An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management
Abstract
:1. Introduction
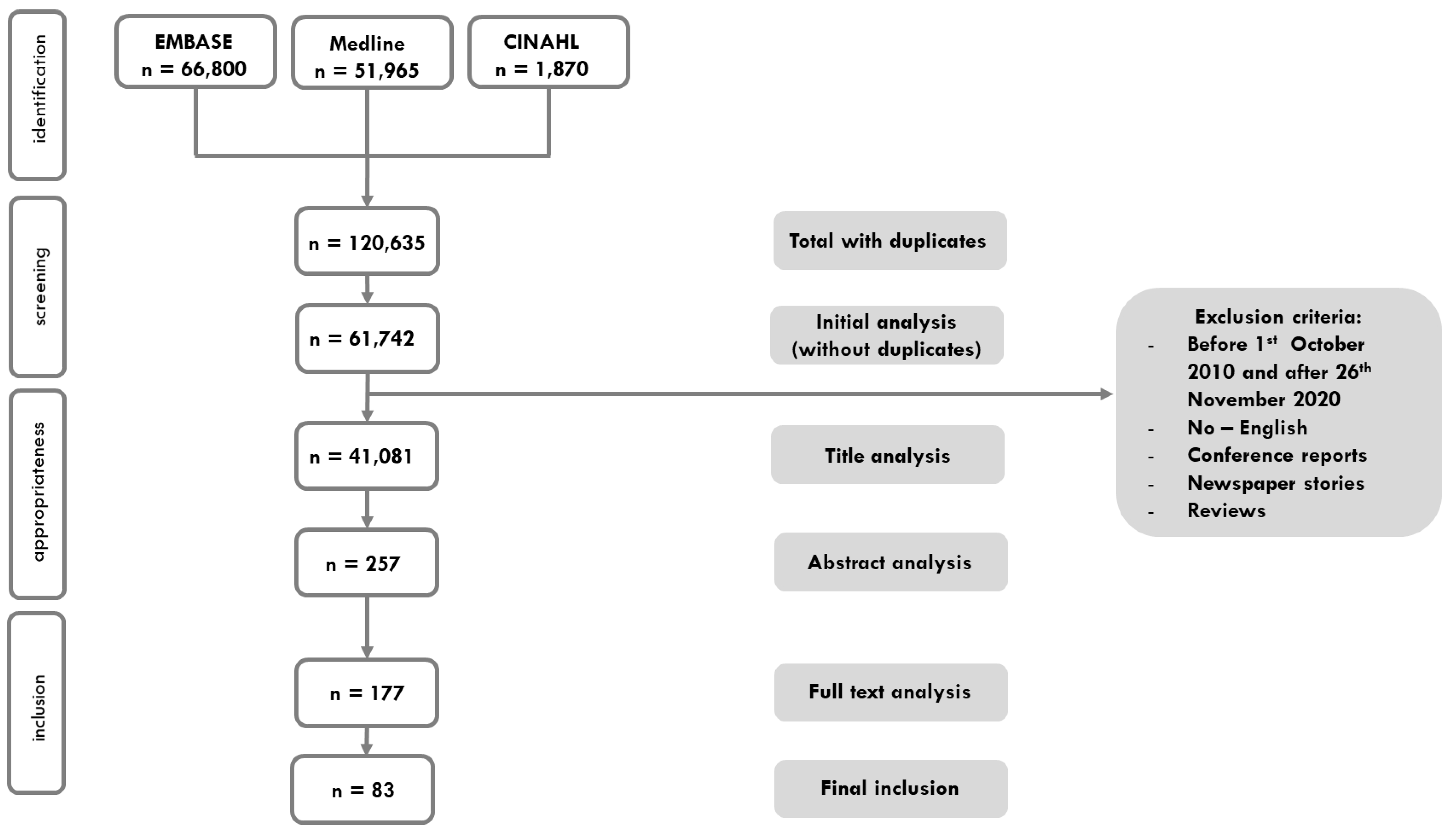
2. Materials and Methods
2.1. Information Sources and Search Strategy
2.2. Eligibility Criteria
2.3. Article Screening
2.4. Data Extraction
2.5. Data Synthesis
2.6. Building the New Definition
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Patient Safety Action Plan 2021–2030. Towards Zero Patients Harm in Healthcare. 2020. Available online: https://www.who.int/teams/integrated-health-services/patient-safety/policy/global-patient-safety-action-plan (accessed on 13 November 2022).
- Wu, A.W. Medical Error: The Second Victim. The Doctor Who Makes the Mistake Needs Help Too. BMJ 2000, 320, 726–727. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.D.; Hirschinger, L.E.; Cox, K.R.; McCoig, M.; Brandt, J.; Hall, L.W. The Natural History of Recovery for the Healthcare Provider “Second Victim” after Adverse Patient Events. Qual. Saf. Health Care 2009, 18, 325–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Gerven, E.; Elst, T.V.; Vandenbroeck, S.; Dierickx, S.; Euwema, M.; Sermeus, W.; De Witte, H.; Godderis, L.; Vanhaecht, K. Increased Risk of Burnout for Physicians and Nurses Involved in a Patient Safety Incident. Med. Care 2016, 54, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Merandi, J.; Winning, A.M.; Liao, N.; Rogers, E.; Lewe, D.; Gerhardt, C.A. Implementation of a Second Victim Program in the Neonatal Intensive Care Unit: An Interim Analysis of Employee Satisfaction. J. Patient Saf. Risk Manag. 2018, 23, 231–238. [Google Scholar] [CrossRef]
- Joaquín, M.J.; Carrillo, I.; Lorenzo, S.; Ferrús, L.; Silvestre, C.; Pérez-Pérez, P.; Olivera, G.; Iglesias, F.; Zavala, E.; Maderuelo-Fernández, J.A.; et al. The Aftermath of Adverse Events in Spanish Primary Care and Hospital Health Professionals. BMC Health Serv. Res. 2015, 15, 151. [Google Scholar]
- Harrison, R.; Lee, H.; Sharma, A. A Survey of the Impact of Patient Adverse Events and near Misses on Anaesthetists in Australia and New Zealand. Anaesth. Intensive Care 2018, 46, 510–515. [Google Scholar] [CrossRef]
- Clarkson, M.D.; Haskell, H.; Hemmelgarn, C.; Skolnik, P.J. Abandon the Term “Second Victim”. BMJ 2019, 364, l1233. [Google Scholar] [CrossRef]
- Gómez-Durán, E.L.; Tolchinsky, G.; Martin-Fumadó, C.; Arimany-Manso, J. Neglecting the “Second Victim” Will Not Help Harmed Patients or Improve Patient Safety. BMJ 2019, 365, l2167. [Google Scholar] [CrossRef]
- Petersen, I.G. The Term “Second Victim” Is Appropriate for Frontline Workers. BMJ 2019, 365, l2157. [Google Scholar] [CrossRef]
- Media, A. ‘Second Victim’ May Not Be the Best Approach to Adverse Events. Healthc. Risk Manag. 2019, 41. Available online: https://www.reliasmedia.com/articles/144971-second-victim-may-not-be-the-best-approach-to-adverse-events (accessed on 13 November 2022).
- Tumelty, M.E. The Second Victim: A Contested Term? J. Patient Saf. 2018, 17, e1488–e1493. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.W.; Shapiro, J.; Harrison, R.; Scott, S.D.; Connors, C.; Kenney, L.; Vanhaecht, K. The Impact of Adverse Events on Clinicians: What’s in a Name? J. Patient Saf. 2020, 16, 65–72. [Google Scholar] [CrossRef] [PubMed]
- The European Researchers’ Network Working on Second Victims (ERNST) (COST CA19113). Available online: https://cost-ernst.eu/about/ (accessed on 26 July 2022).
- Seys, D.; De Decker, E.; Waelkens, H.; Claes, S.; Panella, M.; Danckaerts, M.; Vanhaecht, K. A Comparative Study Measuring the Difference of Healthcare Workers Reactions among Those Involved in a Patent Safety Incident and Healthcare Professionals While Working During Covid-19. J. Patient Saf. 2022, 18, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Van Gerven, E.; Deweer, D.; Scott, S.D.; Panella, M.; Euwema, M.; Sermeus, W.; Vanhaecht, K. Personal, Situational and Organizational Aspects That Influence the Impact of Patient Safety Incidents: A Qualitative Study. Rev. Calid. Asist. 2016, 31, 34–46. [Google Scholar] [CrossRef]
- Van Gerven, E.; Bruyneel, L.; Panella, M.; Euwema, M.; Sermeus, W.; Vanhaecht, K. Psychological Impact and Recovery after Involvement in a Patient Safety Incident: A Repeated Measures Analysis. BMJ Open 2016, 6, e011403. [Google Scholar] [CrossRef] [Green Version]
- Rinaldi, C.; Leigheb, F.; Vanhaecht, K.; Donnarumma, C.; Panella, M. Becoming a “Second Victim” in Health Care: Pathway of Recovery after Adverse Event. Rev. Calid. Asist. 2016, 31 (Suppl. 2), 11–19. [Google Scholar] [CrossRef]
- Panella, M.; Rinaldi, C.; Leigheb, F.; Donnarumma, C.; Kul, S.; Vanhaecht, K.; di Stanislao, F. The Determinants of Defensive Medicine in Italian Hospitals: The Impact of Being a Second Victim. Rev. Calid. Asist. 2016, 31 (Suppl. 2), 20–25. [Google Scholar] [CrossRef]
- Rinaldi, C.; Leigheb, F.; di Dio, A.; Vanhaecht, K.; Donnarumma, C.; Panella, M. Second Victims in Healthcare: The Stages of Recovery Following an Adverse Event. Ig. E Sanita Pubblica 2016, 72, 357–370. [Google Scholar]
- Panella, M.; Rinaldi, C.; Vanhaecht, K.; Donnarumma, C.; Tozzi, Q.; di Stanislao, F. Second Victims of Medical Errors: A Systematic Review of the Literature. Ig. E Sanita Pubblica 2014, 70, 9–28. [Google Scholar]
- Vanhaecht, K.; Seys, D.; Schouten, L.; Bruyneel, L.; Coeckelberghs, E.; Panella, M.; Zeeman, G. Duration of Second Victim Symptoms in the Aftermath of a Patient Safety Incident and Association with the Level of Patient Harm: A Cross-Sectional Study in the Netherlands. BMJ Open 2019, 9, e029923. [Google Scholar] [CrossRef]
- Seys, D.; Wu, A.W.; Gerven, E.V.; Vleugels, A.; Euwema, M.; Panella, M.; Scott, S.D.; Conway, J.; Sermeus, W.; Vanhaecht, K. Health Care Professionals as Second Victims after Adverse Events: A Systematic Review. Eval. Health Prof. 2013, 36, 135–162. [Google Scholar] [CrossRef] [PubMed]
- Rinaldi, C.; Ratti, M.; Russotto, S.; Seys, D.; Vanhaecht, K.; Panella, M. Healthcare Students and Medical Residents as Second Victims: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 12218. [Google Scholar] [CrossRef] [PubMed]
- Vanhaecht, K.; de Ridder, D.; Seys, D.; Brouwers, J.; Claessens, F.; van Wilder, A.; Panella, M.; Batalden, P.; Lachman, P. The History of Quality: From an Eye for an Eye, through Love, and Towards a Multidimensional Concept for Patients, Kin, and Professionals. Eur. Urol. Focus 2021, 7, 937–939. [Google Scholar] [CrossRef] [PubMed]
- Gerven, E.V.; Seys, D.; Panella, M.; Sermeus, W.; Euwema, M.; Federico, F.; Kenney, L.; Vanhaecht, K. Involvement of Health-Care Professionals in an Adverse Event: The Role of Management in Supporting Their Workforce. Pol. Arch. Med. Wewn. 2014, 124, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Zeeman, G.; Schouten, L.; Seys, D.; Coeckelberghs, E.; Weijenborg, P.; Bruyneel, L.; Vanhaecht, K. Prolonged Mental Health Sequelae among Doctors and Nurses Involved in Patient Safety Incidents with Formal Complaints and Lawsuits. Eur. J. Public Health 2020, 30, 777–779. [Google Scholar] [CrossRef]
- Nijs, K.; Seys, D.; Coppens, S.; van de Velde, M.; Vanhaecht, K. Second Victim Support Structures in Anaesthesia: A Cross-Sectional Survey in Belgian Anaesthesiologists. Int. J. Qual. Health Care 2021, 33, mzab058. [Google Scholar] [CrossRef]
- Van Slambrouck, L.; Verschueren, R.; Seys, D.; Bruyneel, L.; Panella, M.; Vanhaecht, K. Second Victims among Baccalaureate Nursing Students in the Aftermath of a Patient Safety Incident: An Exploratory Cross-Sectional Study. J. Prof. Nurs. 2021, 37, 765–770. [Google Scholar] [CrossRef]
- Seys, D.; Scott, S.; Wu, A.; van Gerven, E.; Vleugels, A.; Euwema, M.; Panella, M.; Conway, J.; Sermeus, W.; Vanhaecht, K. Supporting Involved Health Care Professionals (Second Victims) Following an Adverse Health Event: A Literature Review. Int. J. Nurs. Stud. 2013, 50, 678–687. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Larissa, S.; Jennifer, M.T.; Elie, A.A.; Sue, E.B.; et al. The Prisma 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- World Health Organization. Conceptual Framework for the International Classification for Patient Safety Version 1.1: Final Technical Report January 2009. Available online: https://apps.who.int/iris/handle/10665/70882 (accessed on 13 November 2022).
- Lachman, P.; Batalden, P.; Vanhaecht, K. A Multidimensional Quality Model: An Opportunity for Patients, Their Kin, Healthcare Providers and Professionals to Coproduce Health. F1000Res. 2020, 9, 1140. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Psychiatr. Online 2014, 21, 591–643. [Google Scholar]
- Fileni, A.; Magnavita, N.; Mammi, F.; Mandoliti, G.; Lucà, F.; Magnavita, G.; Bergamaschi, A. Malpractice Stress Syndrome in Radiologists and Radiotherapists: Perceived Causes and Consequences. Radiol. Med. 2007, 112, 1069–1084. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Fileni, A.; Magnavita, G.; Mammi, F.; Mirk, P.; Roccia, K.; Bergamaschi, A. Work Stress in Radiologists. A Pilot Study. Radiol. Med. 2008, 113, 329–346. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Magnavita, G.; Fileni, A.; Bergamaschi, A. Ethical Problems in Radiology: Medical Error and Disclosure. Radiol. Med. 2009, 114, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Reason, J. Human Error; Cambridge University: Cambridge, UK, 1990. [Google Scholar]
| Words in Proposed Definition by Academic Taskforce KULeuven-Piemonte University | Words in Final Definition Based on International Expert Consensus Meeting | Explanation of the Adaptation |
|---|---|---|
| Any healthcare provider | Any healthcare worker, directly or indirectly involved … | The event can lead to a negative impact on any type of professional (clinical or non clinical) that was directly involved in an active failure or who was the victim of a latent organizational condition. However, colleagues who were indirectly involved or even not involved in the event itself can have a negative impact. Think about colleagues who were working on the same ward or team during the event, or even non-clinical managers or quality improvement facilitators who feel responsible for the latent condition. |
| unanticipated adverse patient event, medical error, and/or a patient related–injury | … in an unanticipated adverse patient event, unintentional healthcare error, or patient injury … | If a healthcare worker is involved in something potentially catastrophic but with a good outcome, they can also become an SV. Next to this, near misses or events where the clinician had no active failure but there was a negative outcome, should be included. We add “unintentional” as the act was not reckless or malicious and broaden to healthcare error as not all errors are medical. |
| Healthcare provider | … and who becomes victimized in the sense that … | It could be a food service worker, a health facilities worker, a cleaner, who becomes victimized (because of active failures and/or latent conditions) … as long as there is in some way direct or indirect contact with the patient they may feel affected. This is also the case for students. |
| Frequently, second victims feel personally responsible for the unexpected patient outcomes and feel as though they have failed their patient. | Removed | This sentence is a clarification and should not be part of a definition. |
| the healthcare provider | … they are also … (=healthcare worker is also) | We emphasize that patients and kin are the first victims. By “also” we state it is not only the healthcare worker who is negatively impacted. With this we acknowledge the primary impact of the incident on patients and kin. |
| emotionally impacted | … negatively impacted. | It can be any type of negative impact, not only emotional. We acknowledge that there can also be a positive impact of the incident (learning curve, more attention, …). |
| by the event | Removed | This is a repeat and therefore removed in the consensus definition. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vanhaecht, K.; Seys, D.; Russotto, S.; Strametz, R.; Mira, J.; Sigurgeirsdóttir, S.; Wu, A.W.; Põlluste, K.; Popovici, D.G.; Sfetcu, R.; et al. An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management. Int. J. Environ. Res. Public Health 2022, 19, 16869. https://doi.org/10.3390/ijerph192416869
Vanhaecht K, Seys D, Russotto S, Strametz R, Mira J, Sigurgeirsdóttir S, Wu AW, Põlluste K, Popovici DG, Sfetcu R, et al. An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management. International Journal of Environmental Research and Public Health. 2022; 19(24):16869. https://doi.org/10.3390/ijerph192416869
Chicago/Turabian StyleVanhaecht, Kris, Deborah Seys, Sophia Russotto, Reinhard Strametz, José Mira, Sigurbjörg Sigurgeirsdóttir, Albert W. Wu, Kaja Põlluste, Daniela Georgeta Popovici, Raluca Sfetcu, and et al. 2022. "An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management" International Journal of Environmental Research and Public Health 19, no. 24: 16869. https://doi.org/10.3390/ijerph192416869
APA StyleVanhaecht, K., Seys, D., Russotto, S., Strametz, R., Mira, J., Sigurgeirsdóttir, S., Wu, A. W., Põlluste, K., Popovici, D. G., Sfetcu, R., Kurt, S., & Panella, M., on behalf of European Researchers’ Network Working on Second Victims (ERNST). (2022). An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management. International Journal of Environmental Research and Public Health, 19(24), 16869. https://doi.org/10.3390/ijerph192416869









