Challenges in Help-Seeking Behaviors among Rural Older People Mitigated through Family Physician-Driven Outreach: A Systematic Review
Abstract
1. Introduction
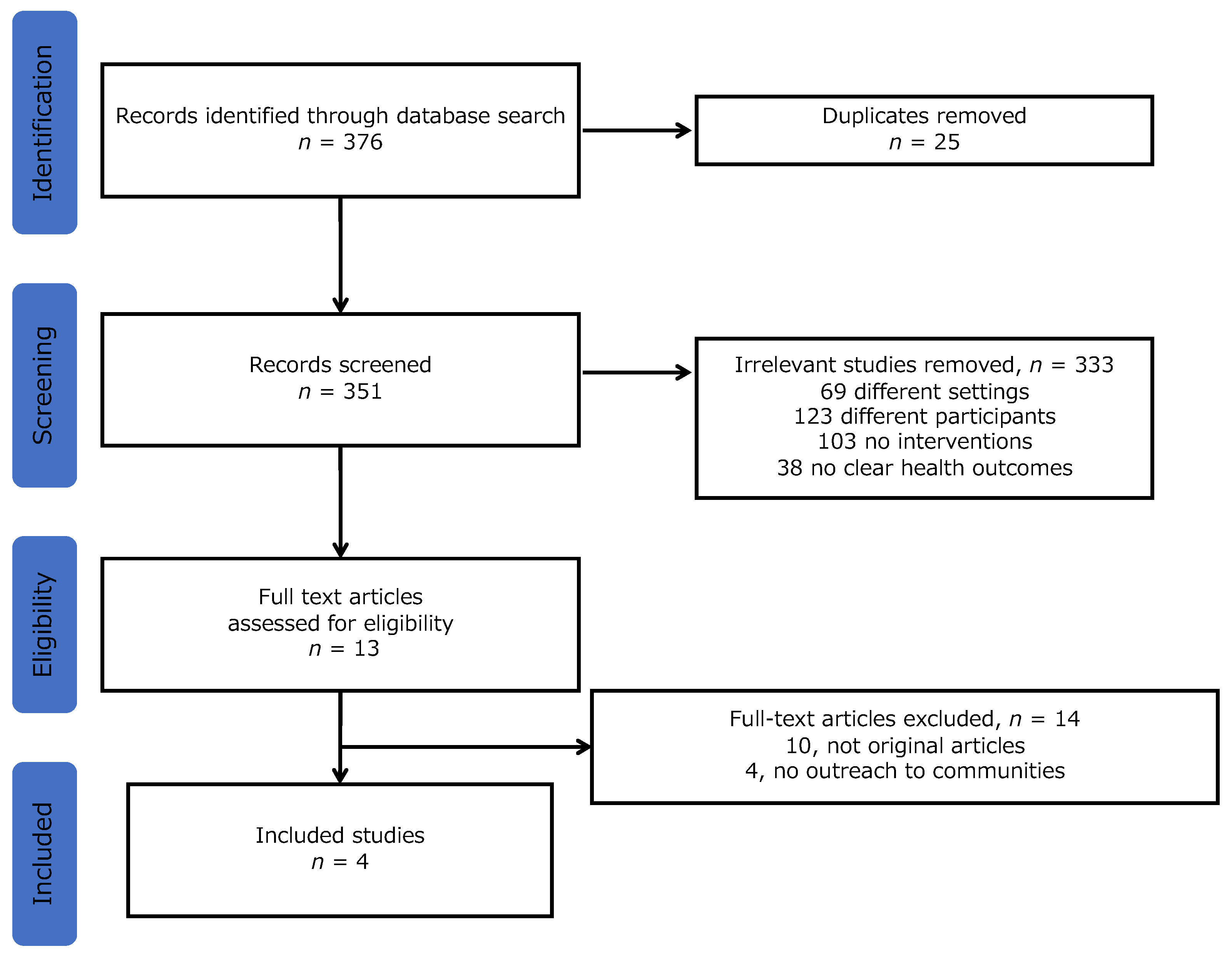
2. Materials and Methods
2.1. Study Selection
2.2. Data Extraction
2.3. Statistical Analysis
3. Results
3.1. Summary of the Study Results
3.2. Suggested limitations of the interventions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ohta, R.; Sato, M.; Ryu, Y.; Kitayuguchi, J.; Maeno, T.; Sano, C. What resources do elderly people choose for managing their symptoms? Clarification of rural older people’s choices of help-seeking behaviors in Japan. BMC Health Serv. Res. 2021, 21, 640. [Google Scholar] [CrossRef] [PubMed]
- Elliott, A.M.; McAteer, A.; Hannaford, P.C. Revisiting the symptom iceberg in today’s primary care: Results from a UK population survey. BMC Fam. Pract. 2011, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.I.C.; Khattignavong, P.; Keomalaphet, S.; Iwagami, M.; Brey, P.; Kano, S.; Jimba, M. Health-seeking behaviours in a malaria endemic district in Lao People’s Democratic Republic: A mixed methods study. BMJ Open 2021, 11, e055350. [Google Scholar] [CrossRef] [PubMed]
- Kerrigan, D.; West, N.; Tudor, C.; Hanrahan, C.F.; Lebina, L.; Msandiwa, R.; Mmolawa, L.; Martinson, N.; Dowdy, D. Improving active case finding for tuberculosis in South Africa: Informing innovative implementation approaches in the context of the Kharitode trial through formative research. Health Res. Policy Syst. 2017, 15, 42. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Sato, M.; Kitayuguchi, J.; Maeno, T.; Sano, C. The association between the self-management of mild symptoms and quality of life of elderly populations in rural communities: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 8857. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Sano, C. Association between self-medication for mild symptoms and quality of life among older adults in Rural Japan: A cross-sectional study. Medicina 2022, 58, 701. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Sano, C. Improvement in quality of life through self-management of mild symptoms during the COVID-19 pandemic: A prospective cohort study. Int. J. Environ. Res. Public Health 2022, 19, 6652. [Google Scholar] [CrossRef]
- Jiao, C.; Leng, A.; Nicholas, S.; Maitland, E.; Wang, J.; Zhao, Q.; Xu, L.; Gong, C. Multimorbidity and mental health: The role of gender among disease-causing poverty, rural, aged households in China. Int. J. Environ. Res. Public Health 2020, 17, 8855. [Google Scholar] [CrossRef]
- Zhao, Q.; Wang, J.; Nicholas, S.; Maitland, E.; Sun, J.; Jiao, C.; Xu, L.; Leng, A. Health-related quality of life and health service use among multimorbid middle-aged and older-aged adults in China: A cross-sectional study in Shandong Province. Int. J. Environ. Res. Public Health 2020, 17, 9261. [Google Scholar] [CrossRef]
- Hopman, P.; de Bruin, S.R.; Forjaz, M.J.; Rodriguez-Blazquez, C.; Tonnara, G.; Lemmens, L.C.; Onder, G.; Baan, C.A.; Rijken, M. Effectiveness of comprehensive care programs for patients with multiple chronic conditions or frailty: A systematic literature review. Health Policy 2016, 120, 818–832. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Sano, C. Older people’s help-seeking behaviors in rural contexts: A systematic review. Int. J. Environ. Res. Public Health 2022, 19, 3233. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.; Nguyen, T.; Tran, D.; Hinton, L. “It’s extremely hard but it’s not a burden”: A qualitative study of family caregiving for people living with dementia in Vietnam. PLoS ONE 2021, 16, e0259788. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Yoshida, T.; Yamada, Y.; Watanabe, Y.; Nanri, H.; Yokoyama, K.; Date, H.; Miyake, M.; Itoi, A.; Yamagata, E.; et al. Sociodemographic and physical predictors of non-participation in community based physical checkup among older neighbors: A case-control study from the Kyoto-Kameoka longitudinal study, Japan. BMC Public Health 2018, 18, 568. [Google Scholar] [CrossRef] [PubMed]
- Ogbolu, Y.; Scrandis, D.A.; Fitzpatrick, G. Barriers and facilitators of care for diverse patients: Nurse leader perspectives and nurse manager implications. J. Nurs. Manag. 2018, 26, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Ali, S.A. Exploratory study into awareness of heart disease and health care seeking behavior among Emirati women (UAE) — Cross sectional descriptive study. BMC Womens Health 2017, 17, 88. [Google Scholar] [CrossRef] [PubMed]
- Laake, J.P.; Vulkan, D.; Quaife, S.L.; Hamilton, W.T.; Martins, T.; Waller, J.; Parmar, D.; Sasieni, P.; Duffy, S.W. Targeted encouragement of GP consultations for possible cancer symptoms: A randomised controlled trial. Br. J. Gen. Pract. 2021, 71, e339–e346. [Google Scholar] [CrossRef] [PubMed]
- Stollenwerk, D.; Kennedy, L.B.; Hughes, L.S.; O’Connor, M. A systematic approach to understanding and implementing patient-centered care. Fam. Med. 2019, 51, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Hammick, M.; Dornan, T.; Steinert, Y. Conducting a best evidence systematic review. Part 1: From idea to data coding. BEME Guide No. 13. BEEE Guide No 13 Med. Teach. 2010, 32, 3–15. [Google Scholar] [CrossRef]
- Majumdar, S.R.; Guirguis, L.M.; Toth, E.L.; Lewanczuk, R.Z.; Lee, T.K.; Johnson, J.A. Controlled trial of a multifaceted intervention for improving quality of care for rural patients with type 2 diabetes. Diabetes Care 2003, 26, 3061–3066. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ploeg, J.; Brazil, K.; Hutchison, B.; Kaczorowski, J.; Dalby, D.M.; Goldsmith, C.H.; Furlong, W. Effect of preventive primary care outreach on health related quality of life among older adults at risk of functional decline: Randomised controlled trial. BMJ 2010, 340, c1480. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stanley, M.A.; Wilson, N.L.; Shrestha, S.; Amspoker, A.B.; Wagener, P.; Bavineau, J.; Turner, M.; Fletcher, T.L.; Freshour, J.; Kraus-Schuman, C.; et al. Community-based outreach and treatment for underserved older adults with clinically significant worry: A randomized controlled trial. Am. J. Geriatr. Psychiatry 2018, 26, 1147–1162. [Google Scholar] [CrossRef] [PubMed]
- Mielenz, T.J.; Tracy, M.; Jia, H.; Durbin, L.L.; Allegrante, J.P.; Arniella, G.; Sorensen, J.A. Creation of the person-centered wellness home in older adults. Innov. Aging 2020, 4, igz055. [Google Scholar] [CrossRef] [PubMed]
- Shiroiwa, T.; Fukuda, T.; Ikeda, S.; Igarashi, A.; Noto, S.; Saito, S.; Shimozuma, K. Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual. Life Res. 2016, 25, 707–719. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Sano, C. Associations between perception of help-seeking behaviors and quality of life among older people in rural communities: A cross-sectional study. Int. J. Environ. Res. Public Health 2022, 19, 13331. [Google Scholar] [CrossRef] [PubMed]
- Göktaş, O. The Goktas definition of family medicine/general practice. Aten. Primaria. 2022, 54, 102468. [Google Scholar] [CrossRef] [PubMed]
- Freeman, T.R. Principles of family medicine. In TR, in McWhinney’s Textbook of Family Medicine; Oxford Academic: New York, NY, USA, 2016. [Google Scholar]
- Mazloomymahmoodabad, S.; Masoudy, G.; Fallahzadeh, H.; Jalili, Z. Education based on precede-proceed on quality of life in elderly. Glob. J. Health Sci. 2014, 6, 178–184. [Google Scholar] [CrossRef] [PubMed]
- De Maeseneer, J.M.; De Prins, L.; Gosset, C.; Heyerick, J. Provider continuity in family medicine: Does it make a difference for total health care costs? Ann. Fam. Med. 2003, 1, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Tourigny, A.; Aubin, M.; Haggerty, J.; Bonin, L.; Morin, D.; Reinharz, D.; Leduc, Y.; St-Pierre, M.; Houle, N.; Giguère, A.; et al. Patients’ perceptions of the quality of care after primary care reform: Family medicine groups in Quebec. Can. Fam. Physician 2010, 56, e273–e282. [Google Scholar] [PubMed]
- Bazemore, A.; Petterson, S.; Peterson, L.E.; Bruno, R.; Chung, Y.; Phillips, R.L. Higher primary care physician continuity is associated with lower costs and hospitalizations. Ann. Fam. Med. 2018, 16, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Tammes, P.; Purdy, S.; Salisbury, C.; MacKichan, F.; Lasserson, D.; Morris, R.W. Continuity of primary care and emergency hospital admissions among older patients in England. Ann. Fam. Med. 2017, 15, 515–522. [Google Scholar] [CrossRef]
- Ventres, W.B. Looking within: Intentions of practice for person-centered care. Ann. Fam. Med. 2017, 15, 171–174. [Google Scholar] [CrossRef]
- Ocloo, J.; Matthews, R. From tokenism to empowerment: Progressing patient and public involvement in healthcare improvement. BMJ Qual. Saf. 2016, 25, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Barcham, R.; Silas, E.; Irie, J. Health promotion and empowerment in Henganofi District, Papua New Guinea. Rural Remote Health 2016, 16, 3553. [Google Scholar] [CrossRef]
- Kaneko, M.; Motomura, K.; Mori, H.; Ohta, R.; Matsuzawa, H.; Shimabukuro, A.; Matsushima, M. Gatekeeping function of primary care physicians under Japan’s free-access system: A prospective open cohort study involving 14 isolated islands. Fam. Pract. 2019, 36, 452–459. [Google Scholar] [CrossRef]
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Population | People > 60 to 65 years old | Other people |
| Setting | Rural or underserved community | Other settings |
| Types of study | Interventional study | Non-empirical studies (editorial, news, review, conference papers) |
| Interventions | Outreach including family physicians | Without outreach |
| Outcome | Health-related | Not health-related |
| Other | Abstract available Full text available in English | Abstract unavailable Full text unavailable in English |
| Year | Country | Purpose | Study Design | Participants | Health Issues | Interventions | Involved Professionals | Results |
|---|---|---|---|---|---|---|---|---|
| 2003 [20] | Canada | To assess the effectiveness of a multidisciplinary diabetes outreach service | Pre–post study | Patients living in rural communities | Diabetes control | 6-month interventions, home visiting educational message to patients | Family physicians Specialists Nurse educators Dieticians Pharmacists | The intervention was associated with a trend toward 10% improvement in blood pressure. |
| 2010 [21] | Canada | To evaluate the impact of a provider initiated primary care outreach intervention to functional decline. | Randomized controlled trial | Older people in communities | Functional decline | 12-month intervention comprehensive initial assessment collaborative care planning health promotion referral to community health and social support services. | Home care nurses Family physicians Patients Family | Changes in functional status and self-rated health did not significantly change. |
| 2018 [22] | USA | To determine the effectiveness of cognitive behavioral therapy to mental conditions | Randomized controlled trial | People in underserved communities | Worry and GAD-related symptom | 9-month intervention cognitive behavioral therapy with resource counseling, facilitation of communication with primary care providers about worry/anxiety, integration of religion/spirituality, person-centered skill content and delivery, and nontraditional community providers | General practitioners Healthcare providers Social worker Case manager | Moderate improvements on worry, GAD-related symptoms, anxiety, depression, sleep, trauma-related symptoms, and mental health QOL. |
| 2020 [23] | USA | To show the effectiveness of person-centered wellness home | Randomized controlled trial | People in underserved communities | Physical functions | 6-month intervention self-management resource center small group programs plus wellness coaching, as a booster intervention in older adults with chronic diseases. | Family physicians Therapists Community health worker | There was an improvement in self-reported physical functioning, not physical activity. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohta, R.; Katsube, T.; Sano, C. Challenges in Help-Seeking Behaviors among Rural Older People Mitigated through Family Physician-Driven Outreach: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 17004. https://doi.org/10.3390/ijerph192417004
Ohta R, Katsube T, Sano C. Challenges in Help-Seeking Behaviors among Rural Older People Mitigated through Family Physician-Driven Outreach: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(24):17004. https://doi.org/10.3390/ijerph192417004
Chicago/Turabian StyleOhta, Ryuichi, Takuji Katsube, and Chiaki Sano. 2022. "Challenges in Help-Seeking Behaviors among Rural Older People Mitigated through Family Physician-Driven Outreach: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 24: 17004. https://doi.org/10.3390/ijerph192417004
APA StyleOhta, R., Katsube, T., & Sano, C. (2022). Challenges in Help-Seeking Behaviors among Rural Older People Mitigated through Family Physician-Driven Outreach: A Systematic Review. International Journal of Environmental Research and Public Health, 19(24), 17004. https://doi.org/10.3390/ijerph192417004







