Effectiveness of a Tailored Fall-Prevention Program for Discharged Older Patients: A Multicenter, Preliminary, Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Trial Design
2.2. Participants
2.3. Randomization
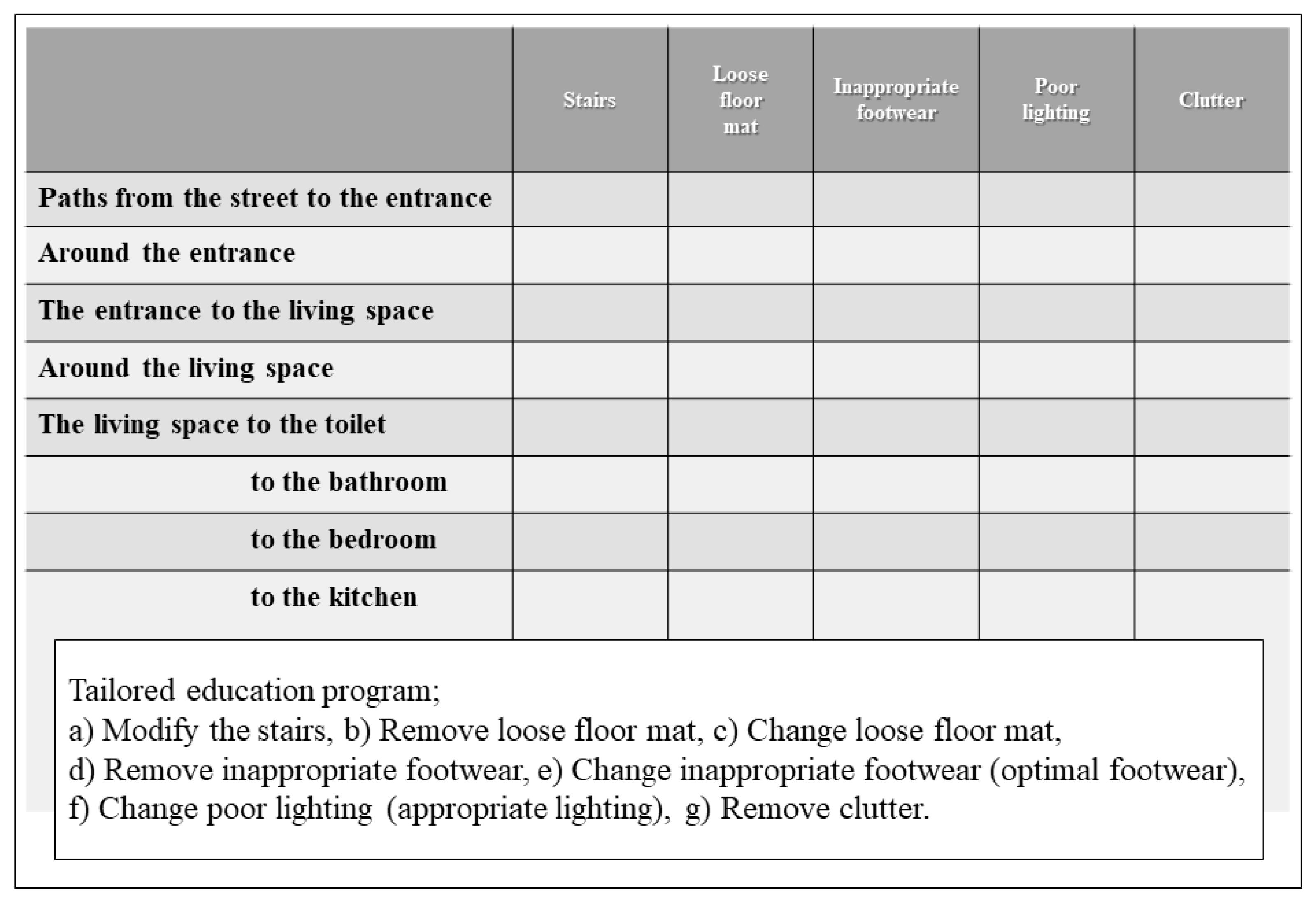
2.4. Interventions
2.5. Baseline Assessment
2.6. Follow-Up
2.7. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Falls (Primary Outcome)
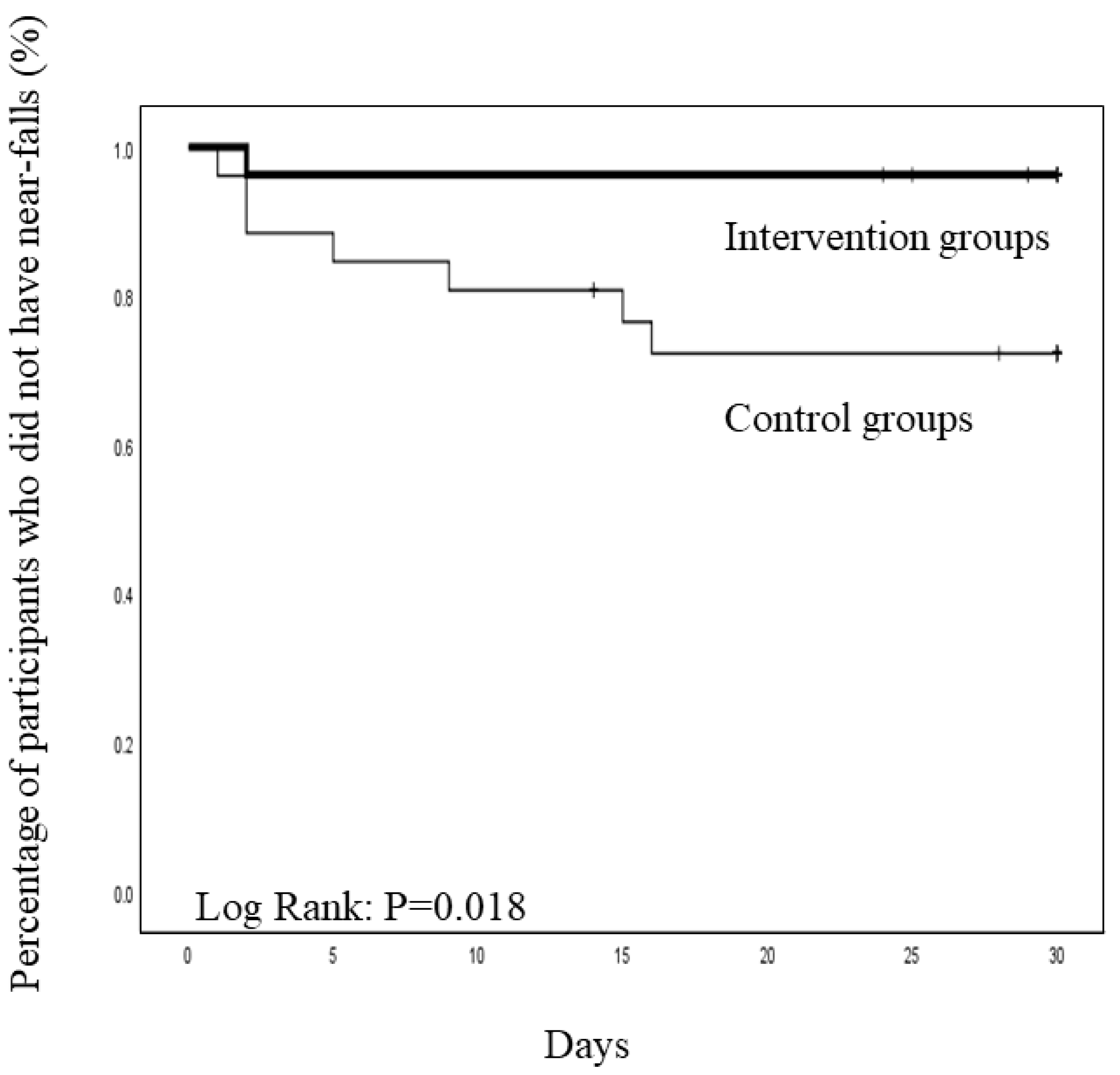
3.3. Near-Falls (Secondary Outcome)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hill, A.M.; Hoffmann, T.; Haines, T.P. Circumstances of falls and falls-related injuries in a cohort of older patients following hospital discharge. Clin. Interv. Aging 2013, 8, 765–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahoney, J.; Sager, M.; Dunham, N.C.; Johnson, J. Risk of falls after hospital discharge. J. Am. Geriatr. Soc. 1994, 42, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Matchar, D.B.; Duncan, P.W.; Lien, C.T.; Ong, M.E.H.; Lee, M.; Gao, F.; Sim, R.; Eom, K. Randomized controlled trial of screening, risk modification, and physical therapy to prevent falls among the elderly recently discharged from the emergency department to the community: The steps to avoid falls in the elderly study. Arch. Phys. Med. Rehabil. 2017, 98, 1086–1096. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Ciol, M.A.; Gruber, W.; Robinson, C. Incidence of and risk factors for falls following hip fracture in community-dwelling older adults. Phys. Ther. 2005, 85, 648–655. [Google Scholar] [CrossRef] [Green Version]
- Wolinsky, F.D.; Bentler, S.E.; Liu, L.; Obrizan, M.; Cook, E.A.; Wright, K.B.; Geweke, J.F.; Chrischilles, E.A.; Pavlik, C.E.; Ohsfeldt, R.L.; et al. Recent hospitalization and the risk of hip fracture among older Americans. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 249–255. [Google Scholar] [CrossRef]
- Close, J.; Ellis, M.; Hooper, R.; Glucksman, E.; Jackson, S.; Swift, C. Prevention of falls in the elderly trial (PROFET): A randomised controlled trial. Lancet 1999, 353, 93–97. [Google Scholar] [CrossRef]
- Day, L.; Fildes, B.; Gordon, I.; Fitzharris, M.; Flamer, H.; Lord, S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002, 325, 128. [Google Scholar] [CrossRef] [Green Version]
- Fu, A.S.; Gao, K.L.; Tung, A.K.; Tsang, W.W.; Kwan, M.M. Effectiveness of exergaming training in reducing risk and incidence of falls in frail older adults with a history of falls. Arch. Phys. Med. Rehabil. 2015, 96, 2096–2102. [Google Scholar] [CrossRef] [Green Version]
- Hansma, A.H.; Emmelot-Vonk, M.H.; Verhaar, H.J. Reduction in falling after a falls-assessment. Arch. Gerontol. Geriatr. 2010, 50, 73–76. [Google Scholar] [CrossRef]
- Hill, A.M.; McPhail, S.; Hoffmann, T.; Hill, K.; Oliver, D.; Beer, C.; Brauer, S.; Haines, T.P. A randomized trial comparing digital video disc with written delivery of falls prevention education for older patients in hospital. J. Am. Geriatr. Soc. 2009, 57, 1458–1463. [Google Scholar] [CrossRef] [Green Version]
- Hill, A.M.; Hoffmann, T.; McPhail, S.; Beer, C.; Hill, K.D.; Oliver, D.; Brauer, S.G.; Haines, T.P. Evaluation of the sustained effect of inpatient falls prevention education and predictors of falls after hospital discharge--follow-up to a randomized controlled trial. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 1001–1012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, A.M.; Etherton-Beer, C.; Haines, T.P. Tailored education for older patients to facilitate engagement in falls prevention strategies after hospital discharge—A pilot randomized controlled trial. PLoS ONE 2013, 8, e63450. [Google Scholar] [CrossRef]
- Keall, M.D.; Pierse, N.; Howden-Chapman, P.; Cunningham, C.; Cunningham, M.; Guria, J.; Baker, M.G. Home modifications to reduce injuries from falls in the home injury prevention intervention (HIPI) study: A cluster-randomised controlled trial. Lancet 2015, 385, 231–238. [Google Scholar] [CrossRef]
- Mirelman, A.; Rochester, L.; Maidan, I.; Del Din, S.; Alcock, L.; Nieuwhof, F.; Rikkert, M.O.; Bloem, B.R.; Pelosin, E.; Avanzino, L.; et al. Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): A randomised controlled trial. Lancet 2016, 388, 1170–1182. [Google Scholar] [CrossRef] [Green Version]
- Kenny, R.A.; Rubenstein, L.Z.; Tinetti, M.E.; Brewer, K.; Cameron, K.A.; Capezuti, E.A.; John, D.P.; Lamb, S.; Martin, F.; Rockey, P.H.; et al. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J. Am. Geriatr. Soc. 2011, 59, 148–157. [Google Scholar] [CrossRef] [Green Version]
- Pighills, A.C.; Torgerson, D.J.; Sheldon, T.A.; Drummond, A.E.; Bland, J.M. Environmental assessment and modification to prevent falls in older people. J. Am. Geriatr. Soc. 2011, 59, 26–33. [Google Scholar] [CrossRef]
- Sjösten, N.M.; Salonoja, M.; Piirtola, M.; Vahlberg, T.; Isoaho, R.; Hyttinen, H.; Aarnio, P.; Kivelä, S.L. A multifactorial fall prevention programme in home-dwelling elderly people: A randomized-controlled trial. Public Health 2007, 121, 308–318. [Google Scholar] [CrossRef]
- Stevens, M.; Holman, C.D.; Bennett, N.; de Klerk, N. Preventing falls in older people: Outcome evaluation of a randomized controlled trial. J. Am. Geriatr. Soc. 2001, 49, 1448–1455. [Google Scholar] [CrossRef]
- Tromp, A.M.; Pluijm, S.M.; Smit, J.H.; Deeg, D.J.; Bouter, L.M.; Lips, P. Fall-risk screening test: A prospective study on predictors for falls in community-dwelling elderly. J. Clin. Epidemiol. 2001, 54, 837–844. [Google Scholar] [CrossRef] [Green Version]
- Ueda, T.; Higuchi, Y.; Imaoka, M.; Todo, E.; Kitagawa, T.; Ando, S. Tailored education program using home floor plans for falls prevention in discharged older patients: A pilot randomized controlled trial. Arch. Gerontol. Geriatr. 2017, 71, 9–13. [Google Scholar] [CrossRef]
- Kamei, T.; Kajii, F.; Yamamoto, Y.; Irie, Y.; Kozakai, R.; Sugimoto, T.; Chigira, A.; Niino, N. Effectiveness of a home hazard modification program for reducing falls in urban community-dwelling older adults: A randomized controlled trial. Jpn. J. Nurs. Sci. 2015, 12, 184–197. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.M.; Faulkner, R.A. The history of falls and the association of the timed up and go test to falls and near-falls in older adults with hip osteoarthritis. BMC Geriatr. 2007, 7, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berg, W.P.; Alessio, H.M.; Mills, E.M.; Tong, C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing 1997, 26, 261–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lord, S.R.; Ward, J.A.; Williams, P.; Anstey, K.J. An epidemiological study of falls in older community-dwelling women: The Randwick falls and fractures study. Aust. J. Public Health 1993, 17, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Nagai, K.; Yamada, M.; Komatsu, M.; Tamaki, A.; Kanai, M.; Miyamoto, T.; Tsukagoshi, R.; Tsuboyama, T. Near falls predict substantial falls in older adults: A prospective cohort study. Geriatr. Gerontol. Int. 2017, 17, 1477–1480. [Google Scholar] [CrossRef] [PubMed]

| Control Group (n = 33) Mean ± SD | Intervention Group (n = 32) Mean ± SD | p-Value | |
|---|---|---|---|
| Age (years) | 77.9 ± 6.6 | 75.1 ± 6.8 | 0.095 † |
| Sex (female), n (%) | 25 (75.8) | 22 (68.8) | 0.528 * |
| Body mass index (kg/m2) | 21.8 ± 3.5 | 22.6 ± 3.6 | 0.385 † |
| Primary diseases, n (%) | 0.783 * | ||
| Upper limb disease | 2 (6.1) | 2 (6.3) | |
| Lower limb disease | 23 (69.7) | 22 (68.8) | |
| Trunk disease | 7 (21.2) | 8 (25.0) | |
| Upper and lower limb disease | 1 (3.0) | 0 (0) | |
| Comorbidities, n (%) | |||
| Hypertension | 15 (45.5) | 17 (53.1) | 0.536 * |
| Diabetes mellitus | 8 (24.2) | 10 (31.3) | 0.528 * |
| Chronic obstructive pulmonary disease | 0 (0) | 0 (0) | 1.000 * |
| Heart disease | 12 (36.4) | 7 (21.9) | 0.199 * |
| Stroke | 2 (6.1) | 2 (6.3) | 0.682 * |
| Musculoskeletal disease (aside from primary disease) | 5 (15.2) | 7 (21.9) | 0.485 * |
| Medication status, n (%) | |||
| Psychotropic drug | 0 (0) | 0 (0) | 1.000 * |
| Benzodiazepine | 1 (3.0) | 0 (0) | 0.508 * |
| Antidepressant | 1 (3.0) | 0 (0) | 0.508 * |
| Anticonvulsant | 0 (0) | 0 (0) | 1.000 * |
| Fall injury causing hospitalization, n (%) | 30 (90.9) | 29 (90.6) | 0.649 * |
| Number of falls in the past year (n) | 1.5 ± 1.8 | 1.8 ± 2.2 | 0.514 † |
| Living environment: alone, together, alone daytime (n) | 10/19/4 | 6/20/6 | 0.494 * |
| House environment: detached house (n) | 25 (75.8) | 27 (84.4) | 0.385 * |
| Certification for long-term care before admission, n (%) | 6 (18.2) | 3 (9.4) | 0.253 * |
| Sedentary time before hospitalization (hours/day) | 8.2 ± 5.5 | 6.4 ± 4.1 | 0.154 † |
| Walking ability prior to admission: walking alone, n (%) | 28 (84.4) | 29 (90.6) | 0.372 * |
| Length of hospital stay (days) | 29.2 ± 15.0 | 26.3 ± 13 | 0.397 † |
| Functional evaluation at discharge | |||
| Barthel Index (score) | 89.2 ± 11.3 | 93.4 ± 8.4 | 0.095 † |
| Timed Up and Go test(secs) | 17 ± 8.6 | 15.9 ± 13.3 | 0.708 † |
| Geriatric Depression Scale 5 (score) | 1.1 ± 1.3 | 0.8 ± 0.8 | 0.408 † |
| Modified Fall Efficacy Scale(scores) | 90.3 ± 36.7 | 95 ± 34.7 | 0.599 † |
| Walking ability at discharge: walking along, n (%) | 11 (33) | 14 (43.8) | 0.388 * |
| Control Group (n = 26) | Intervention Group (n = 27) | p-Value | |
|---|---|---|---|
| Participants who fell, n (%) | 1 (4.3) | 0 (0) | |
| Total falls, n | 1 | 0 | |
| Number of injuries due to falls, n | 0 | 0 | |
| Participants who nearly fell, n (%) | 7 (26.9) | 1 (3.7) | 0.022 * |
| Total near-falls, n | 42 | 1 | 0.175 † |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ueda, T.; Higuchi, Y.; Hattori, G.; Nomura, H.; Yamanaka, G.; Hosaka, A.; Sakuma, M.; Fukuda, T.; Fukumoto, T.; Nemoto, T. Effectiveness of a Tailored Fall-Prevention Program for Discharged Older Patients: A Multicenter, Preliminary, Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 1585. https://doi.org/10.3390/ijerph19031585
Ueda T, Higuchi Y, Hattori G, Nomura H, Yamanaka G, Hosaka A, Sakuma M, Fukuda T, Fukumoto T, Nemoto T. Effectiveness of a Tailored Fall-Prevention Program for Discharged Older Patients: A Multicenter, Preliminary, Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(3):1585. https://doi.org/10.3390/ijerph19031585
Chicago/Turabian StyleUeda, Tetsuya, Yumi Higuchi, Gentoku Hattori, Hiromi Nomura, Gen Yamanaka, Akiko Hosaka, Mina Sakuma, Takato Fukuda, Takanori Fukumoto, and Takashi Nemoto. 2022. "Effectiveness of a Tailored Fall-Prevention Program for Discharged Older Patients: A Multicenter, Preliminary, Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 3: 1585. https://doi.org/10.3390/ijerph19031585
APA StyleUeda, T., Higuchi, Y., Hattori, G., Nomura, H., Yamanaka, G., Hosaka, A., Sakuma, M., Fukuda, T., Fukumoto, T., & Nemoto, T. (2022). Effectiveness of a Tailored Fall-Prevention Program for Discharged Older Patients: A Multicenter, Preliminary, Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(3), 1585. https://doi.org/10.3390/ijerph19031585






