Gender and Socioeconomic Differences in the Prevalence and Patterns of Multimorbidity among Middle-Aged and Older Adults in China
Abstract
:1. Introduction
2. Methods
2.1. Data and Sample
2.2. Variables and Instruments
2.2.1. Multimorbidity and Multimorbidity Patterns
2.2.2. Socioeconomic Status
2.2.3. Covariates
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
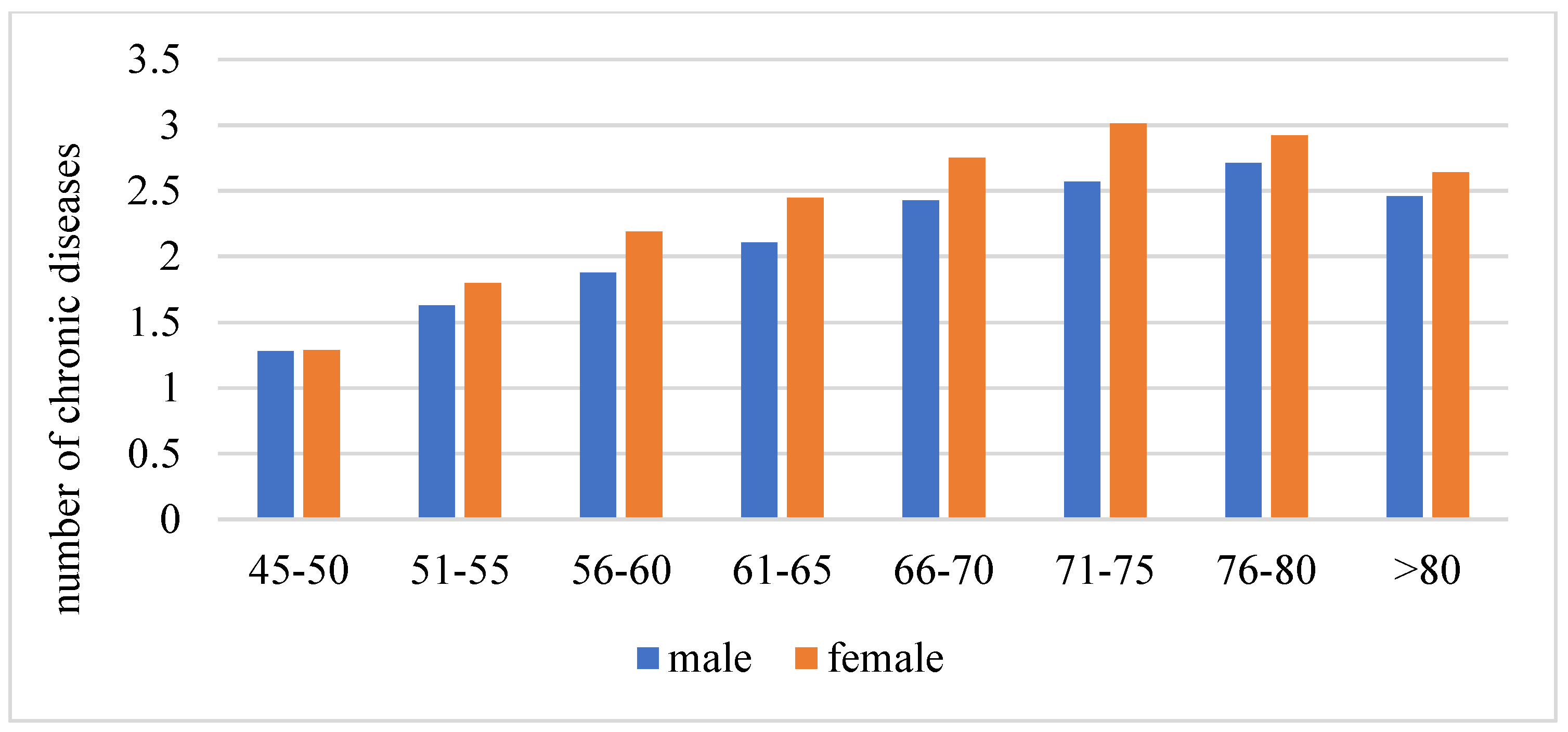
3.2. Gender Differences in Multimorbidity
3.3. Multimorbidity Patterns
3.4. Gender and Socioeconomic Differences in the Patterns of Multimorbidity
4. Discussion
5. Implications
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, Q.; Han, X.; Zhao, X.; Wang, Y. Multimorbidity patterns and associated factors in older Chinese: Results from the China health and retirement longitudinal study. BMC Geriatr. 2022, 22, 470. [Google Scholar] [CrossRef] [PubMed]
- Canever, J.B.; de Souza Moreira, B.; Danielewicz, A.L.; de Avelar, N.C.P. Are multimorbidity patterns associated with fear of falling in community-dwelling older adults? BMC Geriatr. 2022, 22, 192. [Google Scholar] [CrossRef] [PubMed]
- Akugizibwe, R.; Calderón-Larrañaga, A.; Roso-Llorach, A.; Onder, G.; Marengoni, A.; Zucchelli, A.; Rizzuto, D.; Vetrano, D.L. Multimorbidity Patterns and Unplanned Hospitalisation in a Cohort of Older Adults. J. Clin. Med. 2020, 9, 4001. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Mishra, G.D.; Jones, M. Evidence on multimorbidity from definition to intervention: An overview of systematic reviews. Ageing Res. Rev. 2017, 37, 53–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ioakeim-Skoufa, I.; Poblador-Plou, B.; Carmona-Pírez, J.; Díez-Manglano, J.; Navickas, R.; Gimeno-Feliu, L.A.; González-Rubio, F.; Jureviciene, E.; Dambrauskas, L.; Prados-Torres, A.; et al. Multimorbidity Patterns in the General Population: Results from the EpiChron Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 4242. [Google Scholar] [CrossRef] [PubMed]
- Asogwa, O.A.; Boateng, D.; Marzà-Florensa, A.; Peters, S.; Levitt, N.; van Olmen, J.; Klipstein-Grobusch, K. Multimorbidity of non-communicable diseases in low-income and middle-income countries: A systematic review and meta-analysis. BMJ Open 2022, 12, e49133. [Google Scholar] [CrossRef]
- Hu, X.; Huang, J.; Lv, Y.; Li, G.; Peng, X. Status of prevalence study on multimorbidity of chronic disease in China: Systematic review. Geriatr. Gerontol. Int. 2014, 15, 1–10. [Google Scholar] [CrossRef]
- Arokiasamy, P.; Uttamacharya, U.; Jain, K.; Biritwum, R.B.; Yawson, A.E.; Wu, F.; Guo, Y.; Maximova, T.; Espinoza, B.M.; Rodríguez, A.S.; et al. The impact of multimorbidity on adult physical and mental health in low- and middle-income countries: What does the study on global ageing and adult health (SAGE) reveal? BMC Med. 2015, 13, 178. [Google Scholar] [CrossRef] [Green Version]
- Garin, N.; Koyanagi, A.; Chatterji, S.; Tyrovolas, S.; Olaya, B.; Leonardi, M.; Lara, E.; Koskinen, S.; Tobiasz-Adamczyk, B.; Ayuso-Mateos, J.L.; et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J. Gerontol. Ser. A 2016, 71, 205–214. [Google Scholar] [CrossRef] [Green Version]
- Ahmadi, B.; Alimohammadian, M.; Yaseri, M.; Majidi, A.; Boreiri, M.; Islami, F.; Poustchi, H.; Derakhshan, M.H.; Feizesani, A.; Pourshams, A.; et al. Multimorbidity: Epidemiology and Risk Factors in the Golestan Cohort Study, Iran: A Cross-Sectional Analysis. Medicine 2016, 95, e2756. [Google Scholar] [CrossRef]
- Vancampfort, D.; Smith, L.; Stubbs, B.; Swinnen, N.; Firth, J.; Schuch, F.B.; Koyanagi, A. Associations between active travel and physical multi- morbidity in six low- and middle-income countries among community- dwelling older adults: A cross-sectional study. PLoS ONE 2018, 13, e203277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nunes, B.P.; Chiavegatto Filho, A.D.; Pati, S.; Teixeira, D.S.C.; Flores, T.R.; Camargo-Figuera, F.A.; Munhoz, T.N.; Thumé, E.; Facchini, L.A.; Batista, S.R.R. Contextual and individual inequalities of multimorbidity in Brazilian adults: A cross-sectional national- based study. BMJ Open 2017, 7, e15885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aye, S.K.; Hlaing, H.H.; Htay, S.S.; Cumming, R. Multimorbidity and health seeking behaviours among older people in Myanmar: A community survey. PLoS ONE 2019, 14, e219543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, J.; Wang, Y.; Hou, L.; Zuo, Z.; Zhang, N.; Wei, A. Multimorbidity patterns in old adults and their associated multi-layered factors: A cross-sectional study. BMC Geriatr. 2021, 21, 372. [Google Scholar] [CrossRef]
- Yao, S.S.; Cao, G.Y.; Han, L.; Chen, Z.S.; Huang, Z.T.; Gong, P.; Hu, Y.; Xu, B. Prevalence and Patterns of Multimorbidity in a Nationally Representative Sample of Older Chinese. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 1974–1980. [Google Scholar] [CrossRef]
- Abad-Díez, J.M.; Calderón-Larrañaga, A.; Poncel-Falcó, A.; Poblador-Plou, B.; Calderón-Meza, J.M.; Sicras-Mainar, A.; Clerencia-Sierra, M.; Prados-Torres, A. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014, 14, 75. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort Profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef] [Green Version]
- Lei, X.; Sun, X.; Strauss, J.; Zhang, P.; Zhao, Y. Depressive symptoms and SES among the mid-aged and elderly in China: Evidence from the China Health and Retirement Longitudinal Study national baseline. Soc. Sci. Med. 2014, 120, 224–232. [Google Scholar] [CrossRef] [Green Version]
- Lei, X.; Hu, Y.; McArdle, J.J.; Smith, J.P.; Zhao, Y. Gender Differences in Cognition among Older Adults in China. J. Hum. Resour. 2012, 47, 951–971. [Google Scholar]
- Zhang, C.; Xiao, S.; Shi, L.; Xue, Y.; Zheng, X.; Dong, F.; Zhang, J.; Xue, B.; Lin, H.; Ouyang, P. Urban–Rural Differences in Patterns and Associated Factors of Multimorbidity Among Older Adults in China: A Cross-Sectional Study Based on Apriori Algorithm and Multinomial Logistic Regression. Front. Public Health 2021, 9, 707062. [Google Scholar] [CrossRef]
- Li, L.W.; Liu, J.; Xu, H.; Zhang, Z. Understanding Rural-Urban Differences in Depressive Symptoms Among Older Adults in China. J. Aging Health 2016, 28, 341–362. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Eggleston, K.; Hanson, K.; Wu, M. Enhancing financial protection under China’s social health insurance to achieve universal health coverage. BMJ 2019, 365, l2378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, S.; Wang, S.; Feng, X.L. Multimorbidity, depressive symptoms and disability in activities of daily living amongst middle aged and older Chinese: Evidence from the China Health and Retirement Longitudinal Study. J. Affect. Disord. 2021, 295, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Olaya, B.; Moneta, M.V.; Caballero, F.F.; Tyrovolas, S.; Bayes, I.; Ayuso-Mateos, J.L.; Haro, J.M. Latent class analysis of multimorbidity patterns and associated outcomes in Spanish older adults: A prospective cohort study. BMC Geriatr. 2017, 17, 186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sinha, A.; Kerketta, S.; Ghosal, S.; Kanungo, S.; Pati, S. Multimorbidity Among Urban Poor in India: Findings From LASI, Wave-1. Front. Public Health 2022, 10, 881967. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Patel, S.A.; Biswas, S.; Shivashankar, R.; Kondal, D.; Ajay, V.S.; Anjana, R.M.; Fatmi, Z.; Ali, M.; Kadir, M.M.; et al. Multimorbidity in South Asian adults: Prevalence, risk factors and mortality. J. Public Health 2019, 41, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Guisado-Clavero, M.; Roso-Llorach, A.; López-Jimenez, T.; Pons-Vigués, M.; Foguet-Boreu, Q.; Muñoz, M.A.; Violán, C. Multimorbidity patterns in the elderly: A prospective cohort study with cluster analysis. BMC Geriatr. 2018, 18, 16. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Yao, S.; Wang, M.; Cao, G.; Chen, Z.; Huang, Z.; Wu, Y.; Han, L.; Xu, B.; Hu, Y. Multimorbidity among Two Million Adults in China. Int. J. Environ. Res. Public Health 2020, 17, 3395. [Google Scholar] [CrossRef]
- Reddy, M.M.; Zaman, K.; Yadav, R.; Yadav, P.; Kumar, K.; Kant, R. Prevalence, Associated Factors, and Health Expenditures of Noncommunicable Disease Multimorbidity-Findings From Gorakhpur Health and Demographic Surveillance System. Front. Public Health 2022, 10, 842561. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 10204, 1145–1158. [Google Scholar] [CrossRef] [Green Version]
- Park, B.; Lee, H.A.; Park, H. Use of latent class analysis to identify multimorbidity patterns and associated factors in Korean adults aged 50 years and older. PLoS ONE 2019, 14, e216259. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, X.; Yang, J.; Ma, L.; Chen, Y. The prevalence of osteoarthritis in Chinese aged 40 and over: A meta-analysis. Chin. J. Evid.-Based Med. 2021, 21, 407–414. [Google Scholar]
- Nguyen, H.; Chua, K.-C.; Dregan, A.; Vitoratou, S.; Bayes-Marin, I.; Olaya, B.; Prina, A.M. Factors Associated With Multimorbidity Patterns in Older Adults in England: Findings From the English Longitudinal Study of Aging (ELSA). J. Aging Health 2020, 32, 1120–1132. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; He, Y.; Xu, J. Urban-rural disparity in prevalence of multimorbidity in China: A cross sectional nationally representative study. BMJ Open 2020, 10, e38404. [Google Scholar] [CrossRef]
- Sinha, A.; Kerketta, S.; Ghosal, S.; Kanungo, S.; Lee, J.T.; Pati, S. Multimorbidity and Complex Multimorbidity in India: Findings from the 2017–2018 Longitudinal Ageing Study in India (LASI). Int. J. Environ. Res. Public Health 2022, 19, 9091. [Google Scholar] [CrossRef]
- Yi, J.Y.; Kim, H.; Chi, I. Urban-rural differences in multimorbidity and associated factors in China and Korea: A population-based survey study. Geriatr. Gerontol. Int. 2019, 19, 1157–1164. [Google Scholar] [CrossRef]
- Liu, Y.; Jiang, D. Multimorbidity Patterns in US Adults with Subjective Cognitive Decline and Their Relationship with Functional Difficulties. J. Aging Health 2022, 34. [Google Scholar] [CrossRef]

| Variables | Total (%) | Mean Number of Chronic Diseases (SD) | p Value | Proportion with Multimorbidity | p Value |
|---|---|---|---|---|---|
| All participants | 19,559 (100%) | 2.17 (1.88) | 56.73% | ||
| Gender | |||||
| Male | 9307 (47.58%) | 2.08 (1.84) | <0.001 | 54.65% | <0.001 |
| Female | 10,252 (52.42%) | 2.26 (1.92) | 58.71% | ||
| Marriage status | |||||
| Married | 16,619 (84.97%) | 2.09 (1.84) | <0.001 | 55.20% | <0.001 |
| Windowed | 2512 (12.84%) | 2.62 (2.01) | 66.58% | ||
| Others | 428 (2.19%) | 2.31 (2.20) | 53.37% | ||
| Education | |||||
| Sishu/home school and below | 8537 (43.65%) | 2.32 (1.93) | <0.001 | 60.49% | <0.001 |
| Elementary school | 4289 (21.93%) | 2.14 (1.87) | 54.99% | ||
| Middle school | 4258 (21.77%) | 2.01 (1.81) | 53.37% | ||
| High school and above | 2475 (12.65%) | 2.06 (1.85) | 54.18% | ||
| Residence | |||||
| Rural | 11,675 (59.69%) | 2.15 (1.87) | 0.16 | 56.21% | 0.184 |
| Urban | 7884 (40.31%) | 2.19 (1.90) | 57.26% | ||
| Alcohol consumption | |||||
| Never | 12,899 (65.95%) | 2.33 (1.95) | <0.001 | 60.44% | <0.001 |
| Occasionally | 1466 (7.50%) | 1.99 (1.81) | 50.83% | ||
| Usually | 5111 (26.13%) | 1.88 (1.69) | 50.66% | ||
| Smoking status | |||||
| Never | 11,211 (57.32%) | 2.18 (1.88) | <0.001 | 56.93% | <0.001 |
| Quit | 445 (2.28%) | 2.69 (2.04) | 67.11% | ||
| Current | 7825 (40.01%) | 2.16 (1.88) | 56.55% | ||
| Difficulty in ADL | |||||
| Yes | 3615 (18.48%) | 3.40 (2.10) | <0.001 | 81.72% | <0.001 |
| No | 15,944 (81.52%) | 1.90 (1.72) | 51.25% | ||
| Self-rated health | |||||
| Less than good | 15,066 (77.03%) | 2.48 (1.93) | <0.001 | 64.43% | <0.001 |
| Good | 4493 (22.97%) | 1.17 (1.30) | 31.83% | ||
| Health insurance | |||||
| None | 583 (2.98%) | 1.91 (1.83) | <0.001 | 48.96% | <0.001 |
| UEBMI | 2975 (15.21%) | 2.32 (1.97) | 60.63% | ||
| URBMI | 3189 (16.30%) | 2.18 (1.97) | 55.72% | ||
| NRCMS | 12,598 (64.41%) | 2.11 (1.87) | 56.20% | ||
| Others | 214 (1.09%) | 1.91 (2.02) | 49.79% |
| Variables | Relatively Health Class | Respiratory Class | Stomach-Arthritis Class | Vascular Class | |||
|---|---|---|---|---|---|---|---|
| RRR | RRR | 95%CI | RRR | 95%CI | RRR | 95%CI | |
| Gender (ref = Male) | |||||||
| Female | 1.00 | 0.795 | 0.501–1.261 | 1.595 *** | 1.276–1.993 | 0.953 | 0.745–1.220 |
| Age | 1.00 | 1.038 *** | 1.026–1.050 | 1.030 *** | 1.023–1.038 | 1.033 *** | 1.027–1.041 |
| Marriage status (ref = Married) | |||||||
| Windowed | 1.00 | 0.946 | 0.733–1.220 | 0.966 | 0.798–1.170 | 0.921 | 0.778–1.090 |
| Others | 1.00 | 1.675 ** | 1.086–2.584 | 1.660 ** | 1.139–2.418 | 0.728 | 0.487–1.090 |
| Education (ref = Sishu/home school and below) | |||||||
| Elementary school | 1.00 | 0.961 | 0.727–1.271 | 0.997 | 0.845–1.176 | 1.130 | 0.973–1.313 |
| Middle school | 1.00 | 0.958 | 0.667–1.376 | 0.869 | 0.712–1.061 | 1.363 *** | 1.148–1.619 |
| High school and above | 1.00 | 0.627 | 0.403–0.977 | 1.103 | 0.834–1.459 | 1.401 *** | 1.162–1.690 |
| Residence (ref = Rural) | |||||||
| Urban | 1.00 | 1.162 | 0.885–1.526 | 0.897 | 0.776–1.038 | 1.438 *** | 1.236–1.672 |
| In PCE | 1.00 | 1.001 | 0.915–1.096 | 1.095 ** | 1.026–1.168 | 1.114 *** | 1.053–1.179 |
| Alcohol consumption (ref = Never) | |||||||
| Occasionally | 1.00 | 0.604 ** | 0.438–0.832 | 0.793 * | 0.612–1.027 | 0.781 * | 0.613–0.995 |
| Usually | 1.00 | 0.779 * | 0.597–1.017 | 0.794 ** | 0.650–0.970 | 0.894 | 0.747–1.070 |
| Smoking status (ref = Never) | |||||||
| Quit | 1.00 | 1.120 | 0.599–2.090 | 1.581 * | 0.996–2.509 | 1.053 | 0.672–1.649 |
| Current | 1.00 | 1.354 | 0.854–2.145 | 1.458 ** | 1.176–1.808 | 0.933 | 0.715–1.219 |
| Difficulty in ADL (ref = No) | |||||||
| Yes | 1.00 | 2.148 *** | 1.783–2.587 | 3.248 *** | 2.819–3.743 | 1.986 *** | 1.739–2.269 |
| Self-rated health (ref = Less than good) | |||||||
| Good | 1.00 | 0.387 *** | 0.249–0.603 | 0.175 *** | 0.136–0.224 | 0.351 *** | 0.297–0.415 |
| Health insurance (ref = None) | |||||||
| UEBMI | 1.00 | 1.411 | 0.836–2.380 | 2.260 *** | 1.456–3.506 | 3.200 *** | 2.148–4.768 |
| URBMI | 1.00 | 1.259 | 0.774–2.047 | 1.704 ** | 1.134–2.561 | 2.353 *** | 1.608–3.443 |
| NRCMS | 1.00 | 1.550 * | 0.986–2.438 | 1.327 | 0.905–1.946 | 2.021 *** | 1.403–2.912 |
| Others | 1.00 | 1.339 | 0.586–3.057 | 1.145 | 0.562–2.332 | 2.385 ** | 1.198–4.748 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhong, Y.; Xi, H.; Guo, X.; Wang, T.; Wang, Y.; Wang, J. Gender and Socioeconomic Differences in the Prevalence and Patterns of Multimorbidity among Middle-Aged and Older Adults in China. Int. J. Environ. Res. Public Health 2022, 19, 16956. https://doi.org/10.3390/ijerph192416956
Zhong Y, Xi H, Guo X, Wang T, Wang Y, Wang J. Gender and Socioeconomic Differences in the Prevalence and Patterns of Multimorbidity among Middle-Aged and Older Adults in China. International Journal of Environmental Research and Public Health. 2022; 19(24):16956. https://doi.org/10.3390/ijerph192416956
Chicago/Turabian StyleZhong, Yaqin, Hanqing Xi, Xiaojun Guo, Tiantian Wang, Yanan Wang, and Jian Wang. 2022. "Gender and Socioeconomic Differences in the Prevalence and Patterns of Multimorbidity among Middle-Aged and Older Adults in China" International Journal of Environmental Research and Public Health 19, no. 24: 16956. https://doi.org/10.3390/ijerph192416956





