Neighborhood Poverty in Combination with Older Housing Is Associated with Adverse Birth Outcomes: A Study on Ubiquitous Lead Risk among 1 Million Births in Texas
Abstract
:1. Introduction
2. Materials and Methods
2.1. Individual Measures
2.2. Neighborhood Measures
2.3. Analyses
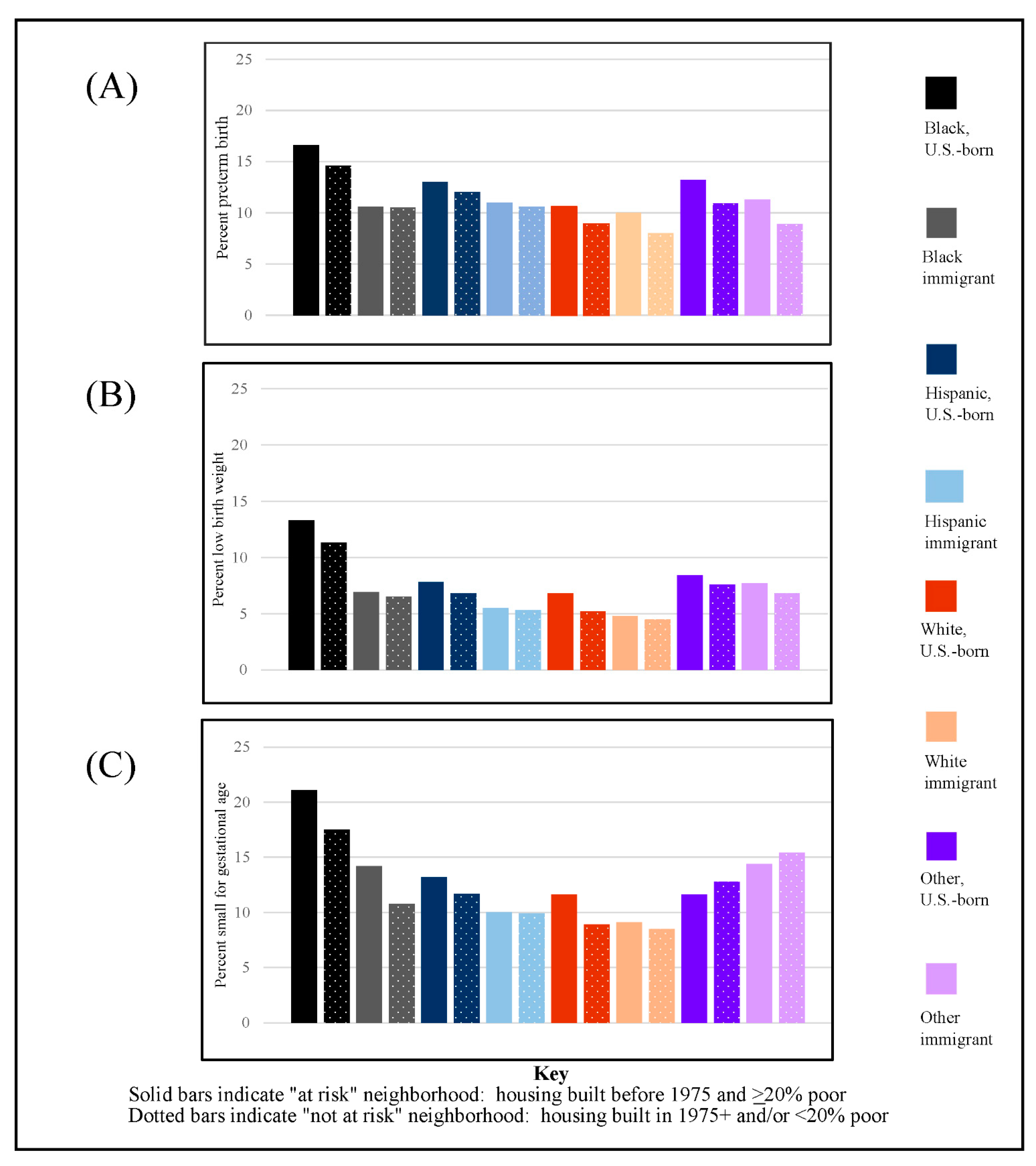
3. Results
4. Discussion
4.1. Testing and Addressing Ubiquitous Lead Risk
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Characteristic | Bivariate Models | Demographic Model | Full Model |
|---|---|---|---|
| Child’s sex | |||
| Female | 1.17 (1.15–1.19) | 1.17 (1.15–1.19) | 1.18 (1.16–1.190) |
| Male | 1 | 1 | 1 |
| Mother’s age (range 11–57) | |||
| 11–19 | 1.33 (1.30–1.36) | 1.01 (0.98–1.03) | 0.89 (0.87–0.92) |
| 20–34 | 1 | 1 | 1 |
| 35+ | 1.17 (1.15–1.20) | 1.32 (1.29–1.35) | 1.40 (1.36–1.43) |
| Mother’s race/ethnicity/nativity | |||
| Black, U.S.-born | 2.36 (2.30–2.42) | 2.16 (2.11–2.22) | 2.02 (1.96–2.07) |
| Black, immigrant | 1.24 (1.15–1.33) | 1.24 (1.15–1.33) | 1.19 (1.10–1.29) |
| Hispanic, U.S.-born | 1.32 (1.30–1.35) | 1.25 (1.22–1.28) | 1.16 (1.13–1.19) |
| Hispanic, immigrant | 0.99 (0.97–1.02) | 0.98 (0.95–1.00) | 0.82 (0.80–0.85) |
| White, U.S.-born | 1 | 1 | 1 |
| White, immigrant | 0.85 (0.79–0.91) | 0.85 (0.79–0.92) | 0.88 (0.81–0.95) |
| Other, U.S.-born | 1.48 (1.38–1.60) | 1.46 (1.36–1.58) | 1.47 (1.36–1.59) |
| Other, immigrant | 1.34 (1.28–1.40) | 1.37 (1.31–1.43) | 1.41 (1.36–1.48) |
| Mother’s marital status | |||
| Unmarried | 1.44 (1.42–1.47) | 1.25 (1.23–1.28) | 1.09 (1.07–1.11) |
| Married | 1 | 1 | 1 |
| Parity | |||
| First birth | 1 | 1 | 1 |
| Second–fourth birth | 0.71 (0.70–0.72) | 0.73 (0.72–0.75) | 0.70 (0.69–0.71) |
| Fifth+ birth | 0.94 (0.91–0.98) | 0.91 (0.87–0.94) | 0.80 (0.77–0.83) |
| Mother’s education | |||
| Did not finish high school | 1.50 (1.46–1.53) | 1.40 (1.35–1.45) | |
| High school graduate | 1.46 (1.43–1.50) | 1.28 (1.23–1.32) | |
| Some college | 1.32 (1.29–1.36) | 1.16 (1.13–1.20) | |
| College graduate | 1 | 1 | |
| Father’s education | |||
| Missing | 2.01 (1.95–2.06) | 1.43 (1.38–1.49) | |
| Did not finish high school | 1.41 (1.37–1.45) | 1.28 (1.23–1.33) | |
| High school graduate | 1.48 (1.45–1.53) | 1.28 (1.24–1.33) | |
| Some college | 1.27 (1.23–1.30) | 1.13 (1.10–1.17) | |
| College graduate | 1 | 1 | |
| Delayed prenatal care | |||
| Yes | 1.13 (1.11–1.15) | 1.02 (1.00–1.04) | |
| No | 1 | 1 | |
| Urban/rural status | |||
| Urban | 0.95 (0.92–0.98) | 0.92 (0.89–0.95) | 0.97 (0.94–1.00) |
| Rural | 1 | 1 | 1 |
| Median housing age + high poverty, tract level | |||
| <1975 and ≥20% poor | 1.24 (1.21–1.28) | 1.14 (1.11–1.16) | 1.09 (1.07–1.11) |
| 1975+ and/or <20% poor | 1 | 1 | 1 |
| U0j | 0.018 | 0.013 | |
| -2LL | 488,982 | 463,575.8 | |
| AIC | 489,016 | 463,625.8 | |
| BIC | 489,127.2 | 463,789.4 |
| Characteristic | Bivariate Models | Demographic Model | Full Model |
|---|---|---|---|
| Child’s sex | |||
| Female | 1.60 (1.58–1.62) | 1.61 (1.59–1.63) | 1.61 (1.59–1.63) |
| Male | 1 | 1 | 1 |
| Mother’s age (range 11–57) | |||
| 11–19 | 1.43 (1.41–1.46) | 1.09 (1.06–1.11) | 0.97 (0.95–0.99) |
| 20–34 | 1 | 1 | 1 |
| 35+ | 0.86 (0.85–0.88) | 0.96 (0.94–0.98) | 1.01 (0.99–1.03) |
| Mother’s race/ethnicity/nativity | |||
| Black, U.S.-born | 2.19 (2.15–2.23) | 2.00 (1.95–2.04) | 1.88 (1.83–1.92) |
| Black, immigrant | 1.24 (1.17–1.31) | 1.31 (1.24–1.40) | 1.23 (1.16–1.31) |
| Hispanic, U.S.-born | 1.32 (1.30–1.34) | 1.23 (1.21–1.25) | 1.16 (1.14–1.18) |
| Hispanic, immigrant | 1.06 (1.04–1.08) | 1.08 (1.06–1.10) | 0.92 (0.90–0.94) |
| White, U.S.-born | 1 | 1 | 1 |
| White, immigrant | 0.94 (0.89–0.99) | 0.99 (0.94–1.05) | 1.00 (0.94–1.06) |
| Other, U.S.-born | 1.45 (1.37–1.54) | 1.43 (1.35–1.52) | 1.44 (1.35–1.53) |
| Other, immigrant | 1.82 (1.77–1.88) | 1.97 (1.91–2.03) | 2.00 (1.93–2.06) |
| Mother’s marital status | |||
| Unmarried | 1.47 (1.45–1.49) | 1.26 (1.25–1.28) | 1.11 (1.09–1.13) |
| Married | 1 | 1 | 1 |
| Parity | |||
| First birth | 1 | 1 | 1 |
| Second–fourth birth | 0.66 (0.66–0.67) | 0.71 (0.70–0.72) | 0.67 (0.66–0.68) |
| Fifth+ birth | 0.67 (0.66–0.70) | 0.73 (0.71–0.76) | 0.63 (0.61–0.66) |
| Mother’s education | |||
| Did not finish high school | 1.51 (1.48–1.54) | 1.39 (1.35–1.43) | |
| High school graduate | 1.48 (1.45–1.51) | 1.31 (1.28–1.35) | |
| Some college | 1.27 (1.25–1.30) | 1.16 (1.13–1.19) | |
| College graduate | 1 | 1 | |
| Father’s education | |||
| Missing | 1.81 (1.78–1.86) | 1.21 (1.18–1.25) | |
| Did not finish high school | 1.33 (1.30–1.36) | 1.11 (1.08–1.14) | |
| High school graduate | 1.38 (1.35–1.41) | 1.13 (1.10–1.16) | |
| Some college | 1.17 (1.15–1.20) | 1.04 (1.01–1.07) | |
| College graduate | 1 | 1 | |
| Delayed prenatal care | |||
| Yes | 1.32 (1.30–1.33) | 1.21 (1.19–1.22) | |
| No | 1 | 1 | |
| Urban/rural status | |||
| Urban | 0.92 (0.89–0.94) | 0.89 (0.87–0.91) | 0.92 (0.90–0.94) |
| Rural | 1 | 1 | 1 |
| Median housing age + high poverty, tract level | |||
| <1975 and ≥20% poor | 1.22 (1.20–1.25) | 1.11 (1.09–1.13) | 1.07 (1.05–1.09) |
| 1975+ and/or <20% poor | 1 | 1 | 1 |
| U0j | 0.015 | 0.012 | |
| -2LL | 708,798.7 | 674,979.4 | |
| AIC | 708,832.7 | 675,029.4 | |
| BIC | 708,943.9 | 675,193 |
References
- Hamilton, B.; Martin, J.A.; Osterman, M.J.K.; Rossen, L.M. Births: Provisional Data for 2018. National Center for Health Statistics (U.S.). Division of Vital Statistics. 2019. Available online: https://stacks.cdc.gov/view/cdc/78430 (accessed on 15 October 2021).
- Chehade, H.; Simeoni, U.; Guignard, J.-P.; Boubred, F. Preterm birth: Long term cardiovascular and renal consequences. Curr. Pediatr. Rev. 2018, 14, 219–226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathewson, K.J.; Chow, C.H.; Dobson, K.G.; Pope, E.I.; Schmidt, L.A.; Van Lieshout, R.J. Mental health of extremely low birth weight survivors: A systematic review and meta-analysis. Psychol. Bull. 2017, 143, 347–383. [Google Scholar] [CrossRef] [PubMed]
- Moster, D.; Lie, R.T.; Markestad, T. Long-term medical and social consequences of preterm birth. N. Engl. J. Med. 2008, 359, 262–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, J.A.; Hamilton, B.E.; Osterman, M.J.K.; Driscoll, A.K.; Drake, P. Births: Final Data for 2017. Natl. Vital. Stat. Rep. 2018, 67, 1–50. [Google Scholar] [PubMed]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Steer, P. The epidemiology of preterm labour. BJOG Int. J. Obstet. Gynaecol. 2005, 112, 1–3. [Google Scholar] [CrossRef]
- Vigeh, M.; Yokoyama, K.; Seyedaghamiri, Z.; Shinohara, A.; Matsukawa, T.; Chiba, M.; Yunesian, M. Blood lead at currently acceptable levels may cause preterm labour. Occup. Environ. Med. 2010, 68, 231–234. [Google Scholar] [CrossRef]
- Jelliffe-Pawlowski, L.L.; Miles, S.Q.; Courtney, J.G.; Materna, B.; Charlton, V. Effect of magnitude and timing of maternal pregnancy blood lead (Pb) levels on birth outcomes. J. Perinatol. 2006, 26, 154–162. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. Third National Report on Human Exposure to Environmental Chemicals; CDC: Atlanta, GA, USA, 2005; pp. 1–467. Available online: https://clu-in.org/download/contaminantfocus/pcb/third-report.pdf (accessed on 7 January 2021).
- Bonnefoy, X. Inadequate Housing and Health: An overview. Int. J. Environ. Pollut. 2007, 30, 411. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, D.E. Environmental health disparities in housing. Am. J. Public Health 2011, 101 (Suppl. 1), S115–S122. [Google Scholar] [CrossRef]
- Vivier, P.M.; Hauptman, M.; Weitzen, S.H.; Bell, S.; Quilliam, D.N.; Logan, J.R. The important health impact of where a child lives: Neighborhood characteristics and the burden of lead poisoning. Matern. Child Health J. 2010, 15, 1195–1202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bae, H. The impact of the residential lead paint disclosure rule on house prices: Findings in the American Housing Survey. J. Hous. Built Environ. 2015, 31, 19–30. [Google Scholar] [CrossRef]
- Wheeler, D.C.; Boyle, J.; Raman, S.; Nelson, E.J. Modeling elevated blood lead level risk across the United States. Sci. Total Environ. 2021, 769, 145237. [Google Scholar] [CrossRef]
- Griffith, D.A.; Doyle, P.G.; Wheeler, D.C.; Johnson, D.L. A tale of two swaths: Urban childhood blood-lead levels across Syracuse, New York. Ann. Assoc. Am. Geogr. 1998, 88, 640–665. [Google Scholar] [CrossRef]
- Barna, M. Momentum Builds Across the United States to Replace Lead Water Pipes. Am. J. Public Health 2019, 109, 1151. [Google Scholar] [CrossRef]
- Ferguson, K.K.; Chin, H.B. Environmental Chemicals and preterm birth: Biological mechanisms and the state of the science. Curr. Epidemiol. Rep. 2017, 4, 56–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, B.; Xia, W.; Li, Y.; Bassig, B.A.; Zhou, A.; Wang, Y.; Li, Z.; Yao, Y.; Hu, J.; Du, X.; et al. Prenatal exposure to lead in relation to risk of preterm low birth weight: A matched case–control study in China. Reprod. Toxicol. 2015, 57, 190–195. [Google Scholar] [CrossRef] [Green Version]
- Berkowitz, Z.; Price-Green, P.; Bove, F.J.; Kaye, W.E. Lead exposure and birth outcomes in five communities in Shoshone County, Idaho. Int. J. Hyg. Environ. Health 2006, 209, 123–132. [Google Scholar] [CrossRef]
- Cantonwine, D.; Hu, H.; Sánchez, B.N.; Lamadrid-Figueroa, H.; Smith, D.; Ettinger, A.S.; Mercado-García, A.; Hernández-Avila, M.; Wright, R.O.; Téllez-Rojo, M.M. Critical windows of fetal lead exposure. J. Occup. Environ. Med. 2010, 52, 1106–1111. [Google Scholar] [CrossRef] [Green Version]
- Behrman, R.E.; Butler, A.S. Preterm Birth: Causes, Consequences, and Prevention; The National Academies Press: Washington, DC, USA, 2007. [Google Scholar]
- Horner, J.M. Lead in House Paints–Still a Health Risk That Should Not Be Overlooked. Citeseer 2010, 3, 1. [Google Scholar]
- Aelion, C.M.; Davis, H.T. Blood lead levels in children in urban and rural areas: Using multilevel modeling to investigate impacts of gender, race, poverty, and the environment. Sci. Total Environ. 2019, 694, 133783. [Google Scholar] [CrossRef]
- Population, Land Area, and Percent Urban and Rural in 2010 and Changes from 2000 to 2010; U.S. Census Bureau: Washington, WA, USA, 2010.
- Sampson, R.J.; Winter, A.S. The racial ecology of lead poisoning: Toxic inequality in Chicago neighborhoods, 1995–2013. Du Bois Rev. Soc. Sci. Res. Race 2016, 13, 261–283. [Google Scholar] [CrossRef] [Green Version]
- Texas Department of State and Health Services. Vital Statistics Section, 2009–2011. Birth Certificate Data. Available online: https://www.dshs.texas.gov/vs/default.aspx (accessed on 8 January 2021).
- Alexander, G.R.; Himes, J.H.; Kaufman, R.B.; Mor, J.; Kogan, M. A United States national reference for fetal growth. Obs. Gynecol. 1996, 87, 163–168. [Google Scholar] [CrossRef]
- U.S. Census Bureau. American Community Survey, 2007–2011 American Community Survey 1-Year Estimates Median Year Structure Built. Available online: https://www.census.gov/programs-surveys/acs/data.html (accessed on 5 January 2021).
- U.S. Census Bureau. American Community Survey, 2006–2010 American Community Survey 1—Year Estimates Poverty. Available online: https://data.census.gov/cedsci/all?q=Income%20and%20Poverty (accessed on 1 January 2021).
- Fowler, T. A Brief History of Lead Regulation. In Science Progress Where Science, Technology, and Policy Meet; Center for American Progress: Washington, DC, USA, 2008. [Google Scholar]
- U.S. Department of Agriculture. Rural-Urban Continuum Codes, 2013 Rural-Urban Continuum Codes. Available online: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx (accessed on 9 December 2021).
- Oken, E.; Kleinman, K.P.; Rich-Edwards, J.; Gillman, M.W. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Vohra-Gupta, S.; Margerison, C.E.; Cubbin, C. Neighborhood Racial/Ethnic Composition Trajectories and Black-White Differences in Preterm Birth among Women in Texas. J. Urban Health 2020, 97, 37–51. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. Changes in Poverty Rates and Poverty Areas over Time: 2005 to 2019. Available online: https://www.census.gov/library/publications/2020/acs/acsbr20-08.html (accessed on 15 December 2021).
- Wang, J.; Xie, H.; Fisher, J.F. Multilevel Models: Applications Using SAS®. In Walter de Gruyter; Higher Education Press: Berlin, Germany, 2011. [Google Scholar]
- Hox, J.J.; Moerbeek, M.; Van de Schoot, R. Multilevel Analysis: Techniques and Applications; Routledge: London, UK, 2017. [Google Scholar]
- How San Antonio Segregated Its Schools—Folo Media. Echoes. Published 19 May 2021. Available online: https://hebfdn.org/echoes/san-antonio-segregated-schools/ (accessed on 10 October 2021).
- Tovar, A. San Antonio’s Redlining and Segregation. Methods of Historical Research: Spring 2020. Published online 1 April 2020. Available online: https://digitalcommons.tamusa.edu/hist4301_spring2020/1 (accessed on 14 December 2021).
- Marshall, A.T.; Betts, S.; Kan, E.C.; McConnell, R.; Lanphear, B.; Sowell, E.R. Association of lead-exposure risk and family income with childhood brain outcomes. Nat. Med. 2020, 26, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Lanphear, B.P.; Byrd, R.S.; Auinger, P.; Stanley, J. Schaffer. Community characteristics associated with elevated blood lead levels in children. Pediatrics 1998, 101, 264–271. [Google Scholar] [CrossRef]
- Jacobs, D.E.; Clickner, R.P.; Zhou, J.Y.; Viet, S.M.; Marker, D.A.; Rogers, J.W.; Zeldin, D.C.; Broene, P.; Friedman, W. The prevalence of lead-based paint hazards in US housing. Environ. Health Perspect. 2002, 110, A599–A606. [Google Scholar] [CrossRef] [Green Version]
- Marshall, A.T.; McConnell, R.; Lanphear, B.P.; Thompson, W.K.; Herting, M.M.; Sowell, E.R. Risk of lead exposure, subcortical brain structure, and cognition in a large cohort of 9-to 10-year-old children. PLoS ONE 2021, 16, e0258469. [Google Scholar] [CrossRef]
- Wheeler, D.C.; Raman, S.; Jones, R.M.; Schootman, M.; Nelson, E.J. Bayesian deprivation index models for explaining variation in elevated blood lead levels among children in Maryland. Spat. Spatio-Temporal Epidemiol. 2019, 30, 100286. [Google Scholar] [CrossRef]
- Raymond, J.; Wheeler, W.; Brown, M.J.; Centers for Disease Control and Prevention. Lead screening and prevalence of blood lead levels in children aged 1–2 years—Child blood lead surveillance system, United States, 2002–2010 and national health and nutrition examination survey, United States, 1999–2010. MMWR Suppl. 2014, 63, 36–42. [Google Scholar] [PubMed]
- Musewe, L. Spatial Data Analysis of Risk Factors for Infant Health in Allegheny County, Pennsylvania. Available online: https://proceedings.esri.com/library/userconf/proc01/professional/papers/pap675/p675.htm (accessed on 14 December 2021).
- Krieger, N.; van Wye, G.; Huynh, M.; Pamela, D.; Waterman, G.M.; Wenhui, L.R.; Gwynn, C.; Barbot, O.; Bassett, M.T. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017. Am. J. Public Health 2020, 110, 1046–1053. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.; Dominguez, T.P.; Burke, W.; Dolan, S.M.; Stevenson, D.K.; Jackson, F.M.; Collins, J.W.J.; Driscoll, D.A.; Haley, T.; Acker, J.; et al. Explaining the black-white disparity in preterm birth: A consensus statement from a multi-disciplinary scientific work group convened by the March of Dimes. Front. Reprod. Health 2021, 49, 3. [Google Scholar] [CrossRef]
- Alhusen, J.L.; Kelly, M.; Bower, E.E.; Sharps, P. Racial discrimination and adverse birth outcomes: An integrative review. J. Midwifery Womens Health 2016, 61, 707–720. [Google Scholar] [CrossRef] [PubMed]
- Chambers, B.D.; Baer, R.J.; McLemore, M.R.; Jelliffe-Pawlowski, L.L. Using index of concentration at the extremes as indicators of structural racism to evaluate the association with preterm birth and infant mortality—California, 2011–2012. J. Urban Health 2019, 96, 159–170. [Google Scholar] [CrossRef] [Green Version]
- Flores, M.E.; Simonsen, S.E.; Manuck, T.A.; Dyer, J.M.; Turok, D.K. The “Latina epidemiologic paradox”: Contrasting patterns of adverse birth outcomes in US-born and foreign-born Latinas. Womens Health Issues 2012, 22, e501–e507. [Google Scholar] [CrossRef]
- Ha, S.; Hu, H.; Roussos-Ross, D.; Haidong, K.; Roth, J.; Xu, X. The effects of air pollution on adverse birth outcomes. Environ. Res. 2014, 134, 198–204. [Google Scholar] [CrossRef] [Green Version]
- Sheldrake, S.; Stifelman, M. A case study of lead contamination cleanup effectiveness at Bunker Hill. Sci. Total Environ. 2003, 303, 105–123. [Google Scholar] [CrossRef]
- Schoof, R.A.; Johnson, D.L.; Handziuk, E.R.; Van Landingham, C.; Feldpausch, A.M.; Gallagher, A.E.; Dell, L.D.; Kephart, A. Assessment of blood lead level declines in an area of historical mining with a holistic remediation and abatement program. Environ. Res. 2016, 150, 582–591. [Google Scholar] [CrossRef] [Green Version]
- Chakraborty, J.; Collins, T.W.; Grineski, S.E.; Montgomery, M.C.; Hernandez, M. Montgomery, and Maricarmen Hernandez. Comparing disproportionate exposure to acute and chronic pollution risks: A case study in Houston, Texas. Risk Anal. 2014, 34, 2005–2020. [Google Scholar] [CrossRef]
- Environmental Protection Agency. Code, Rule. 73 FR 21692; Office of Federal Register, National Archives Administration: Washington, DC, USA, 2008.
- Schuch, L.; Curtis, A.; Davidson, J. Reducing lead exposure risk to vulnerable populations: A proactive geographic solution. Ann. Am. Assoc. Geogr. 2017, 107, 606–624. [Google Scholar] [CrossRef]

| Characteristic | % Distribution | % Preterm Birth | % Low Birth Weight | % Small-for-Gestational Age |
|---|---|---|---|---|
| Total | 10.4 | 6.8 | 11.3 | |
| Child’s sex | ||||
| Female | 48.9 | 10.4 | 7 | 13.7 |
| Male | 51.1 | 11.5 | 6.1 | 9.1 |
| Mother’s age (range 11–57) | ||||
| 11–19 | 12.5 | 12.8 | 8.3 | 15.3 |
| 20–34 | 75.3 | 10.3 | 6.2 | 11 |
| 35+ | 12.2 | 12.6 | 7 | 9.5 |
| Mother’s race/ethnicity | ||||
| Black, U.S.-born | 10.3 | 15.1 | 11.8 | 18.4 |
| Black, immigrant | 1.1 | 10.5 | 6.5 | 11.1 |
| Hispanic, U.S.-born | 26.8 | 12.3 | 7.1 | 12.1 |
| Hispanic, immigrant | 22.5 | 10.7 | 5.4 | 9.9 |
| White, U.S.-born | 32.6 | 9 | 5.3 | 9.2 |
| White, immigrant | 1.7 | 8.2 | 4.5 | 8.6 |
| Other, U.S.-born | 1 | 11.2 | 7.6 | 12.7 |
| Other, immigrant | 4 | 9 | 6.9 | 15.4 |
| Mother’s marital status | ||||
| Unmarried | 42.5 | 12.5 | 7.9 | 13.7 |
| Married | 57.5 | 9.7 | 5.5 | 9.6 |
| Parity | ||||
| First birth | 39.6 | 10.5 | 7.7 | 13.9 |
| Second–fourth birth | 56 | 10.9 | 5.7 | 9.7 |
| Fifth+ birth | 4.4 | 15.4 | 7.5 | 10.1 |
| Mother’s education | ||||
| Did not finish high school | 25.4 | 12.8 | 7.3 | 12.8 |
| High school graduate | 27 | 11.6 | 7.2 | 12.6 |
| Some college | 26.2 | 10.7 | 6.5 | 11 |
| College graduate | 21.5 | 8.1 | 4.9 | 8.7 |
| Father’s education | ||||
| Missing | 14.6 | 18.8 | 9.2 | 15.3 |
| Did not finish high school | 20.9 | 11.8 | 6.6 | 11.5 |
| High school graduate | 24.7 | 11.3 | 6.9 | 11.9 |
| Some college | 21 | 10.2 | 5.9 | 10.2 |
| College graduate | 18.9 | 7.9 | 4.7 | 8.8 |
| Delayed/no prenatal care | ||||
| Yes | 39.3 | 10.8 | 7 | 13.2 |
| No | 60.7 | 10.7 | 6.2 | 10.2 |
| Urban/rural status | ||||
| Urban | 66 | 10.9 | 6.5 | 11.3 |
| Rural | 34.1 | 11.7 | 6.9 | 12.2 |
| Median Housing age | ||||
| <1975 | 32.2 | 11.8 | 7.2 | 12.3 |
| 1975+ | 67.7 | 10.6 | 6.2 | 10.9 |
| Poverty level | ||||
| ≥20% poor | 38.5 | 12.3 | 7.3 | 12.5 |
| <20% poor | 61.5 | 10.1 | 6.1 | 10.6 |
| Median Housing age + poverty level | ||||
| <1975 and ≥20% poor | 19.4 | 12.5 | 7.7 | 13 |
| 1975+ and/or <20% poor | 80.6 | 10.6 | 6.3 | 11 |
| Characteristic | Bivariate Models | Demographic Model | Full Model |
|---|---|---|---|
| Child’s sex | |||
| Female | 0.89 (0.88–0.90) | 0.89 (0.88–0.90) | 0.89 (0.88–0.90) |
| Male | 1 | 1 | 1 |
| Mother’s age (range 11–57) | |||
| 11–19 | 1.22 (1.20–1.24) | 1.12 (1.10–1.15) | 1.03 (1.01–1.06) |
| 20–34 | 1 | 1 | 1 |
| 35+ | 1.30 (1.27–1.32) | 1.32 (1.30–1.35) | 1.38 (1.35–1.41) |
| Mother’s race/ethnicity/nativity | |||
| Black, U.S.-born | 1.75 (1.72–1.79) | 1.61 (1.58–1.65) | 1.53 (1.49–1.56) |
| Black, immigrant | 1.18 (1.12–1.26) | 1.16 (1.08–1.23) | 1.16 (1.09–1.24) |
| Hispanic, U.S.-born | 1.33 (1.31–1.36) | 1.25 (1.23–1.28) | 1.17 (1.15–1.19) |
| Hispanic, immigrant | 1.16 (1.13–1.18) | 1.08 (1.06–1.10) | 0.95 (0.93–0.97) |
| White, U.S.-born | 1 | 1 | 1 |
| White, immigrant | 0.91 (0.86–0.96) | 0.90 (0.85–0.96) | 0.93 (0.88–0.99) |
| Other, U.S.-born | 1.27 (1.20–1.35) | 1.27 (1.19–1.35) | 1.26 (1.18–1.35) |
| Other, immigrant | 1.01 (0.97–1.05) | 1.03 (0.99–1.07) | 1.07 (1.03–1.11) |
| Mother’s marital status | |||
| Unmarried | 1.28 (1.27–1.30) | 1.20 (1.18–1.22) | 1.09 (1.07–1.11) |
| Married | 1 | 1 | 1 |
| Parity | |||
| First birth | 1 | 1 | 1 |
| Second–Fourth birth | 1.03 (1.01–1.04) | 1.07 (1.05–1.08) | 1.03 (1.01–1.05) |
| Fifth+ birth | 1.49 (1.44–1.53) | 1.45 (1.40–1.49) | 1.32 (1.28–1.36) |
| Mother’s education | |||
| Did not finish high school | 1.58 (1.55–1.62) | 1.34 (1.31–1.38) | |
| High school graduate | 1.42 (1.39–1.45) | 1.20 (1.17–1.23) | |
| Some college | 1.31 (1.28–1.34) | 1.14 (1.11–1.17) | |
| College graduate | 1 | 1 | |
| Father’s education | |||
| Missing | 1.85 (1.81–1.89) | 1.43 (1.39–1.48) | |
| Did not finish high school | 1.51 (1.48–1.55) | 1.26 (1.22–1.29) | |
| High school graduate | 1.45 (1.41–1.48) | 1.24 (1.20–1.27) | |
| Some college | 1.30 (1.27–1.33) | 1.17 (1.14–1.21) | |
| College graduate | 1 | 1 | |
| Delayed prenatal care | |||
| Yes | 0.98 (0.97–0.99) | 0.88 (0.87–0.89) | |
| No | 1 | 1 | |
| Urban/rural status | |||
| Urban | 0.93 (0.91–0.96) | 0.92 (0.90–0.95) | 0.96 (0.93–0.98) |
| Rural | 1 | 1 | 1 |
| Median housing age + high poverty, tract level | |||
| <1975 & ≥20% poor | 1.23 (1.20–1.25) | 1.10 (1.08–1.12) | 1.07 (1.04–1.09) |
| 1975+ and/or <20% poor | 1 | 1 | 1 |
| U0j | 0.026 | 0.02 | |
| -2LL | 703,088.00 | 663,655.70 | |
| AIC | 703,122.00 | 663,705.70 | |
| BIC | 703,233.30 | 663,869.30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wood, B.M.; Cubbin, C. Neighborhood Poverty in Combination with Older Housing Is Associated with Adverse Birth Outcomes: A Study on Ubiquitous Lead Risk among 1 Million Births in Texas. Int. J. Environ. Res. Public Health 2022, 19, 1578. https://doi.org/10.3390/ijerph19031578
Wood BM, Cubbin C. Neighborhood Poverty in Combination with Older Housing Is Associated with Adverse Birth Outcomes: A Study on Ubiquitous Lead Risk among 1 Million Births in Texas. International Journal of Environmental Research and Public Health. 2022; 19(3):1578. https://doi.org/10.3390/ijerph19031578
Chicago/Turabian StyleWood, Bethany Marie, and Catherine Cubbin. 2022. "Neighborhood Poverty in Combination with Older Housing Is Associated with Adverse Birth Outcomes: A Study on Ubiquitous Lead Risk among 1 Million Births in Texas" International Journal of Environmental Research and Public Health 19, no. 3: 1578. https://doi.org/10.3390/ijerph19031578






