Abstract
Retrograde intrarenal surgery (RIRS) is an innovative and effective method of kidney stones treatment, as it had great influence on the development of endoscopy in urology. The increasing prevalence of urolithiasis together with the rapid development of endourology leads to a rise in the number of procedures related to the disease. Flexible ureteroscopy is constantly being improved, especially regarding the effectiveness and safety of the procedure. The purpose of this study is to evaluate intraoperative and early post-operative complications of RIRS in the treatment of kidney stones. A retrospective analysis of medical records was performed. A series was comprised of 207 consecutive operations performed from 2017 to 2020. Complications occurred in 19.3% (n = 40) of patients. Occurrence according to the Clavien-Dindo scale was: 11.1% for grade I, 5.8% for grade II and 2.4% for grade IV. Infectious complications included SIRS (5.3%, n = 11) and sepsis (2.4%, n = 5). Statistical analysis revealed a correlation between acute post-operative infections and positive midstream urine culture, history of chronic or recurrent urinary tract infections, and increased body mass index (BMI). Furthermore, a significant correlation was observed between pain requiring the use of opioids with BMI over 25. Consequently, history of urinary tract infections, positive pre-operative urine culture, and increased BMI are considered risk factors and require appropriate management.
Keywords:
RIRS; fURS; ureteroscopy; urolithiasis; kidney stone; complications; infection; UTI; sepsis 1. Introduction
Flexible ureteroscope (fURS) was used for the first time in 1983 by Bagley and collaborators, soon after the development of the modern semirigid ureteroscope in 1980 by Perez-Castro. However, major technological improvements have been made in the last two decades [1]. Although retrograde intrarenal surgery (RIRS) is a relatively new method of kidney stones treatment, it had a tremendous impact on the advancement of minimally invasive surgery in urology [2]. The paramount advantage of flexible scope over semirigid is the ability to inspect the whole kidney collecting system, enabling the opportunity to diagnose and treat not only stones, but also urothelial cancer [3]. The increasing prevalence of urolithiasis together with the rapid development of endourology leads to a rise in the number of procedures related to the disease [4]. European Association of Urology (EAU) recommends RIRS or shock wave lithotripsy (SWL) as first line treatment option for kidney stones of diameter up to 20 mm and second line treatment of stones over 20 mm [5]. Stones larger than 20 mm are qualified for percutaneous nephrolithotripsy (PCNL) mainly due to better irrigation fluid outflow, protecting from septic complications, and shortening operation time [6]. Small kidney stones of diameter less than 10 mm or medium size located in the lower pole of the kidney should primarily be treated with SWL.
Flexible ureteroscopy may be performed in various manners [7]. A typical technique was implemented by the authors: first, a safety guidewire is inserted into the ureter under fluoroscopy, followed by a hydrophilic access sheath, reaching to the upper ureter or uretero-pelvic junction, then the fURS is advanced to the kidney pelvis. Diagnostic ureteroscopy or prior double-J stenting may facilitate access to the ureter. Insertion of ureteral access sheath may cause ureteral trauma, however, pre-stenting lowers that risk [8]. Then ureteroscope is advanced to the kidney pelvis where lithotripsy can be performed, preferably using holmium:yttrium-aluminium-garnet (Ho:YAG) laser [9]. Stone disintegration types include dusting, which is used to produce powder of tiny fragments usually smaller than 2 mm, that are flushed spontaneously through the urinary tract; fragmentation, resulting in fragments that are removed with a basket [10]. After stone removal access sheath is withdrawn and a new double-J stent may be installed, if considered necessary.
Different types of lasers were implemented for endoscopic lithotripsy. Ho:YAG is the most commonly used device, in which energy ranges from 0.2 J to 6 J and 30 W power is considered a standard, however, merged generators can reach as high as 140 W [11]. Improvement made in recent years allowed for wide application of Ho:YAG laser, not only in urolithiasis, but also in prostate enucleation. Another advancement is the invention of the Moses effect, namely the division of laser pulse in two consecutive blasts creating a corridor of vapor in a fluid. The first forms a low attenuation cavity for the final energy impulse, therefore minimising power loss before hitting the target. As a result Ho:YAG amplified with Moses effect has a power of 120 W and frequency 5 to 80 Hz [12,13]. Recently introduced thulium fibre laser (TFL) is expected to revolutionise endourology by the ability to achieve a maximum power of 500 W, on average 60 W, alongside a very wide range of energy from 0.025 J to 6 J [14,15]. High frequency of impulses is an additional advantage of this technology, where peak values can reach 2400 Hz and regular dusting with an average frequency between 100 Hz to 200 Hz was enough to increase efficacy, without compromising complication rates [16,17]. The combination of these two features, high frequency, and low energy, facilitates major advances in dusting technique, which may produce colloid of particles smaller than Ho:YAG laser. Consequently, the time of lithotripsy can be reduced by half, in comparison to commonly used holium lasers. In addition, TFL has the smallest diameter, requiring minimal working channel, and enables the bending of endourological instruments [18,19,20]. A different laser incorporating this chemical element is Thulium: Yttrium-Aluminium-Garnet, however still being under investigation. This technology generates 120 W power, energy 0.1–3 J, and high frequency impulses up to 200 Hz, yet promises a low retropulsion effect due to long energy impulses [21,22].
EAU guidelines report an overall ureteroscopy complication rate of 9–25% [5]. Most of them are minor incidents, thus the procedure is generally considered to be safe. Nevertheless, major complications still occur, those of paramount importance are: acute urinary tract infection (UTI) and sepsis, ureteral avulsion or perforation, stricture of the ureter, vascular or enteric fistula formation, bleeding, cardiovascular events (i.e., stroke, pulmonary embolism), and death. Sepsis is defined as the dysregulated immune host response to infection triggered by simultaneous activation of proinflammatory cytokines, mainly tumour necrosis factor-α (TNF-α), interleukin (IL) 1 and 6, which are insufficiently suppressed by anti-inflammatory mediators including IL-4, IL-9, IL-10, epinephrine, transforming growth factor-β, soluble TNF-α receptors [23,24]. Sepsis mortality rates vary from 17.3% in general population and rise to 35.5%, if multi-organ dysfunction occurs [25]. Furthermore, intensive care generates a high cost of treatment causing a substantial financial burden for the healthcare system [26]. Emerging microbial resistance, especially the selection of new multi-drug resistant bacteria, decreases the effectiveness of antibiotic prophylaxis and empirical treatment. Eventually, it is estimated that 25% of patients with healthcare associated UTI develop sepsis [27]. Urosepsis is the most serious and possibly life-threatening complication of ureteroscopy [28,29].
Endoscopy of the upper urinary tract offers minimally invasive access via a natural orifice, however, requires caution and vigilance since ureteral tissues are very susceptible to injury [30,31]. Common technical mistakes are forceful manipulation of an instrument and accidental laser activation. These may lead to a mucosal lesion, perforation, or even avulsion of the ureter [8,32]. The trauma of the ureter frequently results in the formation of a false route or stricture, which warrants subsequent obstacles in the insertion of auxiliary equipment (guidewire, double-J catheter, access sheath). Perforated ureter, kidney pelvis, or ruptured calyx causes leakage of urine to the abdominal cavity, which may be a source of life-threatening infection. Management encompasses immediate repair or urinary drainage via nephrostomy or double-J catheter and delayed reconstruction if necessary. The main precautions in the prevention of upper tract injuries are the careful handling of equipment with subtle movements. Proper adjustment of instrument size is essential, further advancement of the ureteroscope, access sheath, guidewire, ureteral dilators cannot be forceful [33,34]. Stone extraction baskets and laser beams must only be employed under direct and unobscured vision [35].
The aim of this study is to evaluate the most significant peri-operative and early post-operative complications of retrograde intrarenal surgery in the management of urolithiasis. Another goal is to identify vulnerable patients at high risk of complications, who require special consideration and treatment strategy.
2. Materials and Methods
Retrospective analysis of consecutive medical records was performed. The data acquisition period spans from 2017 to 2020. Qualification criteria for RIRS were: single or multiple kidney stones, diameter ranging from 5 to 25 mm, and age over 18 years. Operations without lithotripsy were excluded, these represent mainly Randall’s plaques or calcifications not connected with kidney pelvis and ablation due to upper tract urothelial cancer. The procedure was carried out only on one side at a time. Many patients were referred after a series of unsuccessful SWL or because of multiple stones. The stone burden was evaluated by computed tomography and updated on ultrasound if shock wave treatment was applied. Double-J catheter was routinely installed, usually 2 weeks before the procedure. It was skipped in patients with a history of stent intolerance. In case of upsetting dysuria, bothersome haematuria, or very high intensity of physical work resulting in abdominal stent-related symptoms, the stent was removed. Mid-stream urine culture was taken prior to double-J insertion and routine antibiotic prophylaxis, or a full course of targeted therapy was administered according to reported bacterial susceptibility. Then the operation was planned on the last days of antibiotic treatment. Ciprofloxacin was first line prophylactic antibiotic until 2019, however, after European Medicines Agency (EMA) announcement was superseded by trimethoprim-sulfamethoxazole [36]. The vast majority of cases were completed by two urologists experienced in this surgical method, assisted by doctors in specialty training. Spinal anaesthesia was the preferred method of analgesia. Ureteral access sheath was used where possible. The following ureteroscopes were used in operations: fiberoptic Cobra Vision (Richard Wolf, Germany), FLEX-X2S (Karl Storz, Germany), and single-use digital Uscope PU3022, Pusen Medical Technology, Zhuhai, China). Lithotripsy was performed using a 30 W Ho:YAG laser with irrigation fluid being pumped manually. For safety reasons, operation time was limited to 60 min. Complications were classified according to Clavien–Dindo scale, which was adapted to evaluate endourological procedures [37]. Post-operative complications analysis comprised of occurrence of SIRS (systemic inflammatory response syndrome) and sepsis, nausea or vomiting, use of opioids, haematuria, mortality. The fever threshold was 38 °C. SIRS was defined by two or more of the following criteria: body temperature less than 36 °C or higher than 38 °C, heart rate greater than 90 beats per minute, a respiratory rate greater than 20 breaths per minute, and white cell count > 12,000/mm3 or <4000/mm3. Sepsis was defined as acute infection leading to organ dysfunction evaluated in biochemical parameters, elevated inflammatory markers, or Sequential Organ Failure Assessment (SOFA) score of minimum 2 points or at least 2 quickSOFA criteria: respiratory rate of 22 beats per minute or greater, altered mentation, or systolic blood pressure of 100 mm Hg or less [38]. Nausea/vomiting was identified by the use of antiemetic drugs. Follow-up encompasses events during hospitalisation. The success rate was based on endoscopy, ultrasound, and kidney-ureter-bladder X-ray, if useful. An evaluation was done on discharge day and defined as the absence of deposits of diameter up to 2 mm. 1. Post-operative pain was managed according to the World Health Organisation analgesic ladder. In the first step, all patients were administered paracetamol, 3 to 4 g daily. In the second step non-steroid anti-inflammatory drugs were given, usually ketoprofen or metamizole. At last tramadol, oxycodone or morphine was used to ease pain, the choice of medicine was at the discretion of the on-call physician. Sepsis was managed with empirical ceftriaxone or meropenem, fluids, and vasopressors in hemodynamically unstable patients. Intensive care was provided in the urology department with anaesthetists’ co-operation, since none of the patients required mechanical ventilation.
A univariate analysis was performed to compare the adverse events group with an uneventful group (Wilcoxon–Mann–Whitney-Test). A logistic regression analysis including patient’s age, body mass index (BMI), comorbidities, preoperative urine culture, stone size, and operation time as possible risk factors was completed using IBM SPSS Statistics Version 21 (International Business Machines Corporation, Armonk, New York, NY, USA). p < 0.05 was considered to indicate statistical significance.
3. Results
Overall, 207 records were included. The median age in the examined group was 58 years (SD = 13.7 years). 73% of patients were overweight, whereas the median BMI in the group was 27.8 (SD = 5.5). Study group characteristics are presented in Table 1.

Table 1.
Study group characteristics.
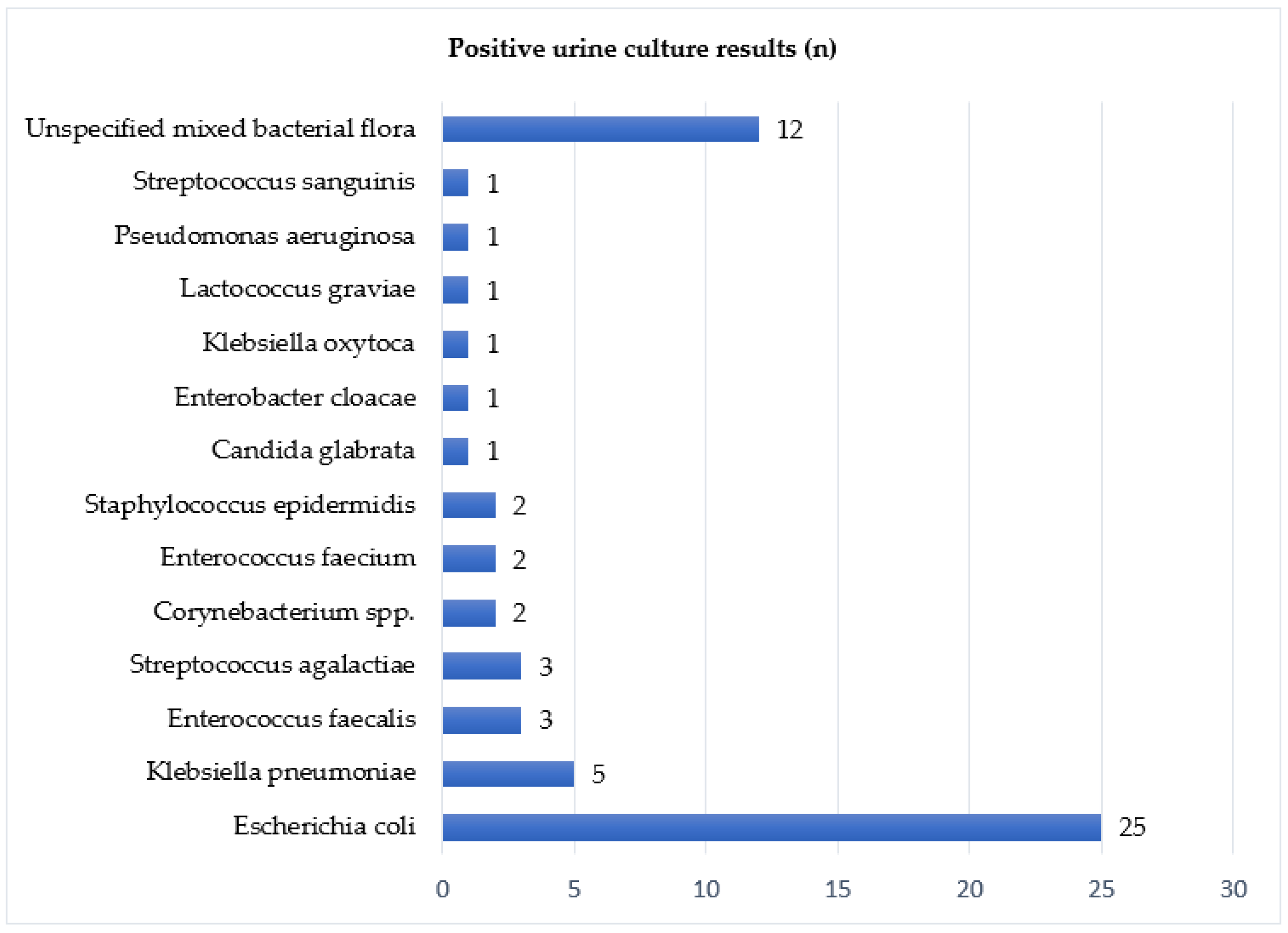
In order to facilitate ureteral access, a vast majority of patients (79%) were pre-stented with a double-J catheter before operation. Urine culture was taken routinely, and results were available for 88.4% of analysed records. Microbial growth was positive in 32.8% of samples. The most prevalent bacterium was Escherichia coli (41.7%), followed by miscellaneous bacterial flora (20%) and Klebsiella pneumoniae (8%). Table 2 contains urine culture results. Figure 1 presents a detailed incidence of bacterial strains.

Table 2.
Mid-stream urine culture results.
Figure 1.
Positive urine culture results.
Although EAU recommends flexible ureteroscopy for a maximum of 20 mm stones, indications were widened in two cases of slightly larger calculi i.e., 23 and 25 mm. These records were also included in order to follow the consecutive series. Stones from 5 to 15 mm dominate the group (88%), therefore the median size of stones was 10 mm. The median time of surgery was 45 min (SD = 15 min), and the 60 min threshold was intentionally minded. Usually, patients were admitted one day before the procedure and discharged the next day after surgery, if not presenting any signs of infection. As result, the average length of stay was two days (SD 1.7).
Overall post-operative complications occurred in 19.3% (n = 40) of patients. Classification according to Clavien-Dindo scale is shown in Table 3. The most vital were infectious complications i.e., SIRS (5.8%, n = 12) and sepsis (2.4%, n = 5).

Table 3.
Results and description of surgical complications according to Clavien-Dindo classification.
Statistical analysis revealed a significant correlation between that group and positive midstream urine culture (p < 0.01), as well as increased BMI and history of chronic or recurrent urinary tract infections (p < 0.01), ischemic heart disease (p < 0.01), and diabetes (p < 0.01). Neither operation time, nor stone size differentiated the occurrence of post-operative infection. Table 4 shows statistical significance of SIRS/sepsis risk factors. Although the size of the largest stone was irrelevant at 0.05 significance level, it was found significant at a level of 0.1 (p = 0.1). Incidence of nausea and vomiting (8.2%; n = 17) was statistically associated with BMI over 25 (p < 0.01), however was not influenced by operation time, nor the largest stone dimension. Pain requiring the use of opioids (i.e., tramadol, morphine, oxycodone) occurred in 4.8% of patients (n = 10). The research found a significant correlation of severe pain with increased BMI (p < 0.01), without association with length of operation or stone size. Clinically important intra- and post-operative hematuria occurred in one patient but did not require surgical intervention or transfusion. Neither reoperation nor deadly complications occurred. Complete lithotripsy was achieved in 80.6% of procedures.

Table 4.
Parameters affecting occurrence of SIRS/sepsis.
Table 5 presents the estimated variance-covariance matrix and estimated correlation matrix is shown in Table 6. Most of the correlation between the variables is negligible or very small, which proves that the occurrence of given variables does not depend on the occurrence of another variable. Moderately significant relationships were found between the size of the largest deposit and the occurrence of UTI or diabetes, which indicates that deposits were greater in people with UTI or diabetes. BMI and UTI are correlated: in people with UTI, the BMI was on average higher. Finally, patients with diabetes are prone to UTI and urine culture was more likely to be positive in people with diabetes.

Table 5.
Estimated variance-covariance matrix.

Table 6.
Estimated correlation matrix.
4. Discussion
Numerous studies aimed to assess common complications of ureteroscopy, both semirigid and flexible, to identify major or modifiable risk factors. Somani et al. in vast CORES URS Global Study conducted in 114 centres and involving 11,885 patients reported relatively low overall rate of complications (7.4%) and mortality (0.042%, n = 5), with only 3.0% of urinary tract infections (UTIs) [39]. Nevertheless, in that mixed group, the majority of ureteroscopies were semirigid, as most stones were located in the ureter, those in the kidney accounted for only 15.6% (n = 1852). Patients included in the CORES study who underwent retrograde intrarenal surgery for a single kidney stone were described by Skolariskos et al. Complication rates varied depending on the stone dimension, from 4.8% (n = 608) for stones less than 10 mm, 6.3% (n = 501) for stones 10–20 mm, reaching 9.3% (n = 54) for stones over 20 mm. The overall rate was 5.7%, in comparison to 19.3% in the presented analysis. Although this disparity could be striking, it may result from detailed reporting of minor events, such as pain and vomiting. This discrepancy lowers to 7.7% (5.8% and 2.4%, respectively) in the discussed study, whereas the incidence of serious infectious complications accounts for 3.6% (2.9% SIRS, 0.8% sepsis) in the research mentioned above.
Study sample comparable to this investigation, concentrating on 316 flexible ureteroscopies by Giusti et al. reported complications occurrence of 29.1%, meaningly higher than 19.3% found here. Nevertheless, the majority were minor events of Clavien-Dindo grade I in 17.4% (n = 55) and II in 9.5% (n = 30), with a very few grade III in 1.9% (n = 6) and grade IV in 1 patient (0.3%), without any of grade V [40]. Although the rates of class I (11.1%, n = 23) and II (5.8%, n = 12) in the presented research are lower, it may stem from the different clinical practices of medication usage, since these comprise of non-surgical management of complications. On the other hand, Berardinelli et al. in 377 RIRS observed 15.1% of adverse events, including 8.4% (n = 30) post-operative, which revealed even lower prevalence: grade I in 6.9% (n = 26), grade II in 0.5% (n = 2), grade III in 0.5% (n = 2) [41]. Similarly, a Swedish study of 486 mixed semirigid and flexible URS groups by Wagenius et al. described: grade I in 12.0% (n = 68), grade II in 6.5% (n = 7), grade III in 1.9% (n = 11) and grade IV in 0.2% (n = 1), which are comparable to the incidence of adverse events in the sample being discussed [42].
A recent systematic review by Chugh et al. states post-URS complications, both semirigid and flexible, in 7.9% (n = 1919), of which 3.9% (n = 972) were infectious, including sepsis in 0.51%, and 4% (n = 1147) were non-infectious. According to the Clavien-Dindo scale these were grade I in 5.3% (n = 1298), grade II in 1.1% (n = 275), grade III in 0.7% (n = 180), grade IV in 0.3% (n = 91), and grade V complications only in 0.0001% (n = 3) patients [43]. Major risk factors of UTI are positive preoperative urine culture, diabetes, female gender, indwelling ureteric stents, stone burden, and operation time [44,45,46]. Although women are more susceptible to urinary tract infections and subsequent recurrences, in the presented study female gender was found to be irrelevant regarding the occurrence of SIRS or sepsis [47,48].
Another research of 3298 standard URS by Southern et al. resulted in 6.9% of post-operative fever or SIRS, similar to a study by Baboudijan et al. where UTI occurred in 6.7% [49,50]. A large cohort analysed by Senocak et al. revealed that 22.1% of 492 patients had post-operative complications after fURS, in total infectious complications occurred in 8.5% [51]. The aforementioned rate is slightly higher than the group investigated herein (7.7%), however, this occurrence is considered comparable. In Berardinelli et al.’s research, infectious complications were recorded in 7.7% of patients, mainly consisting of fever in 4.4%, SIRS 1.7%, and sepsis in 0.7% [52]. In another paper, Blackmur et al. reported 7.4% urosepsis within 28 days after the operation and positive preoperative urine culture was significantly associated with post-operative urosepsis, despite the use of preoperative antibiotic treatment [53]. In the presented research midstream urine culture, together with a history of recurrent or chronic UTI, was confirmed as a risk factor for septic complications. Preoperative urine samples were positive in 68.7% of patients diagnosed with SIRS and sepsis, indicating asymptomatic bacteriuria. Targeted therapy was administered before the operation, without curative intention, rather that reduction of urinary microbiota. Regarding the presence of stones covered with biofilm, rapid recurrence after cessation of the antimicrobial agent was considered highly probable. Antibiotic treatment was continued after the operation and extended in the suspicion of sepsis, with the use of additional meropenem or third generation cephalosporins. Vigilance and rapid response to the development of systemic symptoms, confirmed by the rise of inflammation biomarkers (C-reactive protein or procalcitonin), resulted in a complete reduction of the mortality rate. Studies investigating the incidence of post-operative UTI in patients with a history of sepsis or pyelonephritis brought inconsistent results. On one hand, Youssef et al. found that elective ureteroscopy after successful management of sepsis was associated with a higher overall complication rate, prolonged hospital stay, and longer antibiotic administration [54]. On the other hand, in later studies, the previous acute infection did not escalate the risk of adverse events [55,56].
In the group being presented double-J catheter was inserted usually within two to four weeks before RIRS. Preoperative ureteral stenting decreased the rate of septic events in the group reported by Blackmur. Nevertheless, it was not confirmed in this group, since all patients diagnosed with sepsis were routinely pre-stented with adherence to standard protocol applied in the department. Sepsis rates are correlated with the duration of stent dwelling. Nevo et al. revealed that the presence of ureteral stent for one, two, three, and over three months elevated the risk of sepsis to 1, 4.9, 5.5, and 9.2%, respectively [57]. Clearly, it has been proven that the ureteric catheter should be kept as short as possible before ureteroscopy, preferably up to two weeks.
Ureteral access sheath was employed routinely to facilitate the outflow of irrigation fluid and minimise intrarenal pressure [58]. Reported pressure values range from 40 cm H2O to as high as 199 cm H2O during pumping. Implementation of ureteral access sheath could lower it to less than 30 H2O mm passive irrigation, yet may still reach 200 mm H2O when flushing [59]. Although the role of access sheath remains uncertain, the article by Traxer et al. supported its use to reduce the rate of infectious complications. Another cohort described by Geraghty et al. did not confirm that hypothesis in the treatment of renal stones over 20 mm diameter, however, indicated that high stone burden also increases the risk of sepsis [60]. Higher occurrence of post-operative fever or UTI in stones larger than 20 mm was confirmed by Skolarikos et al. since dimensions affect operation time and may prolong exposure to elevated intrarenal pressure [61].
Taking this into account at the stage of qualification for the procedure, a general prerequisite for the maximum size of 20 mm was made, with only a few exceptions, not exceeding 25 mm in the largest dimension. Consequently, in the investigated group stone size is not correlated with SIRS nor sepsis, which retrospectively validates sound qualification criteria. This finding reinforces recommended thresholds of acceptable stone burden. On top of that, dynamic technological progress in the construction of more powerful lasers and thinner scopes may mitigate known risk indicators and again move acknowledged limits much further.
The age of patients was found to have no impact on adverse events. Research in elderly patients has proven the safety of RIRS, with similar complication rates and results, as in younger patients [62]. Infectious adverse events in the analysed cohort were correlated with ischemic heart disease and diabetes, however, these comorbidities were mutually correlated, indicating that diabetes contributes to heart ischemia. Although the incidence of urinary tract infections is higher in diabetic patients, in other studies it was not a statistically relevant risk factor of SIRS or sepsis after flexible ureteroscopy [63]. Lately published research revealed that previous history of fluoroquinolones may also pose a threat of drug-resistant bacterial infection [64]. In addition, the albumin to globulin ratio can serve as an infection predictive factor, as it may indirectly reflect immune competence [65].
Significant post-operative haematuria resulting in prolonged hospital stay occurred in only 1 patient. The bleeding ceased after pharmacological treatment, without surgical intervention or blood transfusion. The possible sources of haemorrhage are mucosal injury of kidney pelvis, caused by stone fragments, or friction of access sheath against the wall of the ureter, still, these resolve spontaneously. Among available modalities of urinary stone treatment, flexible ureteroscopy in the only method acceptable in compromised coagulation and was proved safe with a reported bleeding rate of 4%, generally described as minor [66,67]. In comparison to perioperative blood loss and transfusions, RIRS presents a clear advantage over PCNL [68,69].
Opioids (i.e., tramadol, morphine, oxycodone) were administered when non-steroidal anti-inflammatory drugs (NSAIDs) did not sufficiently relieve symptoms. Post-operative pain requiring the use of opioids was recorded in 4.8% of patients, Oguz et al. found substantial pain in 18.4% after RIRS, whereas in the CROES study clinically noteworthy pain occurred very rarely (0.33%) [39]. The presence of symptoms was significantly correlated with increased BMI (p < 0.01), however, was not associated with operation time or stone burden, contrary to findings of Oguz et al. who pointed female gender, higher stone burden, and length of access sheath as contributing factors. Antiemetic medicines were given in 8.2%, usage was more frequent in overweight and obese patients, statistically associated with BMI over 25 (p < 0.01). In the CROES study, nausea and vomiting were less frequent (0.03%). Relatively higher incidence of mild complications in the discussed analysis might result from physicians’ susceptibility to pharmacological interventions. Evidence addressing the impact of obesity on post-operative pain and emesis in ureteroscopy is scarce, thus should require further investigation.
In the presented study increased BMI (over 25 kg/m2) was also found to be a risk factor of complications in general. Based on the CROES cohort Krambeck et al. reported a higher incidence of post-operative adverse events in underweight and extremely obese patients, along with the need for additional procedures [70]. Assumption can be made there may have been undiagnosed diabetes or improper fasting glucose in some patients with higher BMI, leading to immune suppression. There are also not yet clearly identified mechanisms of chronic inflammation in obese patients additionally jeopardising immunity. Despite relatively elevated perioperative risk and lower efficacy, ureteroscopy is considered safe in obese patients [71,72].
The occurrence of complications regarding the experience of urologists was evaluated by Komori et al. Study found that climbing the learning curve required a longer operation time and resulted in a lower stone-free rate, together with an increased risk of ureteral injury. Sufficient knowledge of the operation was estimated to be achieved after around one hundred procedures at a high-volume centre. It is noteworthy to state that the incidence of sepsis was unrelated to the surgeon’s experience and occurred at a similar rate [73].
All RIRS procedures analysed in this paper were planned, elective operations. Still, the need for expanding access to flexible ureteroscopy must be underlined, especially in order to avoid unnecessary readmissions, multiple shockwave therapy sessions, and further semirigid operations [74]. Constant improvement of single-use devices leads to gradual price decline and enhanced cost-effectiveness, especially in low-volume centres. Reusable scopes remain the best option for experienced operators, assuming a low damage rate and high durability of the instrument [75,76].
Having considered the limitations of the study, it should be noted that research was conducted retrospectively with a focus on perioperative complications, which occurred during the hospital stay. Furthermore, as long-term follow-up data was limited, lithotripsy effectiveness was based on endoscopic, ultrasound, and X-ray evaluation. The department serves as a stone centre for a wide area, thus the majority of patients received further control in remote practices, and data on long term follow-up was not substantial enough to draw statistical conclusions. Urine culture results were not included in 11.6% of analysed medical records. Application of Clavien–Dindo scale may not comprehend some self-limiting complications.
5. Conclusions
Treatment of kidney stones using flexible ureteroscopy is generally safe and effective, however, rare life-threatening complications may still occur. Significant risk factors for septic complications include a positive midstream urine culture, history of chronic or recurrent urinary tract infections, increased BMI, and diabetes. The research found a significant correlation of opioid pain treatment with an increased BMI. Careful qualification and consideration of risk factors in preparation for surgery minimises potential perioperative risks, therefore, midstream urine culture should be considered obligatory before flexible ureteroscopy.
Author Contributions
Conceptualization, J.M.R. and B.K.; methodology, J.M.R. and M.S.; validation, M.S., M.M.; formal analysis, M.M.; investigation, J.M.R., T.H., B.K. and K.B.; resources, K.B.; data curation, J.M.R. and T.H.; writing—original draft preparation, J.M.R.; writing—review and editing, T.H. and M.S.; visualization, J.M.R.; supervision, M.M.; project administration, M.M.; funding acquisition, M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was conducted within the EU-financed InterDoktorMen project (POWR.03.02.00-00-I027/16).
Institutional Review Board Statement
Ethical committee approval was not sought as anonymous and retrospective data was used in the study, without any prospective intervention in the treatment.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to healthcare facility policy.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Somani, B.K.; Aboumarzouk, O.; Srivastava, A.; Traxer, O. Flexible ureterorenoscopy: Tips and tricks. Urol. Ann. 2013, 5, 1–6. [Google Scholar] [CrossRef]
- Rodríguez-Monsalve Herrero, M.; Doizi, S.; Keller, E.X.; De Coninck, V.; Traxer, O. Retrograde intrarenal surgery: An expanding role in treatment of urolithiasis. Asian J. Urol. 2018, 5, 264–273. [Google Scholar] [CrossRef]
- Rouprêt, M.; Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Cowan, N.C.; Dominguez-Escrig, J.L.; Gontero, P.; Hugh Mostafid, A.; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur. Urol. 2021, 79, 62–79. [Google Scholar] [CrossRef]
- Rukin, N.J.; Siddiqui, Z.A.; Chedgy, E.; Somani, B.K. Trends in Upper Tract Stone Disease in England: Evidence from the Hospital Episodes Statistics Database. Urol. Int. 2017, 98, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Türk, C.; Petřík, A.; Sarica, K.; Seitz, C.; Skolarikos, A.; Straub, M.; Knoll, T. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur. Urol. 2016, 69, 475–482. [Google Scholar] [CrossRef]
- Kim, C.H.; Chung, D.Y.; Rha, K.H.; Lee, J.Y.; Lee, S.H. Effectiveness of Percutaneous Nephrolithotomy, Retrograde Intrarenal Surgery, and Extracorporeal Shock Wave Lithotripsy for Treatment of Renal Stones: A Systematic Review and Meta-Analysis. Medicina 2021, 57, 26. [Google Scholar] [CrossRef] [PubMed]
- Miernik, A.; Wilhelm, K.; Ardelt, P.U.; Adams, F.; Kuehhas, F.E.; Schoenthaler, M. Standardized flexible ureteroscopic technique to improve stone-free rates. Urology 2012, 80, 1198–1202. [Google Scholar] [CrossRef] [PubMed]
- Traxer, O.; Thomas, A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J. Urol. 2013, 189, 580–584. [Google Scholar] [CrossRef]
- Miernik, A.; Schoenthaler, M.; Wilhelm, K.; Wetterauer, U.; Zyczkowski, M.; Paradysz, A.; Bryniarski, P. Combined semirigid and flexible ureterorenoscopy via a large ureteral access sheath for kidney stones >2 cm: A bicentric prospective assessment. World J. Urol. 2014, 32, 697–702. [Google Scholar] [CrossRef]
- Pietropaolo, A.; Jones, P.; Whitehurst, L.; Somani, B.K. Role of ‘dusting and pop-dusting’ using a high-powered (100 W) laser machine in the treatment of large stones (≥ 15 mm): Prospective outcomes over 16 months. Urolithiasis 2019, 47, 391–394. [Google Scholar] [CrossRef] [PubMed]
- De Coninck, V.; Keller, E.X.; Somani, B.; Giusti, G.; Proietti, S.; Rodriguez-Socarras, M.; Rodriguez-Monsalve, M.; Doizi, S.; Ventimiglia, E.; Traxer, O. Complications of ureteroscopy: A complete overview. World J. Urol. 2020, 38, 2147–2166. [Google Scholar] [CrossRef] [PubMed]
- Ventimiglia, E.; Traxer, O. What Is Moses Effect: A Historical Perspective. J. Endourol. 2019, 33, 353–357. [Google Scholar] [CrossRef]
- Elhilali, M.M.; Badaan, S.; Ibrahim, A.; Andonian, S. Use of the Moses Technology to Improve Holmium Laser Lithotripsy Outcomes: A Preclinical Study. J. Endourol. 2017, 31, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Traxer, O.; Keller, E.X. Thulium fiber laser: The new player for kidney stone treatment? A comparison with Holmium:YAG laser. World J. Urol. 2020, 38, 1883–1894. [Google Scholar] [CrossRef] [PubMed]
- Andreeva, V.; Vinarov, A.; Yaroslavsky, I.; Kovalenko, A.; Vybornov, A.; Rapoport, L.; Enikeev, D.; Sorokin, N.; Dymov, A.; Tsarichenko, D.; et al. Preclinical comparison of superpulse thulium fiber laser and a holmium:YAG laser for lithotripsy. World J. Urol. 2020, 38, 497–503. [Google Scholar] [CrossRef]
- Corrales, M.; Traxer, O. Initial clinical experience with the new thulium fiber laser: First 50 cases. World J. Urol. 2021, 39, 3945–3950. [Google Scholar] [CrossRef]
- Enikeev, D.; Taratkin, M.; Klimov, R.; Inoyatov, J.; Azilgareeva, C.; Ali, S.; Korolev, D.; Corrales, M.; Traxer, O.; Glybochko, P. Superpulsed Thulium Fiber Laser for Stone Dusting: In Search of a Perfect Ablation Regimen-A Prospective Single-Center Study. J. Endourol. 2020, 34, 1175–1179. [Google Scholar] [CrossRef]
- De Coninck, V.M.J.; Keller, E.X.; Kovalenko, A.; Vinnichenko, V. Dusting efficiency comparison between Moses technology of Ho: YAG laser and superpulse thulium fiber laser. Eur. Urol. Suppl. 2019, 18, e1757–e1758. [Google Scholar] [CrossRef]
- Traxer, O.; Rapoport, L.; Tsarichenko, D.; Dymov, A.; Enikeev, D.; Sorokin, N.; Akopyan, S.; Korolev, A.; Proskura, V.; Klimov, R. First clinical study on superpulse thulium fiber laser for lithotripsy. J. Urol. 2018, 199, e321–e322. [Google Scholar] [CrossRef]
- Petzold, R.; Suarez-Ibarrola, R.; Miernik, A. Temperature assessment of a novel pulsed Thulium solid-state laser compared to a Holmium:YAG laser. J. Endourol. 2021, 35, 853–859. [Google Scholar] [CrossRef]
- Petzold, R.; Miernik, A.; Suarez-Ibarrola, R. In Vitro Dusting Performance of a New Solid State Thulium Laser Compared to Holmium Laser Lithotripsy. J. Endourol. 2021, 35, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Petzold, R.; Miernik, A.; Suarez-Ibarrola, R. Retropulsion force in laser lithotripsy—An in vitro study comparing a Holmium device to a novel pulsed solid-state Thulium laser. World J. Urol. 2021, 39, 3651–3656. [Google Scholar] [CrossRef] [PubMed]
- Guliciuc, M.; Maier, A.C.; Maier, I.M.; Kraft, A.; Cucuruzac, R.R.; Marinescu, M.; Şerban, C.; Rebegea, L.; Constantin, G.B.; Firescu, D. The Urosepsis—A Literature Review. Medicina 2021, 57, 872. [Google Scholar] [CrossRef]
- Font, M.D.; Thyagarajan, B.; Khanna, A.K. Sepsis and Septic Shock-Basics of diagnosis, pathophysiology and clinical decision making. Med. Clin. N. Am. 2020, 104, 573–585. [Google Scholar] [CrossRef]
- Stoller, J.; Halpin, L.; Weis, M.; Aplin, B.; Qu, W.; Georgescu, C.; Nazzal, M. Epidemiology of severe sepsis: 2008–2012. J. Crit. Care 2016, 31, 58–62. [Google Scholar] [CrossRef]
- Khwannimit, B.; Bhurayanontachai, R. The direct costs of intensive care management and risk factors for financial burden of patients with severe sepsis and septic shock. J. Crit. Care 2015, 30, 929–934. [Google Scholar] [CrossRef]
- Wagenlehner, F.; Tandogdu, Z.; Bartoletti, R.; Cai, T.; Cek, M.; Kulchavenya, E.; Köves, B.; Naber, K.; Perepanova, T.; Tenke, P.; et al. The Global Prevalence of Infections in Urology Study: A Long-Term, Worldwide Surveillance Study on Urological Infections. Pathogens 2016, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Cindolo, L.; Castellan, P.; Scoffone, C.M.; Cracco, C.M.; Celia, A.; Paccaduscio, A.; Schips, L.; Proietti, S.; Breda, A.; Giusti, G. Mortality and flexible ureteroscopy: Analysis of six cases. World J. Urol. 2016, 34, 305–310. [Google Scholar] [CrossRef]
- Cindolo, L.; Castellan, P.; Primiceri, G.; Hoznek, A.; Cracco, C.M.; Scoffone, C.M.; Galfano, A.; Petralia, G.; De Angelis, M.; Annino, F.; et al. Life-threatening complications after ureteroscopy for urinary stones: Survey and systematic literature review. Minerva Urol. Nefrol. 2017, 69, 421–431. [Google Scholar] [CrossRef]
- Tanimoto, R.; Cleary, R.C.; Bagley, D.H.; Hubosky, S.G. Ureteral avulsion associated with ureteroscopy: Insights from the MAUDE database. J. Endourol. 2016, 30, 257–261. [Google Scholar] [CrossRef]
- Taie, K.; Jasemi, M.; Khazaeli, D.; Fatholahi, A. Prevalence and management of complications of ureteroscopy: A seven-year experience with introduction of a new maneuver to prevent ureteral avulsion. Urol. J. 2012, 9, 356–360. [Google Scholar]
- Schoenthaler, M.; Buchholz, N.; Farin, E.; Ather, H.; Bach, C.; Bach, T.; Denstedt, J.D.; Fritsche, H.M.; Grasso, M.; Hakenberg, O.W.; et al. The Post-Ureteroscopic Lesion Scale (PULS): A multicenter video-based evaluation of inter-rater reliability. World J. Urol. 2014, 32, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Ambani, S.N.; Faerber, G.J.; Roberts, W.W.; Hollingsworth, J.M.; Wolf, J.S., Jr. Ureteral stents for impassable ureteroscopy. J. Endourol. 2013, 27, 549–553. [Google Scholar] [CrossRef]
- Lildal, S.K.; Andreassen, K.H.; Jung, H.; Pedersen, M.R.; Osther, P.J.S. Evaluation of ureteral lesions in ureterorenoscopy: Impact of access sheath use. Scand. J. Urol. 2018, 52, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Chotikawanich, E.; Korman, E.; Monga, M. Complications of stone baskets: 14-year review of the manufacturer and user facility device experience database. J. Urol. 2011, 185, 179–183. [Google Scholar] [CrossRef]
- Bonkat, G.; Pilatz, A.; Wagenlehner, F. Time to Adapt Our Practice? The European Commission Has Restricted the Use of Fluoroquinolones since March 2019. Eur. Urol. 2019, 76, 273–275. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Somani, B.K.; Giusti, G.; Sun, Y.; Osther, P.J.; Frank, M.; De Sio, M.; Turna, B.; de la Rosette, J. Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: The Clinical Research Office of Endourological Society URS Global study. World J. Urol. 2017, 35, 675–681. [Google Scholar] [CrossRef]
- Giusti, G.; Proietti, S.; Villa, L.; Cloutier, J.; Rosso, M.; Gadda, G.M.; Doizi, S.; Suardi, N.; Montorsi, F.; Gaboardi, F.; et al. Current Standard Technique for Modern Flexible Ureteroscopy: Tips and Tricks. Eur. Urol. 2016, 70, 188–194. [Google Scholar] [CrossRef]
- Berardinelli, F.; Proietti, S.; Cindolo, L.; Pellegrini, F.; Peschechera, R.; Derek, H.; Dalpiaz, O.; Schips, L.; Giusti, G. A prospective multicenter European study on flexible ureterorenoscopy for the management of renal stone. Int. Braz. J. Urol. 2016, 42, 479–486. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wagenius, M.; Rydberg, M.; Popiolek, M.; Forsvall, A.; Stranne, J.; Linder, A. Ureteroscopy: A population based study of clinical complications and possible risk factors for stone surgery. Cent. Eur. J. Urol. 2019, 72, 285–295. [Google Scholar] [CrossRef]
- Chugh, S.; Pietropaolo, A.; Montanari, E.; Sarica, K.; Somani, B.K. Predictors of Urinary Infections and Urosepsis After Ureteroscopy for Stone Disease: A Systematic Review from EAU Section of Urolithiasis (EULIS). Curr. Urol. Rep. 2020, 21, 16. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Sun, X.-Z.; Lai, D.-H.; Li, X.; He, Y.-Z. Fever and systemic inflammatory response syndrome after retrograde intrarenal surgery: Risk factors and predictive model. Kaohsiung J. Med. Sci. 2018, 201834, 400–408. [Google Scholar] [CrossRef]
- Uchida, Y.; Takazawa, R.; Kitayama, S.; Tsujii, T. Predictive risk factors for systemic inflammatory response syndrome following ureteroscopic laser lithotripsy. Urolithiasis 2018, 46, 375–381. [Google Scholar] [CrossRef]
- Hu, M.; Zhong, X.; Cui, X.; Xu, X.; Zhang, Z.; Guan, L.; Feng, Q.; Huang, Y.; Hu, W. Development and validation of a risk-prediction nomogram for patients with ureteral calculi associated with urosepsis: A retrospective analysis. PLoS ONE 2018, 13, e0201515. [Google Scholar] [CrossRef]
- Czajkowski, K.; Broś-Konopielko, M.; Teliga-Czajkowska, J. Urinary tract infection in women. Menopause Rev. 2021, 20, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Sammon, J.D.; Ghani, K.R.; Karakiewicz, P.I.; Bhojani, N.; Ravi, P.; Sun, M.; Sukumar, S.; Trinh, V.Q.; Kowalczyk, K.J.; Kim, S.P.; et al. Temporal trends, practice patterns, and treatment outcomes for infected upper urinary tract stones in the United States. Eur. Urol. 2013, 64, 85–92. [Google Scholar] [CrossRef]
- Southern, J.B.; Higgins, A.M.; Young, A.J.; Kost, K.A.; Schreiter, B.R.; Clifton, M.; Fulmer, B.R.; Garg, T. Risk factors for postoperative fever and systemic inflammatory response syndrome after ureteroscopy for stone disease. J. Endourol. 2019, 33, 516–522. [Google Scholar] [CrossRef]
- Baboudjian, M.; Gondran-Tellier, B.; Abdallah, R.; Sichez, P.C.; Akiki, A.; Gaillet, S.; Delaporte, V.; Karsenty, G.; Lechevallier, E.; Boissier, R. Predictive risk factors of urinary tract infection following flexible ureteroscopy despite preoperative precautions to avoid infectious complications. World J. Urol. 2019, 38, 1253–1259. [Google Scholar] [CrossRef]
- Senocak, C.; Ozcan, C.; Sahin, T.; Yilmaz, G.; Ozyuvali, E.; Sarikaya, S.; Resorlu, B.; Oguz, U.; Bozkurt, O.F.; Unsal, A.; et al. Risk Factors of Infectious Complications after Flexible Uretero-renoscopy with Laser Lithotripsy. Urol. J. 2018, 15, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Berardinelli, F.; De Francesco, P.; Marchioni, M.; Cera, N.; Proietti, S.; Hennessey, D.; Dalpiaz, O.; Cracco, C.; Scoffone, C.; Schips, L.; et al. Infective complications after retrograde intrarenal surgery: A new standardized classification system. Int. Urol. Nephrol. 2016, 48, 1757–1762. [Google Scholar] [CrossRef]
- Blackmur, J.P.; Maitra, N.U.; Marri, R.R.; Housami, F.; Malki, M.; Mcilhenny, C. Analysis of factors’ association with risk of postoperative urosepsis in patients undergoing ureteroscopy for treatment of stone disease. J. Endourol. 2016, 30, 963–969. [Google Scholar] [CrossRef]
- Youssef, R.F.; Neisius, A.; Goldsmith, Z.G.; Ghaffar, M.; Tsivian, M.; Shin, R.H.; Cabrera, F.; Ferrandino, M.N.; Scales, C.D.; Preminger, G.M.; et al. Clinical outcomes after ureteroscopic lithotripsy in patients who initially presented with urosepsis: Matched pair comparison with elective ureteroscopy. J. Endourol. 2014, 28, 1439–1443. [Google Scholar] [CrossRef] [PubMed]
- Pietropaolo, A.; Hendry, J.; Kyriakides, R.; Geraghty, R.; Jones, P.; Aboumarzouk, O.; Somani, B.K. Outcomes of Elective Ureteroscopy for Ureteric Stones in Patients with Prior Urosepsis and Emergency Drainage: Prospective Study over 5 yr from a Tertiary Endourology Centre. Eur. Urol. Focus. 2020, 6, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Kanno, T.; Matsuda, A.; Sakamoto, H.; Higashi, Y.; Yamada, H. Safety and efficacy of ureteroscopy after obstructive pyelonephritis treatment. Int. J. Urol. 2013, 20, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Nevo, A.; Mano, R.; Baniel, J.; Lifshitz, D.A. Ureteric stent dwelling time: A risk factor for post-ureteroscopy sepsis. BJU Int. 2017, 120, 117–122. [Google Scholar] [CrossRef]
- Tokas, T.; Herrmann, T.R.W.; Skolarikos, A.; Nagele, U. Training and Research in Urological Surgery and Technology (T.R.U.S.T.)-Group. Pressure matters: Intrarenal pressures during normal and pathological conditions, and impact of increased values to renal physiology. World J. Urol. 2019, 37, 125–131. [Google Scholar] [CrossRef]
- Tokas, T.; Skolarikos, A.; Herrmann, T.R.W.; Nagele, U. Training and Research in Urological Surgery and Technology (T.R.U.S.T.)-Group. Pressure matters 2: Intrarenal pressure ranges during upper-tract endourological procedures. World J. Urol. 2019, 37, 133–142. [Google Scholar] [CrossRef]
- Geraghty, R.M.; Ishii, H.; Somani, B.K. Outcomes of flexible ureteroscopy and laser fragmentation for treatment of large renal stones with and without the use of ureteral access sheaths: Results from a university hospital with a review of literature. Scand. J. Urol. 2016, 50, 216–219. [Google Scholar] [CrossRef]
- Skolarikos, A.; Gross, A.J.; Krebs, A.; Unal, D.; Bercowsky, E.; Eltahawy, E.; Somani, B.K.; de la Rosette, J. Outcomes of Flexible Ureterorenoscopy for Solitary Renal Stones in the CROES URS Global Study. J. Urol. 2015, 194, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Prattley, S.; Voss, J.; Cheung, S.; Geraghty, R.; Jones, P.; Somani, B.K. Ureteroscopy and stone treatment in the elderly (≥70 years): Prospective outcomes over 5- years with a review of literature. Int. Braz. J. Urol. 2018, 44, 750–757. [Google Scholar] [CrossRef]
- Emiliani, E.; Piccirilli, A.; Cepeda-Delgado, M.; Kanashiro, A.K.; Mantilla, D.; Amaya, C.A.; Sanchez-Martin, F.M.; Millan-Rodriguez, F.; Territo, A.; Amón-Sesmero, J.H.; et al. Flexible ureteroscopy in extreme elderly patients (80 years of age and older) is feasible and safe. World J. Urol. 2020, 39, 2703–2708. [Google Scholar] [CrossRef] [PubMed]
- Cai, T.; Cocci, A.; Coccarelli, F.; Ruggera, L.; Lanzafame, P.; Caciagli, P.; Malossini, G.; Crisci, A.; Trinchieri, A.; Perletti, G.; et al. Infectious Complications After Laser Vaporization of Urinary Stones During Retrograde Intrarenal Surgery Are Not Associated with Spreading of Bacteria into Irrigation Fluid but with Previous Use of Fluoroquinolones. Eur. Urol. Focus. 2021, 7, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Jian, Z.Y.; Ma, Y.C.; Liu, R.; Li, H.; Wang, K. Preoperative positive urine nitrite and albumin-globulin ratio are independent risk factors for predicting postoperative fever after retrograde Intrarenal surgery based on a retrospective cohort. BMC Urol. 2020, 20, 50. [Google Scholar] [CrossRef] [PubMed]
- Aboumarzouk, O.M.; Somani, B.K.; Monga, M. Flexible ureteroscopy and holmium:YAG laser lithotripsy for stone disease in patients with bleeding diathesis: A systematic review of the literature. Int. Braz. J. Urol. 2012, 38, 298–306. [Google Scholar] [CrossRef]
- Sharaf, A.; Amer, T.; Somani, B.K.; Aboumarzouk, O.M. Ureteroscopy in Patients with Bleeding Diatheses, Anticoagulated, and on Anti-Platelet Agents: A Systematic Review and Meta-Analysis of the Literature. J. Endourol. 2017, 31, 1217–1225. [Google Scholar] [CrossRef]
- Pietropaolo, A.; Reeves, T.; Aboumarzouk, O.; Kallidonis, P.; Ozsoy, M.; Skolarikos, A.; Tailly, T.; Liatsikos, E.; Traxer, O.; Somani, B.K. Endourologic Management (PCNL, URS, SWL) of Stones in Solitary Kidney: A Systematic Review from European Association of Urologists Young Academic Urologists and Uro-Technology Groups. J. Endourol. 2020, 34, 7–17. [Google Scholar] [CrossRef]
- Grosso, A.A.; Sessa, F.; Campi, R.; Viola, L.; Polverino, P.; Crisci, A.; Salvi, M.; Liatsikos, E.; Feu, O.A.; Di Maida, F.; et al. Intraoperative and postoperative surgical complications after ureteroscopy, retrograde intrarenal surgery, and percutaneous nephrolithotomy: A systematic review. Minerva Urol. Nephrol. 2021, 73, 309–332. [Google Scholar] [CrossRef]
- Krambeck, A.; Wijnstok, N.; Olbert, P.; Mitroi, G.; Bariol, S.; Shah, H.N.; El-Abd, A.S.; Onal, B.; de la Rosette, J. The Influence of Body Mass Index on Outcomes in Ureteroscopy: Results from the Clinical Research Office of Endourological Society URS Global Study. J. Endourol. 2017, 31, 20–26. [Google Scholar] [CrossRef]
- Ishii, H.; Couzins, M.; Aboumarzouk, O.; Biyani, C.S.; Somani, B.K. Outcomes of Systematic Review of Ureteroscopy for Stone Disease in the Obese and Morbidly Obese Population. J. Endourol. 2016, 30, 135–145. [Google Scholar] [CrossRef]
- Aboumarzouk, O.M.; Somani, B.K.; Monga, M. Safety and efficacy of ureteroscopic lithotripsy for stone disease in obese patients: A systematic review of the literature. BJU Int. 2012, 110, E374–E380. [Google Scholar] [CrossRef] [PubMed]
- Komori, M.; Izaki, H.; Daizumoto, K.; Tsuda, M.; Kusuhara, Y.; Mori, H.; Kagawa, J.; Yamaguchi, K.; Yamamoto, Y.; Fukumori, T.; et al. Complications of Flexible Ureteroscopic Treatment for Renal and Ureteral Calculi during the Learning Curve. Urol. Int. 2015, 95, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Bres-Niewada, E.; Dybowski, B.; Zapała, P.; Poletajew, S.; Miązek-Zapała, N.; Michałek, I.; Radziszewski, P. A stone pushed back to the collecting system—Long therapeutic path in centers with limited access to flexible instruments. Cent. Eur. J. Urol. 2018, 71, 186–189. [Google Scholar] [CrossRef]
- Talso, M.; Goumas, I.K.; Kamphuis, G.M.; Dragos, L.; Tefik, T.; Traxer, O.; Somani, B.K. Reusable flexible ureterorenoscopes are more cost-effective than single-use scopes: Results of a systematic review from PETRA Uro-group. Transl. Androl. Urol. 2019, 8, S418–S425. [Google Scholar] [CrossRef] [PubMed]
- Ozimek, T.; Schneider, M.H.; Hupe, M.C.; Wiessmeyer, J.R.; Cordes, J.; Chlosta, P.L.; Merseburger, A.S.; Kramer, M.W. Retrospective Cost Analysis of a Single-Center Reusable Flexible Ureterorenoscopy Program: A Comparative Cost Simulation of Disposable fURS as an Alternative. J. Endourol. 2017, 31, 1226–1230. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).