Responding to COVID-19: The Suitability of Primary Care Infrastructure in 33 Countries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sampling and Study Participants
2.3. Outcome Variables
2.4. Explanatory Variables
2.4.1. Practice Characteristics
2.4.2. Infection Control Infrastructure Equipment
2.4.3. Safeguarding the Well-Being of the Staff Members by the Practice
2.4.4. Adequate Government Support for the Proper Functioning of Practice
2.5. Statistical Analysis
2.6. Ethical Approval
3. Results
3.1. Practice Characteristics
3.1.1. Perceived Governmental Support
3.1.2. Safeguarding the Well-Being of the Staff Members by the Practice
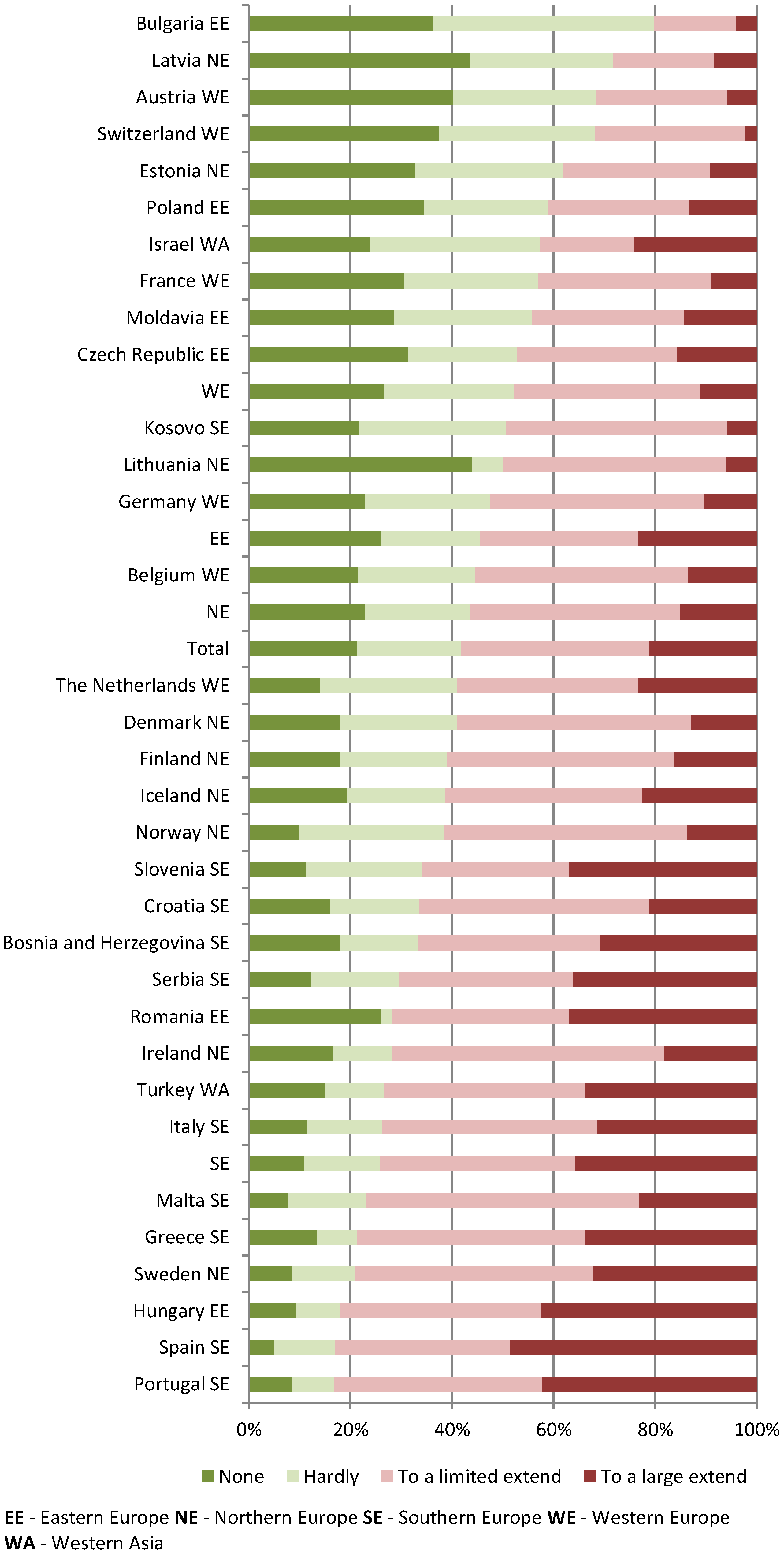
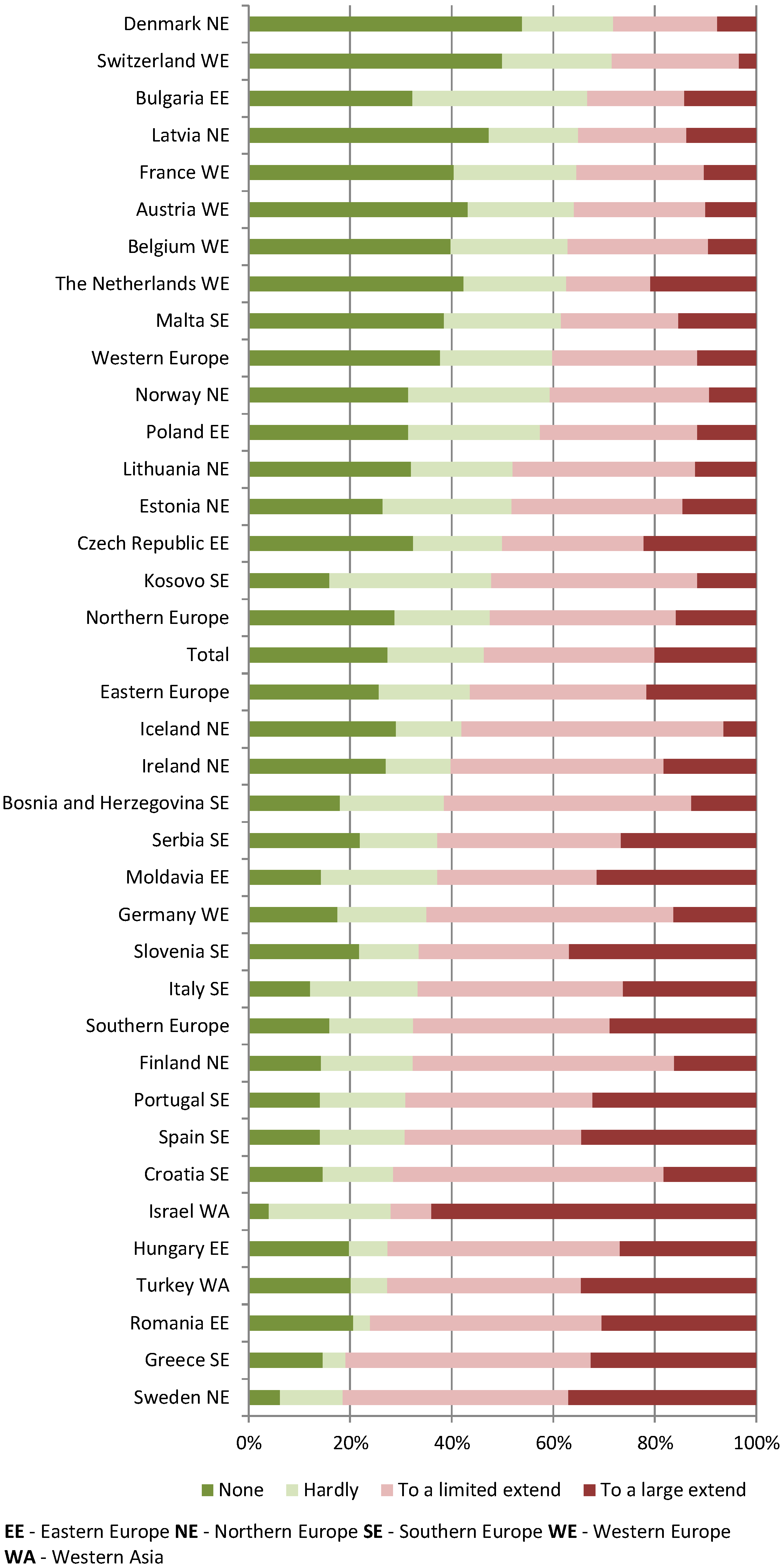
3.2. Perceived Limitations and Needs for Changes in Infrastructure
3.3. Correlation with Practice Characteristics
4. Discussion
4.1. Summary of Main Findings
4.2. Comparison with Existing Literature
4.3. Strengths and Limitations
4.4. Implications for Research, Policy, and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- L’Esperance, V.; Sutton, M.; Schofield, P.; Round, T.; Malik, U.; White, P.; Ashworth, M. Impact of primary care funding on secondary care utilisation and patient outcomes: A retrospective cross-sectional study of English general practice. Br. J. Gen. Pract. 2017, 67, e792–e799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dugani, S.; Veillard, J.; Evans, T.G. Quality primary health care will drive the realization of universal health coverage. CMAJ 2018, 190, E453–E454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Starfield, B.; Shi, L.; Macinko, J. Contribution of primary care to health systems and health. Milbank Q. 2005, 83, 457–502. [Google Scholar] [CrossRef] [PubMed]
- Jarman, B.; Gault, S.; Alves, B.; Hider, A.; Dolan, S.; Cook, A.; Hurwitz, B.; Iezzoni, L.I. Explaining differences in English hospital death rates using routinely collected data. BMJ 1999, 318, 1515–1520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gravelle, H.; Morris, S.; Sutton, M. Are family physicians good for you? Endogenous doctor supply and individual health. Health Serv. Res. 2008, 43, 1128–1144. [Google Scholar] [CrossRef] [Green Version]
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Hanson, K.; Brikci, N.; Erlangga, D.; Alebachew, A.; De Allegri, M.; Balabanova, D.; Blecher, M.; Cashin, C.; Esperato, A.; Hipgrave, D.; et al. The Lancet Global Health Commission on financing primary health care: Putting people at the centre. Lancet Glob. Health 2022, 10, e715–e772. [Google Scholar] [CrossRef]
- Stenberg, K.; Hanssen, O.; Bertram, M.; Brindley, C.; Meshreky, A.; Barkley, S.; Edejer, T.T.-T. Guide posts for investment in primary health care and projected resource needs in 67 low-income and middle-income countries: A modelling study. Lancet Glob. Health 2019, 7, e1500–e1510. [Google Scholar] [CrossRef] [Green Version]
- Global Preparedness Monitoring Board. A World at Risk: Annual Report on Global Preparedness for Health Emergencies; WHO: Geneva, Switzerland, 2019; Available online: https://www.gpmb.org/annual-reports/annual-report-2019 (accessed on 13 December 2022).
- Singer, S.J.; Glassman, J.; Glaseroff, A.; Joseph, G.A.; Jauregui, A.; Mulaney, B.; Kelly, S.S.; Thomas, S.; Vilendrer, S.; Tietschert, M.V. Impact of COVID-19 on Primary Care Practice Sites and Their Vulnerable Patients. Adv. Health Care Manag. 2021, 20, 233–271. [Google Scholar] [CrossRef]
- Yadav, P.; Vohra, C.; Gopalakrishnan, M.; Garg, M.K. Integrating health planning and primary care infrastructure for COVID-19 and tuberculosis care in India: Challenges and opportunities. Int. J. Health Plann Manag. 2022, 37, 632–642. [Google Scholar] [CrossRef]
- Liaw, S.T.; Kuziemsky, C.; Schreiber, R.; Jonnagaddala, J.; Liyanage, H.; Chittalia, A.; Bahniwal, R.; He, J.W.; Ryan, B.L.; Lizotte, D.J. Primary Care Informatics Response to COVID-19 Pandemic: Adaptation, Progress, and Lessons from Four Countries with High ICT Development. Yearb. Med. Inform. 2021, 30, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Duckett, S. What should primary care look like after the COVID-19 pandemic? Aust. J. Prim. Health 2020, 26, 207–211. [Google Scholar] [CrossRef]
- Snoswel, C.L.; Caffery, L.J.; Haydon, H.M.; Thomas, E.E.; Smith, A.C. Telehealth uptake in general practice as a result of the coronavirus (COVID-19) pandemic. Aust. Health Rev. 2020, 44, 737–740. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.; Sanders, C. A reflection on the impact of COVID-19 on primary care in the United Kingdom. J. Interprof. Care 2020, 34, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Tsopra, R.; Frappe, P.; Streit, S.; Neves, A.L.; Honkoop, P.J.; Espinosa-Gonzalez, A.B.; Geroğlu, B.; Jahr, T.; Lingner, H.; Nessler, K.; et al. Reorganisation of GP surgeries during the COVID-19 outbreak: Analysis of guidelines from 15 countries. BMC Fam. Pract. 2021, 22, 96. [Google Scholar] [CrossRef] [PubMed]
- Scholz, S.; Ngoli, B.; Flessa, S. Rapid assessment of infrastructure of primary health care facilities—A relevant instrument for health care systems management. BMC Health Serv. Res 2015, 15, 183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Poel, E.; Vanden Bussche, P.; Klemenc-Ketis, Z.; Willems, S. How did general practices organize care during the COVID-19 pandemic: The protocol of the cross-sectional PRICOV-19 study in 38 countries. BMC Prim. Care 2022, 23, 11. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. BiomedI. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Collins, C.; Van Poel, E.; Milićević, M.; Tripkovic, K.; Adler, L.; Eide, T.B.; Murauskiene, L.; Windak, A.; Nessler, K.; Tahirbegolli, B.; et al. Practice and System Factors Impact on Infection Prevention and Control in General Practice during COVID-19 across 33 Countries: Results of the PRICOV Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2022, 19, 7830. [Google Scholar] [CrossRef]
- Tanne, J.H.; Hayasaki, E.; Zastrow, M.; Pulla, P.; Smith, P.; Rada, A.G. COVID-19: How doctors and healthcare systems are tackling coronavirus worldwide. Br. Med. J. 2020, 368, m1090. [Google Scholar] [CrossRef]
- Krist, A.H.; DeVoe, J.E.; Cheng, A.; Ehrlich, T.; Jones, S.M. Redesigning primary care to address the COVID-19 pandemic in the midst of the pandemic. Ann. Fam. Med. 2020, 18, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Barber, S.; Lorenzoni, L.; Ong, P. Price Setting and Price Regulation in Health Care: Lessons for Advancing Universal Health Coverage. Geneva: World Health Organization, Organisation for Economic Co-operation and Development; 2019. Licence: CC BY-NC-SA 3.0 IGO. Available online: https://www.oecd.org/health/health-systems/oecd-who-price-setting-summary-report.pdf (accessed on 8 November 2022).
- Silva, B.; Ožvačić Adžić, Z.; Vanden Bussche, P.; Van Poel, E.; Seifert, B.; Heaster, C.; Collins, C.; Tuz Yilmaz, C.; Knights, F.; de la Cruz, G.; et al. Safety Culture and the Positive Association of being a Primary Care Training Practice during COVID-19: The Results of the Multi-Country European PRICOV-19 Study. Int. J. Environ. Res. Public Health 2022, 19, 10515. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.R.; Snell, L.; Sherbino, J. (Eds.) Can Meds 2015 Physician Competency Framework; Royal College of Physicians and Surgeons of Canada: Ottawa, ON, Canada, 2015; Available online: https://www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e (accessed on 8 November 2022).
- Key Messages: COVID-19 and Primary Health Care. Available online: https://improvingphc.org/key-messages-covid-19-and-primary-health-care (accessed on 8 November 2022).
- High-Level Event: The Role of Primary Health Care in the COVID-19 Pandemic Response and Leading Equitable Recovery. Available online: https://www.who.int/news-room/events/detail/2021/06/22/default-calendar/high-level-event-the-role-of-primary-health-care-in-the-covid-19-pandemic-response-and-leading-equitable-recovery (accessed on 8 November 2022).
- Brambilla, A.; Sun, T.Z.; Elshazly, W.; Ghazy, A.; Barach, P.; Lindahl, G.; Capolongo, S. Flexiblity during COVID-19 Pandemic Response: Healthcare Facility Assessment Tools for Resilient Evaluation. Int. J. Environ. Res. Public Health 2021, 18, 11478. [Google Scholar] [CrossRef] [PubMed]
- Lyng, H.B.; Macrae, C.; Guise, V.; Haraldseid-Driftland, C.; Fagerdal, B.; Schibevaag, L.; Alsvik, J.G.; Wiig, S. Balancing adaptation and innovation for resilience in healthcare—A metasynthesis of narratives. BMC Health Serv. Res. 2021, 21, 759. [Google Scholar] [CrossRef] [PubMed]

| Total | N 4974 | % 100 |
|---|---|---|
| Location of practice | ||
| Big (inner) city | 1613 | 32.4 |
| Suburbs | 514 | 10.3 |
| (Small) town | 923 | 18.6 |
| Mixed urban-rural | 1013 | 20.4 |
| Rural Missing value | 898 13 | 18.1 0.3 |
| Payment system | ||
| Capitation | 2002 | 40.9 |
| Fee-for-service | 1957 | 40.0 |
| Salary+ mix of salary and other | 507 | 10.4 |
| Other Missing value | 426 82 | 8.7 1.6 |
| Number of GPs | ||
| 1 | 1640 | 33.0 |
| 2-3 | 1320 | 26.5 |
| 4-5 | 786 | 15.8 |
| 6+ Missing value | 1167 61 | 23.5 1.2 |
| GP trainees | ||
| No | 2758 | 55.4 |
| Yes Missing value | 2178 38 | 43.8 0.8 |
| Number of clinical professions * | ||
| 1 | 1669 | 33.6 |
| 2 | 2151 | 43.2 |
| 3+ Missing value | 1154 0 | 23.2 0 |
| Infection equipment indicator | ||
| 0-4 items | 382 | 7.7 |
| 5 items | 970 | 19.5 |
| 6 items | 1627 | 32.7 |
| 7 items Missing value | 1495 500 | 30.1 10.1 |
| Support for Proper Functioning | ||
|---|---|---|
| Total | N 4974 | % 100 |
| Strongly disagree | 823 | 16.5 |
| Disagree | 1419 | 28.5 |
| Neutral | 1014 | 20.4 |
| Agree | 830 | 16.7 |
| Strongly agree | 189 | 3.8 |
| Missing value | 699 | 14.1 |
| Experienced Limitations | Considered Making Adjustments | |||
|---|---|---|---|---|
| N 4974 | % 100 | N 4974 | % 100 | |
| None | 1056 | 21.2 | 1362 | 27.4 |
| Hardly | 1028 | 20.7 | 942 | 18.9 |
| To a limited extent | 1835 | 36.9 | 1674 | 33.7 |
| To a large extent | 1055 | 21.2 | 996 | 20.0 |
| Model I | Model II p < 0.001 | Model III p < 0.001 | Model IV p < 0.001 | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Intercept | 1.43 (1.10; 1.87) p = 0.008 | 1.10 (0.80; 1.51) | 0.69 (0.47; 1.03) | 0.42 (0.26; 0.69) p < 0.001 |
| Location of practice | (p = 0.673) | (p = 0.455) | (p = 0.607) | |
| Big (inner) city | Ref. | Ref. | Ref. | |
| Suburbs | 0.90 (0.72; 1.12) | 0.93 (0.73; 1.18) | 0.94 (0.74; 1.20) | |
| (Small) town | 0.99 (0.82; 1.19) | 1.06 (0.86; 1.29) | 1.04 (0.85; 1.27) | |
| Mixed urban-rural | 1.07 (0.90; 1.29) | 1.15 (0.95; 1.39) | 1.13 (0.93; 1.37) | |
| Rural | 1.02 (0.84; 1.23) | 1.09 (0.89; 1.34) | 1.09 (0.88; 1.34) | |
| Payment system | (p = 0.019) | (p = 0.006) | (p = 0.008) | |
| Capitation | Ref. | Ref. | Ref. | |
| Fee-for-service | 0.78 (0.62; 0.98) p = 0.037 | 0.74 (0.58; 0.94) p = 0.014 | 0.73 (0.57; 0.94) p = 0.014 | |
| Salary+ mix of salary and other | 1.28 (0.68; 2.43) | 1.45 (0.75; 2.78) | 1.37 (0.71; 2.63) | |
| Other | 1.27 (0.92; 1.75) | 1.27 (0.91; 1.78) | 1.26 (0.90; 1.77) | |
| Number of GPs | (p < 0.001) | (p < 0.001) | (p < 0.001) | |
| 1 | Ref. | Ref. | Ref. | |
| 2–3 | 1.57 (1.31; 1.87) p < 0.001 | 1.54 (1.28; 1.85) p < 0.001 | 1.53 (1.27; 1.85) p < 0.001 | |
| 4–5 | 1.46 (1.18; 1.81) p < 0.001 | 1.38 (1.09; 1.74) p = 0.006 | 1.39 (1.10; 1.76) p = 0.005 | |
| 6+ | 1.88 (1.49; 2.39) p < 0.001 | 1.77 (1.38; 2.28) p < 0.001 | 1.86 (1.44; 2.40) p < 0.001 | |
| Clinical professions (1–7)/multidisciplinary team | 0.96 (0.90; 1.02) p = 0.203 | 0.96 (0.90; 1.03) p = 0.231 | 0.94 (0.87; 1.02) p = 0.141 | |
| GP trainees | ||||
| No | Ref. | Ref. | Ref. | |
| Yes | 1.16 (1.01; 1.34) p = 0.035 | 1.16 (0.997; 1.34) p = 0.055 | 1.19 (1.02; 1.38) p = 0.027 | |
| Infection equipment indicator | p = 0.055 | p = 0.107 | ||
| 7 items | Ref. | Ref. | ||
| 6 items | 1.10 (0.94; 1.30) | 1.08 (0.92; 1.27) | ||
| 5 items | 1.20 (0.999; 1.45) p = 0.051 | 1.17 (0.97; 1.42) | ||
| 0–4 items | 1.41 (1.07; 1.85) p = 0.013 | 1.38 (1.05; 1.83) p = 0.023 | ||
| Safeguarding the well-being (score 0–9) | 1.06 (1.02; 1.11) p = 0.002 | 1.07 (1.02; 1.11) p = 0.002 | ||
| Adequate government support | p < 0.001 | |||
| Strongly agree | Ref. | |||
| Agree | 1.23 (0.87; 1.73) | |||
| Neutral | 1.30 (0.92; 1.83) | |||
| Disagree | 1.88 (1.33; 2.64) p < 0.001 | |||
| Strongly disagree | 2.15 (1.50; 3.07) p < 0.001 | |||
| Intercept variance (s.e.) | 0.56 (0.15) p < 0.001 | 0.44 (0.13) p < 0.001 | 0.40 (0.12) p < 0.001 | 0.35 (0.10 p < 0.001 |
| Model information | ||||
| Akaike’s Information Criterion (AIC) | 21,827.13 | 21,178.64 | 18,596.34 | 18,277.96 |
| −2 Log Likelihood | 21,825.13 | 21,176.64 | 18,594.34 | 18,275.96 |
| Likelihood ratio test | 652.49 (df = 17) p < 0.001 | 2582.30 (df = 12) p < 0.001 | 318.38 (df = 4) p < 0.001 |
| Model I | Model II (p < 0.000) | Model III (p = 0.000) | Model IV (p = 0.000) | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Intercept | 1.28 (1.01; 1.62) p = 0.044 | 0.76 (0.56; 1.03) p = 0.080 | 0.36 (0.24; 0.53) p < 0.001 | 0.32 (0.19; 0.53) p < 0.001 |
| Location of practice | (p = 0.063) | (p = 0.017) | (p = 0.024) | |
| Big (inner) city | Ref. | Ref. | Ref. | |
| Suburbs | 0.98 (0.78; 1.22) | 0.94 (0.75; 1.20) | 0.95 (0.75; 1.21) | |
| (Small) town | 0.93 (0.77; 1.11) | 0.92 (0.76; 1.12) | 0.90 (0.74; 1.10) | |
| Mixed urban-rural | 1.14 (0.95; 1.36) | 1.16 (0.96; 1.41) | 1.14 (0.94; 1.38) | |
| Rural | 1.21 (1.002; 1.46) p = 0.048 | 1.28 (1.04; 1.56) p = 0.019 | 1.25 (1.02; 1.54) p = 0.031 | |
| Payment system | (p = 0.204) | (p = 0.093) | (p = 0.043) | |
| Capitation | Ref. | Ref. | Ref. | |
| Fee-for-service | 0.83 (0.66; 1.04) | 0.79 (0.62; 1.01) p = 0.063 | 0.75 (0.59; 0.97) p = 0.025 | |
| Salary+ mix of salary and other | 0.87 (0.49; 1.57) | 0.76 (0.40; 1.44) | 0.71 (0.37; 1.36) | |
| Other | 1.16 (0.85; 1.59) | 1.22 (0.87; 1.70) | 1.20 (0.86; 1.69) | |
| Number of GPs | (p = 0.008) | (p = 0.027) | (p = 0.023) | |
| 1 | Ref. | Ref. | Ref. | |
| 2–3 | 1.27 (1.07; 1.52) p = 0.007 | 1.30 (1.08; 1.57) p = 0.006 | 1.31 (1.09; 1.59) p = 0.005 | |
| 4–5 | 1.27 (1.02; 1.57) p = 0.033 | 1.18 (0.94; 1.49 | 1.21 (0.96; 1.53) | |
| 6+ | 1.47 (1.16; 1.85) p = 0.001 | 1.36 (1.05; 1.74) p = 0.018 | 1.38 (1.07; 1.77) p = 0.013 | |
| Clinical_professions (1–7)/multidisciplinary team | 1.11 (1.04; 1.18) p < 0.001 | 1.08 (1.01; 1.16) p = 0.023 | 1.10 (1.01; 1.19) p = 0.022 | |
| GP trainees | ||||
| No | Ref. | Ref. | Ref. | |
| Yes | 1.27 (1.11; 1.46) p < 0.001 | 1.25 (1.08; 1.45) p = 0.003 | 1.27 (1.09; 1.48) p = 0.002 | |
| Infection equipment indicator | (p = 0.005) | (p = 0.006) | ||
| 7 items | Ref. | Ref. | ||
| 6 items | 1.07 (0.92; 1.26) | 1.06 (0.90; 1.25) | ||
| 5 items | 1.30 (1.08; 1.57) p = 0.006 | 1.30 (1.07; 1.57) p = 0.007 | ||
| 0–4 items | 0.85 (0.65; 1.10) | 0.84 (0.64; 1.10) | ||
| Safeguarding the well-being (score 0–9) | 1.16 (1.11; 1.20) p < 0.001 | 1.16 (1.12; 1.21) p < 0.001 | ||
| Adequate government support | (p < 0.001) | |||
| Strongly agree | Ref. | |||
| Agree | 1.08 (0.76; 1.53) | |||
| Neutral | 1.05 (0.74; 1.48) | |||
| Disagree | 1.46 (1.04; 2.06) p = 0.029 | |||
| Strongly disagree | 1.51 (1.05; 2.16) p = 0.024 | |||
| Intercept variance (s.e.) | 0.44 (0.12) p < 0.001 | 0.41 (0.12) p < 0.001 | 0.42 (0.12) p < 0.001 | 0.40 (0.12) p < 0.001 |
| Model Information | ||||
| AIC | 21,588.44 | 20,952.08 | 18,480.54 | 18,149.25 |
| −2 Log Likelihood | 21,586.44 | 20,950.08 | 18,478.54 | 18,147.25 |
| Likelihood ratio test | 636.36 (df = 17) p < 0.001 | 2471.54 (df = 12) p < 0.001 | 331.29 (df = 4) p < 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Windak, A.; Nessler, K.; Van Poel, E.; Collins, C.; Wójtowicz, E.; Murauskiene, L.; Hoffmann, K.; Willems, S. Responding to COVID-19: The Suitability of Primary Care Infrastructure in 33 Countries. Int. J. Environ. Res. Public Health 2022, 19, 17015. https://doi.org/10.3390/ijerph192417015
Windak A, Nessler K, Van Poel E, Collins C, Wójtowicz E, Murauskiene L, Hoffmann K, Willems S. Responding to COVID-19: The Suitability of Primary Care Infrastructure in 33 Countries. International Journal of Environmental Research and Public Health. 2022; 19(24):17015. https://doi.org/10.3390/ijerph192417015
Chicago/Turabian StyleWindak, Adam, Katarzyna Nessler, Esther Van Poel, Claire Collins, Ewa Wójtowicz, Liubove Murauskiene, Kathryn Hoffmann, and Sara Willems. 2022. "Responding to COVID-19: The Suitability of Primary Care Infrastructure in 33 Countries" International Journal of Environmental Research and Public Health 19, no. 24: 17015. https://doi.org/10.3390/ijerph192417015






