Psychological and Physical Intimate Partner Aggression Are Associated with Broad and Specific Internalizing Symptoms during Pregnancy
Abstract
:1. Introduction
1.1. Intimate Partner Violence as a Risk Factor for Depression and Anxiety
1.2. Embracing a Hierarchical Framework of Internalizing Disorders
1.3. The Present Study
2. Materials and Methods
2.1. Measures
2.2. Data Analytic Approach
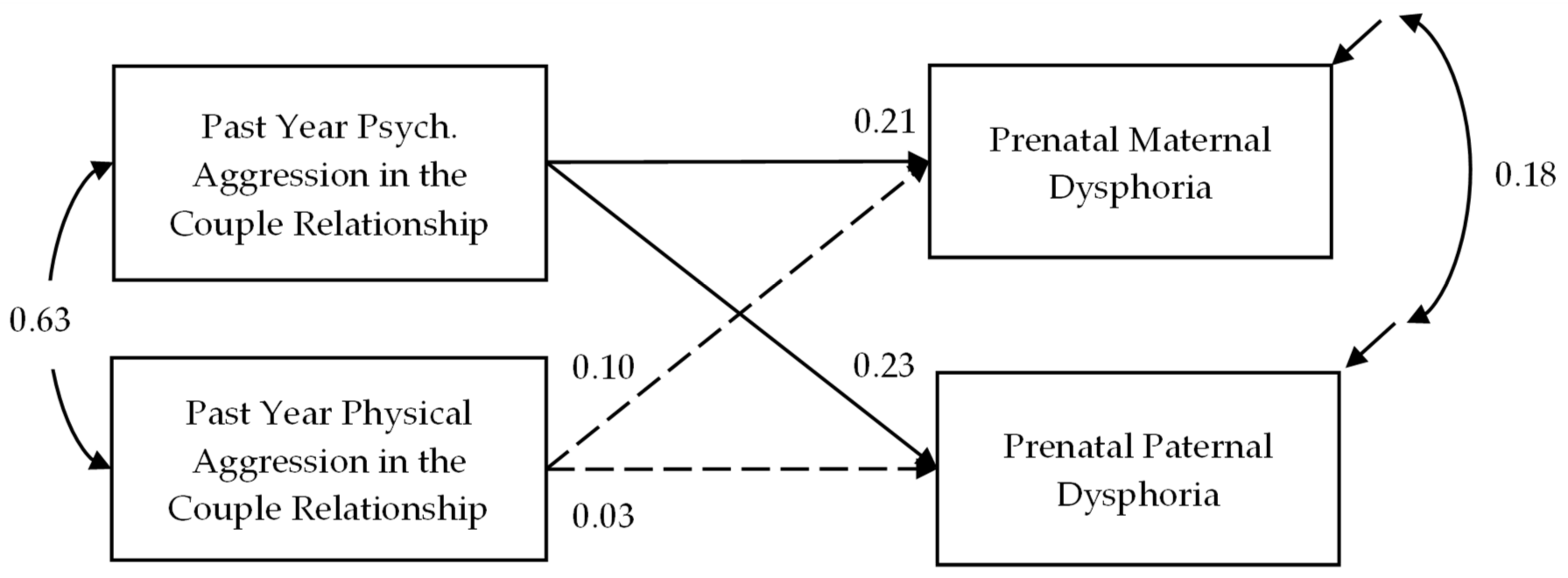
3. Results
4. Discussion
4.1. Limitations
4.2. Research Implications
4.3. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Garcia-Moreno, C.; Jansen, H.A.; Ellsberg, M.; Heise, L.; Watts, C.H. Prevalence of intimate partner violence: Findings from the WHO multi-country study on women’s health and domestic violence. Lancet 2006, 368, 1260–1269. [Google Scholar] [CrossRef]
- Mitchell, J.; Wight, M.; Van Heerden, A.; Rochat, T.J. Intimate partner violence, HIV, and mental health: A triple epidemic of global proportions. Int. Rev. Psychiatry 2016, 28, 452–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, S.G.; Zhang, X.; Basile, K.C.; Merrick, M.T.; Wang, J.; Kresnow, M.; Chen, J. The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data Brief—Updated Release; National Center for Injury Prevention and Control, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018. [Google Scholar]
- Lawrence, E.; Yoon, J.; Langer, A.; Ro, E. Is psychological aggression as detrimental as physical aggression? The independent effects of psychological aggression on depression and anxiety symptoms. Violence Vict. 2009, 24, 20–35. [Google Scholar] [CrossRef] [PubMed]
- Nathanson, A.M.; Shorey, R.C.; Tirone, V.; Rhatigan, D.L. The prevalence of mental health disorders in a sample of female victims of intimate partner violence. Partn. Abus. 2012, 3, 59–75. [Google Scholar] [CrossRef] [Green Version]
- Taft, C.T.; Torres, S.E.; Panuzio, J.; Murphy, M.; O’Farrell, T.J.; Monson, C.M.; Murphy, C.M. Examining the correlates of psychological aggression among a community sample of couples. J. Fam. Psychol. 2006, 20, 581–588. [Google Scholar] [CrossRef]
- Davis, E.P.; Narayan, A.J. Pregnancy as a period of risk, adaptation, and resilience for mothers and infants. Dev. Psychopathol. 2020, 32, 1625–1639. [Google Scholar] [CrossRef]
- Bailey, B.A.; Daugherty, R.A. Intimate partner violence during pregnancy: Incidence and associated health behaviors in a rural population. Matern. Child Health J. 2007, 11, 495–503. [Google Scholar] [CrossRef]
- Mojahed, A.; Alaidarous, N.; Kopp, M.; Pogarell, A.; Thiel, F.; Garthus-Niegel, S. Prevalence of intimate partner violence among intimate partners during the perinatal period: A narrative literature review. Front. Psychiatry 2021, 12, 601236. [Google Scholar] [CrossRef]
- Fairbrother, N.; Janssen, P.; Antony, M.M.; Tucker, E.; Young, A.H. Perinatal anxiety disorder prevalence and incidence. J. Affect. Disord. 2016, 200, 148–155. [Google Scholar] [CrossRef] [Green Version]
- O’Hara, M.W.; McCabe, J.E. Postpartum depression: Current status and future directions. Annu. Rev. Clin. Psychol. 2013, 9, 379–407. [Google Scholar] [CrossRef]
- Alhusen, J.L.; Ray, E.; Sharps, P.; Bullock, L. Intimate partner violence during pregnancy: Maternal and neonatal outcomes. J. Women’s Health 2015, 24, 100–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schetter, C.D.; Tanner, L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr. Opin. Psychiatry 2012, 25, 141–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Field, T. Prenatal depression effects on early development: A review. Infant Behav. Dev. 2011, 34, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health 2019, 15, 1745506519844044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cameron, E.E.; Sedov, I.D.; Tomfohr-Madsen, L.M. Prevalence of paternal depression in pregnancy and the postpartum: An updated meta-analysis. J. Affect. Disord. 2016, 206, 189–203. [Google Scholar] [CrossRef] [PubMed]
- Paulson, J.F.; Bazemore, S.D. Prenatal and postpartum depression in fathers and its association with maternal depression: A meta-analysis. JAMA 2010, 303, 1961–1969. [Google Scholar] [CrossRef] [PubMed]
- Román-Gálvez, R.M.; Martín-Peláez, S.; Martínez-Galiano, J.M.; Khan, K.S.; Bueno-Cavanillas, A. Prevalence of intimate partner violence in pregnancy: An umbrella review. Int. J. Environ. Res. Public Health 2021, 18, 707. [Google Scholar] [CrossRef]
- Lagdon, S.; Armour, C.; Stringer, M. Adult experience of mental health outcomes as a result of intimate partner violence victimisation: A systematic review. Eur. J. Psychotraumatol. 2014, 5, 24794. [Google Scholar] [CrossRef] [Green Version]
- Beach SR, H.; Kim, S.; Cercone-Keeney, J.; Gupta, M.; Arias, I.; Brody, G.H. Physical aggression and depressive symptoms: Gender asymmetry in effects? J. Soc. Pers. Relatsh. 2004, 21, 341–360. [Google Scholar] [CrossRef]
- Dillon, G.; Hussain, R.; Loxton, D.; Rahman, S. Mental and physical health and intimate partner violence against women: A review of the literature. Int. J. Fam. Med. 2013, 2013, 313909. [Google Scholar] [CrossRef]
- Lawrence, E.; Orengo-Aguayo, R.; Langer, A.; Brock, R.L. The impact and consequences of partner abuse on partners. Partn. Abus. 2012, 3, 406–428. [Google Scholar] [CrossRef]
- Castro, R.T.A.; Anderman, C.P.; Glover, V.; O’Connor, T.G.; Ehlert, U.; Kammerer, M. Associated symptoms of depression: Patterns of change during pregnancy. Arch. Women’s Health 2017, 20, 123–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alhusen, J.L.; Bullock, L.; Sharps, P.; Schminkey, D.; Comstock, E.; Campbell, J. Intimate partner violence during pregnancy and adverse neonatal outcomes in low-income women. J. Women’s Health 2014, 23, 920–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoon, J.E.; Lawrence, E. Psychological victimization as a risk factor in the developmental course of marriage. J. Fam. Psychol. 2013, 27, 53–64. [Google Scholar] [CrossRef]
- Kastello, J.C.; Jacobsen, K.H.; Gaffney, K.F.; Kodadek, M.P.; Sharps, P.W.; Bullock, L.C. Predictors of depression symptoms among low-income women exposed to perinatal intimate partner violence. Community Ment. Health J. 2016, 52, 683–690. [Google Scholar] [CrossRef]
- De Cock, E.S.A.; Henrichs, J.; Klimstra, T.A.; Janneke, B.M.; Maas, A.; Vreeswijk, C.M.J.M.; Meeus, W.H.J.; van Bakel, H.J.A. Longitudinal associations between parental bonding, parenting stress, and executive functioning in toddlerhood. J. Child Fam. Stud. 2017, 26, 1723–1733. [Google Scholar] [CrossRef] [Green Version]
- Fisher, S.D.; Cobo, J.; Figueiredo, B.; Fletcher, R.; Garfield, C.F.; Hanley, J.; Ramchandani, P.; Singley, D.B. Expanding the international conversation with fathers’ mental health: Toward an era of inclusion in perinatal research and practice. Arch. Women’s Ment. Health 2021, 24, 841–848. [Google Scholar] [CrossRef]
- Bates, E.A. Current controversies within intimate partner violence: Overlooking bidirectional violence. J. Fam. Violence 2016, 31, 937–940. [Google Scholar] [CrossRef]
- Capaldi, D.M.; Knoble, N.B.; Shortt, J.W.; Kim, H.K. A systematic review of risk factors for intimate partner violence. Partn. Abus. 2012, 3, 231–280. [Google Scholar] [CrossRef]
- Laifer, L.M.; DiLillo, D.; Brock, R.L. Prenatal negative affectivity and trauma-related distress predict mindful parenting during toddler age: Parent-infant bonding as a mechanism. Dev. Psychopathol. 2021, 1–15. [Google Scholar] [CrossRef]
- Saxbe, D.; Rossin-Slater, M.; Goldenberg, D. The transition to parenthood as a critical window for adult health. Am. Psychol. 2018, 73, 1190–1200. [Google Scholar] [CrossRef] [PubMed]
- Heron, J.; O’Connor, T.G.; Evans, J.; Golding, J.; Glover, V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J. Affect. Disord. 2004, 80, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Wai, T.C.; Jin, R.; Ruscio, A.M.; Shear, K.; Walters, E.E. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2006, 63, 415–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotov, R.; Krueger, R.F.; Watson, D.; Achenbach, T.M.; Althoff, R.R.; Bagby, R.M.; Brown, T.A.; Carpenter, W.T.; Caspi, A.; Clark, L.A.; et al. The Hierarchical Taxonomy Of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. J. Abnorm. Psychol. 2017, 126, 454–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraemer, H.C.; Noda, A.; O’Hara, R. Categorical versus dimensional approaches to diagnosis: Methodological challenges. J. Psychiatr. Res. 2004, 38, 17–25. [Google Scholar] [CrossRef]
- Jones, K.D. Dimensional and cross-cutting assessment in the DSM-5. J. Couns. Dev. 2012, 90, 481–487. [Google Scholar] [CrossRef]
- Chmielewski, M.; Clark, L.A.; Bagby, R.M.; Watson, D. Method matters: Understanding diagnostic reliability in DSM-IV and DSM-5. J. Abnorm. Psychol. 2015, 124, 764–769. [Google Scholar] [CrossRef]
- Krueger, R.F. The structure of common mental disorders. Arch. Gen. Psychiatry 1999, 56, 921–926. [Google Scholar] [CrossRef] [Green Version]
- Mineka, S.; Watson, D.; Clark, L.A. Comorbidity of anxiety and unipolar mood disorders. Annu. Rev. Psychol. 1998, 49, 377–412. [Google Scholar] [CrossRef] [Green Version]
- Slade, T.I.M.; Watson, D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychol. Med. 2006, 36, 1593–1600. [Google Scholar] [CrossRef]
- Watson, D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. J. Abnorm. Psychol. 2005, 114, 522–536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watson, D. Differentiating the mood and anxiety disorders: A quadripartite model. Annu. Rev. Clin. Psychol. 2009, 5, 221–247. [Google Scholar] [CrossRef] [PubMed]
- Cisler, J.M.; Begle, A.M.; Amstadter, A.B.; Resnick, H.S.; Danielson, C.K.; Saunders, B.E.; Kilpatrick, D.G. Exposure to interpersonal violence and risk for PTSD, depression, delinquency, and binge drinking among adolescents: Data from the NSA-R. J. Trauma. Stress 2012, 25, 33–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conway, C.C.; Forbes, M.K.; Forbush, K.T.; Fried, E.I.; Hallquist, M.N.; Kotov, R.; Mullins-Sweatt, S.N.; Shackman, A.J.; Skodol, A.E.; South, S.C.; et al. A hierarchical taxonomy of psychopathology can transform mental health research. Perspect. Psychol. Sci. 2019, 14, 419–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bailey, B.A. Partner violence during pregnancy: Prevalence, effects, screening, and management. Int. J. Women’s Health 2010, 2, 183–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koleva, H.; Stuart, S.; O’Hara, M.W.; Bowman-Reif, J. Risk factors for depressive symptoms during pregnancy. Arch. Women’s Ment. Health 2011, 14, 99–105. [Google Scholar] [CrossRef] [Green Version]
- Lancaster, C.A.; Gold, K.J.; Flynn, H.A.; Yoo, H.; Marcus, S.M.; Davis, M.M. Risk factors for depressive symptoms during pregnancy: A systematic review. Am. J. Obstet. Gynecol. 2010, 202, 5–14. [Google Scholar] [CrossRef] [Green Version]
- Vest, J.R.; Catlin, T.K.; Chen, J.J.; Brownson, R.C. Multistate analysis of factors associated with intimate partner violence. Am. J. Prev. Med. 2002, 22, 156–164. [Google Scholar] [CrossRef]
- Straus, M.A.; Douglas, E.M. A short form of the revised conflict tactics scales, and typologies for severity and mutuality. Violence Vict. 2004, 19, 507–520. [Google Scholar] [CrossRef]
- Kan, M.L.; Feinberg, M.E. Measurement and correlates of intimate partner violence among expectant first-time parents. Violence Vict. 2010, 25, 319–331. [Google Scholar] [CrossRef] [Green Version]
- Watson, D.; O’Hara, M.W.; Naragon-Gainey, K.; Koffel, E.; Chmielewski, M.; Kotov, R.; Stasik, S.M.; Ruggero, C.J. Development and validation of new anxiety and bipolar symptom scales for an expanded version of the IDAS (the IDAS-II). Assessment 2012, 19, 399–420. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.A.; Watson, D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. J. Abnorm. Psychol. 1991, 100, 316–336. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.; O’Hara, M.W.; Simms, L.J.; Kotov, R.; Chmielewski, M.; McDade-Montez, E.A.; Gamez, W.; Stuart, S. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychol. Assess. 2007, 19, 253–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watson, D.; O’Hara, M.W.; Chmielewski, M.; McDade-Montez, E.A.; Koffel, E.; Naragon, K.; Stuart, S. Further validation of the IDAS: Evidence of convergent, discriminant, criterion, and incremental validity. Psychol. Assess. 2008, 20, 248–259. [Google Scholar] [CrossRef]
- Stasik-O’Brien, S.M.; Brock, R.L.; Chmielewski, M.; Naragon-Gainey, K.; Koffel, E.; McDade-Montez, E.; O’Hara, M.W.; Watson, D. Clinical utility of the Inventory of Depression and Anxiety Symptoms (IDAS). Assessment 2019, 26, 944–960. [Google Scholar] [CrossRef]
- Nylen, K.J.; Williamson, J.A.; O’Hara, M.W.; Watson, D.; Engeldinger, J. Validity of somatic symptoms as indicators of depression in pregnancy. Arch. Women’s Ment. Health 2013, 16, 203–210. [Google Scholar] [CrossRef]
- Markon, K.E.; Brunette, C.A.; Whitney, B.M.; O’Hara, M.W. Mood during pregnancy: Trends, structure, and invariance by gestational day. J. Psychiatr. Res. 2021, 140, 260–266. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Enders, C.K. Applied Missing Data Analysis; Guilford Press: New York, NY, USA, 2010. [Google Scholar]
- Kenny, D.A.; Kashy, D.A.; Cook, W.L. Dyadic Data Analysis (Methodology in the Social Sciences); Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Becker, K.D.; Stuewig, J.; McCloskey, L.A. Traumatic stress symptoms of women exposed to different forms of childhood victimization and intimate partner violence. J. Interpers. Violence 2010, 25, 1699–1715. [Google Scholar] [CrossRef]
- Taft, C.T.; Creech, S.K.; Murphy, C.M. Anger and aggression in PTSD. Curr. Opin. Psychol. 2017, 14, 67–71. [Google Scholar] [CrossRef]
- Bosman, R.C.; ten Have, M.; de Graaf, R.; Muntingh, A.D.; van Balkom, A.J.; Batelaan, N.M. Prevalence and course of subthreshold anxiety disorder in the general population: A three-year follow-up study. J. Affect. Disord. 2019, 247, 105–113. [Google Scholar] [CrossRef]
- Karsten, J.; Penninx, B.W.; Verboom, C.E.; Nolen, W.A.; Hartman, C.A. Course and risk factors of functional impairment in subthreshold depression and anxiety. Depress. Anxiety 2013, 30, 386–394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.Y.; Stockings, E.A.; Harris, M.G.; Doi, S.A.R.; Page, I.S.; Davidson, S.K.; Barendregt, J.J. The risk of developing major depression among individuals with subthreshold depression: A systematic review and meta-analysis of longitudinal cohort studies. Psychol. Med. 2019, 49, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Cho, H. Racial differences in the prevalence of intimate partner violence against women and associated factors. J. Interpers. Violence 2012, 27, 344–363. [Google Scholar] [CrossRef] [PubMed]
- Cunradi, C.B.; Caetano, R.; Schafer, J. Socioeconomic predictors of intimate partner violence among White, Black, and Hispanic couples in the United States. J. Fam. Violence 2002, 17, 377–389. [Google Scholar] [CrossRef]
- Visschers, J.; Jaspaert, E.; Vervaeke, G. Social desirability in intimate partner violence and relationship satisfaction reports: An exploratory analysis. J. Interpers. Violence 2017, 32, 1401–1420. [Google Scholar] [CrossRef]
- Parfitt, Y.; Ayers, S. Transition to parenthood and mental health in first-time parents. Infant Ment. Health J. 2014, 35, 263–273. [Google Scholar] [CrossRef] [Green Version]
- Feinberg, M.E.; Jones, D.E.; Hostetler, M.L.; Roettger, M.E.; Paul, I.M.; Ehrenthal, D.B. Couple-focused prevention at the transition to parenthood, a randomized trial: Effects on coparenting, parenting, family violence, and parent and child adjustment. Prev. Sci. 2016, 17, 751–764. [Google Scholar] [CrossRef]
- Goedde, D.; Zidack, A.; Li, Y.; Arkava, D.; Mullette, E.; Mullowney, Y.; Brant, J.M. Depression outcomes from a fully integrated obstetric mental health clinic: A 10-year examination. J. Am. Psychiatr. Nurses Assoc. 2020, 27, 123–133. [Google Scholar] [CrossRef]
- Lomonaco-Haycraft, K.C.; Hyer, J.; Tibbits, B.; Grote, J.; Stainback-Tracy, K.; Ulrickson, C.; Lieberman, A.; van Bekkum, L.; Hoffman, M.C. Integrated perinatal mental health care: A national model of perinatal primary care in vulnerable populations. Prim. Health Care Res. Dev. 2019, 20, E77. [Google Scholar] [CrossRef] [Green Version]
- Stover, C.S.; Morgos, D. Fatherhood and intimate partner violence: Bringing the parenting role into intervention strategies. Prof. Psychol. Res. Pract. 2013, 44, 247–256. [Google Scholar] [CrossRef] [Green Version]
- Scott, K. Predictors of change among male batterers: Application of theories and review of empirical findings. Trauma Violence Abus. 2004, 5, 260–284. [Google Scholar] [CrossRef] [PubMed]
- Zarling, A.; Lawrence, E.; Marchman, J. A randomized controlled trial of Acceptance and Commitment Therapy for aggressive behavior. J. Consult. Clin. Psychol. 2015, 83, 199–212. [Google Scholar] [CrossRef] [PubMed]
| IDAS-II Scale | Maternal | Paternal | Paired t (df) | Paired r | ||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| Dysphoria | 17.03 | 5.07 | 16.37 | 5.83 | 1.24 (158) | 0.25 ** |
| Lassitude | 12.93 | 4.42 | 10.89 | 3.91 | 4.73 (158) ** | 0.15 |
| Insomnia | 14.08 | 4.95 | 11.12 | 4.70 | 5.59 (158) ** | 0.04 |
| Well-Being | 27.36 | 4.75 | 26.36 | 5.37 | 1.83 (158) | 0.07 |
| Ill Temper | 6.67 | 2.27 | 6.92 | 2.98 | −0.93 (158) | 0.17 * |
| Panic | 10.60 | 3.06 | 9.23 | 2.72 | 4.37 (158) ** | 0.06 |
| Social Anxiety | 8.16 | 3.24 | 8.59 | 3.59 | −1.17 (158) | 0.06 |
| Claustrophobia | 5.46 | 1.69 | 5.84 | 2.59 | −1.75 (158) | 0.25 ** |
| Traumatic Intrusions | 5.21 | 2.15 | 5.02 | 1.98 | 0.88 (158) | 0.15 |
| Traumatic Avoidance | 5.19 | 2.16 | 5.83 | 3.16 | −2.33 (158) * | 0.19 * |
| Maternal | Paternal | |||
|---|---|---|---|---|
| Psychological | Physical | Psychological | Physical | |
| Dysphoria | 0.27 ** | 0.24 ** | 0.28 ** | 0.19 * |
| Lassitude | 0.06 | 0.14 | 0.26 ** | 0.15 |
| Insomnia | −0.01 | 0.01 | 0.27 ** | 0.24 ** |
| Well-Being | −0.09 | −0.07 | −0.17 * | −0.14 |
| Ill Temper | 0.32 ** | 0.30 ** | 0.44 ** | 0.23 ** |
| Panic | 0.09 | 0.23 ** | 0.21 ** | 0.23 ** |
| Social Anxiety | 0.14 | 0.12 | 0.24 ** | 0.11 |
| Claustrophobia | 0.15 | 0.19 * | 0.22 ** | 0.11 |
| Traumatic Intrusions | 0.24 ** | 0.25 ** | 0.27 ** | 0.24 ** |
| Traumatic Avoidance | 0.23 ** | 0.26 ** | 0.32 ** | 0.20 * |
| Maternal | Paternal | |||||||
|---|---|---|---|---|---|---|---|---|
| b | SE | p-Value | β | b | SE | p-Value | β | |
| Lassitude | ||||||||
| Psychological | −0.03 | 0.06 | 0.583 | −0.06 | 0.11 | 0.05 | 0.019 | 0.24 |
| Physical | 1.69 | 1.45 | 0.245 | 0.14 | −0.24 | 1.12 | 0.834 | −0.02 |
| Insomnia | ||||||||
| Psychological | 0.01 | 0.07 | 0.886 | 0.02 | 0.11 | 0.07 | 0.088 | 0.20 |
| Physical | 0.57 | 1.56 | 0.716 | 0.04 | 0.85 | 1.37 | 0.537 | 0.07 |
| Well-Being | ||||||||
| Psychological | −0.03 | 0.06 | 0.609 | −0.06 | −0.09 | 0.07 | 0.201 | −0.13 |
| Physical | −0.19 | 1.56 | 0.904 | −0.02 | −0.91 | 1.46 | 0.535 | −0.06 |
| Ill Temper | ||||||||
| Psychological | 0.06 | 0.03 | 0.040 | 0.21 | 0.17 | 0.05 | 0.002 | 0.46 |
| Physical | 0.92 | 0.66 | 0.162 | 0.15 | −0.95 | 1.05 | 0.366 | −0.12 |
| Panic | ||||||||
| Psychological | −0.02 | 0.03 | 0.529 | −0.06 | 0.02 | 0.03 | 0.340 | 0.07 |
| Physical | 1.48 | 0.97 | 0.128 | 0.18 | 0.94 | 0.97 | 0.332 | 0.13 |
| Social Anxiety | ||||||||
| Psychological | 0.06 | 0.03 | 0.093 | 0.14 | 0.11 | 0.06 | 0.063 | 0.24 |
| Physical | −0.30 | 0.75 | 0.690 | −0.04 | −0.27 | 1.11 | 0.810 | −0.03 |
| Claustrophobia | ||||||||
| Psychological | 0.02 | 0.03 | 0.514 | 0.09 | 0.07 | 0.05 | 0.134 | 0.22 |
| Physical | 0.20 | 0.54 | 0.710 | 0.05 | −0.54 | 0.86 | 0.529 | −0.08 |
| Traumatic Intrusions | ||||||||
| Psychological | 0.05 | 0.03 | 0.031 | 0.20 | 0.04 | 0.02 | 0.125 | 0.15 |
| Physical | 0.03 | 0.51 | 0.949 | 0.01 | 0.36 | 0.58 | 0.535 | 0.07 |
| Traumatic Avoidance | ||||||||
| Psychological | 0.04 | 0.03 | 0.145 | 0.15 | 0.12 | 0.05 | 0.015 | 0.31 |
| Physical | 0.35 | 0.56 | 0.529 | 0.06 | −0.70 | 0.99 | 0.478 | −0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perez, G.R.; Stasik-O’Brien, S.M.; Laifer, L.M.; Brock, R.L. Psychological and Physical Intimate Partner Aggression Are Associated with Broad and Specific Internalizing Symptoms during Pregnancy. Int. J. Environ. Res. Public Health 2022, 19, 1662. https://doi.org/10.3390/ijerph19031662
Perez GR, Stasik-O’Brien SM, Laifer LM, Brock RL. Psychological and Physical Intimate Partner Aggression Are Associated with Broad and Specific Internalizing Symptoms during Pregnancy. International Journal of Environmental Research and Public Health. 2022; 19(3):1662. https://doi.org/10.3390/ijerph19031662
Chicago/Turabian StylePerez, Gabriela R., Sara M. Stasik-O’Brien, Lauren M. Laifer, and Rebecca L. Brock. 2022. "Psychological and Physical Intimate Partner Aggression Are Associated with Broad and Specific Internalizing Symptoms during Pregnancy" International Journal of Environmental Research and Public Health 19, no. 3: 1662. https://doi.org/10.3390/ijerph19031662
APA StylePerez, G. R., Stasik-O’Brien, S. M., Laifer, L. M., & Brock, R. L. (2022). Psychological and Physical Intimate Partner Aggression Are Associated with Broad and Specific Internalizing Symptoms during Pregnancy. International Journal of Environmental Research and Public Health, 19(3), 1662. https://doi.org/10.3390/ijerph19031662






