Models of Risk Selection in Maternal and Newborn Care: Exploring the Organization of Tasks and Responsibilities of Primary Care Midwives and Obstetricians in Risk Selection across The Netherlands
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
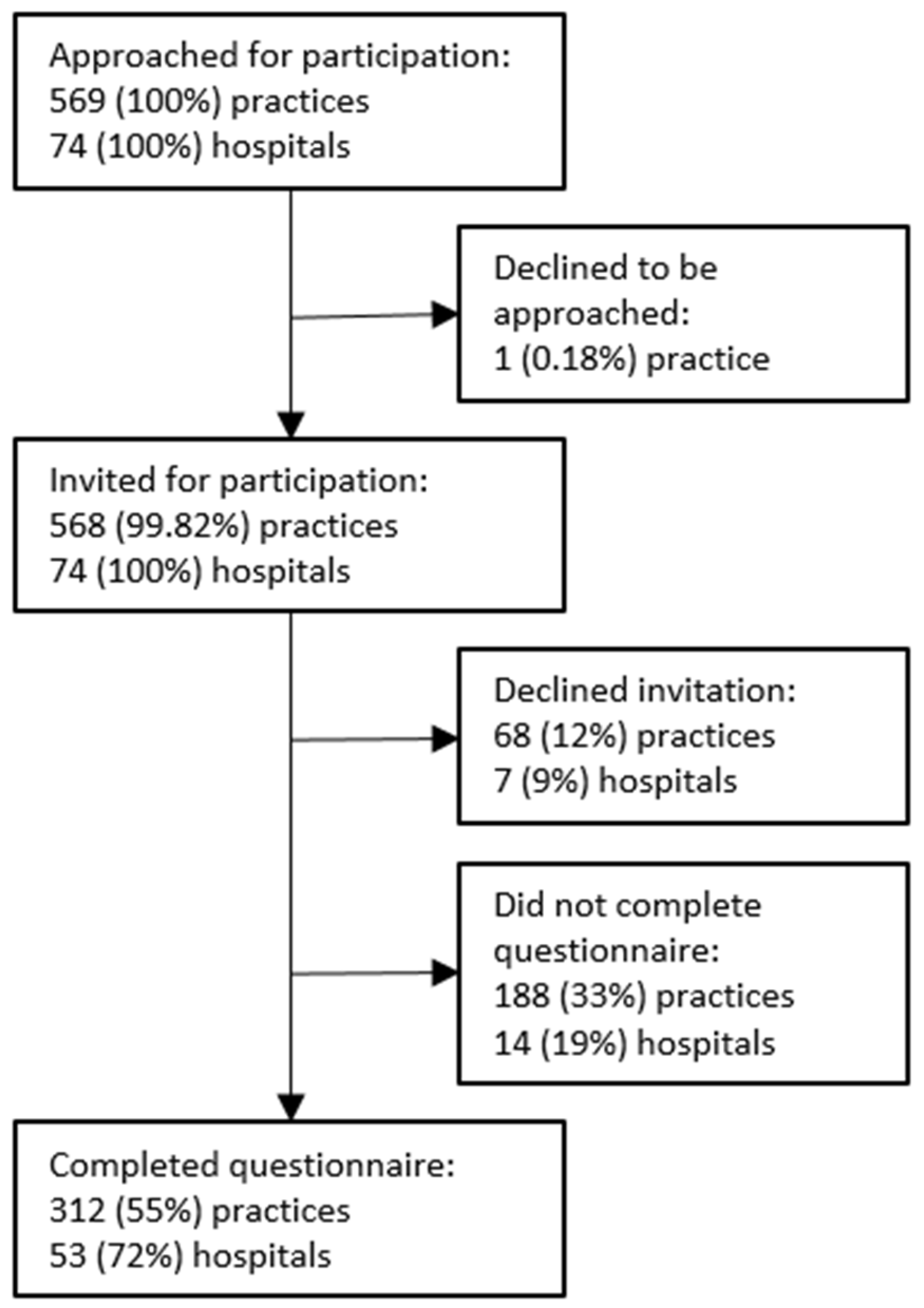
2.2. Study Population
2.3. Questionnaire
2.4. Data Collection
2.5. Analyses
3. Results
3.1. Characteristics of the Included Primary Midwifery Care Practices and Obstetrics Departments
3.2. Characteristics of Models of Risk Selection
3.3. Models of Risk Selection
3.4. Change in the Usual Organization of Tasks and Responsibilities in Risk Selection
3.5. Level of Satisfaction
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Lancet. Lancet Series Every Newborn. 2014. Available online: https://www.thelancet.com/series/everynewborn (accessed on 30 September 2021).
- The Lancet. The Lancet Series Midwifery. 2014. Available online: https://www.thelancet.com/series/midwifery (accessed on 30 September 2021).
- The Lancet. The Lancet Series Child Death in High-Income Countries. 2014. Available online: https://www.thelancet.com/series/child-death-in-high-income-countries (accessed on 30 September 2021).
- The Lancet. The Lancet Series Maternal Health. Available online: https://www.thelancet.com/series/maternal-health-2016 (accessed on 30 September 2021).
- Glasziou, P.; Straus, S.; Brownlee, S.; Trevena, L.; Dans, L.; Guyatt, G.; Elshaug, A.G.; Janett, R.; Saini, V. Evidence for underuse of effective medical services around the world. Lancet 2017, 390, 169–177. [Google Scholar] [CrossRef]
- Brownlee, S.; Chalkidou, K.; Doust, J.; Elshaug, A.G.; Glasziou, P.; Heath, I.; Nagpal, S.; Saini, V.; Srivastava, D.; Chalmers, K.; et al. Evidence for overuse of medical services around the world. Lancet 2017, 390, 156–168. [Google Scholar] [CrossRef] [Green Version]
- Miller, S.; Abalos, E.; Chamillard, M.; Ciapponi, A.; Colaci, D.; Comandé, D.; Diaz, V.; Geller, S.; Hanson, C.; Langer, A.; et al. Beyond too little, too late and too much, too soon: A pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016, 388, 2176–2192. [Google Scholar] [CrossRef]
- Renfrew, M.J.; McFadden, A.; Bastos, M.H.; Campbell, J.; Channon, A.A.; Cheung, N.F.; Silva, D.R.A.D.; Downe, S.; Kennedy, H.P.; Malata, A.; et al. Midwifery and quality care: Findings from a new evidence-informed framework for maternal and newborn care. Lancet 2014, 384, 1129–1145. [Google Scholar] [CrossRef]
- Souza, J.P.; Gülmezoglu, A.M.; Vogel, J.; Carroli, G.; Lumbiganon, P.; Qureshi, Z.; Costa, M.J.; Fawole, B.; Mugerwa, Y.; Nafiou, I.; et al. Moving beyond essential interventions for reduction of maternal mortality (the WHO Multicountry Survey on Maternal and Newborn Health): A cross-sectional study. Lancet 2013, 381, 1747–1755. [Google Scholar] [CrossRef]
- Goodarzi, B.; Walker, A.; Holten, L.; Schoonmade, L.; Teunissen, P.; Schellevis, F.; de Jonge, A. Towards a better understanding of risk selection in maternal and newborn care: A systematic scoping review. PLoS ONE 2020, 15, e0234252. [Google Scholar] [CrossRef] [PubMed]
- Rijksinstituut voor Volksgezondheid en Milieu. Beter Weten: Een Beter Begin. Samen Sneller Naar Een Betere Zorg Rond de Zwangerschap (Knowing Better. A Better Start. Together Faster towards Better Care Perinatal Care); RIVM: Utrecht, The Netherlands, 2020; Available online: https://www.rivm.nl/publicaties/beter-weten-beter-begin-samen-sneller-naar-betere-zorg-rond-zwangerschap (accessed on 1 October 2021).
- Expertgroep Zorgstandaard Integrale Geboortezorg. Zorgstandaard Integrale Geboortezorg Versie 1.2 (Carestandard Integrated Maternal and Newborn Care); Zorginstitut Nederland: Diemen, The Netherlands, 2021; Available online: https://www.zorginzicht.nl/binaries/content/assets/zorginzicht/kwaliteitsinstrumenten/zorgstandaard-integrale-geboortezorg.pdf (accessed on 1 October 2021).
- Veth, V.; van Dillen, J.; Leenders, A.; de Zeeuw, T.; Schippers, D.H.; van Drongelen, J. Gezamenlijke intakebesprekingen, betere uitkomsten? (Joint discussions of bookingsappointments, beter outcomes?). Ned. Tijdschr. Voor Obstet. Gynaecol. 2018, 131, 133. [Google Scholar]
- Smith, M.; Wagener, G.L.P.; van der Laar, F.A.; van Dillen, J. Integrale geboortezorg. Eerste ervaringen met een gezamenlijke intakebespreking (Integrated maternal and newborn care. First experiences with joint discussion of bookingappointments). Ned. Tijdschr. Voor Obstet. Gynaecol. 2016, 129, 191–195. [Google Scholar]
- Jongmans, L.J.G.; Verhoeven-Smeijers, C.J.M.; Wijnen, H.A.A.; van Runnard Heimel, P.J. Waar, en van wie ontvangt de zwangere haar zorg? (Where, and from whom do pregnant women receive care?). Ned. Tijdschr. Voor Obstet. Gynaecol. 2019, 132, 78–82. [Google Scholar]
- Commissie Verloskunde van het College Voor Zorgverzekeringen. Verloskundig Vademecum (Maternal and Newborn Care Vademecum); Zorginstitut Nederland: Diemen, The Netherlands, 2003. [Google Scholar]
- Goodarzi, B.; Holten, L.; van El, C.; de Vries, R.; Franx, A.; Houwaart, E. Risk and the politics of boundary work: Preserving autonomous midwifery in The Netherlands. Health Risk Soc. 2018, 20, 379–407. [Google Scholar] [CrossRef]
- Ministry of Health. Guidelines for Consultation with Bbstetric and Related Medical Services (Referral Guidelines); Ministry of Health: Wellington, New Zealand, 2012. Available online: https://www.health.govt.nz/system/files/documents/publications/referral-glines-jan12.pdf (accessed on 1 October 2021).
- Australian College of Midwives. National Midwifery Guidelines for Consultation and Referral; Australian College of Midwives: Canberra, Australia, 2021; Available online: https://www.midwives.org.au/shop/new-national-midwifery-guidelines-consultation-and-referral (accessed on 1 October 2021).
- Department of Health. Guidelines for Maternity Care in South Africa; Department of Health: Pretoria, South Africa, 2016; Available online: https://www.knowledgehub.org.za/system/files/elibdownloads/2020-08/CompleteMaternalBook.pdf (accessed on 1 October 2021).
- The Bedside Clinical Guidelines Partnership Staffordshire, Shropshire & Black Country Newborn and Maternity Network and Southern West Midlands. Obstetric Guidelines. 2017. Available online: https://www.networks.nhs.uk/nhs-networks/staffordshire-shropshire-and-black-country-newborn/obstetric-guidelines/obstetric-guidelines-2017-19 (accessed on 1 October 2021).
- Britisch Columbia College of Nurses and Midwives. Indications for Discussion, Consultation and Transfer of Care; Britisch Columbia College of Nurses and Midwives: Vancouver, BC, Canada, 2021; Available online: https://www.bccnm.ca/Documents/standards_practice/rm/RM_Indications_for_Discussion_Consultation_and_Transfer_of_Care.pdf (accessed on 1 October 2021).
- Kennedy, H.P.; Yoshida, S.; Costello, A.; Declercq, E.; Dias, M.A.; Duff, E.; Gherissi, A.; Kaufman, K.; McConville, F.; McFadden, A.; et al. Asking different questions: Research priorities to improve the quality of care for every woman, every child. Lancet Glob. Health 2016, 4, e777–e779. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, H.P.; Cheyney, M.; Dahlen, H.G.; Downe, S.; Foureur, M.J.; Homer, C.S.; Jefford, E.; McFadden, A.; Michel-Schuldt, M.; Sandall, J.; et al. Asking different questions: A call to action for research to improve the quality of care for every woman, every child. Birth 2018, 45, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Kenens, R.; van der Velden, L.; Vis, E.; Batenburg, R. Cijfers uit de Registratie van Verloskundigen. Peiling 2018 (Registration of Midwives. 2018); NIVEL: Utrecht, The Netherlands, 2018. [Google Scholar]
- College Perinatale Zorg. Verloskundige Samenwerkingsverband (VSV) (Maternity Care Collaboration (MCC)); College Perinatale Zorg: Utrecht, The Netherlands, 2020; Available online: https://www.kennisnetgeboortezorg.nl/geboortezorg-landschap/verloskundig-samenwerkingsverband/ (accessed on 30 September 2020).
- Nederlandse Vereniging voor Obstetrie en Gynaecologie. Alles Wat u Wilt Weten over de Nederlandse Vereniging voor Obstetrie & Gynaecologie (Evertything You Want to Know About the the Dutch Society of Obstetrics and Gynaecology). Available online: https://www.nvog.nl/ (accessed on 1 October 2021).
- Koninklijke Nederlandse Organistie van Verloskundigen. Beroepsorganisatie Van en Voor Verloskundigen. Available online: https://www.knov.nl/ (accessed on 1 October 2021).
- Castor EDC. Castor Electronic Data Capture. 2019. Available online: https://castoredc.com (accessed on 1 October 2021).
- Goodarzi, B. Onderzoek naar Risicoselectie Binnen Integrale Geboortezorg. Doe Mee! (Study into Risk Selection in Integrated Maternal and Newborn Care. Participcate!); College Perinatale Zorg: Ultrecht, The Netherlands, 2019; Available online: https://www.kennisnetgeboortezorg.nl/nieuws/onderzoek-naar-risicoselectie-binnen-integrale-geboortezorg-doe-mee/ (accessed on 1 October 2021).
- Goodarzi, B. Doe mee aan onderzoek risicoselectie (Particapate in research into risk selection). Tijdschr. Voor Verloskd. 2019, 42, 8. [Google Scholar]
- Goodarzi, B. Onderzoek naar risicoselectie binnen integrale geboortezorg. Doe mee! (Research into risk selection in integrated maternal and newborn care. Participate!). Ned. Tijdschr. Voor Obstet. Gynaecol. 2019, 132, 259. [Google Scholar]
- Goodarzi, B. Samen Weten We Meer over Gezamenlijke Risicoselectie. Doe Mee aan Dit Onderzoek! (We Can Better Understand Joint Risk Selection Together. Participcate in This Study!). Kennispoort Verloskunde. 2019. Available online: https://www.kennispoort-verloskunde.nl/samen-weten-we-meer-over-gezamenlijke-risicoselectie-doe-je-mee-aan-dit-onderzoek/ (accessed on 18 October 2021).
- Microsoft Corporation. Microsoft Excel. 2018. Available online: https://office.microsoft.com/excel (accessed on 1 October 2021).
- StataCorp. STATA, Release 14.1. 2015 College Station, TX: StataCorp LP. Available online: https://www.scirp.org/(S(i43dyn45teexjx455qlt3d2q))/reference/ReferencesPapers.aspx?ReferenceID=1736202 (accessed on 1 October 2021).
- Ministerie van Binnenlandse zakenen Koninkrijksrelaties. Provincies (Provinces). Available online: https://www.regioatlas.nl/regioindelingen/regioindelingen_indeling/t/provincies (accessed on 1 October 2021).
- Perined. Regioteams (Regional Teams). Available online: https://www.perined.nl/onderwerpen/audit/regioteams (accessed on 1 October 2021).
- Warmelink, J.C.; Wiegers, T.A.; de Cock, T.P.; Klomp, T.; Hutton, E.K. Collaboration of midwives in primary care midwifery practices with other maternity care providers. Midwifery 2017, 55, 45–52. [Google Scholar] [CrossRef] [Green Version]
- Stuurgroep Zwangerschap en Geboorte. Een Goed Begin. Veilge Zorg Rond Zwangerschap En Geboorte (A Good Start. Safe Care in Pregnancy and Birth); Stuurgroep Zwangerschap en Geboorte. 2009. Available online: https://www.knov.nl/serve/file/knov.nl/knov_downloads/298/file/Rapport%27Eengoedbegin%27.pdf (accessed on 1 October 2021).
- Posthumus, A.G.; Schölmerich, V.L.N.; Waelput, A.J.M.; Vos, A.A.; De Jong-Potjer, L.C.; Bakker, R.; Bonsel, G.J.; Groenewegen, P.; Steegers, E.A.P.; Denktaş, S. Bridging between professionals in perinatal care: Towards shared care in The Netherlands. Matern Child Health J. 2013, 17, 1981–1989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonsel, G.J.; Birnie, E.; Denktaş, S.; Steegers, E.A.P.; Poeran, V.J.J. Lijnen in de Perinatale Sterfte (Lines in Perinatal Mortality); University Medical Center: Rotterdam, The Netherlands, 2010. [Google Scholar]
- Evers, A.C.; Brouwers, H.A.; Hukkelhoven, C.W.; Nikkels, P.G.; Boon, J.; van Egmond-Linden, A.; Hillegersberg, J.; Snuif, Y.S.; Sterken-Hooisma, S.; Bruinse, H.W.; et al. Perinatal mortality and severe morbidity in low and high risk term pregnancies in The Netherlands: Prospective cohort study. BMJ 2010, 341, c5639. [Google Scholar] [CrossRef] [Green Version]
- Avery, M.D.; Montgomery, O.; Brandl-Salutz, E. Essential components of successful collaborative maternity care models. Obstet. Gynecol. Clin. 2012, 39, 423–434. [Google Scholar] [CrossRef]
- Centre Fédéral D’expertises des Soins de Santé. Tools to Support the Referral Between Midwives and Obstetricians during Midwifery-Led Antenatal Follow-Up. 2019. Available online: https://kce.fgov.be/fr/node/4567 (accessed on 1 October 2021).
- Perdok, H.; Jans, S.; Verhoeven, C.; van Dillen, J.; Batenburg, R.; Mol, B.W.; Schellevis, F.; de Jonge, A. Opinions of professionals about integrating midwife- and obstetrician-led care in The Netherlands. Midwifery 2016, 37, 9–18. [Google Scholar] [CrossRef] [Green Version]
- Perdok, H.; Jans, S.; Verhoeven, C.; Henneman, L.; Wiegers, T.; Mol, B.W.; Schellevis, F.; de Jonge, A. Opinions of maternity care professionals and other stakeholders about integration of maternity care: A qualitative study in The Netherlands. BMC Pregnancy Childbirth 2016, 16, 188. [Google Scholar] [CrossRef] [Green Version]
- Perdok, H.; Mokkink, L.; van Dillen, J.; Westerneng, M.; Jans, S.; Mol, B.W.; de Jonge, A. Opinions of maternity care professionals about integration of care during labor for “moderate risk” indications: A delphi study in The Netherlands. Birth 2014, 41, 195–205. [Google Scholar] [CrossRef]
- Perined. Perinatale Zorg in Nederlands Anno 2019 (Perinatal Care in The Netherlands in 2019); Perined: Utrecht, The Netherlands, 2020; Available online: https://assets.perined.nl/docs/aeb10614-08b4-4a1c-9045-8af8a2df5c16.pdf (accessed on 1 October 2021).
- Haggerty, J.L. Continuity of care: A multidisciplinary review. BMJ 2003, 327, 1219–1221. [Google Scholar] [CrossRef] [Green Version]
- Wiegers, T.A. The quality of maternity care services as experienced by women in The Netherlands. BMC Pregnancy Childbirth 2009, 9, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, D.C. Midwife–physician collaboration: A conceptual framework for interprofessional collaborative practice. J. Midwifery Womens Health 2015, 60, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Van Helmond, I.; Korstjens, I.; Mesman, J.; Nieuwenhuijze, M.; Horstman, K.; Scheepers, H.; Spaanderman, M.; Keulen, J.; de Vries, R. What makes for good collaboration and communication in maternity care? A scoping study. Int. J. Childbirth 2015, 5, 210–223. [Google Scholar] [CrossRef]
- De Vries, E.F.; Scheefhals, Z.T.M.; de Bruin-Kooistra, M.; Baan, C.A.; Struijs, J.N. A scoping review of alternative payment models in maternity care: Insights in key design elements and effects on health and spending. Int. J. Integr. Care 2021, 21, 6. [Google Scholar] [CrossRef] [PubMed]
- Struijs, J.N.; de Vries, E.F.; Scheefhals, Z.T.M.; Molenaar, J.M.; Baan, C.A. Integrale Bekostiging van de Geboortezorg: Ervaringen Na Drie Jaar En de Eerste Zichtbare Effecten (Bundeld Payment Methods in Maternal and Newborn Care: A Three-Year Evaluation of Experiences and Effects); National Institute for Public Health and the Environment: Utrecht, The Netherlands, 2020. [Google Scholar] [CrossRef]
- Porter, M.E. What is value in health care? N. Engl. J. Med. 2010, 363, 2477–2481. [Google Scholar] [CrossRef]
- Expert panel on effective ways of investing in health. Defining Value in “Value-Based Healthcare”; European Commission: Brussels, Belgium, 2019. [Google Scholar]
- De Jonge, A.; Downe, S.; Page, L.; Devane, D.; Lindgren, H.; Klinkert, J.; Gray, M.; Jani, A. Value based maternal and newborn care requires alignment of adequate resources with high value activities. BMC Pregnancy Childbirth 2019, 19, 428. [Google Scholar] [CrossRef]
- Allen, M. Validity, halo effect. In The SAGE Encyclopedia of Communication Research Methods; SAGE Publications, Inc: Thousand Oaks, CA, USA, 2017. [Google Scholar] [CrossRef]
- Powell, R.A.; Holloway, F.; Lee, J.; Sitzia, J. Satisfaction research and the uncrowned king: Challenges and future directions. J. Ment. Health 2004, 13, 11–20. [Google Scholar] [CrossRef]
| Primary Midwifery Care Practices | Obstetrics Departments | ||
|---|---|---|---|
| n (%) | n (%) | ||
| Total | 312 (100) | Total | 53 (100) |
| Profession | Profession | ||
| Primary care midwife | 312 (100) | Hospital-based midwife | 9 (17) |
| Midwife working both as primary care midwife and hospital-based midwife | 1 (2) | ||
| Obstetrician | 30 (57) | ||
| Manager | 13 (25) | ||
| Number of care units/year 1 | Number of births/year 2 | ||
| ≤250 | 181 (58) | ≤1000 | 10 (19) |
| 251–500 | 117 (38) | 1001–2000 | 21 (40) |
| 501–750 | 11 (4) | 2001–3000 | 15 (21) |
| ≥751 | 3 (1) | ≥300–4000 | 6 (12) |
| The Organization of Tasks and Responsibilities Regarding the Booking Appointment | n (%) |
|---|---|
| All women start their care in primary midwifery care practices, regardless of their risk profile. Primary care midwives are responsible for the booking appointment. | 11 (16) |
| All women start their care in secondary obstetrician-led care in the hospital, regardless of their risk profile. Obstetricians are responsible for the booking appointment. | 0 (0) |
| All women with uncomplicated pregnancies start their care in primary midwifery care, and women with a high-risk profile start their care in secondary obstetrician-led care in the hospital. Primary care midwives are responsible for the booking appointment for women with uncomplicated pregnancies and obstetricians are responsible for the booking appointment of women with a high-risk profile. | 52 (75) |
| Contradictory answers amongst respondents within the MCC *. | 6 (9) |
| Organization of tasks and responsibilities regarding risk assessment after booking appointment. | |
| Primary care midwives assess risk and initiate a consultation or transfer of care only if necessary, without discussing this first with the obstetrician. | 42 (61) |
Risk is assessed collaboratively. Primary care midwives and obstetricians discuss whether a consultation or transfer of care is necessary:
| 16 (23)
|
| Contradictory answers amongst respondents within the MCC. | 4 (6) |
| Variation within the MCC. | 3 (4) |
| Unclear. | 4 (6) |
| Organization of tasks and responsibilities in decision-making after discussion between primary care midwives and obstetricians. | |
| Primary care midwives and obstetricians are together responsible for decision-making. | 100 (100) |
| Primary care midwives are responsible for decision-making. | 0 (0) |
| Obstetricians are responsible for decision-making. | 0 (0) |
| Bi-Disciplinary | Multidisciplinary | |
|---|---|---|
| n (%) | n (%) | |
| Discussion is only scheduled at request, and not scheduled routinely. | 9 (13) | 28 (40) |
| Discussion is scheduled at request, and scheduled routinely. | 52 (75) | 37 (54) |
| Contradictory answers amongst respondents within the MCC *. | 1 (1) | 2 (3) |
| Variation within the MCC. | 6 (9) | 0 |
| Unclear. | 1 (1) | 2 (3) |
| n (%) | |
|---|---|
| One or more visits to the obstetrician are scheduled routinely for all women in primary midwife-led care. | 1 (1) |
| One or more visits to the primary care midwife are scheduled routinely for all women in obstetrician-led care. | 3 (4) |
| One or more visits to the obstetrician are scheduled routinely for women with a medium or high-risk profile in primary midwife-led care. | 11 (16) |
| One or more visits to the primary care midwife are scheduled routinely for all women in obstetrician-led care, and vice versa to the obstetrician for all women in primary midwife-led care. | 2 (3) |
| One or more visits to the primary care midwife are scheduled routinely for women in obstetrician-led care, and vice versa to the obstetrician for women with a medium or high-risk profile in primary midwife-led care. | 1 (1) |
| Variation within the MCC *. | 1 (1) |
| Unclear. | 4 (6) |
| Not mentioned in the answers. | 46 (67) |
| MRS * 1 | MRS 2 | MRS 3 | |
|---|---|---|---|
| n (Row %) | n (Row %) | n (Row %) | |
| Total | 42 (61) | 16 (23) | 11 (16) |
| North | 3 (33) | 1 (11) | 5 (56) |
| East | 9 (64) | 4 (29) | 1 (7) |
| South | 2 (14) | 10 (71) | 2 (14) |
| Southwest | 12 (75) | 1 (6) | 3 (19) |
| Northwest | 16 (100) | 0 (0) | 0 (0) |
| Change in the Past Decade | Reversed Change Back to the Usual Model | |
|---|---|---|
| n (%) | n (%) | |
| Total MCCs # | 69 (100) | 50 (100) * |
| No | 15 (22) | 41 (82) |
| Yes | 46 (67) | 9 (18) |
| Variation within the MCC | 4 (5) | |
| Contradictory answers amongst respondents within the MCC | 4 (5) |
| MCC # | Primary Midwifery Care Practices | Obstetrics Departments | ||||
|---|---|---|---|---|---|---|
| Very Satisfied | Not Very Satisfied | Very Satisfied | Not Very Satisfied | Very Satisfied | Not Very Satisfied | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Quality of care | ||||||
| MRS # 1 | 32 (57) | 10 (77) | 34 (61) | 7 (63) | 17 (47) | 13 (81) |
| MRS 2 | 14 (25) | 2 (15) | 13 (23) | 2 (18) | 13 (36) | 1 (6) |
| MRS 3 | 10 (18) | 1 (7) | 9 (16) | 2 (18) | 6 (17) | 2 (13) |
| Collaboration | ||||||
| MRS 1 | 28 (55) | 14 (78) | 26 (54) | 15 (79) | 20 (53) | 10 (71) |
| MRS 2 | 13 (25) | 3 (17) | 13 (27) | 2 (12) | 12 (32) | 2 (14) |
| MRS 3 | 10 (20) | 1 (6) | 9 (19) | 2 (12) | 6 (16) | 2 (14) |
| p-value * | 0.23 | 0.17 | 0.46 | |||
| Organization of care | ||||||
| MRS 1 | 20 (56) | 22 (67) | 22 (63) | 19 (59) | 15 (54) | 15 (63) |
| MRS 2 | 9 (25) | 7 (21) | 7 (20) | 8 (25) | 8 (29) | 6 (25) |
| MRS 3 | 7 (19) | 4 (12) | 6 (17) | 5 (16) | 5 (18) | 3 (13) |
| p-value * | 0.66 | 0.94 | 0.80 | |||
| Time investment | ||||||
| MRS 1 | 12 (67) | 30 (59) | 9 (64) | 32 (60) | 14 (64) | 16 (53) |
| MRS 2 | 3 (17) | 13 (25) | 3 (21) | 12 (23) | 5 (23) | 9 (30) |
| MRS 3 | 3 (17) | 8 (16) | 2 (14) | 9 (17) | 3 (14) | 5 (17) |
| p-value * | 0.74 | 1.00 | 0.74 | |||
| Autonomy | ||||||
| MRS 1 | 32 (64) | 10 (53) | 32 (65) | 9 (50) | 23 (55) | 7 (70) |
| MRS 2 | 11 (22) | 5 (26) | 11 (22) | 4 (22) | 11 (26) | 3 (30) |
| MRS 3 | 7 (14) | 4 (21) | 6 (12) | 5 (28) | 8 (19) | 0 |
| p-value * | 0.64 | 0.29 | 0.44 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goodarzi, B.; Verhoeven, C.; Berks, D.; de Vries, E.F.; de Jonge, A. Models of Risk Selection in Maternal and Newborn Care: Exploring the Organization of Tasks and Responsibilities of Primary Care Midwives and Obstetricians in Risk Selection across The Netherlands. Int. J. Environ. Res. Public Health 2022, 19, 1046. https://doi.org/10.3390/ijerph19031046
Goodarzi B, Verhoeven C, Berks D, de Vries EF, de Jonge A. Models of Risk Selection in Maternal and Newborn Care: Exploring the Organization of Tasks and Responsibilities of Primary Care Midwives and Obstetricians in Risk Selection across The Netherlands. International Journal of Environmental Research and Public Health. 2022; 19(3):1046. https://doi.org/10.3390/ijerph19031046
Chicago/Turabian StyleGoodarzi, Bahareh, Corine Verhoeven, Durk Berks, Eline F. de Vries, and Ank de Jonge. 2022. "Models of Risk Selection in Maternal and Newborn Care: Exploring the Organization of Tasks and Responsibilities of Primary Care Midwives and Obstetricians in Risk Selection across The Netherlands" International Journal of Environmental Research and Public Health 19, no. 3: 1046. https://doi.org/10.3390/ijerph19031046






