Assessing COVID-19-Related Excess Mortality Using Multiple Approaches—Italy, 2020–2021
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Choice of the Models and Description of the Three Models
2.3. Cross-Validation Analysis
3. Results
3.1. Excess Mortality Estimates
- Supplementary Table S1a. Excess mortality estimates using different models according to region for the year 2020. The 95% confidence intervals are included for the three models.
- Supplementary Table S1b. Excess mortality estimates using different models according to region for the year 2021. The 95% confidence intervals are included for the three models.
- Supplementary Table S1c. Relative excess mortality estimates using different models according to region for the year 2020.
- Supplementary Table S1d. Relative excess mortality estimates using different models according to region for the year 2021.
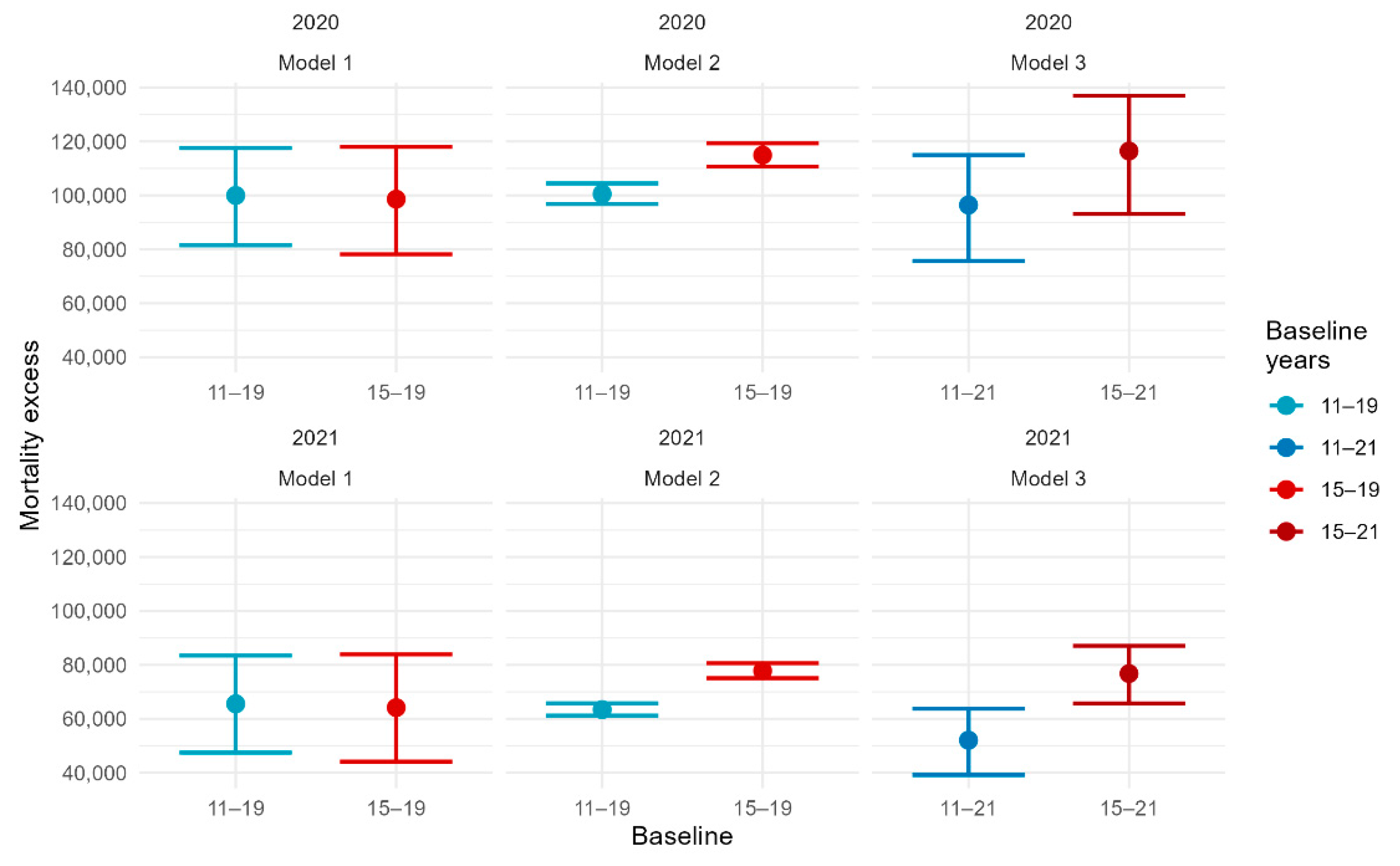
3.2. Change of Baseline and CROSS-Validation Analysis
4. Discussion
4.1. Findings
4.2. Research Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Weekly Epidemiological Update on COVID-19. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19 (accessed on 26 October 2022).
- Acosta, R.J.; Irizarry, R.A. A Flexible Statistical Framework for Estimating Excess Mortality. Epidemiology 2022, 33, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Excess Deaths Associated with COVID-19. CDC, National Center for Health Statistics. Available online: https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm (accessed on 1 October 2022).
- Michelozzi, P.; de’Donato, F.; Scortichini, M.; Pezzotti, P.; Stafoggia, M.; de Sario, M.; Costa, G.; Noccioli, F.; Riccardo, F.; Bella, A.; et al. Temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Public Health 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Nucci, L.B.; Enes, C.C.; Ferraz, F.R.; da Silva, I.V.; Rinaldi, A.E.; Conde, W.L. Excess mortality associated with COVID-19 in Brazil: 2020–2021. J. Public Health 2021. [Google Scholar] [CrossRef]
- ISTAT-ISS, SETTIMO RAPPORTO: Impatto Dell’epidemia COVID-19 Sulla Mortalità Totale Della Popolazione Residente. 2021. Available online: https://www.istat.it/it/files//2022/03/Report_ISS_ISTAT_2022_tab3.pdf (accessed on 1 September 2022).
- León-Gómez, I.; Mazagatos, C.; Delgado-Sanz, C.; Frías, L.; Vega-Piris, L.; Rojas-Benedicto, A.; Larrauri, A. The impact of COVID-19 on mortality in Spain: Monitoring excess mortality (MoMo) and the surveillance of confirmed COVID-19 deaths. Viruses 2021, 13, 2423. [Google Scholar] [CrossRef] [PubMed]
- Scortichini, M.; Santos, R.S.d.; Donato, F.d.; de Sario, M.; Michelozzi, P.; Davoli, M.; Masselot, P.; Sera, F.; Gasparrini, A. Excess mortality during the COVID-19 outbreak in Italy: A two-stage interrupted time-series analysis. Int. J. Epidemiol. 2020, 49, 1909–1917. [Google Scholar] [CrossRef] [PubMed]
- Rossen, L.M.; Norgard, S.K.; Sutton, P.D.; Krause, T.G.; Ahmad, F.B.; Vestergaard, L.S.; Molbak, K.; Anderson, R.N.; Nielsen, J. Excess all-cause mortality in the USA and Europe during the COVID-19 pandemic, 2020 and 2021. Sci. Rep. 2022, 12, 18559. [Google Scholar] [CrossRef] [PubMed]
- Rossen, L.M.; Branum, A.M.; Ahmad, F.B.; Sutton, P.D.; Anderson, R.N. Notes from the Field: Update on Excess Deaths Associated with the COVID-19 Pandemic—United States, 26 January 2020–27 February 2021. MMWR Morb. Mortal Wkly. Rep. 2021 70, 570–571. [CrossRef]
- Nørgaard, S.K.; Vestergaard, L.S.; Nielsen, J.; Richter, L.; Schmid, D.; Bustos, N.; Braye, T.; Athanasiadou, M.; Lytras, T.; Denissov, G.; et al. Real-time monitoring shows substantial excess all-cause mortality during second wave of COVID-19 in Europe, October to December 2020. Eurosurveillance 2021, 26, 2002023. [Google Scholar] [CrossRef]
- Vestergaard, L.S.; Nielsen, J.; Richter, L.; Schmid, D.; Bustos, N.; Braeye, T.; Denissov, G.; Veideman, T.; Luomala, O.; Möttönen, T.; et al. Excess all-cause mortality during the COVID-19 pandemic in Europe–preliminary pooled estimates from the EuroMOMO network, March to April 2020. Eurosurveillance 2020, 25, 2001214. [Google Scholar] [CrossRef]
- Biggeri, A.; Lagazio, C.; Catelan, D.; Barbone, F.; Braga, M. A municipality-level analysis of excess mortality in Italy in the period January-April 2020. Epidemiol. E Prev. 2020, 44 (Suppl. S2), 297–306. [Google Scholar]
- Blangiardo, M.; Cameletti, M.; Pirani, M.; Corsetti, G.; Battaglini, M.; Baio, G. Estimating weekly excess mortality at sub-national level in Italy during the COVID-19 pandemic. PLOS ONE 2020, 15, e0240286. [Google Scholar] [CrossRef]
- Haklai, Z.; Aburbeh, M.; Goldberg, N.; Gordon, E.-S. Excess mortality during the COVID-19 pandemic in Israel, March–November 2020: When, where, and for whom? Isr. J. Health Policy Res. 2021, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Woolf, S.H.; Chapman, D.A.; Sabo, R.T.; Zimmerman, E.B. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA 2021, 325, 1786–1789. [Google Scholar] [CrossRef]
- Bilinsky, A.; Emanuel, E.J. COVID-19 and Excess All-Cause Mortality in the US and 18 Comparison Countries. JAMA 2020, 324, 2100–2102. [Google Scholar] [CrossRef] [PubMed]
- Islam, N.; Shkolnikov, V.M.; Acosta, R.J.; Klimkin, I.; Kawachi, I.; Irizarry, R.A.; Alicandro, G.; Khunti, K.; Yates, T.; Jdanov, D.A.; et al. Excess deaths associated with covid-19 pandemic in 2020: Age and sex disaggregated time series analysis in 29 high income countries. BMJ 2021, 373, n1137. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Excess Deaths Associated with COVID-19. January 2020–December 2021. 2022. Available online: https://www.who.int/data/stories/global-excess-deaths-associated-with-covid-19-january-2020-december-2021 (accessed on 12 October 2022).
- Gianicolo, E.A.L.; Russo, A.; Buchler, B.; Taylor, K.; Stang, A.; Blettner, M. Gender specific excess mortality in Italy during the COVID-19 pandemic accounting for age. Eur. J. Epidemiology 2021, 36, 213–218. [Google Scholar] [CrossRef]
- Magnani, C.; Azzolina, D.; Gallo, E.; Ferrante, D.; Gregori, D. How large was the mortality increase directly and indirectly caused by the COVID-19 epidemic? An analysis on all-causes mortality data in Italy. Int. J. Environ. Res. Public Health 2020, 17, 3452. [Google Scholar] [CrossRef]
- Alicandro, G.; Remuzzi, G.; La Vecchia, C. COVID-19 pandemic and total mortality in the first six months of 2020 in Italy. Med. Lav. 2020, 111, 351. [Google Scholar]
- Barnard, S.; Chiavenna, C.; Fox, S.; Charlett, A.; Waller, Z.; Andrews, N.; Goldblatt, P.; Burton, P.; de Angelis, D. Methods for modelling excess mortality across England during the COVID-19 pandemic. Stat. Methods Med Res. 2022, 31, 1790–1802. [Google Scholar] [CrossRef]
- Maruotti, A.; Jona-Lasinio, G.; Divino, F.; Lovison, G.; Ciccozzi, M.; Farcomeni, A. Estimating COVID-19-induced excess mortality in Lombardy, Italy. Aging Clin. Exp. Res. 2022, 34, 475–479. [Google Scholar] [CrossRef]
- Dorrucci, M.; Minelli, G.; Boros, S.; Manno, V.; Prati, S.; Battaglini, M.; Corsetti, G.; Andrianou, X.; Riccardo, F.; Fabiani, M.; et al. Excess mortality in Italy during the COVID-19 pandemic: Assessing the differences between the first and the second wave, year 2020. Front. Public Heal. 2021, 9, 927. [Google Scholar] [CrossRef] [PubMed]
- Wedderburn, R. Quasi-likelihood functions, generalized linear models, and the Gauss—Newton method. Biometrika 1974, 61, 439–447. [Google Scholar]
- Aron, J.; Giattino, C.; Ritchie, H. A Pandemic Primer On Excess Mortality Statistics and Their Comparability across Countries. Our World in Data. 2020. Available online: https://ourworldindata.org/covid-excess-mortality (accessed on 1 October 2022).
- Chai, T.; Draxler, R.R. Root mean square error (RMSE) or mean absolute error (MAE). Geosci. Model Dev. 2014, 7, 1525–1534. [Google Scholar] [CrossRef] [Green Version]
- Wang, H. Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020–21. Lancet 2022, 399, 1513–1536. [Google Scholar] [CrossRef]
- Adam, D. COVID’s true death toll: Much higher than official records. Nature 2022, 603, 562. [Google Scholar] [CrossRef] [PubMed]
- Konstantinoudis, G.; Cameletti, M.; Gómez-Rubio, V.; Gómez, I.L.; Pirani, M.; Baio, G.; Larrauri, A.; Riou, J.; Egger, M.; Vineis e, M. Blangiardo, P. Regional excess mortality during the 2020. Nat. Commun. 2022, 13, 482. [Google Scholar] [CrossRef] [PubMed]
- Sacco, C.; del Manso, M.; Mateo-Urdiales, A.; Rota, M.C.; Petrone, D.; Riccardo, F.; Bella, A.; Siddu, A.; Battilomo, S.; Proietti, V.; et al. Effectiveness of BNT162b2 vaccine against SARS-CoV-2 infection and severe COVID-19 in children aged 5–11 years in Italy: A retrospective analysis of January–April 2022. Lancet 2022, 400, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Marziano, V.; Guzzetta, G.; Mammone, A.; Riccardo, F.; Poletti, P.; Trentini, F.; Manica, M.; Siddu, A.; Bella, A.; Stefanelli, P.; et al. The effect of COVID-19 vaccination in Italy and perspectives for living with the virus. Nat. Commun. 2021, 12, 1–8. [Google Scholar] [CrossRef]
- Riccardo, F.; Friscale, E.M.; Guzzetta, G.; Ferraro, F.; Merler, S.; Maringhini, G.; Spuri, M.; Petrone, D.; Rota, M.C.; Rapiti, A.; et al. Winning during a pandemic: Epidemiology of SARS-CoV-2 during EURO2020 in Italy. Epidemiol. Infect. 2022, e166, 1–7. [Google Scholar] [CrossRef]
- Task Force COVID-19 del Dipartimento Malattie Infettive e Servizio di Informatica, Istituto Superiore di Sanità. 21 Settembre 2022. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_21-settembre-2022.pdf (accessed on 4 November 2022).
- Nobre, J.S.; Singer, J.d.M. Residual analysis for linear mixed models. Biom. J. J. Math. Methods Biosci. 2007, 49, 863–875. [Google Scholar]
- Eurostat, Excess Mortality by Month. 2022. Available online: https://ec.europa.eu/eurostat/databrowser/view/demo_mexrt/default/table?lang=en (accessed on 15 November 2022).
- Kepp, K.P.; Björk, J.; Kontis, V.; Parks, R.M.; Bæk, K.T.; Emilsson, L.; Lallukka, T. Estimates of excess mortality for the five Nordic countries during the COVID-19 pandemic 2020–2021. medRxiv 2022. [Google Scholar] [CrossRef] [PubMed]
- Economist, T. Tracking COVID-19 Excess Deaths across Countries. Available online: https://www.economist.com/graphic-detail/coronavirus-excess-deaths-tracker (accessed on 30 October 2022).
- Levitt, M.; Zonta, F.; Ioannidis, J.P. Comparison of pandemic excess mortality in 2020–2021 across different empirical calculations. medRxiv 2022. [Google Scholar] [CrossRef] [PubMed]
- WHO. Methods for Estimating the Excess Mortality Associated with the COVID-19 Pandemic. 29 March 2022. Available online: https://www.who.int/publications/m/item/methods-for-estimating-the-excess-mortality-associatedwith-the-covid-19-pandemic (accessed on 30 October 2022).
- Biggeri, A.; Saltelli, A. The Strange Numbers of COVID-19. Argumenta 7 2021, 1, 97–107. [Google Scholar]

| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Models compared (reference) | (Generalized mixed effects models; Maruotti A, et al.). | (Generalized additive models; Dorrucci M, et al.). | (Time-series with temperatures distributions; Scortichini M, et al.). |
| Statistical model/approach | Negative binomial mixed model with seasonal patterns. | Negative binomial model/epidemiological approach. | Quasi-Poisson time-series regression model/time-series. |
| Type of time modelling and time unit | Time (weeks) modelled by Fourier series; number of terms chosen by goodness of fit criteria (AIC; BIC). | Time (weeks) modelled by quadratic splines, with one knot per month. | A linear term corresponding to time to model long-term trends, a cyclic cubic B-spline with three equally spaced knots for the day of the year used to model seasonality, and indicators for day of the week to account for weekly variations in mortality. |
| Estimate of the number of expected deaths | Mortality baseline estimated over (2011–2019). The weekly predictions of mortality data for years 2020 and 2021 are based on the 2019 year-specific conditional best linear unbiased predictions of the generalized linear mixed model. | Mean number of deaths during pre-pandemic years (2015–19). | Smooth functions that define a baseline risk accounting for temporal trends and variation in temperature distribution. |
| Estimate of excess deaths | Difference from the estimated baseline along with 95% prediction intervals. If zero is included in the intervals, no difference from the expected number of deaths is hypothesized. | Difference in the number of deaths in 2020/21 adjusted by seasonality with the number of expected deaths. | The excess risk In mortality during the COVID-19 outbreak defined through a constrained quadratic B-spline with four equally spaced knots. |
| Strengths of the model | Simple interpretation and very good in-sample fitting performance are obtained for all Italian regions. | Simple interpretation. | Presence of covariates containing the information regarding mean temperatures. |
| Limitation of the model | Socio-demographic and hospital-related information may improve the accuracy of the estimates and may contribute to explaining heterogeneity across regions. No harvesting effect is considered. | No secular trend estimate. | Low number of cases prevents the full application of the two-stage modelling process in age groups <50 years old. |
| Part a | ||||
|---|---|---|---|---|
| ISTAT-ISS REPORT | Model 1 | Model 2 | Model 3 | |
| North Italy, 0–49 years | −552 | −149 (−679; 348) | −551 (−564, −539) | 195 (−152, 497) |
| North Italy; 50–64 years | 3164 | 3263 (2610; 3882) | 3157 (3072, 3252) | 4030 (3161, 4789) |
| North Italy; 65–79 years | 15,004 | 17447 (15,,519; 19,275) | 14920 (14,231, 15,653) | 21051 (18355, 23,322) |
| North Italy; 80+ years | 56,681 | 51,684 (42,501; 60,472) | 56,722 (54,362, 59,198) | 59,189 (51,678, 65,606) |
| Entire North Italy | 74,296 | 72,695 (63,722; 81,224) | 74,241 (71,273, 77,345) | 84,507 (73,298, 94,050) |
| Central Italy; 0–49 years | −431 | −64 (−371; 216) | −432 (−451, −411) | 78 (−102, 232) |
| Central Italy; 50–64 years | 392 | 369 (−16; 728) | 389 (381, 402) | 796 (375, 1168) |
| Central Italy; 65–79 years | 1375 | 2526 (1513; 3478) | 1381 (1339, 1411) | 3564 (2408, 4556) |
| Central Italy; 80+ years | 8566 | 7743 (3789; 11471) | 8574 (8272, 8888) | 9304 (6148, 12,059) |
| Entire Central Italy | 9903 | 10,769 (6480; 14786) | 9907 (9588, 10,245) | 13,727 (9017, 17,852) |
| South Italy and islands; 0–49 years | −671 | −16 (−468; 411) | −673 (−684, −655) | 201 (−112, 476) |
| South Italy and islands; 50–64 years | 1807 | 2027 (1480; 2544) | 1802 (1764, 1855) | 1933 (1162, 2599) |
| South Italy and islands; 65–79 years | 3731 | 4898 (3322; 6383) | 3739 (3624, 3866) | 6436 (4391, 8215) |
| South Italy and islands; 80+ years | 11,461 | 9260 (3239; 15,001) | 11,477 (10,968, 12,005) | 11,471 (6698, 15,701) |
| Entire South Italy and islands | 16,328 | 16,588 (10,068; 22,781) | 16349 (15,734, 16,995) | 20,065 (12,503, 26,896) |
| Entire Italy; 0–49 years | −1654 | −183 (−1296; 877) | −1650 (−1679, −1625) | 334 (−392, 969) |
| All of Italy; 50–64 years | 5363 | 5767 (4594; 6887) | 5362 (5227, 5502) | 6600 (4708, 8242) |
| All of Italy; 65–79 years | 20,110 | 25,033 (21,102; 28815) | 20,076 (19,300, 20,882) | 30,469 (24,724, 35,487) |
| All of Italy; 80+ years | 76,708 | 68,554 (50,239; 86,130) | 76,760 (73,682, 79,970) | 78,973 (63,764, 92,199) |
| All of Italy | 100,526 | 99,968 (81,474; 117,585) | 100,530 (96,805, 104,417) | 116,431 (93,146, 136,888) |
| part b | ||||
| ISTAT-ISS REPORT | Model 1 | Model 2 | Model 3 | |
| North Italy; 0–49 years | −694 | −253 (−778; 250) | −699 (−718, −665) | 321 (120, 502) |
| North Italy; 50–64 years | 1680 | 1870 (1232; 2501) | 1677 (1637, 1731) | 2687 (2230, 3102) |
| North Italy; 65–79 years | 3866 | 6683 (4808; 8546) | 3862 (3662, 4085) | 10,963 (9482, 12,278) |
| North Italy; 80+ years | 19,798 | 15,829 (6723; 24,651) | 19800 (18,991, 20649) | 20,982 (17,180, 24,455) |
| Entire North Italy | 24,649 | 24,523 (15,682; 33,273) | 24,654 (23,656, 25,702) | 35,056 (29,546, 40,214) |
| Central Italy; 0–49 years | −315 | 61 (−241; 344) | −313 (−332, −300) | 253 (128, 368) |
| Central Italy; 50–64 years | 895 | 913 (538; 1277) | 895 (876, 915) | 1482 (1247, 1701) |
| Central Italy; 65–79 years | 2030 | 3296 (2311; 4265) | 2030 (1969, 2091) | 4878 (4290, 5415) |
| Central Italy; 80+ years | 8766 | 8310 (4430; 12,107) | 8768 (8461, 9089) | 9072 (7520, 10,530) |
| Entire Central Italy | 11,377 | 12,742 (8586; 16,865) | 11,374 (11,001, 11,774) | 15,759 (13,471, 17,854) |
| South Italy and Islands; 0–49 years | −339 | 339 (−111; 770) | −338 (−348, −330) | 594 (412, 762) |
| South Italy and Islands; 50–64 years | 3227 | 3543 (3011; 4070) | 3227 (3148, 3304) | 3253 (2851, 3617) |
| South Italy and Islands; 65–79 years | 7443 | 8842 (7316; 10,349) | 7445 (7197, 7694) | 10444 (9458, 11,373) |
| South Italy and Islands; 80+ years | 17,059 | 15,335 (9389; 21,136) | 17,068 (16,341, 17,820) | 13,886 (11,543, 16,057) |
| Entire South Italy and Islands | 27,390 | 28,435 (22,064; 34,742) | 27,392 (26,379, 28,453) | 28,383 (24,698, 31,975) |
| All of Italy; 0–49 years | −1348 | 190 (−917; 1249) | −1345 (−1372, −1312) | 1069 (688, 1415) |
| All of Italy; 50–64 years | 5802 | 6432 (5283; 7573) | 5804 (5663, 5939) | 7282 (6368, 8140) |
| All of Italy; 65–79 years | 13,339 | 18,984 (15103; 22,819) | 13,340 (12,827, 13880) | 25,627 (22,907, 28,172) |
| All of Italy; 80+ years | 45,623 | 39,338 (21216; 57001) | 45619 (43,914, 47403) | 42,530 (35,147, 49,408) |
| All of Italy | 63,415 | 65,575 (47,496; 83,478) | 63421 (61,186, 65750) | 76,781 (65,696, 87,079) |
| part c | ||||
| ISTAT-ISS REPORT | Model 1 | Model 2 | Model 3 | |
| North Italy; 0–49 years | −6.67 | −1.91 | −6.66 | 2.59 |
| North Italy; 50–64 years | 13.97 | 14.58 | 13.94 | 18.5 |
| North Italy; 65–79 years | 19.9 | 24.12 | 19.79 | 30.36 |
| North Italy; 80+ years | 28.98 | 25.99 | 29 | 30.66 |
| Entire North Italy | 24.61 | 24.15 | 24.59 | 28.97 |
| Central Italy; 0–49 years | −11.73 | −1.95 | −11.75 | 2.46 |
| Central Italy; 50–64 years | 3.91 | 3.7 | 3.88 | 8.27 |
| Central Italy; 65–79 years | 4.28 | 8.22 | 4.3 | 11.91 |
| Central Italy; 80+ years | 9.98 | 9 | 9.99 | 10.93 |
| Entire Central Italy | 7.52 | 8.29 | 7.53 | 10.74 |
| South Italy and Islands; 0–49 years | −8.95 | −0.24 | −8.98 | 3.04 |
| South Italy and Islands; 50–64 years | 9.33 | 10.68 | 9.31 | 10.05 |
| South Italy and Islands; 65–79 years | 6.53 | 8.82 | 6.55 | 11.83 |
| South Italy and Islands; 80+ years | 8.95 | 7.16 | 8.96 | 8.95 |
| Entire South Italy and Islands | 7.7 | 7.88 | 7.71 | 9.63 |
| All of Italy; 0–49 years | −8.51 | −1.02 | −8.49 | 1.91 |
| All of Italy; 50–64 years | 10.31 | 11.25 | 10.3 | 12.99 |
| All of Italy; 65–79 years | 12.22 | 15.8 | 12.2 | 19.75 |
| All of Italy; 80+ years | 18.73 | 16.54 | 18.74 | 19.39 |
| All of Italy | 15.57 | 15.59 | 15.57 | 18.49 |
| part d | ||||
| ISTAT-ISS REPORT | Model 1 | Model 2 | Model 3 | |
| North Italy; 0–49 years | −8.39 | −3.24 | −8.45 | 4.42 |
| North Italy; 50–64 years | 7.42 | 8.35 | 7.4 | 12.42 |
| North Italy; 65–79 years | 5.13 | 9.24 | 5.12 | 16.05 |
| North Italy; 80+ years | 10.12 | 7.96 | 10.12 | 10.79 |
| Entire North Italy | 8.17 | 8.15 | 8.17 | 12.03 |
| Central Italy; 0–49 years | −8.58 | 1.86 | −8.51 | 8.14 |
| Central Italy; 50–64 years | 8.93 | 9.14 | 8.93 | 15.7 |
| Central Italy; 65–79 years | 6.32 | 10.72 | 6.32 | 16.67 |
| Central Italy; 80+ years | 10.21 | 9.66 | 10.21 | 10.61 |
| Entire Central Italy | 8.64 | 9.81 | 8.64 | 12.38 |
| South Italy and Islands; 0–49 years | −4.52 | 4.99 | −4.51 | 9.05 |
| South Italy and Islands; 50–64 years | 16.67 | 18.66 | 16.67 | 16.83 |
| South Italy and Islands; 65–79 years | 13.03 | 15.91 | 13.04 | 19.3 |
| South Italy and Islands; 80+ years | 13.31 | 11.85 | 13.32 | 10.58 |
| Entire South Italy and Islands | 12.91 | 13.52 | 12.92 | 13.45 |
| All of Italy; 0–49 years | −6.93 | 1.06 | −6.92 | 6.28 |
| All of Italy; 50–64 years | 11.15 | 12.55 | 11.15 | 14.4 |
| All of Italy; 65–79 years | 8.1 | 11.98 | 8.1 | 16.83 |
| All of Italy; 80+ years | 11.14 | 9.49 | 11.14 | 10.31 |
| All of Italy | 9.82 | 10.22 | 9.82 | 12.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceccarelli, E.; Dorrucci, M.; Minelli, G.; Jona Lasinio, G.; Prati, S.; Battaglini, M.; Corsetti, G.; Bella, A.; Boros, S.; Petrone, D.; et al. Assessing COVID-19-Related Excess Mortality Using Multiple Approaches—Italy, 2020–2021. Int. J. Environ. Res. Public Health 2022, 19, 16998. https://doi.org/10.3390/ijerph192416998
Ceccarelli E, Dorrucci M, Minelli G, Jona Lasinio G, Prati S, Battaglini M, Corsetti G, Bella A, Boros S, Petrone D, et al. Assessing COVID-19-Related Excess Mortality Using Multiple Approaches—Italy, 2020–2021. International Journal of Environmental Research and Public Health. 2022; 19(24):16998. https://doi.org/10.3390/ijerph192416998
Chicago/Turabian StyleCeccarelli, Emiliano, Maria Dorrucci, Giada Minelli, Giovanna Jona Lasinio, Sabrina Prati, Marco Battaglini, Gianni Corsetti, Antonino Bella, Stefano Boros, Daniele Petrone, and et al. 2022. "Assessing COVID-19-Related Excess Mortality Using Multiple Approaches—Italy, 2020–2021" International Journal of Environmental Research and Public Health 19, no. 24: 16998. https://doi.org/10.3390/ijerph192416998





