Morphometric Analysis of the Midline Mandibular Lingual Canal and Mandibular Lingual Foramina: A Cone Beam Computed Tomography (CBCT) Evaluation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
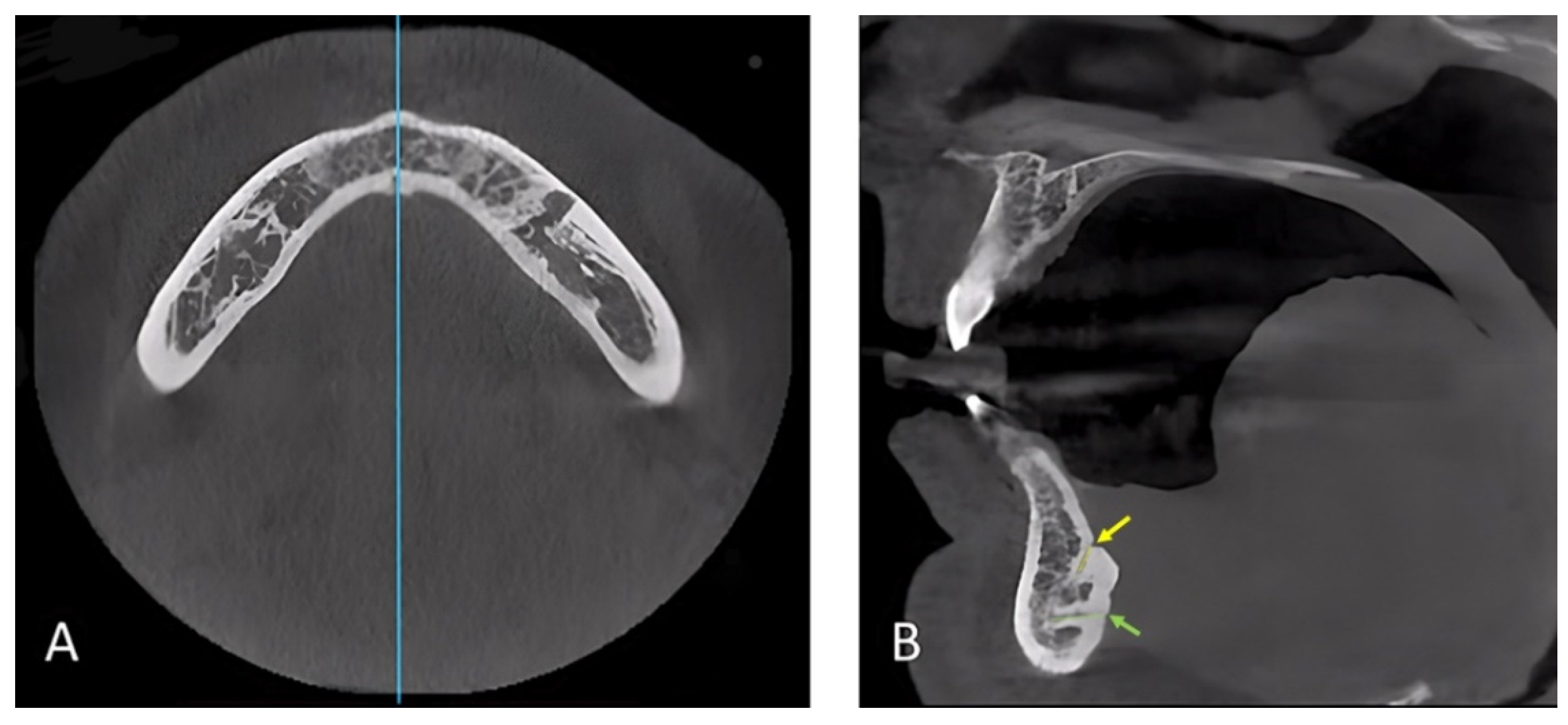
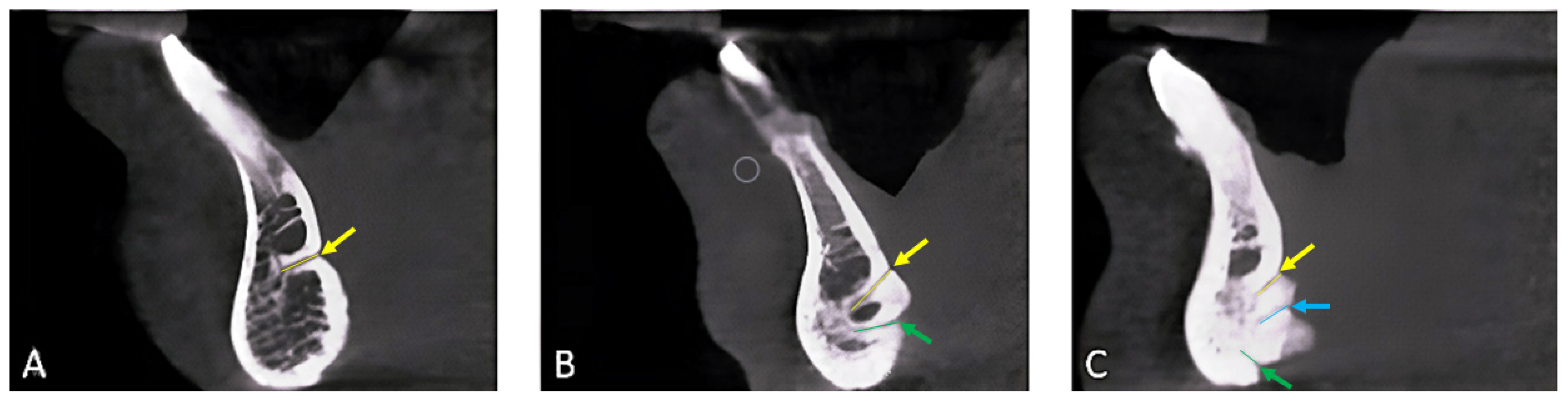
2.2. Data Collection, Image Reconstruction, and Assessments
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Woo, B.M.; Al-Bustani, S.; Ueeck, B.A. Floor of Mouth Haemorrhage and Life-Threatening Airway Obstruction during Immediate Implant Placement in the Anterior Mandible. Int. J. Oral Maxillofac. Surg. 2006, 35, 961–964. [Google Scholar] [CrossRef] [PubMed]
- Goller Bulut, D.; Köse, E. Available Bone Morphology and Status of Neural Structures in the Mandibular Interforaminal Region: Three-Dimensional Analysis of Anatomical Structures. Surg. Radiol. Anat. 2018, 40, 1243–1252. [Google Scholar] [CrossRef] [PubMed]
- Alqutaibi, A.Y.; Kaddah, A.F.; Farouk, M. Randomized Study on the Effect of Single-Implant versus Two-Implant Retained Overdentures on Implant Loss and Muscle Activity: A 12-Month Follow-up Report. Int. J. Oral Maxillofac. Surg. 2017, 46, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Alqutaibi, A.Y.; Esposito, M.; Algabri, R.; Alfahad, A.; Kaddah, A.F.; Farouk, M.; Alsourori, A. Single vs. Two Implant-Retained Overdentures for Edentulous Mandibles: A Systematic Review. Eur. J. Oral Implantol. 2017, 10, 243–261. [Google Scholar] [PubMed]
- Liang, X.; Jacobs, R.; Lambrichts, I.; Vandewalle, G. Lingual Foramina on the Mandibular Midline Revisited: A Macroanatomical Study. Clin. Anat. 2007, 20, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Asaumi, R.; Sato, I.; Yoshida, S.; Yosue, T.; Kawai, T.; Asaumi, R.; Yosue, T.; Sato, I.; Yoshida, S. Classification of the Lingual Foramina and Their Bony Canals in the Median Region of the Mandible: Cone Beam Computed Tomography Observations of Dry Japanese Mandibles. Oral Radiol. 2007, 23, 42–48. [Google Scholar] [CrossRef]
- Rosano, G.; Taschieri, S.; Gaudy, J.F.; Testori, T.; del Fabbro, M. Anatomic Assessment of the Anterior Mandible and Relative Hemorrhage Risk in Implant Dentistry: A Cadaveric Study. Clin. Oral Implants Res. 2009, 20, 791–795. [Google Scholar] [CrossRef]
- Mordenfeld, A. Hemorrhage in the Floor of the Mouth During Implant. Int. J. Oral Maxillofac. Implants 1997, 12, 558–561. [Google Scholar]
- Longoni, S.; Sartori, M.; Braun, M.; Bravetti, P.; Lapi, A.; Baldoni, M. Lingual Vascular Canals of the Mandible: The Risk of Bleeding Complications during Implant Procedures. Implants Dent. 2007, 16, 131–138. [Google Scholar] [CrossRef]
- Jacobs, R.; Mraiwa, N.D.; Gijbels, F.; Quirynen, M. Appearance, Location, Course, and Morphology of the Mandibular Incisive Canal: An Assessment on Spiral CT Scan. Dentomaxillofac. Radiol. 2002, 31, 322–327. [Google Scholar] [CrossRef]
- Aoun, G.; Nasseh, I.; Sokhn, S.; Rifai, M. Lingual Foramina and Canals of the Mandible: Anatomic Variations in a Lebanese Population. J. Clin. Imaging Sci. 2017, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Poovannan, S.; Sarumathi, T. Prevalence and Anatomic Variations of Lingual Foramina and Lingual Canal in Anterior Mandible Using Cone Beam Computed Tomography—A Cross-Sectional Study. J. Indian Acad. Oral Med. Radiol. 2022, 34, 324. [Google Scholar] [CrossRef]
- Tepper, G.; Hofschneider, U.B.; Gahleitner, A.; Ulm, C. Computed Tomographic Diagnosis and Localization of Bone Canals in the Mandibular Interforaminal Region for Prevention of Bleeding Complications during Implant Surgery. Int. J. Oral Maxillofac. Implants 2001, 16, 68–72. [Google Scholar] [PubMed]
- Babiuc, I.; Tarlungeanu, I.; Pauna, M. Cone Beam Computed Tomography Observations of the Lingual Foramina and Their Bony Canals in the Median Region of the Mandible. Rom. J. Morphol. Embryol. 2011, 52, 827–829. [Google Scholar] [PubMed]
- Sheikhi, M.; Mosavat, F.; Ahmadi, A. Assessing the Anatomical Variations of Lingual Foramen and Its Bony Canals with CBCT Taken from 102 Patients in Isfahan. Dent. Res. J. Isfahan 2012, 9, 45–51. [Google Scholar]
- Barbosa, D.A.F.; de Mendonça, D.S.; de Carvalho, F.S.R.; Kurita, L.M.; de Barros Silva, P.G.; Neves, F.S.; Costa, F.W.G. Systematic Review and Meta-Analysis of Lingual Foramina Anatomy and Surgical-Related Aspects on Cone-Beam Computed Tomography: A Prospero-Registered Study. Oral Radiol. 2022, 38, 1–16. [Google Scholar] [CrossRef]
- Choi, D.Y.; Woo, Y.J.; Won, S.Y.; Kim, D.H.; Kim, H.J.; Hu, K.S. Topography of the Lingual Foramen Using Micro-Computed Tomography for Improving Safety during Implant Placement of Anterior Mandibular Region. J. Craniofac. Surg. 2013, 24, 1403–1407. [Google Scholar] [CrossRef]
- Sanchez-Perez, A.; Boix-Garcia, P.; Lopez-Jornet, P. Cone-Beam CT Assessment of the Position of the Medial Lingual Foramen for Dental Implant Placement in the Anterior Symphysis. Implants Dent. 2018, 27, 43–48. [Google Scholar] [CrossRef]
- Lakha, T.; Kheur, M.; Mühlemann, S.; Kheur, S.; Le, B. Ultrasound and CBCT Analysis of Blood Flow and Dimensions of the Lingual Vascular Canal: A Case Control Study. J. Oral Biol. Craniofac. Res. 2020, 11, 40–46. [Google Scholar] [CrossRef]
- Mraiwa, N.; Jacobs, R.; Moerman, P.; Lambrichts, I.; van Steenberghe, D.; Quirynen, M. Presence and Course of the Incisive Canal in the Human Mandibular Interforaminal Region: Two-Dimensional Imaging versus Anatomical Observations. Surg. Radiol. Anat. 2003, 25, 416–423. [Google Scholar] [CrossRef]
- Yılmaz, S.; Calikoglu, E.O.; Kosan, Z. For an Uncommon Neurosurgical Emergency in a Developing Country. Niger. J. Clin. Pract. 2017, 22, 1070–1077. [Google Scholar] [CrossRef]
- Jasa, G.R.; Shimizu, M.; Okamura, K.; Tokumori, K.; Takeshita, Y.; Weerawanich, W.; Yoshiura, K. Effects of Exposure Parameters and Slice Thickness on Detecting Clear and Unclear Mandibular Canals Using Cone Beam CT. Dentomaxillofac. Radiol. 2017, 46, 20160315. [Google Scholar] [CrossRef] [PubMed]
- Oettlé, A.C.; Fourie, J.; Human-Baron, R.; Zyl, A.W. The Midline Mandibular Lingual Canal: Importance in Implant Surgery. Clin. Implants Dent. Relat. Res. 2013, 17, 93–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, P.; Truong, M.K.; Adeeb, N.; Tubbs, R.S.; Iwanaga, J. Clinical Anatomy and Surgical Significance of the Lingual Foramina and Their Canals. Clin. Anat. 2017, 30, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.N.R.; Zhang, Y.; Zuben, M.; Vargas, W.; Seedat, H.C.; Santiago, F. Worldwide Prevalence of a Lingual Canal in Mandibular Premolars: A Multicenter Cross-Sectional Study with Meta-Analysis. J. Endod. 2021, 47, 1253–1264. [Google Scholar] [CrossRef]
- Katakami, K.; Mishima, A.; Kuribayashi, A.; Shimoda, S.; Hamada, Y.; Kobayashi, K. Anatomical Characteristics of the Mandibular Lingual Foramina Observed on Limited Cone-Beam CT Images. Clin. Oral Res. 2009, 20, 386–390. [Google Scholar] [CrossRef]
- Liang, X.; Jacobs, R.; Corpas, L.S.; Semal, P.; Lambrichts, I. Chronologic and Geographic Variability of Neurovascular Structures in the Human Mandible. Forensic Sci. Int. 2009, 190, 24–32. [Google Scholar] [CrossRef]
- Tagaya, A.; Matsuda, Y.; Nakajima, K.; Seki, K.; Okano, T. Assessment of the Blood Supply to the Lingual Surface of the Mandible for Reduction of Bleeding during Implant Surgery. Clin. Oral Implants Res. 2009, 20, 351–355. [Google Scholar] [CrossRef]
- von Arx, T.; Matter, D.; Buser, D.; Bornstein, M.M. Evaluation of Location and Dimensions of Lingual Foramina Using Limited Cone-Beam Computed Tomography. J. Oral Maxillofac. Surg. 2011, 69, 2777–2785. [Google Scholar] [CrossRef]
- He, X.; Jiang, J.; Cai, W.; Pan, Y.; Yang, Y.; Zhu, K.; Zheng, Y. Assessment of the Appearance, Location and Morphology of Mandibular Lingual Foramina Using Cone Beam Computed Tomography. Int. Dent. J. 2016, 66, 272–279. [Google Scholar] [CrossRef]
- Nimigean, V.; Sîrbu, V.D.; Nimigean, V.R.; Bădiţă, D.G.; Poll, A.; Moraru, S.A.; Păun, D.L. Morphological Assessment of the Mandibular Canal Trajectory in Edentate Subjects. Rom. J. Morphol. Embryol. 2018, 59, 235–242. [Google Scholar] [PubMed]
- Taschieri, S.; Corbella, S.; Silnovic, A.; Francetti, L.; Messina, C.; Sconfienza, L.M.; Albano, D. Frequency and Anatomic Variability of the Mandibular Lingual Foramina: A Cone-Beam CT Study. BMC Med. Imaging 2022, 22, 12. [Google Scholar] [CrossRef] [PubMed]


| No. | % | |
|---|---|---|
| Supra-spinosum only | 83 | 25.9 |
| Infra-spinosum only | 15 | 4.7 |
| Supra with Inter-spinosum | 0 | 0.0 |
| Supra with Infra -spinosum | 175 | 54.7 |
| Supra-Inter-Infra together | 47 | 14.7 |
| Variable | Category | Min.–Max. | Mean ± SD | Median (IQR) |
|---|---|---|---|---|
| Inferior border to buccal terminal (mm) | supra-spinosum | 5.30–17.75 | 11.03 ± 2.40 | 11.18 (9.3–12.67) |
| inter-spinosum | 3.68–13.85 | 8.26 ± 2.16 | 8.17 (6.60–9.91) | |
| infra-spinosum | 0.53–12.55 | 6.44 ± 2.13 | 6.42 (4.99–7.73) | |
| Inferior border to lingual terminal (mm) | supra-spinosum | 6.86–20.05 | 14.95 ± 2.19 | 15.15 (13.6–16.4) |
| inter-spinosum | 2.97–13.85 | 8.70 ± 2.42 | 8.49 (7.77–10.26) | |
| infra-spinosum | 0.58–14.15 | 5.25 ± 2.71 | 4.78 (3.36–6.73) | |
| Buccal cortex to buccal terminal (mm) | supra-spinosum | 1.66–10.50 | 5.84 ± 1.69 | 5.76 (4.53–6.96) |
| inter-spinosum | 2.75–9.58 | 5.96 ± 1.70 | 5.84 (4.61–7.12) | |
| infra-spinosum | 1.54–13.0 | 5.81 ± 1.76 | 5.65 (4.44–6.86) | |
| Length (mm) | supra-spinosum | 1.50–12.33 | 5.81 ± 2.08 | 5.54 (4.15–7.36) |
| inter-spinosum | 2.41–9.39 | 5.52 ± 1.75 | 4.98 (4.12–7.0) | |
| infra-spinosum | 1.35–9.53 | 5.16 ± 1.86 | 4.91 (3.65–6.61) | |
| Diameter at buccal terminal (mm) | supra-spinosum | 0.22–1.76 | 0.60 ± 0.20 | 0.59 (0.48–0.70) |
| inter-spinosum | 0.18–1.21 | 0.54 ± 0.22 | 0.53 (0.41–0.62) | |
| infra-spinosum | 0.13–1.58 | 0.55 ± 0.20 | 0.52 (0.41–0.66) | |
| Diameter at lingual terminal (mm) | supra-spinosum | 0.30–1.97 | 0.87 ± 0.30 | 0.83 (0.65–1.03) |
| inter-spinosum | 0.38–1.69 | 0.76 ± 0.35 | 0.66 (0.55–0.91) | |
| infra-spinosum | 0.18–2.06 | 0.80 ± 0.32 | 0.75 (0.59–0.95) |
| Male (n = 160) | Female (n = 160) | p Value | |||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Number of canals | <0.001 * | ||||
| 1 | 30 | 18.0 | 69 | 43.1 | |
| 2 | 96 | 60.0 | 78 | 48.8 | |
| 3 | 34 | 21.3 | 13 | 8.1 | |
| Supra-spinosum | 0.791 | ||||
| Present | 152 | 95.0 | 153 | 95.6 | |
| Absent | 8 | 5.0 | 7 | 4.4 | |
| Inter-spinosum | 0.001 * | ||||
| Present | 34 | 21.3 | 13 | 8.1 | |
| Absent | 126 | 78.8 | 147 | 91.9 | |
| Infra-spinosum | <0.001 * | ||||
| Present | 138 | 86.3 | 99 | 61.9 | |
| Absent | 22 | 13.8 | 61 | 38.1 | |
| Variable | Category | Male (n = 160) (Mean ± SD) | Female (n = 160) (Mean ± SD) | p Value |
|---|---|---|---|---|
| Inferior border to buccal terminal (mm) | supra-spinosum | 11.55 ± 2.49 | 10.51 ± 2.21 | <0.001 * |
| inter-spinosum | 8.97 ± 2.0 | 6.53 ± 1.47 | <0.001 * | |
| infra-spinosum | 7.12 ± 2.06 | 5.52 ± 1.87 | <0.001 * | |
| Inferior border to lingual terminal (mm) | supra-spinosum | 15.45 ± 2.25 | 14.44 ± 2.01 | <0.001 * |
| inter-spinosum | 9.21 ± 2.47 | 7.45 ± 1.78 | 0.020 * | |
| infra-spinosum | 5.30 ± 2.91 | 5.17 ± 2.43 | 0.85 | |
| Buccal cortex to buccal terminal (mm) | supra-spinosum | 6.0 ± 1.59 | 5.69 ± 1.77 | 0.11 |
| inter-spinosum | 6.29 ± 1.65 | 5.15 ± 1.61 | 0.033 * | |
| infra-spinosum | 5.89 ± 1.65 | 5.69 ± 1.90 | 0.38 | |
| Length (mm) | supra-spinosum | 6.18 ± 2.16 | 5.45 ± 1.93 | 0.006 * |
| inter-spinosum | 5.46 ± 1.73 | 5.65 ± 1.84 | 0.74 | |
| infra-spinosum | 5.40 ± 1.79 | 4.82 ± 1.91 | 0.015 * | |
| Diameter at the buccal terminal (mm) | supra-spinosum | 0.65 ± 0.19 | 0.55 ± 0.20 | <0.001 * |
| inter-spinosum | 0.60 ± 0.21 | 0.41 ± 0.20 | 0.004 * | |
| infra-spinosum | 0.58 ± 0.17 | 0.50 ± 0.22 | <0.001 * | |
| Diameter at the lingual terminal (mm) | supra-spinosum | 0.84 ± 0.27 | 0.90 ± 0.33 | 0.233 |
| inter-spinosum | 0.85 ± 0.37 | 0.55 ± 0.09 | 0.002 * | |
| infra-spinosum | 0.84 ± 0.33 | 0.74 ± 0.30 | 0.008 * |
| N | Length (mm) vs. Diameter at the Lingual Terminal (mm) | ||
|---|---|---|---|
| rs | p | ||
| Supra-spinosum | 304 | 0.169 * | 0.003 * |
| Inter-spinosum | 48 | 0.139 | 0.345 |
| Infra-spinosum | 238 | 0.079 | 0.222 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqutaibi, A.Y.; Alassaf, M.S.; Elsayed, S.A.; Alharbi, A.S.; Habeeb, A.T.; Alqurashi, M.A.; Albulushi, K.A.; Elboraey, M.O.; Alsultan, K.; Mahmoud, I.I. Morphometric Analysis of the Midline Mandibular Lingual Canal and Mandibular Lingual Foramina: A Cone Beam Computed Tomography (CBCT) Evaluation. Int. J. Environ. Res. Public Health 2022, 19, 16910. https://doi.org/10.3390/ijerph192416910
Alqutaibi AY, Alassaf MS, Elsayed SA, Alharbi AS, Habeeb AT, Alqurashi MA, Albulushi KA, Elboraey MO, Alsultan K, Mahmoud II. Morphometric Analysis of the Midline Mandibular Lingual Canal and Mandibular Lingual Foramina: A Cone Beam Computed Tomography (CBCT) Evaluation. International Journal of Environmental Research and Public Health. 2022; 19(24):16910. https://doi.org/10.3390/ijerph192416910
Chicago/Turabian StyleAlqutaibi, Ahmed Yaseen, Muath Saad Alassaf, Shadia A. Elsayed, Abdulmajeed Saud Alharbi, Abdulsamad Talaat Habeeb, Marwan Ahmad Alqurashi, Khalid Ahmed Albulushi, Mohamed Omar Elboraey, Kamal Alsultan, and Ihab Ismail Mahmoud. 2022. "Morphometric Analysis of the Midline Mandibular Lingual Canal and Mandibular Lingual Foramina: A Cone Beam Computed Tomography (CBCT) Evaluation" International Journal of Environmental Research and Public Health 19, no. 24: 16910. https://doi.org/10.3390/ijerph192416910









