; Porada, S.; Pop, T. Role of Body Mass Category in the Development of Faulty Postures in School-Age Children from a Rural Area in South-Eastern Poland: A Cross-Sectional Study. BMJ Open 2019, 9, e030610. [Google Scholar] [CrossRef]
- Molina-Garcia, P.; Mora-Gonzalez, J.; Migueles, J.H.; Rodriguez-Ayllon, M.; Esteban-Cornejo, I.; Cadenas-Sanchez, C.; Plaza-Florido, A.; Gil-Cosano, J.J.; Pelaez-Perez, M.A.; Garcia-Delgado, G.; et al. Effects of Exercise on Body Posture, Functional Movement, and Physical Fitness in Children With Overweight/Obesity. J. Strength Cond. Res. 2020, 34, 2146–2155. [Google Scholar] [CrossRef]
- Kendall, F. Chapter 2: Posture. In Muscles: Testing and Function with Posture and Pain; Lippincott Williams & Wilkins: Baltimore, MD, USA, 1952; pp. 49–117. [Google Scholar]
- Woodhull, A.M.; Maltrud, K.; Mello, B.L. Alignment of the Human Body in Standing. Eur. J. Appl. Physiol. 1985, 54, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Kapandji, A. The Physiology of the Joints; Churchill Livingstone: New York, NY, USA, 1974. [Google Scholar]
- Yu, C.W.; Sung, R.Y.; So, R.; Lam, K.; Nelson, E.A.; Li, A.M.; Yuan, Y.; Lam, P.K. Energy Expenditure and Physical Activity of Obese Children: Cross-Sectional Study. J. Hong Kong Med. Assoc. 2002, 8, 313–317. [Google Scholar]
- Stolzman, S.; Irby, M.B.; Callahan, A.B.; Skelton, J.A. Pes Planus and Paediatric Obesity: A Systematic Review of the Literature. Clin. Obes. 2015, 5, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Kasović, M.; Štefan, L.; Piler, P.; Zvonar, M. Longitudinal Associations between Sport Participation and Fat Mass with Body Posture in Children: A 5-Year Follow-up from the Czech ELSPAC Study. PLoS ONE 2022, 17, e0266903. [Google Scholar] [CrossRef]
- Batistão, M.V.; Moreira, R.d.F.C.; Coury, H.J.C.G.; Salasar, L.E.B.; Sato, T.D. Prevalence of Postural Deviations and Associated Factors in Children and Adolescents: A Cross-Sectional Study. Fisioter. Em Mov. 2016, 29, 777–786. [Google Scholar] [CrossRef]
- Brzęk, A.; Dworrak, T.; Strauss, M.; Sanchis-Gomar, F.; Sabbah, I.; Dworrak, B.; Leischik, R. The Weight of Pupils’ Schoolbags in Early School Age and Its Influence on Body Posture. BMC Musculoskelet. Disord. 2017, 18, 117. [Google Scholar] [CrossRef]
- Esposito, P.W.; Caskey, P.; Heaton, L.E.; Otsuka, N. Childhood Obesity Case Statement. Semin. Arthritis Rheum. 2013, 42, 539–544. [Google Scholar] [CrossRef]
- Calvete, S. The Relationship between Posture Alterations and Injuries Sporting in Obese Children and Adolescents. Mot. Rev. Educ. Física 2007, 10. [Google Scholar] [CrossRef]
- Stanos, S.; Prather, H.; Press, J.M.; Young, J.L. Physical Medicine and Rehabilitation Approaches to Pain Management. In SPEC Essentials of Pain Medicine and Regional Anesthesia, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2005; pp. 197–202. [Google Scholar] [CrossRef]
- Aleixo, A.; Guimarães, E.; Walsh, I.; Pereira, K. Influence of Overweight and Obesity on Posture, Overall Praxis and Balance in Schoolchildren. J. Hum. Growth Dev. 2012, 22, 239–245. [Google Scholar] [CrossRef]
- Gijon-Nogueron, G.; Montes-Alguacil, J.; Martinez-Nova, A.; Alfageme-Garcia, P.; Cervera-Marin, J.A.; Morales-Asencio, J.M. Overweight, Obesity and Foot Posture in Children: A Cross-Sectional Study. J. Paediatr. Child Health 2017, 53, 33–37. [Google Scholar] [CrossRef]
- Grabara, M.; Pstrągowska, D. Estimation of the Body Posture in Girls and Boys Related to Their Body Mass Index (BMI). Pol. J. Sports Med. 2008, 24, 231–239. [Google Scholar]
- Bayartai, M.E.; Schaer, C.E.; Luomajoki, H.; Tringali, G.; De Micheli, R.; Sartorio, A. Differences in Spinal Posture and Mobility between Children/Adolescents with Obesity and Age-Matched Normal-Weight Individuals. Sci. Rep. 2022, 12, 15570. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; Ramachandran, J.; Weisman, P.; Jung, E.S. Obesity Effect on Male Active Joint Range of Motion. Ergonomics 2010, 53, 102–108. [Google Scholar] [CrossRef]
- Valdovino, A.G.; Bastrom, T.P.; Reighard, F.G.; Cross, M.; Bartley, C.E.; Shah, S.A.; Yaszay, B.; Newton, P.O.; Upasani, V.V. Obesity Is Associated With Increased Thoracic Kyphosis in Adolescent Idiopathic Scoliosis Patients and Nonscoliotic Adolescents. Spine Deform. 2019, 7, 865–869. [Google Scholar] [CrossRef]
- The Effect of Age, BMI, and Bone Mineral Density on the Various Lumbar Vertebral Measurements in Females. SpringerLink. Available online: https://link.springer.com/article/10.1007/s00276-020-02560-1 (accessed on 27 September 2022).
- Romero-Vargas, S.; Zárate-Kalfópulos, B.; Otero-Cámara, E.; Rosales-Olivarez, L.; Alpízar-Aguirre, A.; Morales-Hernández, E.; Reyes-Sánchez, A. The Impact of Body Mass Index and Central Obesity on the Spino-Pelvic Parameters: A Correlation Study. Eur. Spine J. 2013, 22, 878–882. [Google Scholar] [CrossRef]
- Smith, A.J.; O’Sullivan, P.B.; Beales, D.J.; de Klerk, N.; Straker, L.M. Trajectories of Childhood Body Mass Index Are Associated with Adolescent Sagittal Standing Posture. Int. J. Pediatr. Obes. IJPO Off. J. Int. Assoc. Study Obes. 2011, 6, e97–e106. [Google Scholar] [CrossRef]
- Rodacki, A.L.F.; Fowler, N.E.; Provensi, C.L.G.; Rodacki, C.d.L.N.; Dezan, V.H. Body Mass as a Factor in Stature Change. Clin. Biomech. Bristol Avon 2005, 20, 799–805. [Google Scholar] [CrossRef]
- Tsiros, M.D.; Tian, E.J.; Shultz, S.P.; Olds, T.; Hills, A.P.; Duff, J.; Kumar, S. Obesity, the New Childhood Disability? An Umbrella Review on the Association between Adiposity and Physical Function. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2020, 21, e13121. [Google Scholar] [CrossRef]
- Barnett, L.M.; van Beurden, E.; Morgan, P.J.; Brooks, L.O.; Beard, J.R. Childhood Motor Skill Proficiency as a Predictor of Adolescent Physical Activity. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2009, 44, 252–259. [Google Scholar] [CrossRef]
- Cattuzzo, M.T.; Dos Santos Henrique, R.; Ré, A.H.N.; de Oliveira, I.S.; Melo, B.M.; de Sousa Moura, M.; de Araújo, R.C.; Stodden, D. Motor Competence and Health Related Physical Fitness in Youth: A Systematic Review. J. Sci. Med. Sport 2016, 19, 123–129. [Google Scholar] [CrossRef]
- Mahaffey, R.; Morrison, S.C.; Stephensen, D.; Drechsler, W.I. Clinical Outcome Measures for Monitoring Physical Function in Pediatric Obesity: An Integrative Review. Obes. Res. J. 2016, 24, 993–1017. [Google Scholar] [CrossRef] [PubMed]
- Tsiros, M.D.; Brinsley, J.; Mackintosh, S.; Thewlis, D. Relationships between Adiposity and Postural Control in Girls during Balance Tasks of Varying Difficulty. Obes. Res. Clin. Pract. 2019, 13, 358–364. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, G.; Keating, R.; Elmes, M.; Killeen, S.; Sheridan, N.; Murphy, S.; Brinkley, A. Standing Balance and Health-Related Quality of Life in Children Who Are Obese. Appetite 2015, 89, 309. [Google Scholar] [CrossRef]
- Liang, J.; Matheson, B.E.; Kaye, W.H.; Boutelle, K.N. Neurocognitive Correlates of Obesity and Obesity-Related Behaviors in Children and Adolescents. Int. J. Obes. 2014, 38, 494–506. [Google Scholar] [CrossRef]
- Slotte, S.; Sääkslahti, A.; Kukkonen-Harjula, K.; Rintala, P. Fundamental Movement Skills and Weight Status in Children: A Systematic Review. Balt. J. Health Phys. Act. 2017, 9, 115–127. [Google Scholar] [CrossRef]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A Developmental Perspective on the Role of Motor Skill Competence in Physical Activity: An Emergent Relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental Movement Skills in Children and Adolescents: Review of Associated Health Benefits. Sports Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef]
- Holfelder, B.; Schott, N. Relationship of Fundamental Movement Skills and Physical Activity in Children and Adolescents: A Systematic Review. Psychol. Sport Exerc. 2014, 15, 382–391. [Google Scholar] [CrossRef]
- Malatesta, D.; Vismara, L.; Menegoni, F.; Galli, M.; Romei, M.; Capodaglio, P. Mechanical External Work and Recovery at Preferred Walking Speed in Obese Subjects. Med. Sci. Sports Exerc. 2009, 41, 426–434. [Google Scholar] [CrossRef]
- Pataky, Z.; Armand, S.; Müller-Pinget, S.; Golay, A.; Allet, L. Effects of Obesity on Functional Capacity. Obes. Res. J. 2014, 22, 56–62. [Google Scholar] [CrossRef]
- Lafortuna, C.L.; Maffiuletti, N.A.; Agosti, F.; Sartorio, A. Gender Variations of Body Composition, Muscle Strength and Power Output in Morbid Obesity. Int. J. Obes. 2005, 29, 833–841. [Google Scholar] [CrossRef]
- Rodrigues de Lima, T.; Custódio Martins, P.; Henrique Guerra, P.; Augusto Santos Silva, D. Muscular Fitness and Cardiovascular Risk Factors in Children and Adolescents: A Systematic Review. J. Strength Cond. Res. 2020, 34, 2394–2406. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramírez-Campillo, R.; Izquierdo, M. Is Muscular Fitness Associated with Future Health Benefits in Children and Adolescents? A Systematic Review and Meta-Analysis of Longitudinal Studies. Sports Med. 2019, 49, 1079–1094. [Google Scholar] [CrossRef] [PubMed]
- Grao-Cruces, A.; Ruiz-Ariza, A.; De La Torre-Cruz, M.J.; Martínez-López, E.J. Students with Excess Weight Obtain Lower Physical Fitness Test Scores in Physical Education than Normal Weight Pairs: Myth or Reality? J. Phys. Educ. Sport 2018, 18, 1562–1571. [Google Scholar]
- Thivel, D.; Ring-Dimitriou, S.; Weghuber, D.; Frelut, M.-L.; O’Malley, G. Muscle Strength and Fitness in Pediatric Obesity: A Systematic Review from the European Childhood Obesity Group. Obes. Facts 2016, 9, 52–63. [Google Scholar] [CrossRef]
- Duvigneaud, N.; Matton, L.; Wijndaele, K.; Deriemaeker, P.; Lefevre, J.; Philippaerts, R.; Thomis, M.; Delecluse, C.; Duquet, W. Relationship of Obesity with Physical Activity, Aerobic Fitness and Muscle Strength in Flemish Adults. J. Sports Med. Phys. Fit. 2008, 48, 201–210. [Google Scholar]
- O’Malley, G.C.; Shultz, S.P.; Thivel, D.; Tsiros, M.D. Neuromusculoskeletal Health in Pediatric Obesity: Incorporating Evidence into Clinical Examination. Curr. Obes. Rep. 2021, 10, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Sanders, R.H.; Han, A.; Baker, J.S.; Cobley, S. Childhood Obesity and Its Physical and Psychological Co-Morbidities: A Systematic Review of Australian Children and Adolescents. Eur. J. Pediatr. 2015, 174, 715–746. [Google Scholar] [CrossRef]
- Palmer, A.J.; Poveda, J.L.; Martinez-Laguna, D.; Reyes, C.; de Bont, J.; Silman, A.; Carr, A.J.; Duarte-Salles, T.; Prieto-Alhambra, D. Childhood Overweight and Obesity and Back Pain Risk: A Cohort Study of 466,997 Children. BMJ Open 2020, 10, e036023. [Google Scholar] [CrossRef]
- Azabagic, S.; Pranjic, N. The Site of Musculoskeletal Pain in School Children with Excessive Body Weight and Obesity in Bosnia and Herzegovina. Mater. Socio-Med. 2019, 31, 88–92. [Google Scholar] [CrossRef]
- Molina-Garcia, P.; Migueles, J.H.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Mora-Gonzalez, J.; Rodriguez-Ayllon, M.; Plaza-Florido, A.; Vanrenterghem, J.; Ortega, F.B. A Systematic Review on Biomechanical Characteristics of Walking in Children and Adolescents with Overweight/Obesity: Possible Implications for the Development of Musculoskeletal Disorders. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2019, 20, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Molina-Garcia, P.; Miranda-Aparicio, D.; Ubago-Guisado, E.; Alvarez-Bueno, C.; Vanrenterghem, J.; Ortega, F.B. The Impact of Childhood Obesity on Joint Alignment: A Systematic Review and Meta-Analysis. Phys. Ther. 2021, 101, pzab066. [Google Scholar] [CrossRef] [PubMed]
- Shohat, N.; Machluf, Y.; Farkash, R.; Finestone, A.S.; Chaiter, Y. Clinical Knee Alignment among Adolescents and Association with Body Mass Index: A Large Prevalence Study. Isr. Med. Assoc. J. IMAJ 2018, 20, 75–79. [Google Scholar] [PubMed]
- Dolphens, M.; Cagnie, B.; Vleeming, A.; Vanderstraeten, G.; Danneels, L. Gender Differences in Sagittal Standing Alignment before Pubertal Peak Growth: The Importance of Subclassification and Implications for Spinopelvic Loading. J. Anat. 2013, 223, 629–640. [Google Scholar] [CrossRef]
- Chen, J.-P.; Chung, M.-J.; Wang, M.-J. Flatfoot Prevalence and Foot Dimensions of 5- to 13-Year-Old Children in Taiwan. Foot Ankle Int. 2009, 30, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, M.; Kotz, R.; Ledl, T.; Hauser, G.; Sluga, M. Prevalence of Flat Foot in Preschool-Aged Children. Pediatrics 2006, 118, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Capodaglio, P.; Castelnuovo, G.; Brunani, A.; Vismara, L.; Villa, V.; Capodaglio, E.M. Functional Limitations and Occupational Issues in Obesity: A Review. Int. J. Occup. Saf. Ergon. JOSE 2010, 16, 507–523. [Google Scholar] [CrossRef]
- Ciaccia, M.C.C.; de Castro, J.S.; Rahal, M.A.; Penatti, B.S.; Selegatto, I.B.; Giampietro, J.L.M.; Rullo, V.E.V. PREVALÊNCIA DE ESCOLIOSE EM ESCOLARES DO ENSINO FUNDAMENTAL PÚBLICO. Rev. Paul. Pediatr. 2017, 35, 191–198. [Google Scholar] [CrossRef]
- Yang, L.; Lu, X.; Yan, B.; Huang, Y. Prevalence of Incorrect Posture among Children and Adolescents: Finding from a Large Population-Based Study in China. iScience 2020, 23, 101043. [Google Scholar] [CrossRef]
- Jankowicz-Szymańska, A.; Fałatowicz, M.; Smoła, E.; Błyszczuk, R.; Wódka, K. Relationship between Frontal Knee Position and the Degree of Thoracic Kyphosis and Lumbar Lordosis among 10-12-Year-Old Children with Normal Body Weight. PLoS ONE 2020, 15, e0236150. [Google Scholar] [CrossRef]
- Laita, L.; Cubillo, C.; Gòmez, T.; Del Barrio, S. Effects of Corrective, Therapeutic Exercise Techniques on Adolescent Idiopathic Scoliosis. A Systematic Review. Arch. Argent. Pediatr. 2018, 116, 582–589. [Google Scholar] [CrossRef]
- Lafond, D.; Descarreaux, M.; Normand, M.C.; Harrison, D.E. Postural Development in School Children: A Cross-Sectional Study. Chiropr. Osteopat. 2007, 15, 1. [Google Scholar] [CrossRef] [PubMed]
- Grivas, T.B.; Vasiliadis, E.S.; Koufopoulos, G.; Segos, D.; Triantafyllopoulos, G.; Mouzakis, V. Study of Trunk Asymmetry in Normal Children and Adolescents. Scoliosis 2006, 1, 19. [Google Scholar] [CrossRef] [PubMed]
- Marin, L.; Lovecchio, N.; Pedrotti, L.; Manzoni, F.; Febbi, M.; Albanese, I.; Patanè, P.; Carnevale Pellino, V.; Vandoni, M. Acute Effects of Self-Correction on Spine Deviation and Balance in Adolescent Girls with Idiopathic Scoliosis. Sensors 2022, 22, 1883. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; So, W.-Y. The Effect of the Schroth Rehabilitation Exercise Program on Spinal and Feet Alignment in Adolescent Patients with Idiopathic Scoliosis: A Pilot Study. Healthcare 2022, 10, 398. [Google Scholar] [CrossRef]
- Latalski, M.; Bylina, J.; Fatyga, M.; Repko, M.; Filipovic, M.; Jarosz, M.J.; Borowicz, K.B.; Matuszewski, Ł.; Trzpis, T. Risk Factors of Postural Defects in Children at School Age. Ann. Agric. Environ. Med. AAEM 2013, 20, 583–587. [Google Scholar] [PubMed]
- Simoneau, M.; Teasdale, N. Balance Control Impairment in Obese Individuals Is Caused by Larger Balance Motor Commands Variability. Gait Posture 2015, 41, 203–208. [Google Scholar] [CrossRef]
- Colné, P.; Frelut, M.L.; Pérès, G.; Thoumie, P. Postural Control in Obese Adolescents Assessed by Limits of Stability and Gait Initiation. Gait Posture 2008, 28, 164–169. [Google Scholar] [CrossRef]
- Deforche, B.I.; Hills, A.P.; Worringham, C.J.; Davies, P.S.W.; Murphy, A.J.; Bouckaert, J.J.; De Bourdeaudhuij, I.M. Balance and Postural Skills in Normal-Weight and Overweight Prepubertal Boys. Int. J. Pediatr. Obes. 2009, 4, 175–182. [Google Scholar] [CrossRef]
- Minghelli, B.; Oliveira, R.; Nunes, C. Postural Habits and Weight of Backpacks of Portuguese Adolescents: Are They Associated with Scoliosis and Low Back Pain? Work 2016, 54, 197–208. [Google Scholar] [CrossRef]
- Mikkelsson, L.O. Adolescent Flexibility, Endurance Strength, and Physical Activity as Predictors of Adult Tension Neck, Low Back Pain, and Knee Injury: A 25 Year Follow up Study. Br. J. Sports Med. 2006, 40, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Nga, V.T.; Dung, V.N.T.; Chu, D.-T.; Tien, N.L.B.; Van Thanh, V.; Ngoc, V.T.N.; Hoan, L.N.; Phuong, N.T.; Pham, V.-H.; Tao, Y.; et al. School Education and Childhood Obesity: A Systemic Review. Diabetes Metab. Syndr. 2019, 13, 2495–2501. [Google Scholar] [CrossRef] [PubMed]
- Wright, M.D.; Portas, M.D.; Evans, V.J.; Weston, M. The Effectiveness of 4 Weeks of Fundamental Movement Training on Functional Movement Screen and Physiological Performance in Physically Active Children. J. Strength Cond. Res. 2015, 29, 254–261. [Google Scholar] [CrossRef] [PubMed]

| System | Complications |
|---|---|
| Metabolic–endocrine |
|
| Cardiovascular |
|
| Gastroenterological |
|
| Respiratory |
|
| Renal |
|
| Neurological |
|
| Dermatological |
|
| Condition | Recent Key Supporting Evidence | Type of Study | Main Findings |
|---|---|---|---|
| Impaired coordination | Tsiros et al. [78] Barnett et al. [79] | UR SR | Motor skill development should be a key strategy in childhood interventions aiming to promote long-term physical activity. |
| Reduced motor skill proficiency | Tsiros et al. [78] Slotte et al. [85] Barnett et al. [79] Cattuzzo et al. [80] Mahaffey et al. [81] | UR SR SR SR SR | Motor skill development is necessary to promote motor competence in children and to enhance the participation in later motor activities such as sport-related or recreational activities. |
| Impaired balance (e.g., during challenging balance tasks involving a narrowed stance ± vision) | Tsiros et al. [78] Tsiros et al. [82] O’Malley et al. [83] Barnett et al. [79] Mahaffey et al. [81] | UR CS CS SR SR | Balance influences functional activities except sleeping. Poor balance could be ameliorated by working on coordination and propriocetive stimuli. |
| Reduced lower limb muscle strength (relative to body mass or during mass-dependent tasks) | Tsiros et al. [78] Rodrigues de Lima et al. [92] Garcia-Hermoso et al. [93] Grao-Cruces et al. [94] Mahaffey et al. [81] Thivel et al. [95] | UR SR SR SR SR SR | Children and adolescents with obesity display a decrease in muscular fitness compared to normal-weight peers. |
| Increased pain (e.g., musculoskeletal pain, neck/back pain, lower limb pain) | Tsiros et al. [78] Sanders et al. [98] Palmer et al. [99] Azabagic e Pranjic [100] | UR SR C C | The mantainment of normal weight from an early age reduces back pain in children. |
| Gait deviation (e.g., increased pelvic/hip/knee motion, prolonged stance phase, wider-based gait) | Molina-Garcia et al. [101] | SR | Children with obesity had higher difficulties, with greater step width, longer stance phase, higher tibiofemoral contact forces, higher ankle plantarflexion moments, and greater power generation. |
| Postural malalignment (increased lumbar lordosis, genu valgum) | Molina-Garcia et al. [102] | SR and MA | Children with obesity had a significantly higher risk of lumbar hyperlordosis, genu valgum, flatfoot, and any joint malalignment compared to their peers of normal weight. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calcaterra, V.; Marin, L.; Vandoni, M.; Rossi, V.; Pirazzi, A.; Grazi, R.; Patané, P.; Silvestro, G.S.; Carnevale Pellino, V.; Albanese, I.; et al. Childhood Obesity and Incorrect Body Posture: Impact on Physical Activity and the Therapeutic Role of Exercise. Int. J. Environ. Res. Public Health 2022, 19, 16728. https://doi.org/10.3390/ijerph192416728
Calcaterra V, Marin L, Vandoni M, Rossi V, Pirazzi A, Grazi R, Patané P, Silvestro GS, Carnevale Pellino V, Albanese I, et al. Childhood Obesity and Incorrect Body Posture: Impact on Physical Activity and the Therapeutic Role of Exercise. International Journal of Environmental Research and Public Health. 2022; 19(24):16728. https://doi.org/10.3390/ijerph192416728
Chicago/Turabian StyleCalcaterra, Valeria, Luca Marin, Matteo Vandoni, Virginia Rossi, Agnese Pirazzi, Roberta Grazi, Pamela Patané, Giustino Simone Silvestro, Vittoria Carnevale Pellino, Ilaria Albanese, and et al. 2022. "Childhood Obesity and Incorrect Body Posture: Impact on Physical Activity and the Therapeutic Role of Exercise" International Journal of Environmental Research and Public Health 19, no. 24: 16728. https://doi.org/10.3390/ijerph192416728
APA StyleCalcaterra, V., Marin, L., Vandoni, M., Rossi, V., Pirazzi, A., Grazi, R., Patané, P., Silvestro, G. S., Carnevale Pellino, V., Albanese, I., Fabiano, V., Febbi, M., Silvestri, D., & Zuccotti, G. (2022). Childhood Obesity and Incorrect Body Posture: Impact on Physical Activity and the Therapeutic Role of Exercise. International Journal of Environmental Research and Public Health, 19(24), 16728. https://doi.org/10.3390/ijerph192416728











