Delivering Digital Healthcare for Elderly: A Holistic Framework for the Adoption of Ambient Assisted Living
Abstract
1. Introduction
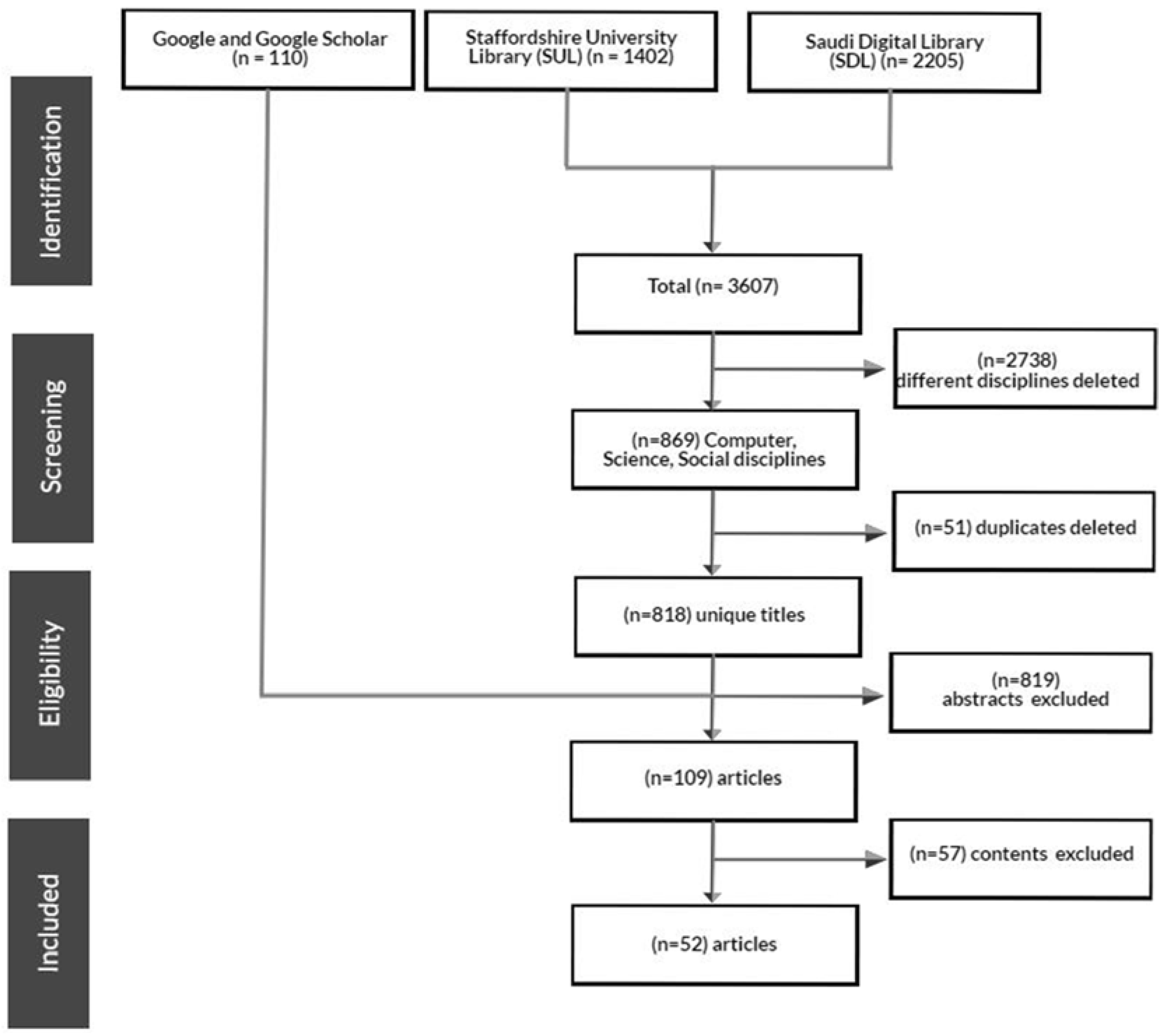
2. Materials and Methods
2.1. Review Procedures
2.2. Thematic Analysis Procedures
3. Results
3.1. Characteristics of the Included Studies
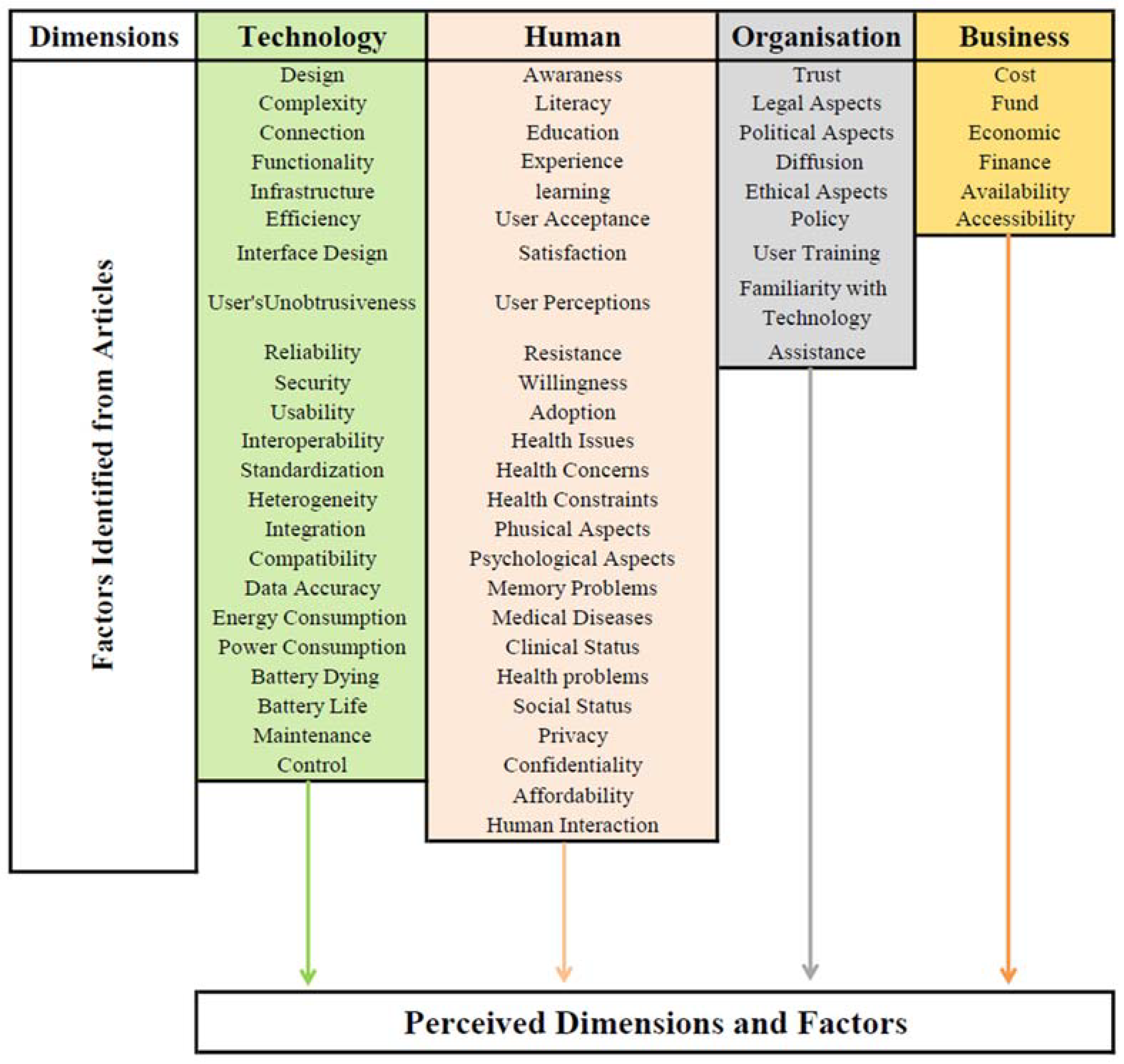
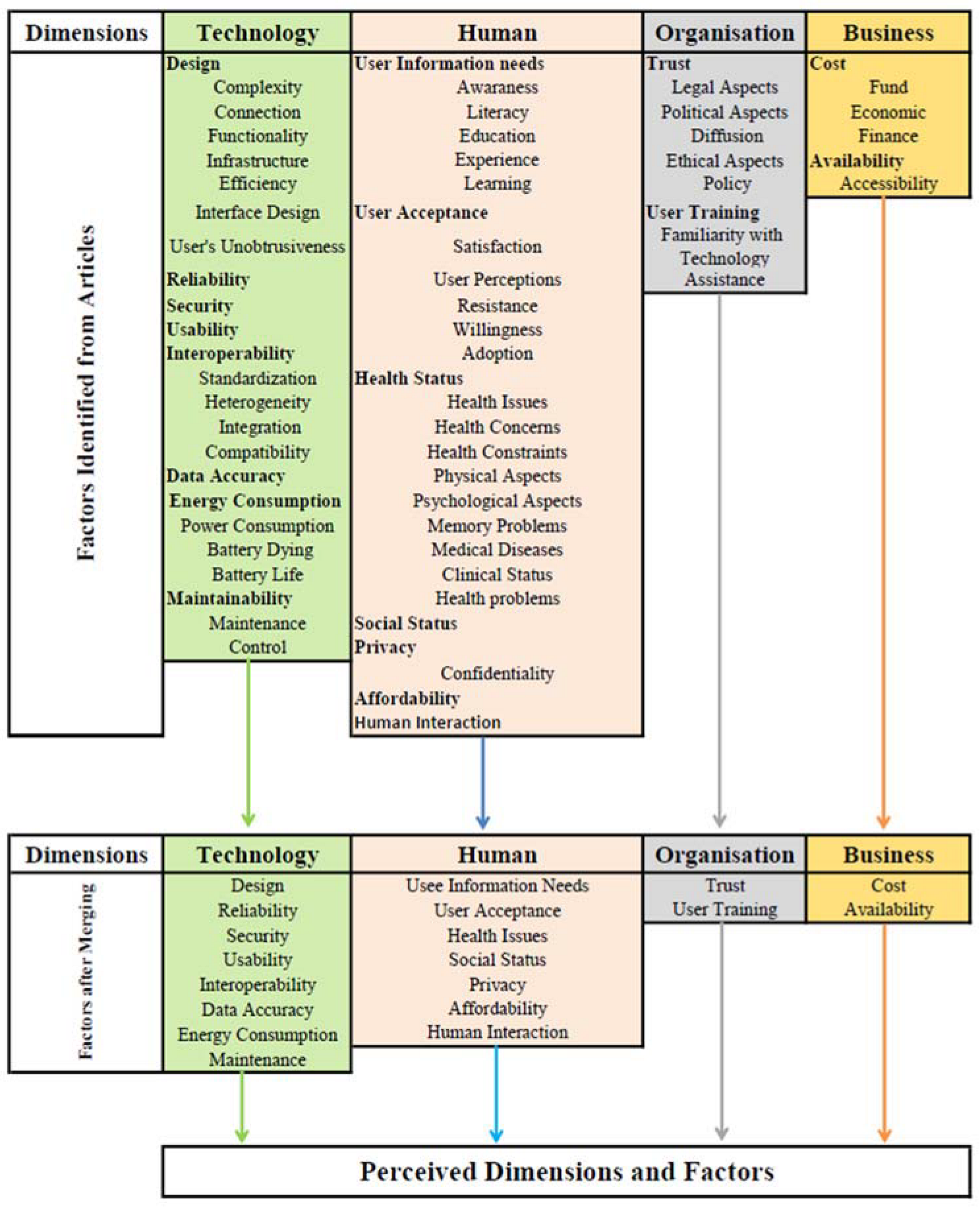
3.2. Our Approach Establishing the Framework of AAL Adoption
- Technology dimension has eight factors:
- ∘
- Design, complexity, connection, functionality, infrastructure, efficiency, interface design, and user’s unobtrusiveness were abstracted and placed under “design” factor.
- ∘
- Interoperability, standardization, heterogeneity, integration, and compatibility were grouped and placed under the interoperability factor.
- ∘
- Energy consumption, power consumption, battery dying, and battery life were grouped and renamed as energy consumption factor.
- ∘
- Maintenance and control were grouped and renamed maintainability.
- ∘
- Reliability, security, usability, and data accuracy factors were all retained with no changes.
- Human dimension has seven factors:
- ∘
- Awareness, literacy, education, experience, and learning were abstracted and renamed as user’s information needs.
- ∘
- User Acceptance, satisfaction, user perceptions, resistance, willingness, and adoption were grouped and renamed as user acceptance factor.
- ∘
- Health issues, health concerns, health constraints, physical aspects, psychological aspects, memory problems, medical diseases, clinical status, and health problems were grouped and placed under health status factor.
- ∘
- Privacy and confidentiality were grouped and renamed as privacy factor.
- ∘
- Social status, affordability, and human interaction were all kept with no change.
- Organisation dimension has two factors:
- ∘
- Trust, legal aspects, political aspects, diffusion, ethical aspects, and policy were abstracted and placed under trust factor.
- ∘
- User training, familiarity with technology, and assistance need were grouped and renamed as user training factor.
- Business dimension has two factors:
- ∘
- Costs, funds, economic, and finance were grouped and renamed as costs factor.
- ∘
- Availability and accessibility were grouped and renamed availability factor.
3.3. Key Factors Contributing to AAL Technologies Adoption
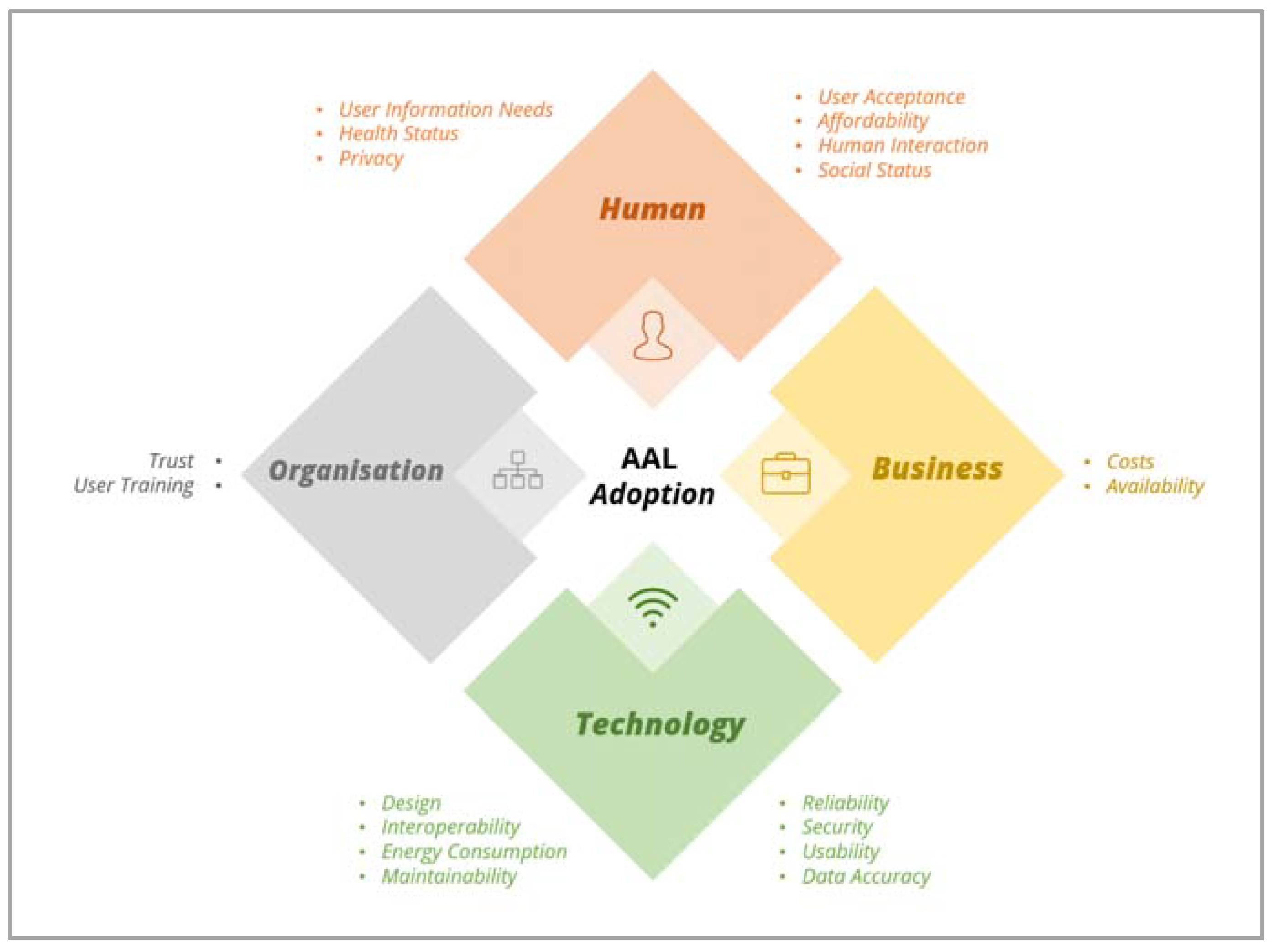
- Privacy factor was noted in 50% of the included studies. It refers to the privacy of AAL users’ personal information. Poor privacy of AAL technologies can cause invasion of users’ private lives and leads to refusal of adoption by users [11].
- Trust factor was noted in 44% of the included studies. It indicates a lack of trust and acknowledgement of organisations and ambient towards technologies [11].
- Security factor was noted in 40% of the included studies. It indicates secure communication among main components of AAL technologies [64]. Studies suggested that new technologies should be designed with security measures taken into consideration in order to increase AAL technologies’ adoption among older adult users [59].
- Design factor was noted in 35% of the included studies. It is concerned with the constructability of AAL technologies that includes, but not limited to, complexity, connection, functionality, infrastructure, efficiency, interface design, and user’s unobtrusiveness. Studies suggested that aging users should be engaged in designing new technologies to enhance their design [65].
- Interoperability was noted in 27% of the included studies. It refers to the ability of different systems to communicate with each other to provide the intended services. Lack of interoperability among AAL devices used by older adult users could hinder its long-term adoption [59].
- User’s information needs factor was noted in 23% of the included studies. It indicates that AAL technologies’ capability to fulfill the users’ information needs, which may differ based on several elements such as the user’s health status, literacy, technical skills and the like.
- User acceptance factor was noted in 23% of the included studies. It refers to the acceptance of AAL technologies by its perceived users [11]. The acceptance of AAL technologies varies for different age groups and influences many aspects such as ease of use.
- Social status factor was noted in 23% of the included studies. It is related to understanding the gender position that older persons hold in a group (e.g., grandfather, unmarried) and the impact of AAL technologies on their social activities. According to Wu et al. (2014) [43], AAL technologies could reduce communication between the users and their family members.
- Health status factor was noted in 19% of the included studies. It refers to providing elderly people with technologies that can help them monitor their health and understand users’ wellness and illness including physical disabilities, chorionic diseases, mental impairments, etc. [45].
- User training factor was noted in 15% of the included studies. It refers to providing the ability for older users to use AAL technologies through training and customer services to enhance their autonomy in human-free assistance [63].
- Usability factor was noted in 15% of the included studies. It is concerned with the older users’ ability and desire to use the AAL technology. Limited ability of the older adults could be due to several factors such as lack of confidence in using new technologies [65].
- Reliability factor was noted in 13% of the included studies. It can be described as the possibility of the technology to provide its perceived benefits. Poor reliability of AAL technologies can lead to low utilization by users [59].
- Availability factor was noted in 13% of the included studies. It indicates the availability of AAL technologies and services to consumers in the required or local markets [11] despite any change in the company or service provider.
- Energy consumption factor was noted in 12% of the included studies. It is concerned with efficiency in energy usage. Low energy consumption of AAL technology reduces users’ expenses and improves their usage [64].
- Human interaction factor was noted in 12% of the included studies. It is concerned with the interaction between the devices and their users to get the functions completed. Here the balance of manual functions that must be performed by the users and automatic functions that are performed by the devices should be maintained for effective human interaction and engagement of the older users [65].
- Maintainability factor was noted in 10% of the included studies. It refers to the capability of maintaining the AAL system and keeping it up to date. Maintainability is essential for a long-term adoption [63].
- Affordability was noted in 4% of the included studies. It refers to whether the price of the AAL technology is within most ageing consumers’ budget [54].
- Data accuracy factor was noted in 4% of the included studies. It refers to the correctness of data values produced by AAL technologies with high accuracy [55].
4. Discussion
4.1. The AAL Adoption Diamond Framework
4.2. Comparison between Findings from the Included Studies and Our Study
4.3. Comparison between Our AAL Adoption Diamond Framework and Popular Technology Adoption Models and Frameworks
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 7 November 2022).
- Al-Aama, T. Falls in the elderly: Spectrum and prevention. Can. Fam. Physician 2011, 57, 771–776. [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention. Facts about Falls. Available online: https://www.cdc.gov/falls/facts.html#print (accessed on 11 November 2022).
- Al-Shaqi, R.; Mourshed, M.; Rezgui, Y. Progress in ambient assisted systems for independent living by the elderly. Springerplus 2016, 5, 624. [Google Scholar] [CrossRef] [PubMed]
- Arni, A.; Vasvi, K.; Amir, T.-K.; Junhua, L.; Pradeep, K.R. Challenges in Seniors Adopting Assistive Robots: A Systematic Review. Int. Technol. Manag. Rev. 2016, 6, 25–36. [Google Scholar] [CrossRef][Green Version]
- Muñoz, A.; Augusto, J.C.; Villa, A.; Blaya, J.A.B. Design and evaluation of an ambient assisted living system based on an argumentative multi-agent system. Pers. Ubiquitous Comput. 2011, 15, 377–387. [Google Scholar] [CrossRef]
- Ayala, I.; Amor, M.; Fuentes, L. Self-configuring agents for ambient assisted living applications. Pers. Ubiquitous Comput. 2013, 17, 1159–1169. [Google Scholar] [CrossRef]
- Gonçalves, C.; Ferreira da Silva, A.; Gomes, J.; Simoes, R. Wearable E-Textile Technologies: A Review on Sensors, Actuators and Control Elements. Inventions 2018, 3, 14. [Google Scholar] [CrossRef]
- Balta-Ozkan, N.; Davidson, R.; Bicket, M.; Whitmarsh, L. Social barriers to the adoption of smart homes. Energy Policy 2013, 63, 363–374. [Google Scholar] [CrossRef]
- Berglin, L. Smart Textiles and Wearable Technology; Högskolan i Borås: Borås, Sweden, 2013. [Google Scholar]
- Schomakers, E.-M.; Heek, J.O.-v.; Ziefle, M. Playfully Assessing the Acceptance and Choice of Ambient Assisted Living Technologies by Older Adults. In Proceedings of the ICT4AWE 2018: Information and Communication Technologies for Ageing Well and e-Health, Madeira, Portugal, 22–23 March 2018. [Google Scholar]
- Alsulami, M.H.; Atkins, A.S.; Campion, R.J. Factors Influencing the Adoption of Ambient Assisted Living Technologies by Healthcare Providers in the Kingdom of Saudi Arabia. Staffordshire University. In Proceedings of the AIT2S 2017: Advanced Information Technology, Services and Systems, Tangier, Morocco, 14–15 April 2017. [Google Scholar]
- Maranesi, E.; Amabili, G.; Cucchieri, G.; Bolognini, S.; Margaritini, A.; Bevilacqua, R. Understanding the Acceptance of IoT and Social Assistive Robotics for the Healthcare Sector: A Review of the Current User-Centred Applications for the Older Users. In Internet of Things for Human-Centered Design: Application to Elderly Healthcare; Scataglini, S., Imbesi, S., Marques, G., Eds.; Springer Nature Singapore: Singapore, 2022; pp. 331–351. [Google Scholar]
- Smit, D.; Eybers, S. Towards a Socio-specific Artificial Intelligence Adoption Framework. In Proceedings of the 43rd Conference of the South African Institute of Computer Scientists and Information Technologists, Online, 18–20 July 2022; pp. 270–282. [Google Scholar]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User Acceptance of Computer Technology: A Comparison of Two Theoretical Models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Taylor, S.; Todd, P.A. Understanding Information Technology Usage: A Test of Competing Models. Inf. Syst. Res. 1995, 6, 144–176. [Google Scholar] [CrossRef]
- Fishbein, M.; Ajzen, I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Philos. Rhetor. 1977, 10, 130–132. [Google Scholar]
- Tornatzky, L.G.; Fleischer, M.; Chakrabarti, A.K. The Processes of Technological Innovation, Issues in Organization and Management Series; Lexington books: Lexington, MA, USA, 1990. [Google Scholar]
- AALIANCE2. Ambient Assisted Living Roadmap. Available online: http://www.aaliance2.eu/sites/default/files/AA2_WP2_D27_RM2_rev5.0.pdf (accessed on 17 April 2022).
- Carnemolla, P. Ageing in place and the internet of things—How smart home technologies, the built environment and caregiving intersect. Vis. Eng. 2018, 6, 7. [Google Scholar] [CrossRef]
- Tessarolo, F.; Petsani, D.; Conotter, V.; Nollo, G.; Conti, G.; Nikolaidou, M.; Onorati, G.; Bamidis, P.D.; Konstantinidis, E.I. Developing ambient assisted living technologies exploiting potential of user-centred co-creation and agile methodology: The CAPTAIN project experience. J. Ambient. Intell. Humaniz. Comput. 2022, 1–16. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Sun, H.; Florio, V.D.; Gui, N.; Blondia, C. Promises and Challenges of Ambient Assisted Living Systems. In Proceedings of the 2009 Sixth International Conference on Information Technology: New Generations, Las Vegas, NV, USA, 27–29 April 2009; pp. 1201–1207. [Google Scholar]
- Ding, D.; Cooper, R.A.; Pasquina, P.F.; Fici-Pasquina, L. Sensor technology for smart homes. Maturitas 2011, 69, 131–136. [Google Scholar] [CrossRef]
- Pogorelc, B.; Bosnić, Z.; Gams, M. Automatic recognition of gait-related health problems in the elderly using machine learning. Multimed. Tools Appl. 2012, 58, 333–354. [Google Scholar] [CrossRef]
- Wu, Y.-H.; Fassert, C.; Rigaud, A.-S. Designing robots for the elderly: Appearance issue and beyond. Arch. Gerontol. Geriatr. 2012, 54, 121–126. [Google Scholar] [CrossRef]
- Grgurić, A. ICT Towards Elderly Independent Living; AAL Forum: Trieste, Italy, 2012; pp. 1–8. [Google Scholar]
- Chan, M.; Estève, D.; Fourniols, J.-Y.; Escriba, C.; Campo, E. Smart wearable systems: Current status and future challenges. Artif. Intell. Med. 2012, 56, 137–156. [Google Scholar] [CrossRef]
- Paoli, R.; Fernández-Luque, F.J.; Doménech, G.; Martínez, F.; Zapata, J.; Ruiz, R. A system for ubiquitous fall monitoring at home via a wireless sensor network and a wearable mote. Expert Syst. Appl. 2012, 39, 5566–5575. [Google Scholar] [CrossRef]
- Lê, Q.; Nguyen, H.B.; Barnett, T. Smart Homes for Older People: Positive Aging in a Digital World. Future Internet 2012, 4, 607–617. [Google Scholar] [CrossRef]
- Flandorfer, P. Drivers, Barriers and long-term Requirements of assistive Technologies supporting older Persons in living longer independently at Home: A systematic Review of European, US-American and Japanese Policy Papers and Assessment Studies. In Proceedings of the European Population Conference, Stockholm, Sweden, 13–16 June 2012. [Google Scholar]
- Portet, F.; Vacher, M.; Golanski, C.; Roux, C.; Meillon, B. Design and evaluation of a smart home voice interface for the elderly: Acceptability and objection aspects. Pers. Ubiquitous Comput. 2011, 17, 127–144. [Google Scholar] [CrossRef]
- Khosla, R.; Chu, M.-T.; Nguyen, K. Affective Robot Enabled Capacity and Quality Improvement of Nursing Home Aged Care Services in Australia. In Proceedings of the 2013 IEEE 37th Annual Computer Software and Applications Conference Workshops, Kyoto, Japan, 22–26 July 2013; pp. 409–414. [Google Scholar]
- Kim, S.-C.; Jeong, Y.-S.; Park, S.-O. RFID-based indoor location tracking to ensure the safety of the elderly in smart home environments. Pers. Ubiquitous Comput. 2013, 17, 1699–1707. [Google Scholar] [CrossRef]
- Parker, S.J.; Jessel, S.; Richardson, J.E.; Reid, M.C. Older adults are mobile too!Identifying the barriers and facilitators to older adults’ use of mHealth for pain management. BMC Geriatr. 2013, 13, 43. [Google Scholar] [CrossRef] [PubMed]
- Rashidi, P.; Mihailidis, A. A survey on ambient-assisted living tools for older adults. IEEE J. Biomed. Health Inform. 2013, 17, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Spitalewsky, K.; Rochon, J.; Ganzinger, M.; Knaup, P. Potential and requirements of IT for ambient assisted living technologies. Results of a Delphi study. Methods Inf. Med. 2013, 52, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.E.; Adair, B.; Miller, K.J.; Ozanne, E.; Hansen, R.; Pearce, A.J.; Santamaria, N.; Viegas, L.; Long, M.; Said, C.M. Smart-Home Technologies to Assist Older People to Live Well at Home. J. Aging Sci. 2013, 1, 1–9. [Google Scholar]
- Memon, M.; Wagner, S.R.; Pedersen, C.F.; Beevi, F.H.; Hansen, F.O. Ambient assisted living healthcare frameworks, platforms, standards, and quality attributes. Sensors 2014, 14, 4312–4341. [Google Scholar] [CrossRef] [PubMed]
- Spasova, V.; Iliev, I. A survey on automatic fall detection in the context of ambient assisted living systems. Int. J. Adv. Comput. Res. 2014, 4, 94. [Google Scholar]
- Wu, Y.H.; Wrobel, J.; Cornuet, M.; Kerhervé, H.; Damnée, S.; Rigaud, A.S. Acceptance of an assistive robot in older adults: A mixed-method study of human-robot interaction over a 1-month period in the Living Lab setting. Clin. Interv. Aging 2014, 9, 801–811. [Google Scholar] [CrossRef]
- Hersh, M. Overcoming Barriers and Increasing Independence—Service Robots for Elderly and Disabled People. Int. J. Adv. Robot. Syst. 2015, 12, 114. [Google Scholar] [CrossRef]
- Jaschinski, C.; Allouch, S.B. An extended view on benefits and barriers of ambient assisted living solutions. Adv. Life Sci. 2015, 7, 40–53. [Google Scholar]
- Peruzzini, M.; Germani, M. Design of a service-oriented architecture for Ambient-assisted Living. Int. J. Agil. Syst. Manag. 2016, 9, 154–178. [Google Scholar] [CrossRef]
- Li, R.; Lu, B.; McDonald-Maier, K.D. Cognitive assisted living ambient system: A survey. Digit. Commun. Netw. 2015, 1, 229–252. [Google Scholar] [CrossRef]
- Dasios, A.; Gavalas, D.; Pantziou, G.; Konstantopoulos, C. Hands-On Experiences in Deploying Cost-Effective Ambient-Assisted Living Systems. Sensors 2015, 15, 14487–14512. [Google Scholar] [CrossRef]
- Fletcher, J.; Jensen, R. Overcoming Barriers to Mobile Health Technology Use in the Aging Population: OJNI. J. Nurs. Inform. 2015, 19. Available online: http://www.himss.org/ojni (accessed on 1 December 2022).
- Ni, Q.; García Hernando, A.B.; De la Cruz, I.P. The Elderly’s Independent Living in Smart Homes: A Characterization of Activities and Sensing Infrastructure Survey to Facilitate Services Development. Sensors 2015, 15, 11312–11362. [Google Scholar] [CrossRef]
- Jacobsson, A.; Boldt, M.; Carlsson, B. A risk analysis of a smart home automation system. Future Gener. Comput. Syst. 2016, 56, 719–733. [Google Scholar] [CrossRef]
- Wang, J.; Carroll, D.; Peck, M.; Myneni, S.; Gong, Y. Mobile and Wearable Technology Needs for Aging in Place: Perspectives from Older Adults and Their Caregivers and Providers. Study Health Technol. Inform. 2016, 225, 486–490. [Google Scholar]
- Wilson, C.; Hargreaves, T.; Hauxwell-Baldwin, R. Benefits and risks of smart home technologies. Energy Policy 2017, 103, 72–83. [Google Scholar] [CrossRef]
- Alsinglawi, B.; Nguyen, Q.V.; Gunawardana, U.; Maeder, A.; Simoff, S. RFID Systems in Healthcare Settings and Activity of Daily Living in Smart Homes: A Review. E-Health Telecommun. Syst. Netw. 2017, 6, 1–17. [Google Scholar] [CrossRef][Green Version]
- Majumder, S.; Aghayi, E.; Noferesti, M.; Memarzadeh-Tehran, H.; Mondal, T.; Pang, Z.; Deen, M.J. Smart Homes for Elderly Healthcare-Recent Advances and Research Challenges. Sensors 2017, 17, 2496. [Google Scholar] [CrossRef] [PubMed]
- Hallewell Haslwanter, J.; Fitzpatrick, G. The Development of Assistive Systems to Support Older People: Issues that Affect Success in Practice. Technologies 2017, 6, 2. [Google Scholar] [CrossRef]
- Do, H.M.; Pham, M.; Sheng, W.; Yang, D.; Liu, M. RiSH: A robot-integrated smart home for elderly care. Robot. Auton. Syst. 2018, 101, 74–92. [Google Scholar] [CrossRef]
- Biermann, H.; Offermann-van Heek, J.; Himmel, S.; Ziefle, M. Ambient Assisted Living as Support for Aging in Place: Quantitative Users’ Acceptance Study on Ultrasonic Whistles. JMIR Aging 2018, 1, e11825. [Google Scholar] [CrossRef]
- Pal, D.; Funilkul, S.; Vanijja, V.; Papasratorn, B. Analyzing the Elderly Users’ Adoption of Smart-Home Services. IEEE Access 2018, 6, 51238–51252. [Google Scholar] [CrossRef]
- Spann, A.; Stewart, E. Barriers and facilitators of older people’s mHealth usage: A qualitative review of older people’s views. Hum. Technol. 2018, 14, 264–296. [Google Scholar] [CrossRef]
- Bozan, K.; Berger, A. Revisiting the technology challenges and proposing enhancements in ambient assisted living for the elderly. In Proceedings of the Annual Hawaii International Conference on System Sciences IEEE Computer Society, Wailea, HI, USA, 8–11 January 2019; pp. 4307–4316. [Google Scholar]
- Marikyan, D.; Papagiannidis, S.; Alamanos, E. A systematic review of the smart home literature: A user perspective. Technol. Forecast. Soc. Chang. 2019, 138, 139–154. [Google Scholar] [CrossRef]
- El Murabet, A.; Abtoy, A. Understanding the ambient Assisted Living systems: Concepts, architectural trends and challenges. Int. J. Open Inf. Technol. 2019, 7, 25–33. [Google Scholar]
- Grgurić, A.; Mošmondor, M.; Huljenić, D. The SmartHabits: An Intelligent Privacy-Aware Home Care Assistance System. Sensors 2019, 19, 907. [Google Scholar] [CrossRef]
- Wang, S.; Bolling, K.; Mao, W.; Reichstadt, J.; Jeste, D.; Kim, H.C.; Nebeker, C. Technology to Support Aging in Place: Older Adults’ Perspectives. Healthcare 2019, 7, 60. [Google Scholar] [CrossRef] [PubMed]
- Choukou, M.A.; Shortly, T.; Leclerc, N.; Freier, D.; Lessard, G.; Demers, L.; Auger, C. Evaluating the acceptance of ambient assisted living technology (AALT) in rehabilitation: A scoping review. Int. J. Med. Inform. 2021, 150, 104461. [Google Scholar] [CrossRef] [PubMed]
- ISO. Ergonomics of Human-System Interaction—Part 11: Usability: Definitions and Concepts; International Organization for Standardization: Geneva, Switzerland, 2018. [Google Scholar]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
|
|
|
|
| Authors and Years | Types of Technologies | ||||
|---|---|---|---|---|---|
| Ambient Assisted Living (AAL) | Smart Home (SH) | Assistive Robotics (AR) | Wearable and Mobile Devices (WMD) | e-T | |
| Sun et al. (2009) [25] | ✓ | ||||
| Muñoz et al. (2011) [6] | ✓ | ||||
| Ding et al. (2011) [26] | ✓ | ||||
| Pogorelc et al. (2012) [27] | ✓ | ||||
| Wu et al. (2012) [28] | ✓ | ||||
| Grgurić, (2012) [29] | ✓ | ||||
| Chan et al. (2012) [30] | ✓ | ||||
| Paoli et al. (2012) [31] | ✓ | ||||
| Lê et al. (2012) [32] | ✓ | ||||
| Flandorfer, (2012) [33] | ✓ | ||||
| Balta-Ozkan et al. (2013) [9] | ✓ | ||||
| Portet et al. (2013) [34] | ✓ | ||||
| Berglin, (2013) [10] | ✓ | ||||
| Ayala & Amor (2013) [7] | ✓ | ||||
| Khosla et al. (2013) [35] | ✓ | ||||
| Kim & Jeong (2013) [36] | ✓ | ||||
| Parker et al. (2013) [37] | ✓ | ||||
| Rashidi & Mihailidis (2013) [38] | ✓ | ||||
| Spitalewsky et al. (2013) [39] | ✓ | ||||
| Morris et al. (2013) [40] | ✓ | ||||
| AALIANCE2, (2014) [19] | ✓ | ||||
| Memon et al. (2014) [41] | ✓ | ||||
| Spasova & Iliev (2014) [42] | ✓ | ||||
| Wu et al. (2014) [43] | ✓ | ||||
| Hersh (2015) [44] | ✓ | ||||
| Jaschinski & Allouch (2015) [45] | ✓ | ||||
| Peruzzini & Germani (2015) [46] | ✓ | ||||
| Li et al. (2015) [47] | ✓ | ||||
| Dasios et al. (2015) [48] | ✓ | ||||
| Fletcher & Jensen (2015) [49] | ✓ | ||||
| Ni et al. (2015) [50] | ✓ | ||||
| Jacobsson et al. (2016) [51] | ✓ | ||||
| Al-Shaqi et al. (2016) [4] | ✓ | ||||
| Ariani et al. (2016) [5] | ✓ | ||||
| Wang et al. (2016) [52] | ✓ | ||||
| Wilson et al. (2017) [53] | ✓ | ||||
| Alsinglawi et al. (2017) [54] | ✓ | ||||
| Majumder et al. (2017) [55] | ✓ | ||||
| Halslwanter & Fitzpatrick (2017) [56] | ✓ | ||||
| Gonçalves et al.,(2018) [8] | ✓ | ||||
| Do et al. (2018) [57] | ✓ | ||||
| Biermann et al. (2018) [58] | ✓ | ||||
| Pal et al. (2018) [59] | ✓ | ||||
| Carnemolla, (2018) [20] | ✓ | ||||
| Spann & Stewart (2018) [60] | ✓ | ||||
| Bozan & Berger (2019) [61] | ✓ | ||||
| Marikyan et al. (2019) [62] | ✓ | ||||
| Pal et al. (2019) [59] | ✓ | ||||
| El & Abtoy (2019) [63] | ✓ | ||||
| Grgurić et al. (2019) [64] | ✓ | ||||
| Wang et al. (2019) [65] | ✓ | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almalki, M.; Alsulami, M.H.; Alshdadi, A.A.; Almuayqil, S.N.; Alsaqer, M.S.; Atkins, A.S.; Choukou, M.-A. Delivering Digital Healthcare for Elderly: A Holistic Framework for the Adoption of Ambient Assisted Living. Int. J. Environ. Res. Public Health 2022, 19, 16760. https://doi.org/10.3390/ijerph192416760
Almalki M, Alsulami MH, Alshdadi AA, Almuayqil SN, Alsaqer MS, Atkins AS, Choukou M-A. Delivering Digital Healthcare for Elderly: A Holistic Framework for the Adoption of Ambient Assisted Living. International Journal of Environmental Research and Public Health. 2022; 19(24):16760. https://doi.org/10.3390/ijerph192416760
Chicago/Turabian StyleAlmalki, Manal, Majid H. Alsulami, Abdulrahman A. Alshdadi, Saleh N. Almuayqil, Mohammed S. Alsaqer, Anthony S. Atkins, and Mohamed-Amine Choukou. 2022. "Delivering Digital Healthcare for Elderly: A Holistic Framework for the Adoption of Ambient Assisted Living" International Journal of Environmental Research and Public Health 19, no. 24: 16760. https://doi.org/10.3390/ijerph192416760
APA StyleAlmalki, M., Alsulami, M. H., Alshdadi, A. A., Almuayqil, S. N., Alsaqer, M. S., Atkins, A. S., & Choukou, M.-A. (2022). Delivering Digital Healthcare for Elderly: A Holistic Framework for the Adoption of Ambient Assisted Living. International Journal of Environmental Research and Public Health, 19(24), 16760. https://doi.org/10.3390/ijerph192416760







