The Importance of Physical Activity to Augment Mood during COVID-19 Lockdown
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Protocol
2.3. Measurements
2.4. Statistical Analysis
3. Results
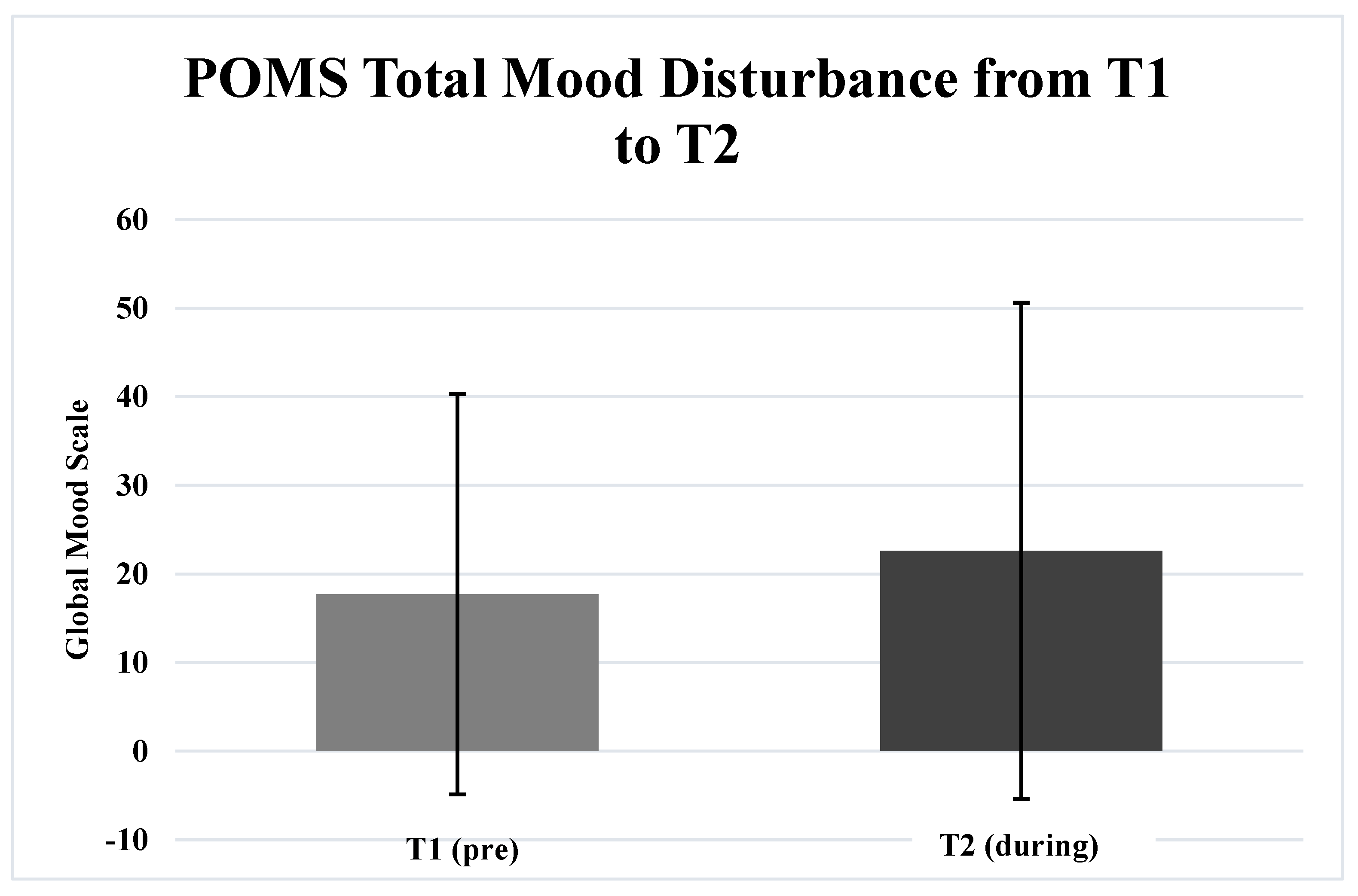
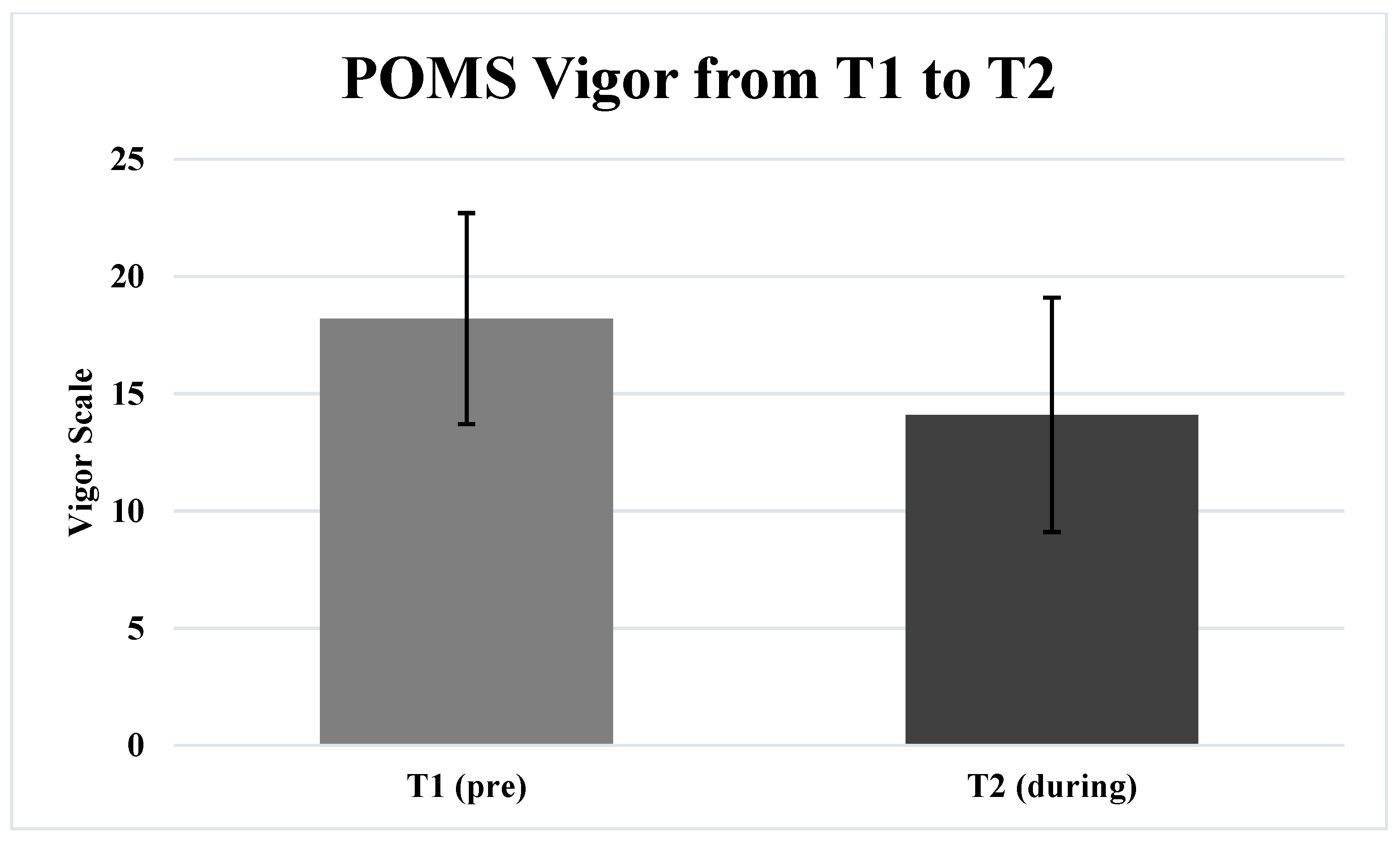
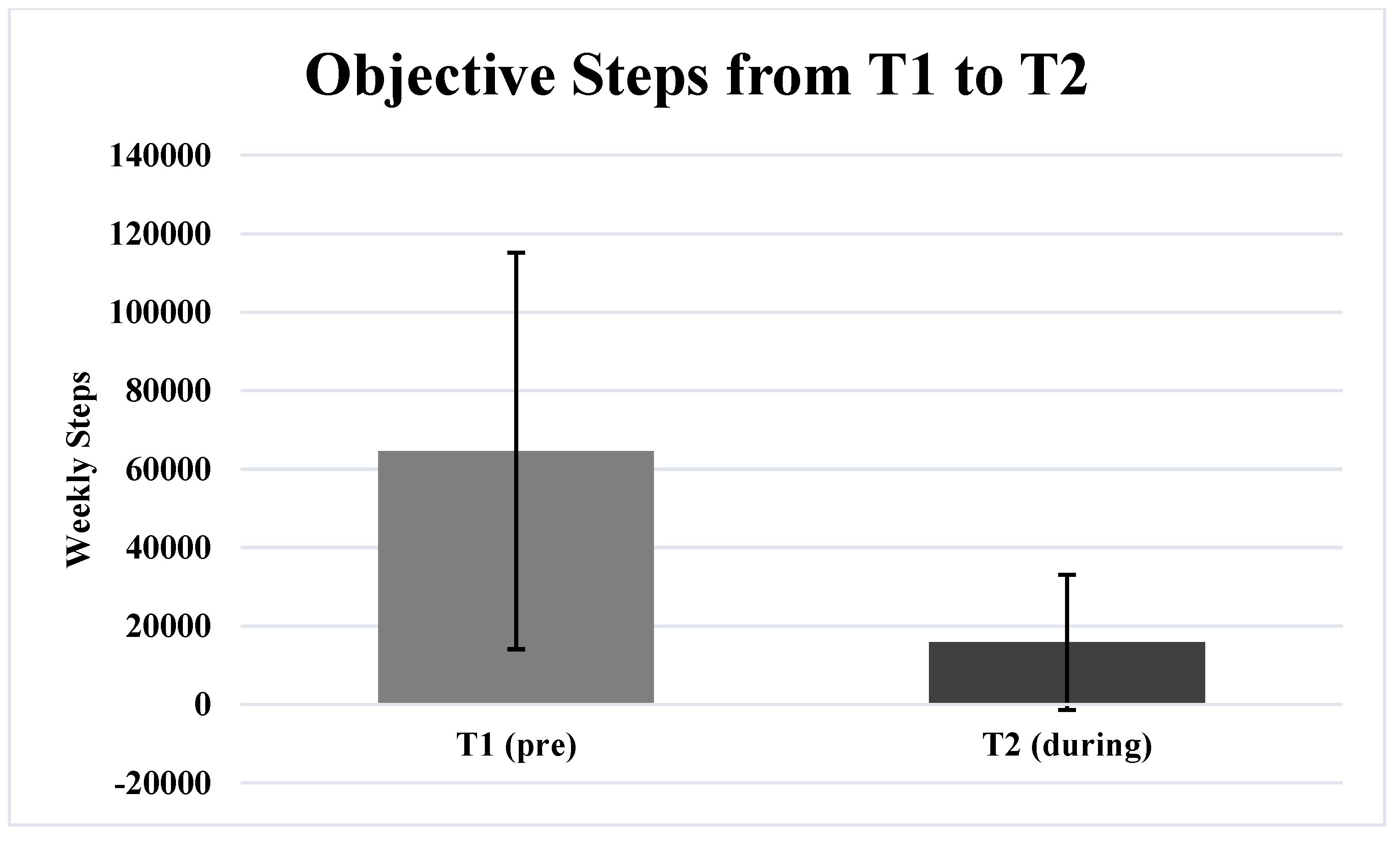
3.1. Pre-Lockdown to During-Lockdown Differences
3.2. Associations of Variables
4. Discussion
5. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sañudo, B.; Fennell, C.; Sánchez-Oliver, A.J. Objectively-Assessed Physical Activity, Sedentary Behavior, Smartphone Use, and Sleep Patterns Pre- and during-COVID-19 Quarantine in Young Adults from Spain. Sustainability 2020, 12, 5890. [Google Scholar] [CrossRef]
- Barkley, J.E.; Lepp, A.; Glickman, E.; Farnell, G.B.; Wiet, R.; Dowdell, B. The Acute Effects of the COVID-19 Pandemic on Physical Activity and Sedentary Behavior in University Students and Employees. Int. J. Exerc. Sci. 2020, 13, 1326–1339. [Google Scholar] [PubMed]
- Lee, S.A.; Ju, Y.J.; Lee, J.E.; Hyun, I.S.; Nam, J.Y.; Han, K.-T.; Park, E.-C. The Relationship between Sports Facility Accessibility and Physical Activity among Korean Adults. BMC Pub. Health 2016, 16, 893. [Google Scholar] [CrossRef] [Green Version]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- López-Bueno, R.; Calatayud, J.; Ezzatvar, Y.; Casajús, J.A.; Smith, L.; Andersen, L.L.; López-Sánchez, G.F. Association between Current Physical Activity and Current Perceived Anxiety and Mood in the Initial Phase of COVID-19 Confinement. Front. Psychol. 2020, 11, 729. [Google Scholar] [CrossRef]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Murray, G.; Gottlieb, J.; Swartz, H.A. Maintaining Daily Routines to Stabilize Mood: Theory, Data, and Potential Intervention for Circadian Consequences of COVID-19. Can. J. Psychiatry 2020, 66, 9–13. [Google Scholar] [CrossRef]
- Sonza, A.; Sá-Caputo, D.; Sartorio, A.; Tamini, S.; Seixas, A.; Sañudo, B.; Süßenbach, J.; Provenza, M.; Xavier, V.; Taiar, R.; et al. COVID-19 Lockdown and the Behavior Change on Physical Exercise, Pain and Psychological Well-Being: An International Multicentric Study. Int. J. Environ. Res. Public Health 2021, 18, 3810. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.; Smith, L.; Woodland, L.; Wessely, S.; Greenberg, N. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.; Ho, R. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, S.; Wang, Y.; Rauch, A.; Wei, F. Unprecedented Disruption of Lives and Work: Health, Distress and Life Satisfaction of Working Adults in China One Month into the COVID-19 Outbreak. Psychiatry Res. 2020, 288, 112958. [Google Scholar] [CrossRef] [PubMed]
- DeMello, M.M.; Pinto, B.; Dunsiger, S.; Shook, R.; Burgess, S.; Hand, G.; Blair, S. Reciprocal Relationship between Sedentary Behavior and Mood in Young Adults over One-Year Duration. Ment. Health Phys. Act. 2017, 14, 157–162. [Google Scholar] [CrossRef]
- Jiménez-Pavón, D.; Carbonell-Baeza, A.; Lavie, C.J. Physical Exercise as Therapy to Fight against the Mental and Physical Consequences of COVID-19 Quarantine: Special Focus in Older People. Prog. Cardiovasc. Dis. 2020, 63, 386–388. [Google Scholar] [CrossRef]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Ozemek, C.; Laddu, D.R.; Lavie, C.J.; Claeys, H.; Kaminsky, L.A.; Ross, R.; Wisloff, U.; Arena, R.; Blair, S.N. An Update on the Role of Cardiorespiratory Fitness, Structured Exercise and Lifestyle Physical Activity in Preventing Cardiovascular Disease and Health Risk. Prog. Cardiovasc. Dis. 2018, 61, 484–490. [Google Scholar] [CrossRef] [Green Version]
- Fletcher, G.F.; Landolfo, C.; Niebauer, J.; Ozemek, C.; Arena, R.; Lavie, C.J. Promoting Physical Activity and Exercise: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1622–1639. [Google Scholar] [CrossRef]
- Kaminsky, L.A.; Arena, R.; Ellingsen, Ø.; Harber, M.P.; Myers, J.; Ozemek, C.; Ross, R. Cardiorespiratory Fitness and Cardiovascular Disease—The Past, Present, and Future. Prog. Cardiovasc. Dis. 2019, 62, 86–93. [Google Scholar] [CrossRef]
- Imboden, M.T.; Harber, M.P.; Whaley, M.H.; Finch, W.H.; Bishop, D.L.; Fleenor, B.S.; Kaminsky, L.A. The Association between the Change in Directly Measured Cardiorespiratory Fitness across Time and Mortality Risk. Prog. Cardiovasc. Dis. 2019, 62, 157–162. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Lee, D.C.; Brellenthin, A.G.; Sui, X.; Church, T.S.; Lavie, C.J.; Blair, S.N. Association of Muscular Strength and Incidence of Type 2 Diabetes. Mayo Clin. Proc. 2019, 94, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Lee, D.C.; Li, Y.; Zhu, W.; Zhang, R.; Sui, X.; Lavie, C.J.; Blair, S.N. Associations of Resistance Exercise with Cardiovascular Disease Morbidity and Mortality. Med. Sci. Sport Exerc. 2019, 51, 499–508. [Google Scholar] [CrossRef] [PubMed]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef] [PubMed]
- Get the Facts—National Network of Depression Centers. Available online: https://nndc.org/facts/?gclid=CjwKCAjw95yJBhAgEiwAmRrutJh5ChYPaHQliIaJ2rITui3FNnb9UssEwe5pzjF2pLh_PLNELUMjchoCtF8QAvD_BwE (accessed on 27 December 2021).
- Clemente-Suárez, V.J.; Dalamitros, A.A.; Beltran-Velasco, A.I.; Mieglo-Ayuso, J.; Tornero-Aguilera, J.F. Social and psychophysiological consequences of the COVID-19 pandemic: An extensive literature review. J. Front. Psychol. 2020, 11, 3077. [Google Scholar] [CrossRef]
- Terry, P.C.; Parsons-Smith, R.L.; Terry, V. Mood responses associated with COVID-19 Restrictions. J. Front. Psychol. 2020, 11, 3090. [Google Scholar] [CrossRef]
- Li, S.; Wan, Y.; Xue, J.; Zhao, N.; Zhu, T. The impact of COVID-19 epidemic declaration on psychological consequences: A study on active Weibo users. Int. J. Environ. Res. Public Health 2020, 17, 2032. [Google Scholar] [CrossRef] [Green Version]
- Ammar, A.; Trabelsi, K.; Brach, M.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: Insight from the “ECLB-COVID19” multi countries survey. Biol. Sport 2021, 38, 9–21. [Google Scholar] [CrossRef]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of Exercise Is a Major Cause of Chronic Diseases. Comp. Phys. 2012, 2, 1143–1211. [Google Scholar]
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J. Fam. Med. 2020, 41, 365–373. [Google Scholar] [CrossRef]
- Warren, T.Y.; Barry, V.; Hooker, S.P.; Sui, X.; Church, T.S.; Blair, S.N. Sedentary Behaviors Increase Risk of Cardiovascular Disease Mortality in Men. Med. Sci. Sport Exerc. 2010, 42, 879. [Google Scholar] [CrossRef] [Green Version]
- Al-Musharaf, S.; Aljuraiban, G.; Bogis, R.; Alnafisah, R.; Aldhwayan, M.; Tahrani, A. Lifestyle Changes Associated with COVID-19 Quarantine among Young Saudi Women: A Prospective Study. PLoS ONE 2021, 16, e0250625. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Wen, D.; Liang, L.; Jia, Y.; Gao, L.; Lei, J. Evaluating the Validity of Current Mainstream Wearable Devices in Fitness Tracking under Various Physical Activities: Comparative Study. JMIR MHealth UHealth 2018, 6, e9754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Degroote, L.; Hamerlinck, G.; Poels, K.; Maher, C.; Crombez, G.; De Bourdeaudhuij, I.; Vandendriessche, A.; Curtis, R.G.; DeSmet, A. Low-Cost Consumer-Based Trackers to Measure Physical Activity and Sleep Duration among Adults in Free-Living Conditions: Validation Study. JMIR MHealth UHealth 2020, 8, e16674. [Google Scholar] [CrossRef] [PubMed]
- McNair, D.M.; Lorr, M.; Droppleman, L.F. Profile of Mood States Questionnaire; EDITS Educational and Industrial Testing Service: San Diego, CA, USA, 1981; pp. 4–13. [Google Scholar]
- Puccinelli, P.J.; Taline, C.S.; Seffrin, A.; Lira, C.; Vancini, R.L.; Knechtle, B.; Nikolaidis, P.T.; Andrade, M.S. Physical Activity Levels and Mental Health during the COVID-19 Pandemic: Preliminary Results of a Comparative Study between Convenience Samples from Brazil and Switzerland. Medicina 2021, 57, 48. [Google Scholar] [CrossRef] [PubMed]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in Physical Activity and Sedentary Behaviours from before to during the COVID-19 Pandemic Lockdown: A Systematic Review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef] [PubMed]
- Stella, A.; Ajčević, M.; Furlanis, G.; Cillotta, T.; Menichelli, A. Smart Technology for Physical Activity and Health Assessment during COVID-19 Lockdown. J. Sports Med. Phys. Fitness 2020, 61, 452–460. [Google Scholar]
- Muriel, X.; Courel-Ibáñez, J.; Cerezuela-Espejo, V.; Pallarés, J.G. Training Load and Performance Impairments in Professional Cyclists during COVID-19 Lockdown. Int. J. Sports Physiol. Perform. 2020, 16, 735–738. [Google Scholar] [CrossRef]
- Vetrovsky, T.; Frybova, T.; Gant, I.; Semerad, M.; Cimler, R.; Bunc, V.; Siranec, M.; Miklikova, M.; Vesely, J.; Griva, M.; et al. The Detrimental Effect of COVID-19 Nationwide Quarantine on Accelerometer-Assessed Physical Activity of Heart Failure Patients. ESC Heart Fail. 2020, 7, 2093–2097. [Google Scholar] [CrossRef]
- Anyan, F.; Tahrani, O.; Tahrani, L.; Havnen, A. Change in Physical Activity during the Coronavirus Disease 2019 Lockdown in Norway: The Buffering Effect of Resilience on Mental Health. Front. Psychol. 2020, 11, 3514. [Google Scholar] [CrossRef]
- Peterson, J.A.; Chesbro, G.; Larson, R.; Larson, D.; Black, C.D. Short-Term Analysis (8 Weeks) of Social Distancing and Isolation on Mental Health and Physical Activity Behavior during COVID-19. Frontiers 2021, 12, 738. [Google Scholar] [CrossRef]
- Vrijheid, M.; Armstrong, B.K.; Bédard, D.; Brown, J.; Deltour, I.; Iavarone, I.; Krewski, D.; Lagorio, S.; Moore, S.; Richardson, L.; et al. Recall Bias in the Assessment of Exposure to Mobile Phones. J. Expos. Sci. Environ. Epidemiol. 2009, 19, 369–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fennell, C.; Barkley, J.E.; Lepp, A. The Relationship between Cell Phone Use, Physical Activity, and Sedentary Behavior in Adults Aged 18–80. Comp. Hum. Behav. 2019, 90, 53–59. [Google Scholar] [CrossRef]
- Katapally, T.R.; Chu, L.M. Methodology to Derive Objective Screen-State from Smartphones: A Smart Platform Study. Int. J. Environ. Res. Public Health 2019, 16, 2275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozemek, C.; Lavie, C.J.; Rognmo, Ø. Global Physical Activity Levels—Need for Intervention. Prog. Cardiovasc. Dis. 2019, 62, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Adlakha, D.; Oyeyemi, A.; Salvo, D. An International Physical Activity and Public Health Research Agenda to Inform Coronavirus Disease-2019 Policies and Practices. J. Sport Health Sci. 2020, 9, 328–334. [Google Scholar] [CrossRef]
- Sharma, A.; Madaan, V.; Petty, F.D. Exercise for Mental Health. Prim. Care Companion CNS Disord. 2006, 8, 24919. [Google Scholar] [CrossRef]
- Sarris, J.; Thomson, R.; Hargraves, F.; Eaton, M.; de Manincor, M.; Veronese, N.; Solmi, M.; Stubbs, B.; Yung, A.R.; Firth, J. Multiple Lifestyle Factors and Depressed Mood: A Cross-Sectional and Longitudinal Analysis of the UK Biobank (N = 84,860). BMC Med. 2020, 18, 354. [Google Scholar] [CrossRef]
- Weinstein, A.A.; Koehmstedt, C.; Kop, W.J. Mental Health Consequences of Exercise Withdrawal: A Systematic Review. Gen. Hosp. Psychiatry 2017, 49, 11–18. [Google Scholar] [CrossRef]
- Lee, I.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Lippi, G.; Henry, B.M.; Sanchis-Gomar, F. Physical Inactivity and Cardiovascular Disease at the Time of Coronavirus Disease 2019 (COVID-19). Eur. J. Prev. Cardiol. 2020, 27, 906–908. [Google Scholar] [CrossRef]
- Sallis, R.; Young, D.R.; Tartof, S.Y.; Sallis, J.F.; Sall, J.; Li, Q.; Smith, G.N.; Cohen, D.A. Physical Inactivity Is Associated with a Higher Risk for Severe COVID-19 Outcomes: A Study in 48 440 Adult Patients. Br. J. Sports Med. 2021, 55, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Hamar, M.; Kivimäki, M.; Gale, C.G.; Batty, D. Lifestyle Risk Factors, Inflammatory Mechanisms, and COVID-19 Hospitalization: A Community-Based Cohort Study of 387,109 Adults in UK. Brain Behav. Immun. 2020, 87, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Hojman, P. Exercise Protects from Cancer through Regulation of Immune Function and Inflammation. Biochem. Soc. Trans. 2017, 45, 905–911. [Google Scholar] [CrossRef] [PubMed]
- Nieman, D.C.; Wentz, L.M. The Compelling Link between Physical Activity and the Body’s Defense System. J. Sport Health Sci. 2019, 8, 201–217. [Google Scholar] [CrossRef] [PubMed]
- Osimo, S.A.; Aiello, M.; Gentili, C.; Ionta, S.; Cecchetto, C. The Influence of Personality, Resilience, and Alexithymia on Mental Health During COVID-19 Pandemic. J. Front. Psychol. 2021, 12, 341. [Google Scholar]
- Cecchetto, C.; Aiello, M.; Gentili, C.; Ionta, S.; Osimo, S.A. Increased emotional eating during COVID-19 associated with lockdown, psychological and distress. Appetite 2021, 160, 105122. [Google Scholar] [CrossRef]
- Ingram, J.; Maciejewski, G.; Hand, C.F. Changes in Diet, Sleep, and Physical Activity Are Associated With Differences in Negative Mood During COVID-19 Lockdown. J. Front. Psychol. 2020, 11, 2328. [Google Scholar]
- Brand, R.; Timme, S.; Nosrat, S. When pandemic hits; exercise frequency and subjective well-being during COVID-19 pandemic. J. Front. Psychol. 2020, 11, 2391. [Google Scholar] [CrossRef]
| Characteristic | N | % |
|---|---|---|
| Male | 52 (22.2 ± 3.4 years old) | 66.7 |
| Female | 26 (22.9 ± 2.5 years old) | 33.3 |
| Class | 1 sophomore 69 juniors 8 seniors | 1.2 88.5 10.2 |
| Professional Status | 30 employed 48 unemployed | 38.5 61.5 |
| Variables | t-Value | p-Value |
|---|---|---|
| Tension | 0.197 | 0.845 |
| Depression | 1.376 | 0.173 |
| Anger | 0.621 | 0.536 |
| Vigour | −7.455 | ≤0.001 |
| Fatigue | −0.874 | 0.385 |
| Confusion | −0.197 | 0.844 |
| Total Mood Disturbance | 2.255 | 0.027 |
| Steps/wk | −8.259 | ≤0.001 |
| Variables | Adjusted R2 | Beta | t-Value | p-Value |
|---|---|---|---|---|
| T1 Tension | −0.010 | 0.055 | 0.481 | 0.632 |
| T2 Tension | 0.024 | −0.0192 | −1.707 | 0.092 |
| T1 Depression | −0.013 | 0.001 | 0.007 | 0.994 |
| T2 Depression | 0.064 | −0.277 | −2.511 | 0.014 |
| T1 Anger | −0.001 | −0.111 | −0.971 | 0.334 |
| T2 Anger | 0.042 | −0.233 | −2.091 | 0.040 |
| T1 Vigor | −0.010 | 0.053 | 0.463 | 0.644 |
| T2 Vigor | 0.068 | 0.283 | 2.570 | 0.012 |
| T1 Fatigue | −0.012 | −0.032 | −0.277 | 0.782 |
| T2 Fatigue | 0.033 | −0.213 | −1.901 | 0.061 |
| T1 Confusion | −0.013 | −0.021 | −0.179 | 0.858 |
| T2 Confusion | 0.021 | −1.84 | −1.629 | 0.108 |
| T1 TMD | 0.044 | −0.035 | −0.302 | 0.764 |
| T2 TMD | 0.079 | −0.302 | −2.754 | 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fennell, C.; Eremus, T.; Puyana, M.G.; Sañudo, B. The Importance of Physical Activity to Augment Mood during COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2022, 19, 1270. https://doi.org/10.3390/ijerph19031270
Fennell C, Eremus T, Puyana MG, Sañudo B. The Importance of Physical Activity to Augment Mood during COVID-19 Lockdown. International Journal of Environmental Research and Public Health. 2022; 19(3):1270. https://doi.org/10.3390/ijerph19031270
Chicago/Turabian StyleFennell, Curtis, Thomas Eremus, Moisés Grimaldi Puyana, and Borja Sañudo. 2022. "The Importance of Physical Activity to Augment Mood during COVID-19 Lockdown" International Journal of Environmental Research and Public Health 19, no. 3: 1270. https://doi.org/10.3390/ijerph19031270
APA StyleFennell, C., Eremus, T., Puyana, M. G., & Sañudo, B. (2022). The Importance of Physical Activity to Augment Mood during COVID-19 Lockdown. International Journal of Environmental Research and Public Health, 19(3), 1270. https://doi.org/10.3390/ijerph19031270








