Epidemiology of SARS-CoV-2 Infection in Italy Using Real-World Data: Methodology and Cohort Description of the Second Phase of Web-Based EPICOVID19 Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development of the EPICOVID19 Questionnaires
2.2. Content of the EPICOVID19 Questionnaire
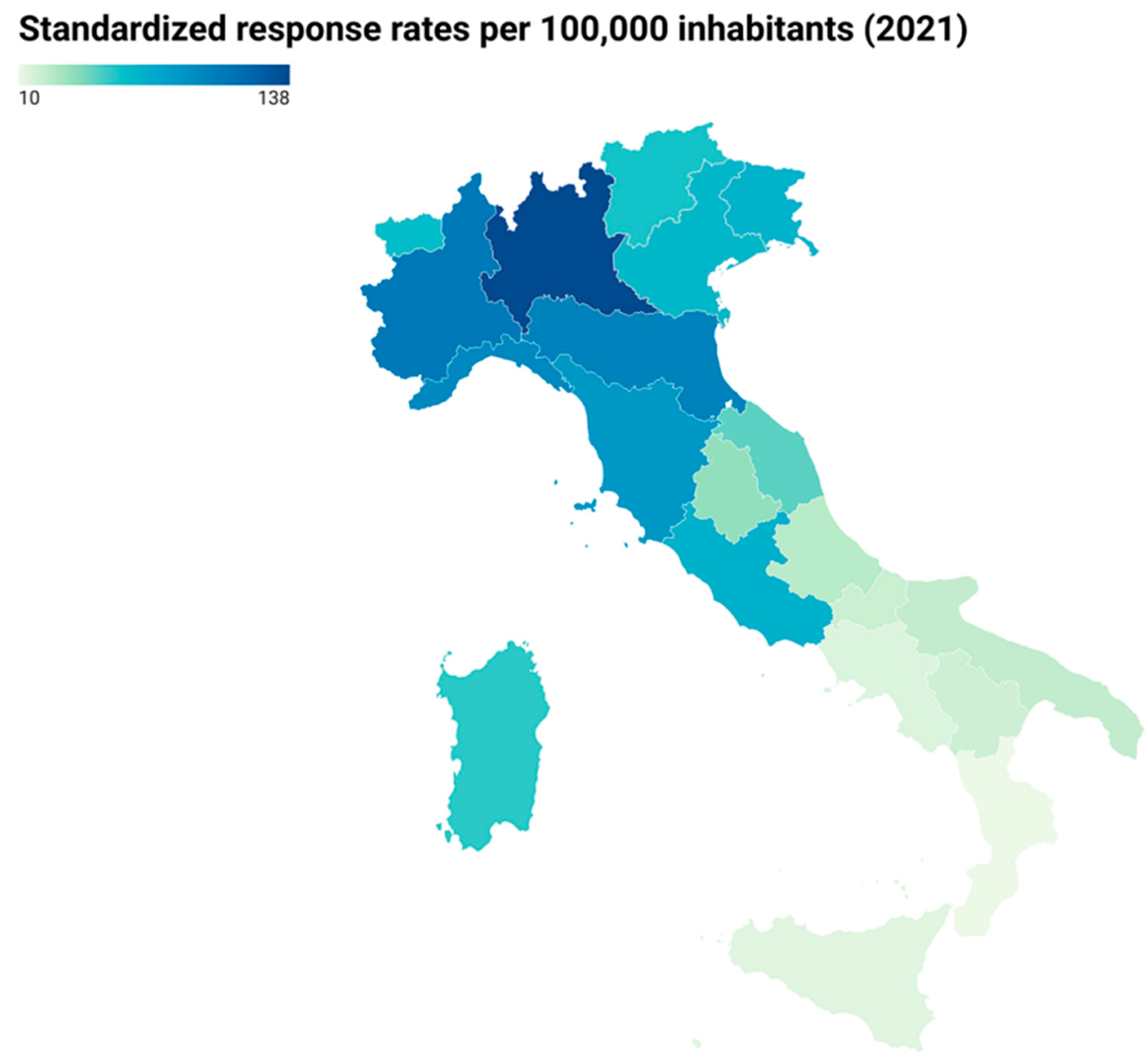
2.3. Sample Recruitment and Study Population
2.4. Variables Collected and Data Transformations
2.5. Statistical Analysis
2.6. Dissemination and Provision of Results to Participants
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Centre for Disease Prevention and Control. Available online: https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-resurgence-reported-cases-covid-19 (accessed on 18 December 2021).
- Arcgis COVID-19 Situazione Italia. Available online: http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1 (accessed on 20 December 2021).
- Russell, T.W.; Golding, N.; Hellewell, J.; Abbott, S.; Wright, L.; Pearson, C.A.; van Zandvoort, K.; Jarvis, C.I.; Gibbs, H.; Liu, Y.; et al. Reconstructing the early global dynamics of under-ascertained COVID-19 cases and infections. BMC Med. 2020, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Pullano, G.; Di Domenico, L.; Sabbatini, C.E.; Valdano, E.; Turbelin, C.; Debin, M.; Guerrisi, C.; Kengne-Kuetche, C.; Souty, C.; Hanslik, T.; et al. Underdetection of cases of COVID-19 in France threatens epidemic control. Nature 2021, 590, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Chen, X.; Deng, X.; Chen, Z.; Gong, H.; Yan, H.; Wu, Q.; Shi, H.; Lai, S.; Ajelli, M.; et al. Disease burden and clinical severity of the first pandemic wave of COVID-19 in Wuhan, China. Nat. Commun. 2020, 11, 5411. [Google Scholar] [CrossRef] [PubMed]
- Budd, J.; Miller, B.S.; Manning, E.M.; Lampos, V.; Zhuang, M.; Edelstein, M.; Rees, G.; Emery, V.C.; Stevens, M.M.; Keegan, N.; et al. Digital technologies in the public-health response. Nat. Med. 2020, 26, 1183–1192. [Google Scholar] [CrossRef]
- McCall, B. COVID-19 and artificial intelligence: Protecting health-care workers and curbing the spread. Lancet Digit. Health 2020, 2, e166–e167. [Google Scholar] [CrossRef]
- Menni, C.; Valdes, A.M.; Freidin, M.B.; Sudre, C.H.; Nguyen, L.H.; Drew, D.A.; Ganesh, S.; Varsavsky, T.; Cardoso, M.J.; Moustafa, J.S.E.-S.; et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat. Med. 2020, 26, 1037–1040. [Google Scholar] [CrossRef]
- Robertson, M.M.; Kulkarni, S.G.; Rane, M.; Kochhar, S.; Berry, A.; Chang, M.; Mirzayi, C.; You, W.; Maroko, A.; Zimba, R.; et al. Cohort profile: A national, community-based prospective cohort study of SARS-CoV-2 pandemic outcomes in the USA-the CHASING COVID Cohort study. BMJ Open 2021, 11, e048778. [Google Scholar] [CrossRef]
- Rossman, H.; Keshet, A.; Shilo, S.; Gavrieli, A.; Bauman, T.; Cohen, O.; Shelly, E.; Balicer, R.; Geiger, B.; Dor, Y.; et al. A framework for identifying regional outbreak and spread of COVID-19 from one-minute population-wide surveys. Nat. Med. 2020, 26, 634–638. [Google Scholar] [CrossRef] [Green Version]
- Krausz, M.; Westenberg, J.N.; Vigo, D.; Spence, R.T.; Ramsey, D. Emergency Response to COVID-19 in Canada: Platform Development and Implementation for eHealth in Crisis Management. JMIR Public Health Surveill. 2020, 6, e18995. [Google Scholar] [CrossRef]
- Wu, D.C.; Jha, P.; Lam, T.; Brown, P.; Gelband, H.; Nagelkerke, N.; Birnboim, H.C.; Reid, A.; Action to Beat Coronavirus in Canada/Action pour Battre le Coronavirus (Ab-C) Study Group. Predictors of self-reported symptoms and testing for COVID-19 in Canada using a nationally representative survey. PLoS ONE 2020, 15, e0240778. [Google Scholar] [CrossRef]
- Sudre, C.H.; Keshet, A.; Graham, M.S.; Joshi, A.D.; Shilo, S.; Rossman, H.; Murray, B.; Molteni, E.; Klaser, K.; Canas, L.D.; et al. Anosmia, ageusia, and other COVID-19-like symptoms in association with a positive SARS-CoV-2 test, across six national digital surveillance platforms: An observational study. Lancet Digit. Health 2021, 3, e577–e586. [Google Scholar] [CrossRef]
- Adorni, F.; Prinelli, F.; Bianchi, F.; Giacomelli, A.; Pagani, G.; Bernacchia, D.; Rusconi, S.; Maggi, S.; Trevisan, C.; Noale, M.; et al. Self-Reported Symptoms of SARS-CoV-2 Infection in a Nonhospitalized Population in Italy: Cross-Sectional Study of the EPICOVID19 Web-Based Survey. JMIR Public Health Surveill. 2020, 6, e21866. [Google Scholar] [CrossRef] [PubMed]
- Bastiani, L.; Fortunato, L.; Pieroni, S.; Bianchi, F.; Adorni, F.; Prinelli, F.; Giacomelli, A.; Pagani, G.; Maggi, S.; Trevisan, C.; et al. Rapid COVID-19 Screening Based on Self-Reported Symptoms: Psychometric Assessment and Validation of the EPICOVID19 Short Diagnostic Scale. J. Med. Internet Res. 2021, 23, e23897. [Google Scholar] [CrossRef]
- Trevisan, C.; Noale, M.; Prinelli, F.; Maggi, S.; Sojic, A.; Di Bari, M.; Molinaro, S.; Bastiani, L.; Giacomelli, A.; Galli, M.; et al. Age-Related Changes in Clinical Presentation of Covid-19: The EPICOVID19 Web-Based Survey. J. Med. Internet Res. 2021, 23, e23897. [Google Scholar] [CrossRef]
- Prinelli, F.; Bianchi, F.; Drago, G.; Ruggieri, S.; Sojic, A.; Jesuthasan, N.; Molinaro, S.; Bastiani, L.; Maggi, S.; Noale, M.; et al. Association Between Smoking and SARS-CoV-2 Infection: Cross-sectional Study of the EPICOVID19 Internet-Based Survey. JMIR Public Health Surveill. 2021, 7, e27091. [Google Scholar] [CrossRef]
- Noale, M.; Trevisan, C.; Maggi, S.; Antonelli Incalzi, R.; Pedone, C.; Di Bari, M.; Adorni, F.; Jesuthasan, N.; Sojic, A.; Galli, M.; et al. The Association between Influenza and Pneumococcal Vaccinations and SARS-Cov-2 Infection: Data from the EPICOVID19 Web-Based Survey. Vaccines 2020, 8, 471. [Google Scholar] [CrossRef]
- Giacomelli, A.; Galli, M.; Maggi, S.; Pagani, G.; Incalzi, R.A.; Pedone, C.; Di Bari, M.; Noale, M.; Trevisan, C.; Bianchi, F.; et al. Missed Opportunities of Flu Vaccination in Italian Target Categories: Insights from the Online EPICOVID 19 Survey. Vaccines 2020, 8, 669. [Google Scholar] [CrossRef]
- Cori, L.; Curzio, O.; Adorni, F.; Prinelli, F.; Noale, M.; Trevisan, C.; Fortunato, L.; Giacomelli, A.; Bianchi, F. Fear of COVID-19 for Individuals and Family Members: Indications from the National Cross-Sectional Study of the EPICOVID19 Web-Based Survey. Int. J. Environ. Res. Public Health 2021, 18, 3248. [Google Scholar] [CrossRef]
- Trevisan, C.; Pedone, C.; Maggi, S.; Noale, M.; Di Bari, M.; Sojic, A.; Molinaro, S.; Giacomelli, A.; Bianchi, F.; Tavio, M.; et al. Accessibility to SARS-CoV-2 swab test during the Covid-19 pandemic: Did age make the difference? Health Policy 2021, 125, 1580–1586. [Google Scholar] [CrossRef]
- Eurostat. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Glossary:Self-perceived_health (accessed on 18 December 2021).
- Townsend, P.; Phillimore, P.; Beattie, A. Health and Deprivation. Inequality and the North; Croom Helm Ltd.: London, UK, 1987; p. 221. ISBN 0-7099-4352-0. [Google Scholar]
- Jenkins, C.D.; Stanton, B.A.; Niemcryk, S.J.; Rose, R.M. A scale for the estimation of sleep problems in clinical research. J. Clin. Epidemiol. 1988, 41, 313–321. [Google Scholar] [CrossRef]
- Monterrosa-Castro, Á.; Portela-Buelvas, K.; Salguedo-Madrid, M.; Mo-Carrascal, J.; Leidy, C.D.-M. Instruments to study sleep disorders in climacteric women. Sleep Sci. 2016, 9, 169–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- I.Stat. Available online: http://dati.istat.it/ (accessed on 15 November 2021).
- Eurostat. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20210517-2 (accessed on 18 December 2021).
- Osservatori.net. Digital Innovation. Available online: https://www.osservatori.net/it/ricerche/comunicati-stampa/smart-working-emergenza-covid19-new-normal (accessed on 18 December 2021).
- Alimoradi, Z.; Broström, A.; Tsang, H.W.H.; Griffiths, M.D.; Haghayegh, S.; Ohayon, M.M.; Lin, C.Y.; Pakpour, A.H. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: A systematic review and meta-analysis. EClinicalMedicine 2021, 36, 100916. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.Y.; Wang, J.; Ou-Yang, X.Y.; Miao, Q.; Chen, R.; Liang, F.-X.; Zhang, Y.-P.; Tang, Q.; Wang, T. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021, 77, 348–354. [Google Scholar] [CrossRef]
- García-Fernández, L.; Romero-Ferreiro, V.; Padilla, S.; David, L.P.; Monzó-García, M.; Rodriguez-Jimenez, R. Gender differences in emotional response to the COVID-19 outbreak in Spain. Brain Behav. 2021, 11, e01934. [Google Scholar] [CrossRef]
- Guadagni, V.; Umilta, A.; Iaria, G. Sleep Quality, Empathy, and Mood During the Isolation Period of the COVID-19 Pandemic in the Canadian Population: Females and Women Suffered the Most. Front. Glob. Women’s Health 2020, 1, 585938. [Google Scholar] [CrossRef]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef]
- Galasso, V.; Pons, V.; Profeta, P.; Becher, M.; Brouard, S.; Foucault, M. Gender differences in COVID-19 attitudes and behavior: Panel evidence from eight countries. Proc. Natl. Acad. Sci. USA 2020, 117, 27285–27291. [Google Scholar] [CrossRef]
- Giacomelli, A.; Pezzati, L.; Conti, F.; Bernacchia, D.; Siano, M.; Oreni, L.; Rusconi, S.; Gervasoni, C.; Ridolfo, A.L.; Rizzardini, G.; et al. Self-reported Olfactory and Taste Disorders in Patients With Severe Acute Respiratory Coronavirus 2 Infection: A Cross-sectional Study. Clin. Infect. Dis. 2020, 71, 889–890. [Google Scholar] [CrossRef] [Green Version]
- Vena, A.; Berruti, M.; Adessi, A.; Blumetti, P.; Brignole, M.; Colognato, R.; Gaggioli, G.; Giacobbe, D.R.; Bracci-Laudiero, L.; Magnasco, L.; et al. Prevalence of Antibodies to SARS-CoV-2 in Italian Adults and Associated Risk Factors. J. Clin. Med. 2020, 9, 2780. [Google Scholar] [CrossRef]
- De Santi, M.; Diotallevi, A.; Brandi, G. Seroprevalence of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection in an Italian cohort in Marche Region, Italy. Acta Biomed. 2021, 92, e2021070. [Google Scholar] [CrossRef] [PubMed]
- Pagani, G.; Conti, F.; Giacomelli, A.; Bernacchia, D.; Rondanin, R.; Prina, A.; Scolari, V.; Gandolfi, C.E.; Castaldi, S.; Marano, G.; et al. Seroprevalence of SARS-CoV-2 significantly varies with age: Preliminary results from a mass population screening. J. Infect. 2020, 81, e10–e12. [Google Scholar] [CrossRef] [PubMed]
- Ministero della Salute. Available online: http://www.salute.gov.it/imgs/C_17_notizie_4998_0_file.pdf (accessed on 18 December 2021).
- Rostami, A.; Sepidarkish, M.; Leeflang, M.M.G.; Riahi, S.M.; Shiadeh, M.N.; Esfandyari, S.; Mokdad, A.H.; Hotez, P.J.; Gasser, R.B. SARS-CoV-2 seroprevalence worldwide: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Abate, B.B.; Kassie, A.M.; Kassaw, M.W.; Aragie, T.G.; Masresha, S.A. Sex difference in coronavirus disease (COVID-19): A systematic review and meta-analysis. BMJ Open 2020, 10, e040129. [Google Scholar] [CrossRef]
- The Sex, Gender and COVID-19 Project, Men, Sex Gender and COVID-19. Available online: https://globalhealth5050.org/the-sex-gender-and-covid-19-project/ (accessed on 18 December 2021).
- Daniali, H.; Flaten, M.A. What Psychological Factors Make Individuals Believe They Are Infected by Coronavirus 2019? Front. Psychol. 2021, 12, 667722. [Google Scholar] [CrossRef]
- Daniali, H.; Flaten, M.A. Experiencing COVID-19 symptoms without the disease: The role of nocebo in reporting of symptoms. Scand. J. Public Health 2021. [Google Scholar] [CrossRef]
- Aslaksen, P.M.; Myrbakk, I.N.; Høifødt, R.S.; Flaten, M.A. The effect of experimenter gender on autonomic and subjective responses to pain stimuli. Pain 2007, 129, 260–268. [Google Scholar] [CrossRef]
- Biolè, C.; Bianco, M.; Núñez-Gil, I.J.; Cerrato, E.; Spirito, A.; Roubin, S.R.; Viana-Llamas, M.C.; Gonzalez, A.; Castro-Mejia, A.F.; Eid, C.M.; et al. Gender Differences in the Presentation and Outcomes of Hospitalized Patients With COVID-19. J. Hosp. Med. 2021, 16, 349–352. [Google Scholar] [CrossRef]
- Lechien, J.R.; Chiesa-Estomba, C.M.; Place, S.; Van Laethem, Y.; Cabaraux, P.; Mat, Q.; Huet, K.; Plzak, J.; Horoi, M.; Hans, S.; et al. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J. Intern. Med. 2020, 288, 335–344. [Google Scholar] [CrossRef]
- Ancochea, J.; Izquierdo, J.L.; Soriano, J.B. Evidence of Gender Differences in the Diagnosis and Management of Coronavirus Disease 2019 Patients: An Analysis of Electronic Health Records Using Natural Language Processing and Machine Learning. J. Women’s Health 2021, 30, 393–404. [Google Scholar] [CrossRef]
- Eurostat. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/DDN-20200409-2 (accessed on 18 December 2021).
- Ministero della Salute. Available online: https://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=5208 (accessed on 18 December 2021).
- World Health Organization. Available online: https://www.who.int/publications/i/item/WHO-UHL-PHC-SP-2021.02 (accessed on 18 December 2021).
- Oran, D.P.; Topol, E.J. The Proportion of SARS-CoV-2 Infections That Are Asymptomatic: A Systematic Review. Ann. Intern. Med. 2021, 174, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Stringhini, S.; Wisniak, A.; Piumatti, G.; Azman, A.S.; Lauer, S.A.; Baysson, H.; De Ridder, D.; Petrovic, D.; Schrempft, S.; Marcus, K.; et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): A population-based study. Lancet 2020, 396, 313–319. [Google Scholar] [CrossRef]
- Pollán, M.; Pérez-Gómez, B.; Pastor-Barriuso, R.; Oteo, J.; Hernán, M.A.; Pérez-Olmeda, M.; Sanmartín, J.L.; Fernández-García, A.; Cruz, I.; de Larrea, N.F.; et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): A nationwide, population-based seroepidemiological study. Lancet 2020, 396, 535–544. [Google Scholar] [CrossRef]
- Madewell, Z.J.; Yang, Y.; Longini, I.M.; Halloran, M.E.; Dean, N.E. Household Transmission of SARS-CoV-2: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e2031756. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.; Wei, H.; Han, Y.; Catt, H.; Denning, D.W.; Hall, I.; Regan, M.; Verma, A.; Whitfield, C.A.; van Tongeren, M. Risk factors associated with respiratory infectious disease-related presenteeism: A rapid review. BMC Public Health 2021, 21, 1955. [Google Scholar] [CrossRef] [PubMed]
- Drew, D.A.; Nguyen, L.H.; Steves, C.J.; Menni, C.; Freydin, M.; Varsavsky, T.; Sudre, C.H.; Cardoso, M.J.; Ourselin, S.; Wolf, J.; et al. Rapid implementation of mobile technology for real-time epidemiology of COVID-19. Science 2020, 368, 1362–1367. [Google Scholar] [CrossRef]
- Astley, C.M.; Tuli, G.; Mc Cord, K.A.; Cohn, E.L.; Rader, B.; Varrelman, T.J.; Chiu, S.L.; Deng, X.; Stewart, K.; Farag, T.H.; et al. Global monitoring of the impact of the COVID-19 pandemic through online surveys sampled from the Facebook user base. Proc. Natl. Acad. Sci. USA 2021, 118, e2111455118. [Google Scholar] [CrossRef]



| Sex at Birth | ||||
|---|---|---|---|---|
| Females n = 25,146 (60.6) | Males n = 16,327 (39.4) | p-Value | Total n = 41,473 (100) | |
| n (%) | n (%) | n (%) | ||
| Age (mean ± SD) | 49.8 ± 13.0 | 52.2 ± 14.3 | 0.000 | 50.7 ± 13.5 |
| Class of age | ||||
| 19–29 | 1700 (6.8) | 1027 (6.3) | 0.000 | 2727 (6.6) |
| 30–39 | 4434 (17.6) | 2620 (16.0) | 7054 (17.0) | |
| 40–49 | 5815 (23.1) | 3209 (19.7) | 9024 (21.8) | |
| 50–59 | 6802 (27.1) | 3905 (23.9) | 10,707 (25.8) | |
| 60–69 | 5017 (20.0) | 3628 (22.2) | 8645 (20.8) | |
| 70–79 | 1262 (5.0) | 1707 (10.5) | 2969 (7.2) | |
| 80+ | 116 (0.5) | 231 (1.4) | 347 (0.8) | |
| Educational level a | 0.000 | |||
| Low | 723 (2.9) | 658 (4.0) | 1381 (3.3) | |
| Middle | 7286 (29.0) | 5648 (34.6) | 12,934 (31.2) | |
| High | 17,137 (68.2) | 10,021 (61.4) | 27,158 (65.5) | |
| Employment status | ||||
| Employed, stable position | 15,676 (62.3) | 10,448 (64.0) | 0.000 | 26,124 (63.0) |
| Employed, occasional worker | 1056 (4.2) | 407 (2.5) | 1463 (3.5) | |
| Temporary layoff | 379 (1.5) | 114 (0.7) | 493 (1.2) | |
| Unemployed, as before Jun 2020 | 1243 (4.9) | 271 (1.7) | 1514 (3.7) | |
| Unemployed, I lost my employment since Jun 2020 | 446 (1.8) | 193 (1.2) | 639 (1.5) | |
| Student | 850 (3.4) | 583 (3.6) | 1433 (3.5) | |
| Retired | 3471 (13.8) | 3420 (20.9) | 6891 (16.6) | |
| Other | 2025 (8.1) | 891 (5.5) | 2916 (7.0) | |
| Working at | 0.000 | |||
| Workplace | 7798 (46.6) | 4479 (41.3) | 12,277 (44.5) | |
| Home and workplace | 6188 (37.0) | 4270 (39.3) | 10,458 (37.9) | |
| Home | 2746 (16.4) | 2106 (19.4) | 4852 (17.6) | |
| Work category at risk for the infection | 0.000 | |||
| No | 10,242 (61.2) | 8331 (76.7) | 18,573 (67.3) | |
| Personnel who work indoors with high turnout | 896 (5.4) | 477 (4.4) | 1373 (5.0) | |
| School staff | 2880 (17.2) | 773 (7.1) | 3653 (13.2) | |
| Healthcare workers | 2572 (15.4) | 951 (8.8) | 3523 (12.8) | |
| Other (armed forces, haidressers, pilots, etc) | 142 (0.8) | 323 (3.0) | 465 (1.7) | |
| Deprivation Score b | 0.000 | |||
| Zero | 15,005 (59.7) | 10,368 (63.5) | 25,373 (61.2) | |
| One | 8248 (32.8) | 4995 (30.6) | 13,243 (31.9) | |
| Two | 1704 (6.8) | 893 (5.5) | 2597 (6.3) | |
| Three | 182 (0.7) | 68 (0.4) | 250 (0.6) | |
| Four | 7 (0.0) | 3 (0.0) | 10 (0.0) | |
| Body Mass Index | 23.6 ± 4.0 | 25.6 ± 3.5 | 0.000 | 24.4 ± 3.9 |
| N° of morbidities | 0.000 | |||
| None | 15,369 (61.1) | 10,660 (65.3) | 26,029 (62.8) | |
| One | 6042 (24.0) | 3553 (21.8) | 9595 (23.1) | |
| Two | 2416 (9.6) | 1389 (8.5) | 3805 (9.2) | |
| Three or more | 1319 (5.2) | 725 (4.4) | 2044 (4.9) | |
| Smoking habit | 0.000 | |||
| No | 14,939 (59.4) | 8979 (55.0) | 23,918 (57.7) | |
| Former smoker | 5538 (22.0) | 4545 (27.8) | 10,083 (24.3) | |
| Current smoker | 4669 (18.6) | 2803 (17.2) | 7472 (18.0) | |
| Frequency of alcohol beverages between meals | 0.000 | |||
| Never | 5739 (22.8) | 2043 (12.5) | 7782 (18.8) | |
| <5 times a month | 11,409 (45.4) | 6763 (41.4) | 18,172 (43.8) | |
| 2–3 times a week | 4240 (16.9) | 3337 (20.4) | 7577 (18.3) | |
| 4–5 times a week | 2033 (8.1) | 1794 (11.0) | 3827 (9.2) | |
| 6+ times a week | 1725 (6.9) | 2390 (14.6) | 4115 (9.9) | |
| Self-perceived health status | ||||
| Bad or very bad | 418 1.7) | 221 (1.4) | 0.000 | 639 (1.5) |
| Adequate | 5263 (20.9) | 2941 (18.0) | 8204 (19.8) | |
| Good or very good | 19,465 (77.4) | 13,165 (80.6) | 32,630 (78.7) | |
| Sleep problems c | 2509 (10.0) | 850 (5.2) | 0.000 | 3359 (8.1) |
| Perceived stress d | 0.000 | |||
| Low | 10,748 (44.1) | 9550 (61.5) | 20,298 (50.9) | |
| Moderate | 12,445 (51.1) | 5633 (36.3) | 18,078 (45.3) | |
| High | 1168 (4.8) | 343 (2.2) | 1511 (3.8) | |
| Fear about COVID-19 pandemic (mean ± SD) e | 8.6 ± 3.6 | 7.9 ± 3.5 | 0.000 | 8.4 ± 3.6 |
| Feeling to be sufficiently informed about COVID-19 | 23,443 (93.2) | 15,200 (93.1) | 0.607 | 38,643 (93.2) |
| Sex at Birth | ||||
|---|---|---|---|---|
| Females n = 25,146 (60.6) | Males n = 16,327 (39.4) | p-Value | Total n = 41,473 (100) | |
| n (%) | n (%) | n (%) | ||
| Close contact with COVID-19 cases | 0.000 | |||
| No | 17,356 (69.0) | 11,944 (73.2) | 29,300 (70.6) | |
| Yes, wearing a face mask | 4630 (18.4) | 2504 (15.3) | 7134 (17.2) | |
| Yes, at least once without wearing a face mask | 3160 (12.6) | 1879 (11.5) | 5039 (12.2) | |
| Quarantine or self-isolation | 0.000 | |||
| Never | 17,441 (69.4) | 11,834 (72.5) | 29,275 (70.6) | |
| Once | 6500 (25.8) | 3768 (23.1) | 10,268 (24.8) | |
| More than once | 1205 (4.8) | 725 (4.4) | 1930 (4.7) | |
| NPS test for SARS-CoV-2 ^ * | 0.000 | |||
| Not done | 11,592 (46.1) | 8004 (49.0) | 19,596 (47.3) | |
| Yes, always negative | 11,792 (46.9) | 7183 (44.0) | 18,975 (45.8) | |
| Yes, positive at least once | 1762 (7.0) | 1140 (7.0) | 2902 (7.0) | |
| If tested, number of NPS | 0.071 | |||
| 1 | 5715 (42.2) | 3615 (43.4) | 9330 (42.6) | |
| 2 | 3129 (23.1) | 1948 (23.4) | 5077 (23.2) | |
| 3 | 1902 (14.0) | 1148 (13.8) | 3050 (13.9) | |
| 4+ | 2808 (20.7) | 1612 (19.4) | 4420 (20.2) | |
| Molecular NPS test type | 1590 (90.2) | 995 (87.3) | 0.030 | 2585 (89.1) |
| NPS test performed for free | 1405 (79.7) | 870 (76.3) | 0.029 | 2275 (78.4) |
| Reasons for the positive NPS test performed | ||||
| Presence of symptoms | 1124 (63.8) | 748 (65.6) | 0.316 | 1872 (64.5) |
| Contact with COVID-19 case | 827 (46.9) | 455 (39.9) | 0.000 | 1282 (44.2) |
| Check at workplace | 205 (11.6) | 93 (8.2) | 0.003 | 298 (10.3) |
| Own choice | 79 (4.5) | 77 (6.8) | 0.008 | 156 (5.4) |
| Other reasons | 86 (4.9) | 69 (6.1) | 0.170 | 155 (5.3) |
| Places attended two weeks before the positive NPS test | ||||
| School | 215 (12.2) | 54 (4.7) | 0.000 | 269 (9.3) |
| Bar/restaurants | 408 (23.2) | 373 (32.7) | 0.000 | 781 (26.9) |
| Gym/swimming pool/club/discotheques | 125 (7.1) | 84 (7.4) | 0.780 | 209 (7.2) |
| Churches | 175 (9.9) | 98 (8.6) | 0.229 | 273 (9.4) |
| Hairdresser/aesthetic centre | 223 (12.7) | 45 (3.9) | 0.000 | 268 (9.2) |
| Theatres/cinemas/museum | 35 (2.0) | 23 (2.0) | 0.953 | 58 (2.0) |
| Parties (friends, family) | 298 (16.9) | 241 (21.1) | 0.004 | 539 (18.6) |
| Public transports>3 times/week | 132 (7.5) | 82 (7.2) | 0.764 | 214 (7.4) |
| Shared workplace | 759 (43.1) | 440 (38.6) | 0.017 | 1199 (41.3) |
| Hospitalization after NPS positive test | 180 (10.2) | 179 (15.7) | 0.000 | 359 (12.4) |
| ST for SARS-CoV-2 ** | 0.000 | |||
| Not done | 14,054 (55.9) | 10,025 (61.4) | 24,079 (58.1) | |
| Yes, always negative | 9788 (38.9) | 5533 (33.9) | 15,321 (36.9) | |
| Yes, positive at least once | 1304 (5.2) | 769 (4.7) | 2073 (5.0) | |
| Reasons for the positive ST performed | ||||
| Check at workplace | 450 (34.5) | 188 (24.4) | 0.000 | 638 (30.8) |
| Own choice | 594 (45.6) | 440 (57.2) | 0.000 | 1034 (49.9) |
| Other reasons | 311 (23.8) | 168 (21.8) | 0.296 | 479 (23.1) |
| Vaccinated for COVID-19 at 2nd interview | 0.000 | |||
| No | 21,967 (87.4) | 14,853 (91.0) | 36,820 (88.8) | |
| Yes, only the first dose | 1540 (6.1) | 742 (4.5) | 2282 (5.5) | |
| Yes, both doses | 1639 (6.5) | 732 (4.5) | 2371 (5.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adorni, F.; Jesuthasan, N.; Perdixi, E.; Sojic, A.; Giacomelli, A.; Noale, M.; Trevisan, C.; Franchini, M.; Pieroni, S.; Cori, L.; et al. Epidemiology of SARS-CoV-2 Infection in Italy Using Real-World Data: Methodology and Cohort Description of the Second Phase of Web-Based EPICOVID19 Study. Int. J. Environ. Res. Public Health 2022, 19, 1274. https://doi.org/10.3390/ijerph19031274
Adorni F, Jesuthasan N, Perdixi E, Sojic A, Giacomelli A, Noale M, Trevisan C, Franchini M, Pieroni S, Cori L, et al. Epidemiology of SARS-CoV-2 Infection in Italy Using Real-World Data: Methodology and Cohort Description of the Second Phase of Web-Based EPICOVID19 Study. International Journal of Environmental Research and Public Health. 2022; 19(3):1274. https://doi.org/10.3390/ijerph19031274
Chicago/Turabian StyleAdorni, Fulvio, Nithiya Jesuthasan, Elena Perdixi, Aleksandra Sojic, Andrea Giacomelli, Marianna Noale, Caterina Trevisan, Michela Franchini, Stefania Pieroni, Liliana Cori, and et al. 2022. "Epidemiology of SARS-CoV-2 Infection in Italy Using Real-World Data: Methodology and Cohort Description of the Second Phase of Web-Based EPICOVID19 Study" International Journal of Environmental Research and Public Health 19, no. 3: 1274. https://doi.org/10.3390/ijerph19031274
APA StyleAdorni, F., Jesuthasan, N., Perdixi, E., Sojic, A., Giacomelli, A., Noale, M., Trevisan, C., Franchini, M., Pieroni, S., Cori, L., Mastroianni, C. M., Bianchi, F., Antonelli-Incalzi, R., Maggi, S., Galli, M., Prinelli, F., & on behalf of the EPICOVID19 Working Group. (2022). Epidemiology of SARS-CoV-2 Infection in Italy Using Real-World Data: Methodology and Cohort Description of the Second Phase of Web-Based EPICOVID19 Study. International Journal of Environmental Research and Public Health, 19(3), 1274. https://doi.org/10.3390/ijerph19031274











