Evaluation of the Efficiency in Public Health Centers in Greece Regarding the Human Resources Occupied: A Bootstrap Data Envelopment Analysis Application
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Review
2.2. Model Specification—Data Envelopment Analysis
2.3. Data
3. Results
3.1. Efficiency of the Total Model (M0), Which Includes all Inputs and Outputs in the DEA Analysis under Both the CRS and VRS Assumptions
3.2. Different Models—To Study the Contribution of Human Resources to the Overall Efficiency of Health Centers
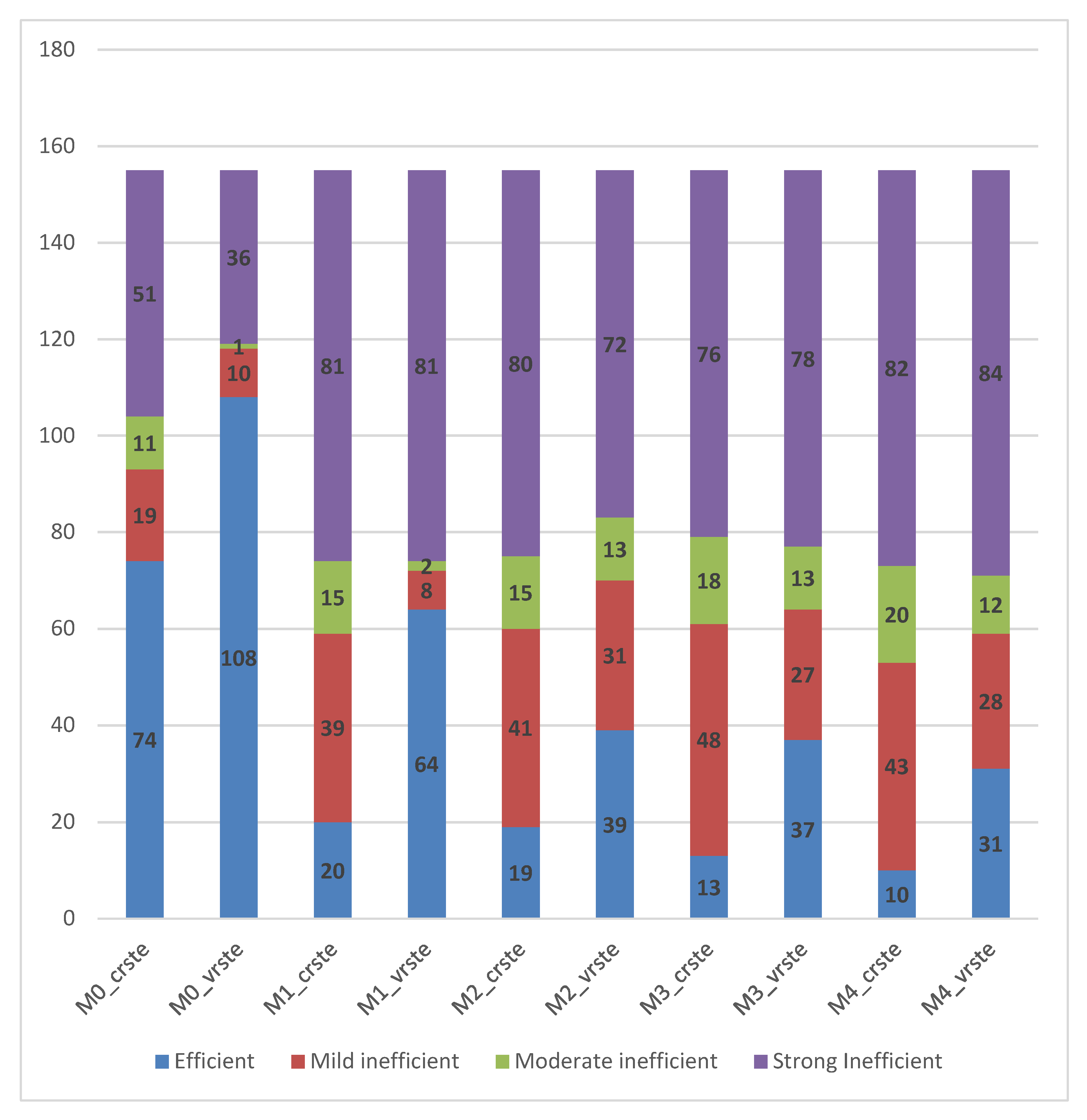
- Mild inefficiency: 1 > R ≥ Upper;
- Moderate inefficiency: Upper > IR ≥ Lower;
- Strong inefficiency: IR < Lower [11].
3.3. Model Validation—Internal Validity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| WHO | World Health Organization |
| OECD | Organization for Economic Co-operation and Development |
| PEDY | National Primary Health Care Network |
| ESY | Regional Health Care Authorities |
| TOMY | Local Health Unit |
| DEA | Data Envelopment Analysis |
| DMU | Decision-Making Unit |
| CRS | Constant Return to Scale |
| VRS | Variable Return to Scale |
References
- World Health Organization. Roadmap to Monitoring Health Services Delivery in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2017; Available online: https://www.euro.who.int/__data/assets/pdf_file/0007/355066/Roadmap-EFFA.pdf (accessed on 15 June 2017).
- Myloneros, T.; Sakellariou, D. The effectiveness of primary health care reforms in Greece towards achieving universal health coverage: A scoping review. BMC Health Serv. Res. 2021, 21, 628. [Google Scholar] [CrossRef] [PubMed]
- OECD/European Observatory on Health Systems and Policies. Greece: Country Health Profile 2017, State of Health in the EU; Paris/European Observatory on Health Systems and Policies; OECD Publishing: Brussels, Belgium, 2017. [Google Scholar]
- OECD/European Observatory on Health Systems and Policies. Greece: Country Health Profile 2019, State of Health in the EU; Paris/European Observatory on Health Systems and Policies; OECD Publishing: Brussels, Belgium, 2019. [Google Scholar]
- Androutsou, L.; Geitona, M.; Yfantopoulos, J.; Mehta, S. Measuring Efficiency and Productivity Across Hospitals in the Regional Health Authority of Thessaly, in Greece. J. Health Manag. 2011, 13, 121–140. [Google Scholar] [CrossRef]
- Tountas, Y.; Karnaki, P.; Pavi, E. Reforming the reform: The greek national health system in transition. Health Policy 2002, 62, 15–29. [Google Scholar] [CrossRef]
- Economou, C.; Giorno, C. Improving the Performance of the Public Health Care System in Greece; OECD Economics Department Working Papers 2009,722; OECD Publishing: Paris, France, 2009. [Google Scholar]
- Lionis, C.; Symvoulakis, E.K.; Markaki, A.; Vardavas, C.; Papadakaki, M.; Daniilidou, N.; Souliotis, K.; Kyriopoulos, I. Integrated primary health care in Greece, a missing issue in the current health policy agenda: A systematic review. Int. J. Integr. Care 2009, 9, e88. [Google Scholar] [CrossRef] [PubMed]
- Emmanouilidou, M. The 2017 Primary Health Care (PHC) reform in Greece: Improving access despite economic and professional constraints? Health Policy 2021, 125, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Trakakis, A.; Nektarios, M.; Tziaferi, S.; Prezerakos, P. Total productivity change of Health Centers in Greece in 2016–2018: A Malmquist index data envelopment analysis application for the primary health system of Greece. Cost Eff. Resour. Alloc. 2021, 19, 72. [Google Scholar] [CrossRef] [PubMed]
- Vrabková, I.; Vaňková, I. Efficiency of Human Resources in Public Hospitals: An Example from the Czech Republic. Int. J. Environ. Res. Public Health 2021, 18, 4711. [Google Scholar] [CrossRef]
- Seiford, L.M.; Thrall, R.M. Recent developments in DEA: The mathematical programming approach to frontier analysis. J. Econ. 1990, 46, 7–38. [Google Scholar] [CrossRef]
- Worthington, A. Frontier Efficiency Measurement in Health Care: A Review of Empirical Techniques and Selected Applications. Med. Care Res. Rev. 2004, 61, 135–170. [Google Scholar] [CrossRef] [Green Version]
- Dimas, G.; Goula, A.; Soulis, S. Productive performance and its components in Greek public hospitals. Oper. Res. 2012, 12, 15–27. [Google Scholar] [CrossRef]
- Farrell, M.J. The Measurement of Productive Efficiency. J. R. Stat. Soc. Ser. A Gen. 1957, 120, 253–290. [Google Scholar] [CrossRef]
- Debreu, G. The coefficient of resource utilization. Econometrica 1951, 19, 272–292. [Google Scholar] [CrossRef]
- Koopmans, T.C. Activity Analysis of Production and Allocation; Wiley: New York, NY, USA, 1951; pp. 33–97. [Google Scholar]
- Charnes, A.; Cooper, W.W.; Rhodes, E. Measuring the efficiency of decision making units. Eur. J. Oper. Res. 1978, 2, 429–444. [Google Scholar] [CrossRef]
- Hollingsworth, B.; Dawson, P.; Maniadakis, N. Efficiency measurement of health care: A review of non-parametric methods and applications. Health Care Manag. Sci. 1999, 2, 161–172. [Google Scholar] [CrossRef]
- Banker, R.D.; Charnes, A.; Cooper, W.W. Some Models for Estimating Technical and Scale Inefficiencies in Data Envelopment Analysis. Manag. Sci. 1984, 30, 1078–1092. [Google Scholar] [CrossRef] [Green Version]
- Trakakis, A.; Nektarios, M.; Tziaferi, S.; Prezerakos, P. Measuring Technical Efficiency of Health Centres in Greece: A Data Envelopment Analysis Application for the Primary Health System of Greece. Eur. Res. Stud. J. 2021, 24, 1333–1353. [Google Scholar]
- Fragkiadakis, G.; Doumpos, M.; Zopounidis, C.; Germain, C. Operational and economic efficiency analysis of public hospitals in Greece. Ann. Oper. Res. 2016, 247, 787–806. [Google Scholar] [CrossRef]
- Xenos, P.; Yfantopoulos, J.; Nektarios, M.; Polyzos, N.; Tinios, P.; Constantopoulos, A. Efficiency and productivity assessment of public hospitals in Greece during the crisis period 2009–2012. Cost Eff. Resour. Alloc. 2017, 15, 6. [Google Scholar] [CrossRef] [Green Version]
- Prezerakos, P.; Maniadakis, N.; Kaitelidou, D.; Kotsopoulos, N.; Yfantopoulos, J. Measuring Across Hospital Efficiency and Productivity: The Case of Second Regional Health Authority of Attica. Eur. Res. Stud. J. 2007, 10, 83–96. [Google Scholar]
- Daouia, A.; Simar, L. Nonparametric efficiency analysis: A multivariate conditional quantile approach. J. Econ. 2007, 140, 375–400. [Google Scholar] [CrossRef] [Green Version]
- Johnson, P.T.J.; Ostfeld, R.; Keesing, F. Frontiers in research on biodiversity and disease. Ecol. Lett. 2015, 18, 1119–1133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simar, L.; Wilson, P.W. Two-Stage Efficiency Analysis for Stata; FAU Discussion Papers in Economics; EconStor: Hamburg, Germany, 2018. [Google Scholar]
- Coelli, T.J. A Guide to DEAP Version 2.1: A Data Envelopment Analysis (Computer) Program; CEPA Working Paper 96/08; University of New England: Armidale, Australia, 1996. [Google Scholar]
- Wang, M.-L.; Fang, H.-Q.; Tao, H.-B.; Cheng, Z.-H.; Lin, X.; Cai, M.; Xu, C.; Jiang, S. Bootstrapping data envelopment analysis of efficiency and productivity of county public hospitals in Eastern, Central, and Western China after the public hospital reform. Curr. Med. Sci. 2017, 37, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Sarkis, J.; Talluri, S. A Model for Strategic Supplier Selection. J. Supply Chain Manag. 2002, 38, 18–28. [Google Scholar] [CrossRef]
- Sarkis, J. Preparing Your Data for DEA. In Modeling Data Irregularities and Structural Complexities in Data Envelopment Analysis; Springer: Boston, MA, USA, 2007; Volume 17, pp. 305–320. [Google Scholar]
- Färe, R.; Grosskopf, S. Modeling undesirable factors in efficiency evaluation: Comment. Eur. J. Oper. Res. 2004, 157, 242–245. [Google Scholar] [CrossRef]
- Grosskopf, S. Some Remarks on Productivity and its Decompositions. J. Prod. Anal. 2003, 20, 459–474. [Google Scholar] [CrossRef]
- Färe, R.; Grosskopf, S.; Norris, M.; Zhang, Z. Productivity growth, technical progress, and efficiency change in industrialized countries. Am. Econ. Rev. 1994, 84, 66–83. [Google Scholar]
- Grosskopf, S. Efficiency and Productivity. In The Measurement of Productive Efficiency: Techniques and Applications; Fried, H.O., Lovell, C.A.K., Schmidt, S.S., Eds.; Oxford University Press: New York, NY, USA, 1993; pp. 94–160. [Google Scholar]
- Reddy, G.T. Comparison and Correlation Coefficient between CRS and VRS models of OC Mines. Int. J. Ethics Eng. Manag. Educ. 2015, 2, 2348–4748. [Google Scholar]
- Ramakrishnan, M.; Chandrasekaran, R. Global Economic Crisis and Productivity Changes of Banks in India: A DEA-MPI Analysis. Int. J. Data Envel. Anal. Oper. Res. 2014, 1, 40–48. [Google Scholar] [CrossRef]
- Smith, P.; Ganley, J.A.; Cubbin, J.S. Public Sector Efficiency Measurements: Applications of Data Envelopment Analysis. J. Oper. Res. Soc. 1994, 45, 117. [Google Scholar] [CrossRef]
- Hollingsworth, B. Non-Parametric and Parametric Applications Measuring Efficiency in Health Care. Health Care Manag. Sci. 2003, 6, 203–218. [Google Scholar] [CrossRef]
- Parkin, D.; Hollingsworth, B. Measuring production efficiency of acute hospitals in Scotland, 1991–1994: Validity issues in data envelopment analysis. Appl. Econ. 1997, 29, 1425–1433. [Google Scholar] [CrossRef]
- Valdmanis, V. Sensitivity Analysis for DEA Models: An Empirical Example Using Public vs. NFP Hospitals. J. Public Econ. 1992, 48, 185–205. [Google Scholar] [CrossRef]
| N/N | Data | Description |
|---|---|---|
| Output_1 | Nursing operations | Average number applied (2016–2018) |
| Output_2 | Microsurgeries | Average number applied (2016–2018) |
| Output_3 | Dental procedures | Average number applied (2016–2018) |
| Output_4 | Chronic disease cases | Average number faced (2016–2018) |
| Output_5 | Emergencies | Average number faced (2016–2018) |
| Output_6 | Regular incidents | Average number faced (2016–2018) |
| Output_7 | Urgent incidents | Average number faced (2016–2018) |
| Output_8 | Transcriptions | Average number given (2016–2018) |
| Output_9 | Biopathological and laboratory exams | Average number applied (2016–2018) |
| Output_10 | Mantoux test | Average number applied (2016–2018) |
| Output_11 | Vaccinations for adults | Average number applied (2016–2018) |
| Output_12 | Vaccinations for kids and teenagers | Average number applied (2016–2018) |
| Input_1 | Number of managers | Average number employed (2016–2018) |
| Input_2 | Number of physicians | Average number employed (2016–2018) |
| Input_3 | Number of nursing staff | Average number employed (2016–2018) |
| Input_4 | Number of non-medical staff | Average number employed (2016–2018) |
| Data (Inputs-Outputs) | Minimum | Maximum | Mean | Std. Deviation |
|---|---|---|---|---|
| Nursing operations | 0 | 31,376 | 4177.67 | 4441.781 |
| Microsurgeries | 0 | 17,992 | 475.19 | 1526.713 |
| Dental procedures | 0 | 11,417 | 1191.77 | 1630.295 |
| Chronic disease cases | 0 | 34,036 | 4553.23 | 7154.341 |
| Emergency cases | 0 | 20,443 | 1664.09 | 2124.164 |
| Regular incidents | 0 | 56,402 | 13,645.38 | 9716.818 |
| Urgent incidents | 920 | 38,239 | 9129.65 | 7394.567 |
| Transcriptions | 0 | 61,460 | 11,679.42 | 8786.179 |
| Bio-pathological and Laboratory exams | 0 | 146,277 | 15,463.58 | 21,816.909 |
| Test Mantoux | 0 | 855 | 64.82 | 107.757 |
| Vaccinations applied for adults | 0 | 4155 | 498.87 | 605.530 |
| Vaccinations applied for Kids and teenagers | 0 | 2656 | 519.34 | 586.265 |
| Number of managers | 1 | 11 | 2.57 | 1.673 |
| Number of physicians | 2 | 32 | 9.46 | 6.360 |
| Number of nursing staff | 2 | 51 | 16.25 | 9.820 |
| Number of non-medical staff | 1 | 32 | 7.38 | 4.285 |
| Statistics | CRS | VRS |
|---|---|---|
| Arithmetic mean | 0.82046 | 0.93188 |
| Geometric mean | 0.82 | 0.932 |
| Std. Deviation | 0.234338 | 0.136112 |
| Minimum | 0.243 | 0.260 |
| Maximum | 1.000 | 1.000 |
| Model Type | CRS Total Model | VRS Total Model |
|---|---|---|
| CRS total model | 1.000 | 0.646 * |
| VRS total model | 0.646 * | 1.000 |
| Models/Variables | O1 | O2 | O3 | O4 | O5 | O6 | O7 | O8 | O9 | O10 | O11 | O12 | I1 | I2 | I3 | I4 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M0_CRS/VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ |
| M1_CRS/VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | |
| M2_CRS/VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | |
| M3_CRS/VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | |
| M4_CRS/VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ |
| Models | Stat. | Bootstrap * | ||||
|---|---|---|---|---|---|---|
| Bias | Std. Error | 95% Confidence Interval | ||||
| Lower | Upper | |||||
| MO_CRS | Mean | 0.82046 | −0.00027 | 0.01892 | 0.78254 | 0.85619 |
| Std. Deviation | 0.234338 | −0.000838 | 0.012096 | 0.208610 | 0.254964 | |
| MO_VRS | Mean | 0.93188 | −0.00034 | 0.01112 | 0.90906 | 0.95162 |
| Std. Deviation | 0.136112 | −0.000488 | 0.014381 | 0.108685 | 0.164017 | |
| M1_CRS | Mean | 0.49852 | −0.00059 | 0.02198 | 0.45914 | 0.54502 |
| Std. Deviation | 0.275431 | −0.001470 | 0.011573 | 0.250244 | 0.296290 | |
| M1_VRS | Mean | 0.68973 | −0.00023 | 0.02343 | 0.64653 | 0.73417 |
| Std. Deviation | 0.291907 | −0.000951 | 0.007704 | 0.275718 | 0.305765 | |
| M2_CRS | Mean | 0.57935 | 0.00051 | 0.02048 | 0.53783 | 0.62132 |
| Std. Deviation | 0.260694 | −0.000680 | 0.009663 | 0.239598 | 0.277406 | |
| M2_VRS | Mean | 0.68061 | 0.00053 | 0.01987 | 0.64151 | 0.72187 |
| Std. Deviation | 0.253099 | −0.000768 | 0.008542 | 0.235300 | 0.269455 | |
| M3_CRS | Mean | 0.49004 | −0.00007 | 0.02173 | 0.44610 | 0.53466 |
| Std. Deviation | 0.270005 | −0.001039 | 0.012431 | 0.244536 | 0.294106 | |
| M3_VRS | Mean | 0.57066 | −0.00001 | 0.02514 | 0.52114 | 0.61963 |
| Std. Deviation | 0.310264 | −0.001232 | 0.009881 | 0.290893 | 0.327554 | |
| M4_CRS | Mean | 0.42086 | 0.00000 | 0.02240 | 0.37935 | 0.46659 |
| Std. Deviation | 0.278288 | −0.000682 | 0.013285 | 0.250353 | 0.302795 | |
| M4_VRS | Mean | 0.51788 | −0.00002 | 0.02520 | 0.46881 | 0.56558 |
| Std. Deviation | 0.314267 | −0.001064 | 0.010558 | 0.292209 | 0.332964 | |
| Models | Efficiency | Mild | Moderate | Strong |
|---|---|---|---|---|
| M0_CRS | 74 | 19 | 11 | 51 |
| M0_VRS | 108 | 10 | 1 | 36 |
| M1_CRS | 20 | 39 | 15 | 81 |
| M1_VRS | 64 | 8 | 2 | 81 |
| M2_CRS | 19 | 41 | 15 | 80 |
| M2_VRS | 39 | 31 | 13 | 72 |
| M3_CRS | 13 | 48 | 18 | 76 |
| M3_VRS | 37 | 27 | 13 | 78 |
| M4_CRS | 10 | 43 | 20 | 82 |
| M4_VRS | 31 | 28 | 12 | 84 |
| Spearman’s Rho | M0_CRS | MO_VRS | M1_CRS | M1_VRS | M2_CRS | M2_VRS | M3_CRS | M3_VRS | M4_CRS | M4_VRS |
|---|---|---|---|---|---|---|---|---|---|---|
| M0_CRS | 1 | 0.646 ** | 0.624 ** | 0.214 ** | 0.645 ** | 0.612 ** | 0.701 ** | 0.711 ** | 0.740 ** | 0.686 ** |
| M0_VRS | 0.646 ** | 1 | 0.476 ** | 0.570 ** | 0.389 ** | 0.486 ** | 0.441 ** | 0.487 ** | 0.412 ** | 0.451 ** |
| M1_CRS | 0.624 ** | 0.476 ** | 1 | 0.719 ** | 0.486 ** | 0.474 ** | 0.489 ** | 0.520 ** | 0.454 ** | 0.432 ** |
| M1_VRS | 0.214 ** | 0.570 ** | 0.719 ** | 1 | 0.132 | 0.289 ** | 0.223 ** | 0.304 ** | 0.085 | 0.193 * |
| M2_CRS | 0.645 ** | 0.389 ** | 0.486 ** | 0.132 | 1 | 0.866 ** | 0.364 ** | 0.361 ** | 0.410 ** | 0.362 ** |
| M2_VRS | 0.612 ** | 0.486 ** | 0.474 ** | 0.289 ** | 0.866 ** | 1 | 0.370 ** | 0.446 ** | 0.412 ** | 0.457 ** |
| M3_CRS | 0.701 ** | 0.441 ** | 0.489 ** | 0.223 ** | 0.364 ** | 0.370 ** | 1 | 0.935 ** | 0.447 ** | 0.461 ** |
| M3_VRS | 0.711 ** | 0.487 ** | 0.520 ** | 0.304 ** | 0.361 ** | 0.446 ** | 0.935 ** | 1 | 0.494 ** | 0.557 ** |
| M4_CRS | 0.740 ** | 0.412 ** | 0.454 ** | 0.085 | 0.410 ** | 0.412 ** | 0.447 ** | 0.494 ** | 1 | 0.913 ** |
| M4_VRS | 0.686 ** | 0.451 ** | 0.432 ** | 0.193 * | 0.362 ** | 0.457 ** | 0.461 ** | 0.557 ** | 0.913 ** | 1 |
| Models/Variables | O1 | O2 | O3 | O4 | O5 | O6 | O7 | O8 | O9 | O10 | O11 | O12 | I1 | I2 | I3 | I4 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M0_VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ |
| M1_VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | |
| M2_VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | |
| M3_VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | |
| M4_VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | |
| M5_VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | ||
| M6_VRS | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ | Χ |
| Spearman’s Rho | M0_VRS | M1_VRS | M2_VRS | M3_VRS | M4_VRS | M5_VRS | M6_VRS |
|---|---|---|---|---|---|---|---|
| M0_VRS | 1 | 0.570 ** | 0.486 ** | 0.487 ** | 0.451 ** | 0.906 ** | 0.524 ** |
| M1_VRS | 0.570 ** | 1 | 0.289 ** | 0.304 ** | 0.193 * | 0.606 ** | 0.202 * |
| M2_VRS | 0.486 ** | 0.289 ** | 1 | 0.446 ** | 0.457 ** | 0.460 ** | 0.672 ** |
| M3_VRS | 0.487 ** | 0.304 ** | 0.446 ** | 1 | 0.557 ** | 0.434 ** | 0.661 ** |
| M4_VRS | 0.451 ** | 0.193 * | 0.457 ** | 0.557 ** | 1 | 0.386 ** | 0.370 ** |
| M5_VRS | 0.906 ** | 0.606 ** | 0.460 ** | 0.434 ** | 0.386 ** | 1 | 0.477 ** |
| M6_VRS | 0.524 ** | 0.202 * | 0.672 ** | 0.661 ** | 0.370 ** | 0.477 ** | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trakakis, A.; Nektarios, M.; Tziaferi, S.; Prezerakos, P. Evaluation of the Efficiency in Public Health Centers in Greece Regarding the Human Resources Occupied: A Bootstrap Data Envelopment Analysis Application. Int. J. Environ. Res. Public Health 2022, 19, 1597. https://doi.org/10.3390/ijerph19031597
Trakakis A, Nektarios M, Tziaferi S, Prezerakos P. Evaluation of the Efficiency in Public Health Centers in Greece Regarding the Human Resources Occupied: A Bootstrap Data Envelopment Analysis Application. International Journal of Environmental Research and Public Health. 2022; 19(3):1597. https://doi.org/10.3390/ijerph19031597
Chicago/Turabian StyleTrakakis, Anastasios, Miltiadis Nektarios, Styliani Tziaferi, and Panagiotis Prezerakos. 2022. "Evaluation of the Efficiency in Public Health Centers in Greece Regarding the Human Resources Occupied: A Bootstrap Data Envelopment Analysis Application" International Journal of Environmental Research and Public Health 19, no. 3: 1597. https://doi.org/10.3390/ijerph19031597
APA StyleTrakakis, A., Nektarios, M., Tziaferi, S., & Prezerakos, P. (2022). Evaluation of the Efficiency in Public Health Centers in Greece Regarding the Human Resources Occupied: A Bootstrap Data Envelopment Analysis Application. International Journal of Environmental Research and Public Health, 19(3), 1597. https://doi.org/10.3390/ijerph19031597






