Investigating the Association between Unhealthy Dietary Habits and Obesity among Libyan Adults
Abstract
:1. Background
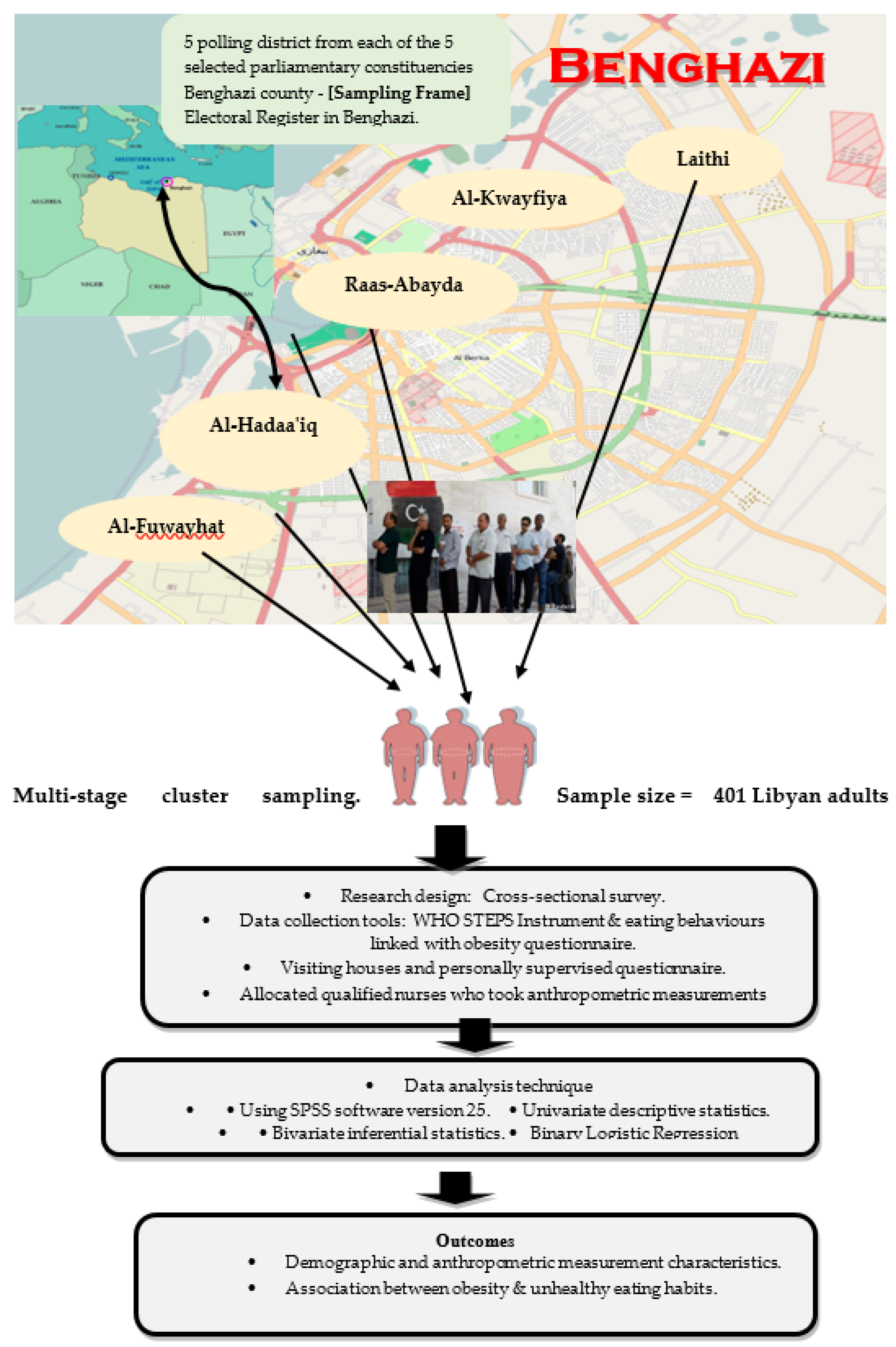
2. Methods
2.1. Study Design and Setting
2.2. Participants and Procedure
2.3. Ethical Considerations
2.4. Measures
2.4.1. Anthropometric Measuring Tools
2.4.2. Sociodemographic Characteristics
2.4.3. Unhealthy Eating Behavior Assessment
2.5. Translation Technique
2.6. Statistical Analysis
2.7. Validity and Reliability of the Two Questionnaires
3. Results
4. Summary and Interpretation of Binary Logistic Regression Model
5. Discussion
5.1. Fast-Food Consumption
5.2. Consumption of Sugar-Sweetened Beverages (SSBs)
5.3. Eating Less than Five Daily Portions of Fruit and Vegetables
5.4. A High Frequency of Skipping Breakfast
5.5. The Consumption of Large Food Portion Sizes
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| SES | socioeconomic status |
| SSBs | Sugar-Sweetened Beverages |
| FV | Fruit and vegetable |
| FPS | Food Portion Size |
| SEM | Socio-Ecological Model |
| SBF | Skipping Breakfast |
| FFR | Fast Food Restaurant |
References
- NCD Risk Factor Collaboration (NCD-RisC). Height and Body-Mass Index Trajectories of School-Aged Children and Adolescents from 1985 to 2019 in 200 Countries and Territories: A Pooled Analysis of 2181 Population-Based Studies with 65 Million Participants. Lancet 2020, 396, 1511–1524. [Google Scholar] [CrossRef]
- Pineda, E.; Sanchez-Romero, L.M.; Brown, M.; Jaccard, A.; Jewell, J.; Galea, G.; Webber, L.; Breda, J. Forecasting Future Trends in Obesity across Europe: The Value of Improving Surveillance. Obes. Facts 2018, 11, 360–371. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation (WHO). Obesity and Overweight Fact Sheet No. 311. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight/ (accessed on 8 August 2021).
- Lemamsha, H. Exploring the Risk and Protective Factors Associated with Obesity Amongst Libyan Adults (20–65 years). Ph.D. Thesis, University of Bedfordshire, Luton, UK, 2016. Available online: https://core.ac.uk/download/pdf/77037983.pdf (accessed on 5 October 2021).
- Lemamsha, H.; Papadopoulos, C.; Randhawa, G. Understanding the Risk and Protective Factors Associated with Obesity amongst Libyan Adults-a Qualitative Study. BMC Public Health. 2018, 18, 493. [Google Scholar] [CrossRef] [Green Version]
- Lemamsha, H.; Papadopoulos, C.; Randhawa, G. Perceived Environmental Factors Associated with Obesity in Libyan Men and Women. Int. J. Environ. Res. Public Health 2018, 15, 301. [Google Scholar] [CrossRef] [Green Version]
- Lachat, C.; Otchere, S.; Roberfroid, D.; Abdulai, A.; Seret, F.M.; Milesevic, J.; Xuereb, G.; Candeias, V.; Kolsteren, P. Diet and Physical Activity for the Prevention of Noncommunicable Diseases in Low- and Middle-Income Countries: A Systematic Policy Review. PLoS Med. 2013, 10, e1001465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global Nutrition Transition and the Pandemic of Obesity in Developing Countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the Double Burden of Malnutrition and the Changing Nutrition Reality. Lancet. 2020, 395, 65–74. [Google Scholar] [CrossRef]
- Greenwood, J.L.; Murtaugh, M.A.; Omura, E.M.; Alder, S.C.; Stanford, J.B. Creating a Clinical Screening Questionnaire for Eating Behaviors Associated with Overweight and Obesity. J. Am. Board Fam. Med. 2008, 21, 539–548. [Google Scholar] [CrossRef]
- Lemamsha, H.; Papadopoulos, C.; Randhawa, G. Prevalence of overweight and obesity among libyan men and women. Biomed. Res. Int. 2019, 2019, 8531360. [Google Scholar] [CrossRef]
- Yoo, S. Dynamic Energy Balance and Obesity Prevention. J. Obes. Metab. Syndr. 2018, 27, 203–212. [Google Scholar] [CrossRef]
- González-Gross, M.; Aparicio-Ugarriza, R.; Calonge-Pascual, S.; Gómez-Martínez, S.; García-Carro, A.; Zaragoza-Martí, A.; Sanz-Valero, J.; Wanden-Berghe, C.; Martínez, J.A.; Gil, Á.; et al. Is Energy Expenditure or Physical Activity Considered When Energy Intake Is Measured? A Scoping Review 1975–2015. Nutrients 2021, 13, 3262. [Google Scholar] [CrossRef]
- Abdelaal, M.; le Roux, C.W.; Docherty, N.G. Morbidity and Mortality Associated with Obesity. Ann. Transl. Med. 2017, 5, 161. [Google Scholar] [CrossRef] [Green Version]
- Darmon, N.; Drewnowski, A. Contribution of Food Prices and Diet Cost to Socioeconomic Disparities in Diet Quality and Health: A Systematic Review and Analysis. Nutr. Rev. 2015, 73, 643–660. [Google Scholar] [CrossRef]
- Rao, M.; Afshin, A.; Singh, G.; Mozaffarian, D. Abstract 059: Do Healthier Foods or Diet Patterns Cost More than Less Healthy Options? A Systematic Review and Meta-Analysis. Circulation 2013, 127 (Suppl. S12), A059. [Google Scholar] [CrossRef]
- Sehib, K.; Jackson, E.; Gorton, M. Gender, Social Acceptability and the Adoption of Supermarkets: Evidence from Libya. Int. J. Consum. Stud. 2013, 37, 379–386. [Google Scholar] [CrossRef]
- International Institute for Counter-Terrorism, I.C.T. ISIS in Libya-Exploitation and Governance of Areas of Limited Statehood. Available online: https://www.ict.org.il/UserFiles/ICTWPS-36-Schnitt.pdf (accessed on 3 November 2021).
- United Nations Office for the Coordination of Humanitarian Affairs, U.N.O.C.H.A. Libya Humanitarian Appeal 2014. Available online: https://docs.unocha.org/sites/dms/CAP/2014_Libya_Humanitarian_Appeal.pdf (accessed on 13 October 2021).
- Charan, J.; Biswas, T. How To Calculate Sample Size For Different Study Designs In Medical Research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maukonen, M.; Männistö, S.; Tolonen, H. A Comparison of Measured versus Self-Reported Anthropometrics for Assessing Obesity in Adults: A Literature Review. Scand. J. Public Health 2018, 46, 565–579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). WHO Steps Instrument. 2013. Available online: https://www.who.int/ncds/surveillance/steps/STEPS_Instrument_v2.1.pdf (accessed on 18 August 2021).
- Lee, W.L.; Chinna, K.; Abdullah, K.L.; Abidin, I.Z. The Forward-Backward and Dual-Panel Translation Methods Are Comparable in Producing Semantic Equivalent Versions of a Heart Quality of Life Questionnaire. Int. J. Nurs. Pract. 2019, 25, e12715. [Google Scholar] [CrossRef] [PubMed]
- Chamieh, M.C.; Moore, H.J.; Summerbell, C.; Tamim, H.; Sibai, A.M.; Hwalla, N. Diet, Physical Activity and Socio-Economic Disparities of Obesity in Lebanese Adults: Findings from a National Study. BMC Public Health. 2015, 15, 279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chukwuonye, I.I.; Madukwe, O.; Chuku, A.; Onyeonoro, U.; Okpechi, I.; Ogah, O.S.; Okafor, G.O.C. Socioeconomic Status and Obesity in Abia State, South East Nigeria. Diabetes Metab. Syndr. Obes. 2013, 6, 371–378. [Google Scholar] [CrossRef] [Green Version]
- Adole, A.A.; Ware, M.B. Assessment of Breakfast Eating Habits and Its Association with Cognitive Performance of Early Adolescents (11–13 Years) in Shebedino District, Sidama Zone, Southern Ethiopia. J. Food Nutr. Sci. 2014, 2, 130–137. [Google Scholar] [CrossRef]
- León-Muñoz, L.M.; García-Esquinas, E.; Soler-Vila, H.; Guallar-Castillón, P.; Banegas, J.R.; Rodríguez-Artalejo, F. Unhealthy Eating Behaviors and Weight Gain: A Prospective Study in Young and Middle-Age Adults. Obesity 2016, 24, 1178–1184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bryman, A. Social Research Methods, 5th ed.; Oxford University Press: Oxford, UK, 2016. [Google Scholar]
- Blundell, J.E. The Contribution of Behavioural Science to Nutrition: Appetite Control. Nutr. Bull. 2017, 42, 236–245. [Google Scholar] [CrossRef]
- Gibbons, C.; Blundell, J.E. Quantifying Appetite and Satiety. Translational Research Methods in Diabetes, Obesity, and Nonalcoholic Fatty Liver Disease. Springer 2019, 2019, 121–140. [Google Scholar]
- Varela, C.; Andrés, A.; Saldaña, C. The Behavioral Pathway Model to Overweight and Obesity: Coping Strategies, Eating Behaviors and Body Mass Index. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2019, 25, 1277–1283. [Google Scholar] [CrossRef]
- Souza, A.M.; Bezerra, I.W.L.; Pereira, G.S.; Torres, K.G.; Costa, R.M.; Oliveira, A.G. Relationships between Motivations for Food Choices and Consumption of Food Groups: A Prospective Cross-Sectional Survey in Manufacturing Workers in Brazil. Nutrients 2020, 12, 1490. [Google Scholar] [CrossRef]
- Marsola, C.D.M.; Cunha, L.M.; De Carvalho-Ferreira, J.P.; Da Cunha, D.T. Factors Underlying Food Choice Motives in a Brazilian Sample: The Association with Socioeconomic Factors and Risk Perceptions about Chronic Diseases. Foods 2020, 9, 1114. [Google Scholar] [CrossRef]
- Burgoine, T.; Sarkar, C.; Webster, C.J.; Monsivais, P. Examining the Interaction of Fast-Food Outlet Exposure and Income on Diet and Obesity: Evidence from 51,361 UK Biobank Participants. Int. J. Behav. Nutr. 2018, 15, 1–12. [Google Scholar]
- Liu, J.; Rehm, C.D.; Micha, R.; Mozaffarian, D. Quality of Meals Consumed by US Adults at Full-Service and Fast-Food Restaurants, 2003–2016: Persistent Low Quality and Widening Disparities. J. Nutr. 2020, 150, 873–883. [Google Scholar] [CrossRef]
- Okuyama, K.; Li, X.; Abe, T.; Hamano, T.; Franks, P.W.; Nabika, T.; Sundquist, K. Fast Food Outlets, Physical Activity Facilities, and Obesity among Adults: A Nationwide Longitudinal Study from Sweden. Int. J. Obes. 2020, 44, 1703–1711. [Google Scholar] [CrossRef]
- Zaghloul, S.; Al-Hooti, S.N.; Al-Hamad, N.; Al-Zenki, S.; Alomirah, H.; Alayan, I.; Al-Attar, H.; Al-Othman, A.; Al-Shami, E.; Al-Somaie, M.; et al. Evidence for Nutrition Transition in Kuwait: Over-Consumption of Macronutrients and Obesity. Public Health Nutr. 2012, 16, 596–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandoura, N.; Al-Raddadi, R.; Abdulrashid, O.; Shah, H.; Kassar, S.; Adel Hawari, A.; Jahhaf, J. Factors Associated With Consuming Junk Food Among Saudi Adults In Jeddah City. Cureus 2017, 9, 2–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shori, A.; Albaik, M.; Bokhari, F. Fast Food Consumption And Increased Body Mass Index As Risk Factors For Weight Gain And Obesity In Saudi Arabia. Obes. Med. 2017, 8, 1–5. [Google Scholar] [CrossRef]
- Coxon, C. Drivers of Obesity? Characterising Biopsychological and Environmental Factors Associated with Overeating. Ph.D. Thesis, University of Roehampton, London, UK, 2021. [Google Scholar]
- Stinson, E.J.; Votruba, S.B.; Venti, C.; Perez, M.; Krakoff, J.; Gluck, M.E. Food Insecurity Is Associated with Maladaptive Eating Behaviors and Objectively Measured Overeating. Obesity 2018, 26, 1841–1848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romieu, I.; Dossus, L.; Barquera, S.; Blottière, H.M.; Franks, P.W.; Gunter, M.; Hwalla, N.; Hursting, S.D.; Leitzmann, M.; Margetts, B.; et al. Energy Balance and Obesity: What Are the Main Drivers? Cancer Causes Control 2017, 28, 247–258. [Google Scholar] [CrossRef] [Green Version]
- Omar, H.; Omar, A.; Muhammed, A.; Elderbi, M. Energy Drinks Consumption and Awareness Among Secondary School Students in Benghazi-Libya. AlQalam J. Med. Appl. Sci. 2021, 4, 116–121. [Google Scholar]
- Von Philipsborn, P.; Stratil, J.M.; Burns, J.; Busert, L.K.; Pfadenhauer, L.M.; Polus, S.; Holzapfel, C.; Hauner, H.; Rehfuess, E. Environmental Interventions to Reduce the Consumption of Sugar-Sweetened Beverages and Their Effects on Health. Cochrane Database Syst. Rev. 2019, 2019, CD012292. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). WHO Urges Global Action to Curtail Consumption and Health Impacts of Sugary Drinks. Available online: https://www.who.int/news/item/11-10-2016-who-urges-global-action-to-curtail-consumption-and-health-impacts-of-sugary-drinks (accessed on 25 December 2021).
- Nikpartow, N.; Danyliw, A.D.; Whiting, S.J.; Lim, H.; Vatanparast, H. Fruit Drink Consumption Is Associated with Overweight and Obesity in Canadian Women. Can. J. Public Health. 2012, 103, 178–182. [Google Scholar] [CrossRef]
- Odegaard, A.O.; Koh, W.-P.; Arakawa, K.; Yu, M.C.; Pereira, M.A. Soft Drink and Juice Consumption and Risk of Physician-Diagnosed Incident Type 2 Diabetes: The Singapore Chinese Health Study. Am. J. Epidemiol. 2010, 171, 701–708. [Google Scholar] [CrossRef] [Green Version]
- Trumbo, P.R.; Rivers, C.R. Systematic Review of the Evidence for an Association between Sugar-Sweetened Beverage Consumption and Risk of Obesity. Nutr. Rev. 2014, 72, 566–574. [Google Scholar] [CrossRef] [Green Version]
- Woodward-Lopez, G.; Gosliner, W.; Samuels, S.E.; Craypo, L.; Kao, J.; Crawford, P.B. Lessons Learned from Evaluations of California’s Statewide School Nutrition Standards. Am. J. Public Health. 2010, 100, 2137–2145. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Increasing Fruit and Vegetable Consumption to Reduce the Risk of Non-Communicable Diseases. Available online: https://www.who.int/elena/titles/fruit_vegetables_ncds/en/ (accessed on 26 December 2021).
- Public Health England, P.H.E. PHE Publishes Latest Data on Nation’s Diet. 2018. Available online: http://www.gov.uk/government/news/phe-publishes-latest-data-on-nations-diet (accessed on 17 October 2021).
- National Health Service (NHS). Five-a-Day Portion Sizes. 2018. Available online: http://www.nhs.uk/live-well/eat-well/5-a-day-portion-sizes/ (accessed on 20 October 2021).
- Swesi, R.; El-Anis, I.; Islam, M.M. Food Insecurity Coping Strategies in Conflict-Affected Libya. Dev. Pract. 2020, 30, 394–408. [Google Scholar] [CrossRef]
- Musaiger, A.O. Overweight and Obesity in Eastern Mediterranean Region: Prevalence and Possible Causes. J. Obes. 2011, 2011, 407237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Bkerat, M. Nutritional Beliefs and Practices of Arabic Speaking Middle Eastern Mothers. Ph.D. Thesis, University of Rhode Island, Kingston, RI, USA, 2019. [Google Scholar]
- Tayyem, R.; Hammad, S.; Allehdan, S.S.; Abdelrahim, D.; Djellouli, L.; Al-Asali, F. Exploring of Dietary Patterns, and Possible Association with Educational Level, among Jordanian Pregnant Women. Curr. Res. Nutr. Food Sci. 2021, 9, 31–39. [Google Scholar] [CrossRef]
- Sabzghabaee, A.M.; Mirmoghtadaee, P.; Mohammadi, M. Fruit and vegetable consumption among community dwelling elderly in an Iranian population. Int. J. Prev. Med. 2010, 1, 98–102. [Google Scholar] [PubMed]
- Charlton, K.; Kowal, P.; Soriano, M.; Williams, S.; Banks, E.; Vo, K.; Byles, J. Fruit and Vegetable Intake and Body Mass Index in a Large Sample of Middle-Aged Australian Men and Women. Nutrients 2014, 6, 2305–2319. [Google Scholar] [CrossRef] [Green Version]
- Moradi-Lakeh, M.; El Bcheraoui, C.; Afshin, A.; Daoud, F.; AlMazroa, M.A.; Al Saeedi, M.; Basulaiman, M.; Memish, Z.A.; Al Rabeeah, A.A.; Mokdad, A.H. Diet in Saudi Arabia: Findings from a Nationally Representative Survey. Public Health Nutr. 2016, 20, 1075–1081. [Google Scholar] [CrossRef] [Green Version]
- Azagba, S.; Sharaf, M.F. Fruit and Vegetable Consumption and Body Mass Index. J. Prim. Care Community Health 2012, 3, 210–220. [Google Scholar] [CrossRef]
- Heo, M.; Kim, R.S.; Wylie-Rosett, J.; Allison, D.B.; Heymsfield, S.B.; Faith, M.S. Inverse Association between Fruit and Vegetable Intake and BMI Even after Controlling for Demographic, Socioeconomic and Lifestyle Factors. Obes. Facts 2011, 4, 449–455. [Google Scholar] [CrossRef] [Green Version]
- Nour, M.; Lutze, S.; Grech, A.; Allman-Farinelli, M. The Relationship between Vegetable Intake and Weight Outcomes: A Systematic Review of Cohort Studies. Nutrients 2018, 10, 1626. [Google Scholar] [CrossRef] [Green Version]
- Ham, E.; Kim, H.-J. Evaluation of Fruit Intake and Its Relation to Body Mass Index of Adolescents. Clin. Nutr. Res. 2014, 3, 126–133. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.A.; Moore, L.V.; Galuska, D.; Wright, A.P.; Harris, D.; Grummer-Strawn, L.M.; Merlo, C.L.; Nihiser, A.J.; Rhodes, D.G. Vital signs: Fruit and vegetable intake among children—United States, 2003–2010. Morb. Mortal. Wkly. Rep. (MMWR) 2014, 63, 671–676. [Google Scholar]
- Godoy-Izquierdo, D.; Ogallar, A.; Lara, R.; Rodríguez-Tadeo, A.; Arbinaga, F. Association of a Mediterranean Diet and Fruit and Vegetable Consumption with Subjective Well-Being among Adults with Overweight and Obesity. Nutrients 2021, 13, 1342. [Google Scholar] [CrossRef]
- Watanabe, Y.; Saito, I.; Henmi, I.; Yoshimura, K.; Maruyama, K.; Yamauchi, K.; Matsuo, T.; Kato, T.; Tanigawa, T.; Kishida, T.; et al. Skipping Breakfast Is Correlated with Obesity. J. Rural Med. 2014, 9, 51–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akbarzade, Z.; Mohammadpour, S.; Djafarian, K.; Clark, C.C.; Ghorbaninejad, P.; Mohtashami, M.; Shab-Bidar, S. Breakfast-Based Dietary Patterns and Obesity in Tehranian Adults. Int. J. Obes. Relat. Metab. Disord. 2020, 29, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Guinter, M.A.; Park, Y.-M.; Steck, S.E.; Sandler, D.P. Day-to-Day Regularity in Breakfast Consumption Is Associated with Weight Status in a Prospective Cohort of Women. Int. J. Obes. 2019, 44, 186–194. [Google Scholar] [CrossRef]
- Ma, X.; Chen, Q.; Pu, Y.; Guo, M.; Jiang, Z.; Huang, W.; Long, Y.; Xu, Y. Skipping Breakfast Is Associated with Overweight and Obesity: A Systematic Review and Meta-Analysis. Obes. Res. Clin. Pract. 2020, 14, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Alhilabi, H.S.; Payne, A. The Impact of Skipping Breakfast on the Body Weight of Children and Young People in Saudi Arabia; a Systematic Review. Arab. J. Nutr. Exerc. (AJNE) 2018, 3, 67–104. [Google Scholar] [CrossRef]
- Wicherski, J.; Schlesinger, S.; Fischer, F. Association between Breakfast Skipping and Body Weight—a Systematic Review and Meta-Analysis of Observational Longitudinal Studies. Nutrients 2021, 13, 272. [Google Scholar] [CrossRef]
- Zanella, P.B. Highlights about the Association of Health and Skipping Breakfast in Adolescents and Adults. Br. J. Nutr. 2021, 126, 276–284. [Google Scholar] [CrossRef]
- Salehi, Z. Cultural Factors Related to the Obesity Epidemic. Obesity 2020, 141–154. [Google Scholar] [CrossRef]
- Benton, D. Portion Size: What We Know and What We Need to Know. Crit. Rev. Food Sci. Nutr. 2015, 55, 988–1004. [Google Scholar] [CrossRef] [Green Version]
- Nurdeng, D. Lawful and Unlawful Foods in Islamic Law Focus on Islamic Medical and Ethical Aspects. Int. Food Res. J. 2009, 16, 469–478. [Google Scholar]
- Aleshaiwi, A.; Harries, T. A Step in the Journey to Food Waste: How and Why Mealtime Surpluses Become Unwanted. Appetite 2021, 158, 105040. [Google Scholar] [CrossRef] [PubMed]
- Rippin, H.L.; Hutchinson, J.; Jewell, J.; Breda, J.J.; Cade, J.E. Portion Size of Energy-Dense Foods in French and UK Adults by BMI Status: Is There an Association between Portion Size and BMI? Nutrients 2019, 11, 12. [Google Scholar] [CrossRef] [Green Version]
- Higgins, K.; Hudson, J.; Mattes, R.; Gunaratna, N.; McGowon, B.; Hunter, S.; Braun, E.; Reister, E.; Cheon, E.; Wang, Y.; et al. Systematic Review and Meta-Analysis of the Effect of Portion Size and Ingestive Frequency on Energy Intake and Body Weight among Adults in Randomized Controlled Trials (P08-007-19). Curr. Dev. Nutr. 2019, 3, nzz044-P08. [Google Scholar] [CrossRef]
- Zangirolami-Raimundo, J.; Echeimberg, J.D.; Leone, C. Research Methodology Topics: Cross-Sectional Studies. J. Hum. Growth Dev. 2018, 28, 356–360. [Google Scholar] [CrossRef] [Green Version]
| Variable | Variable Recoding into Two Categories for Binary Regression Analysis |
|---|---|
| Marital Status | Single: Never married. Married: Married, divorced, separated, and widowed. |
| Level of education | Low Level: No formal schooling, less than primary school and primary school completed Moderate level: Secondary school and high school completed. High level: College/university completed. Post-graduate degree. |
| Occupation | Employed: Government employee, non-government employee, self-employed Unemployed: retired, housework, unemployed (able to work) and unemployed |
| Income (Libyan Dinar = ½ Pound) | Low income: <500 and 500–999. Moderate income: 100–1999 and 2000–2999. High income: 3000–3999 and ≥4000 |
| Fast-food consumption | Infrequent fast-food consumption in a day: ≤1 time. Excessive consumption of fast food in a day: ≥2 times. Infrequent fast-food consumption in a week: ≤4 times. Excessive consumption of fast food in a week: ≥5 times. |
| SSBs consumption | Infrequent SSBs consumption in a day: ≤1 time. Excessive SSBs consumption in a day: ≥2 times. Infrequent SSBs consumption in a week: ≤6 times. Excessive SSBs consumption in a week: >6 times. |
| Fruits and vegetable Consumption | Inadequate fruits and vegetables intake in a day: ≤3 times. Adequate fruits and vegetable intake in a day: >3 times. Inadequate fruits and vegetables intake in a week: ≤3 times. Adequate fruits and vegetable intake in a week: >3 times. |
| Skipping breakfast | A high frequency of skipping breakfast every day on a daily basis A high frequency of skipping breakfast in a week: >3 times. |
| Consumption large food portion sizes at one sitting | Never and rarely large FPS consumed at one sitting Occasionally and always large FPS consumed at one sitting |
| The dichotomous outcome of obesity (BMI) | Not obese (BMI < 30 kg/m2) Obese (BMI ≥ 30 kg/m2) |
| Demographic and Socio-Economic Characteristics | Female (F) n (%) | Male (M) n (%) | Total n (%) |
|---|---|---|---|
| Gender | 253 (63) | 148 (37) | 401 (100) |
| Age | |||
| 20–29 | 51 (20) | 27 (18) | 78 (19) |
| 30–39 | 56 (22) | 27 (18) | 83 (21) |
| 40–49 | 78 (31) | 37 (25) | 115 (29) |
| 50–59 | 32 (13) | 18 (12) | 50 (12) |
| 60–65 | 36 (14) | 39 (26) | 75 (19) |
| Marital Status | |||
| Single | 85 (33.6) | 47 (31.8) | 132 (32.9) |
| Married | 152 (60) | 88 (59.5) | 240 (59.9) |
| Divorced | 10 (4) | 6 (4.1) | 16 (4) |
| Widowed | 5 (2) | 2 (1.4) | 7 (1.7) |
| Separated | 1 (0.4) | 5 (3.4) | 6 (1.5) |
| Racial group | |||
| Arabic | 210 (83) | 129 (87.2) | 339 (84.6) |
| Berbers ‘Imazighen’ | 28 (11.1) | 15 (10.1) | 43 (10.7) |
| Toubou | 15 (5.9) | 4 (2.7) | 19 (4.7) |
| Level of education: | |||
| No formal schooling | 17 (6.7) | 13 (8.8) | 30 (7.5) |
| Less than primary school | 16 (6.3) | 14 (9.5) | 30 (7.5) |
| Primary school completed | 12 (4.7) | 5 (3.4) | 17 (4.2) |
| Secondary school completed | 45 (17.8) | 20 (13.5) | 65 (16.2) |
| High school completed | 32 (12.6) | 21 (14.2) | 53 (13.2) |
| College/university completed | 98 (38.7) | 57 (38.5) | 155 (38.7) |
| Post graduate degree | 33 (13) | 18 (12.2) | 51 (12.7) |
| Occupation | |||
| Government employee | 116 (45.8) | 64 (43.2) | 180 (44.9) |
| Non-government employee | 22 (8.7) | 24 (16.2) | 46 (11.5) |
| Self-employed | 32 (12.6) | 15 (10.1) | 47 (11.7) |
| Non-paid | 20 (7.9) | 16 (10.8) | 36 (9) |
| Student | 1 (0.4) | 1 (0.7) | 2 (0.5) |
| Housework | 27 (10.7) | 10 (6.8) | 37 (9.2) |
| Retired | 2 (.8) | 1 (0.7) | 3 (0.7) |
| Unemployed (able to work) | 27 (10.7) | 17 (11.5) | 44 (11) |
| Unemployed (unable to work) | 6 (2.4) | 0 (0) | 6 (1.5) |
| Monthly Income: “(LYD)” * | |||
| <500 | 6 (2.4) | 5 (3.4) | 11 (2.7) |
| 500–999 | 48 (19) | 38 (25.7) | 86 (21.4) |
| 1000–1999 | 19 (7.5) | 11 (7.4) | 30 (7.5) |
| 2000–2999 | 56 (22.1) | 17 (11.5) | 73 (18.2) |
| 3000–3999 | 100 (39.5) | 59 (39.9) | 159 (39.7) |
| ≥4000 | 24 (9.5) | 18 (12) | 42 (10.5) |
| Anthropometric measurements | Female Mean (±SD) | Male Mean (±SD) | Participants Mean (±SD) |
| BMI values (kg/m2) | 30.12 (±6.54) | 28.50 (±5.40) | 29.52 (±6.19) |
| Visceral Fat Rating (1–12) | 10.65 (±4.2) | 10.04 (±3.9) | 10.42 (±4.1) |
| Body fat % | 34.24 (±9.51) | 27.01 (±7.31) | 31.57 (±9.42) |
| Three weight status categories (BMI categories) | Female N (%) | Male N (%) | Prevalence of overweight and obesity Mean (±SD) |
| Normal weight (BMI = 18.5–24.9 kg/m2) | 50 (33.8) | 49 (19.4) | 99 (24.7) |
| Overweight (BMI = 25–29.9 kg/m2) | 48 (32.4) | 84 (33.2) | 132 (32.9) |
| Obese (BMI ≥ 30 kg/m2) | 50 (33.8) | 120 (47.4) | 170 (42.4) |
| Unhealthy Eating Habits | Mean (±SD) TIMES/a Typical Day | Mean (±SD) Times/a Typical Week | Spearman’s Rank Test Value (rho) | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | |||
| The amount of fast food intake | 1.23 (±0.7) | 1.46 (±0.8) | 1.37 (±0.8) | 5.51 (±2.9) | 5.62 (±3.1) | 5.54 (±3.1) | 0.440 | 0.000 ** |
| The amount of sugar sweetened beverages intake | 3.0 (±.25) | 3.5 (±0.5) | 3.15 (±1.2) | 10.18 (±1.5) | 11.55 (±1.35) | 11.68 (±1.23) | 0.467 | 0.000 ** |
| The amount of vegetable and fruit intake | 2.47 (±1.3) | 2.57 (±1.1) | 2.53 (±1.2) | 10.33 (±1.4) | 9.17 (±1.9) | 10.1 (±1.6) | 0.081 | 0.107 |
| The number of times skipping breakfast | 0.5 (±0.6) | 0.6 (±0.6) | 0.5 (±0.3) | 3.33 (±1.9) | 3.9 (±1.7) | 3.18 (±1.83) | −0.506 | 0.000 ** |
| Consumption of a full large portion size meal served at one sitting | Male (M) N (%) | Female (F) N (%) | Total N (%) | Chi-square (X2) | p-Value | |||
| Always | 71 (48) | 95 (37.5) | 166 (41.4) | 13.8 | 0.032 * | |||
| Occasionally | 26 (17.6) | 47 (18.6) | 73 (18.2) | |||||
| Rarely | 21 (14.2) | 46 (18.2) | 67 (16.7) | |||||
| Never | 30 (20.3) | 65 (25.7) | 95 (23.7) | |||||
| Variables for Unhealthy Eating Habits | Sig. | Exp(B) | 95% CI for EXP(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| 1. The amount of fast-food intake in a typical day. | 0.042 * | 3.14 | 1.04 | 9.46 |
| 2. The amount of fast-food intake in a typical week. | 0.000 ** | 6.83 | 2.59 | 12.01 |
| 3. The amount of sugar-sweetened beverages intake in a typical day. | 0.316 | .61 | 0.23 | 1.61 |
| 4. The amount of sugar-sweetened beverages intake in a typical week. | 0.051 | 2.66 | 0.99 | 7.10 |
| 5. The amount of vegetable and fruit intake in a typical day. | 0.510 | 1.42 | 0.50 | 4.05 |
| 6. The amount of vegetable and fruit intake in a typical week. | 0.339 | 0.63 | 0.240 | 1.63 |
| 7. The number of times skipping breakfast in a typical day. | 0.03 * | 0.67 | 0.03 | 0.25 |
| 8. The number of times skipping breakfast in a typical week. | 0.000 ** | 0.08 | 0.45 | 0.67 |
| 9. Consumption of a full large portion size meal, served at one sitting. | 0.000 ** | 4.78 | 1.84 | 12.46 |
| Variables for Unhealthy Eating Habits | Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Sig p-Value | Odds Ratio (OR) | 95% CI for Exp(B) | Sig p-Value | Odds Ratio (OR) | 95% CI for Exp(B) | ||||
| Lower | Upper | Lower | Upper | ||||||
| 0.05 * | 0.015 | 0.000 | 1.07 | 0.01 * | 11.7 | 1.65 | 83.02 | |
| 0.91 | 0.86 | 0.07 | 10.40 | 0.37 | 0.54 | 0.13 | 2.11 | |
| 0.82 | 1.91 | 0.01 | 447.40 | 0.50 | 2.45 | 0.18 | 32.56 | |
| 0.04 * | 0.03 | 0.001 | 0.79 | 0.001 ** | 0.05 | 0.01 | 0.30 | |
| 0.03 * | 14.1 | 1.53 | 35.50 | 0.19 | 2.73 | 0.61 | 12.17 | |
| 0.416 | 1.68 | 0.48 | 5.92 | 0.59 | 1.22 | 0.59 | 2.55 | |
| 0.047 * | 2.52 | 4.04 | 12.32 | 0.043 | 2.14 | 3.32 | 11.12 | |
| 0.014 * | 4.65 | 1.04 | 9.46 | 0.002 ** | 5.50 | 1.88 | 16.11 | |
| 0.094 | 0.089 | 0.01 | 1.52 | 0.810 | 0.87 | 0.298 | 2.61 | |
| 0.452 | 2.53 | 0.22 | 28.61 | 0.013 * | 4.02 | 1.35 | 11.99 | |
| 0.408 | 2.86 | 0.24 | 34.50 | 0.580 | 0.72 | 0.23 | 2.30 | |
| 0.379 | 0.34 | 0.03 | 3.83 | 0.538 | 0.72 | 0.25 | 2.08 | |
| 0.042 * | 0.02 | 0.01 | 0.77 | 0.000 ** | 0.11 | 0.03 | 0.43 | |
| 0.011 * | 0.03 | 0.01 | 0.24 | 0.005 ** | 0.21 | 0.08 | 0.63 | |
| 0.027 * | 19.5 | 1.41 | 27.74 | 0.024 * | 3.40 | 1.18 | 9.84 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lemamsha, H.; Randhawa, G.; Papadopoulos, C. Investigating the Association between Unhealthy Dietary Habits and Obesity among Libyan Adults. Int. J. Environ. Res. Public Health 2022, 19, 1076. https://doi.org/10.3390/ijerph19031076
Lemamsha H, Randhawa G, Papadopoulos C. Investigating the Association between Unhealthy Dietary Habits and Obesity among Libyan Adults. International Journal of Environmental Research and Public Health. 2022; 19(3):1076. https://doi.org/10.3390/ijerph19031076
Chicago/Turabian StyleLemamsha, Hamdi, Gurch Randhawa, and Chris Papadopoulos. 2022. "Investigating the Association between Unhealthy Dietary Habits and Obesity among Libyan Adults" International Journal of Environmental Research and Public Health 19, no. 3: 1076. https://doi.org/10.3390/ijerph19031076






