A Scoping Review of Moral Stressors, Moral Distress and Moral Injury in Healthcare Workers during COVID-19
Abstract
:1. Introduction
1.1. Moral Stressors
1.2. Moral Distress and Moral Injury
“(a) shame, (b) guilt, (c) a loss of trust in self, others, and/or transcendental/ultimate beings, and (d) spiritual/existential conflict including an ontological loss of meaning in life. These core symptomatic features, influence the development of secondary indicators such as (a) depression, (b) anxiety, (c) anger, (d) re-experiencing the moral conflict, (e) social problems (e.g., social alienation), and (f) relationship issues (e.g., collegian, spousal, family), and ultimately (g) self-harm (i.e., self-sabotage, substance abuse, suicidal ideation, and death)”.([56], p. 126)
1.3. Vulnerability Indicators for Moral Distress and Moral Injury in Healthcare Workers
1.4. Scope of This Paper
- i.
- The identification of moral stressors, PMIEs, MD, and MI in HCWs during COVID-19.
- ii.
- The identification of predictors of MD and MI in HCWs during COVID-19.
2. Materials and Methods
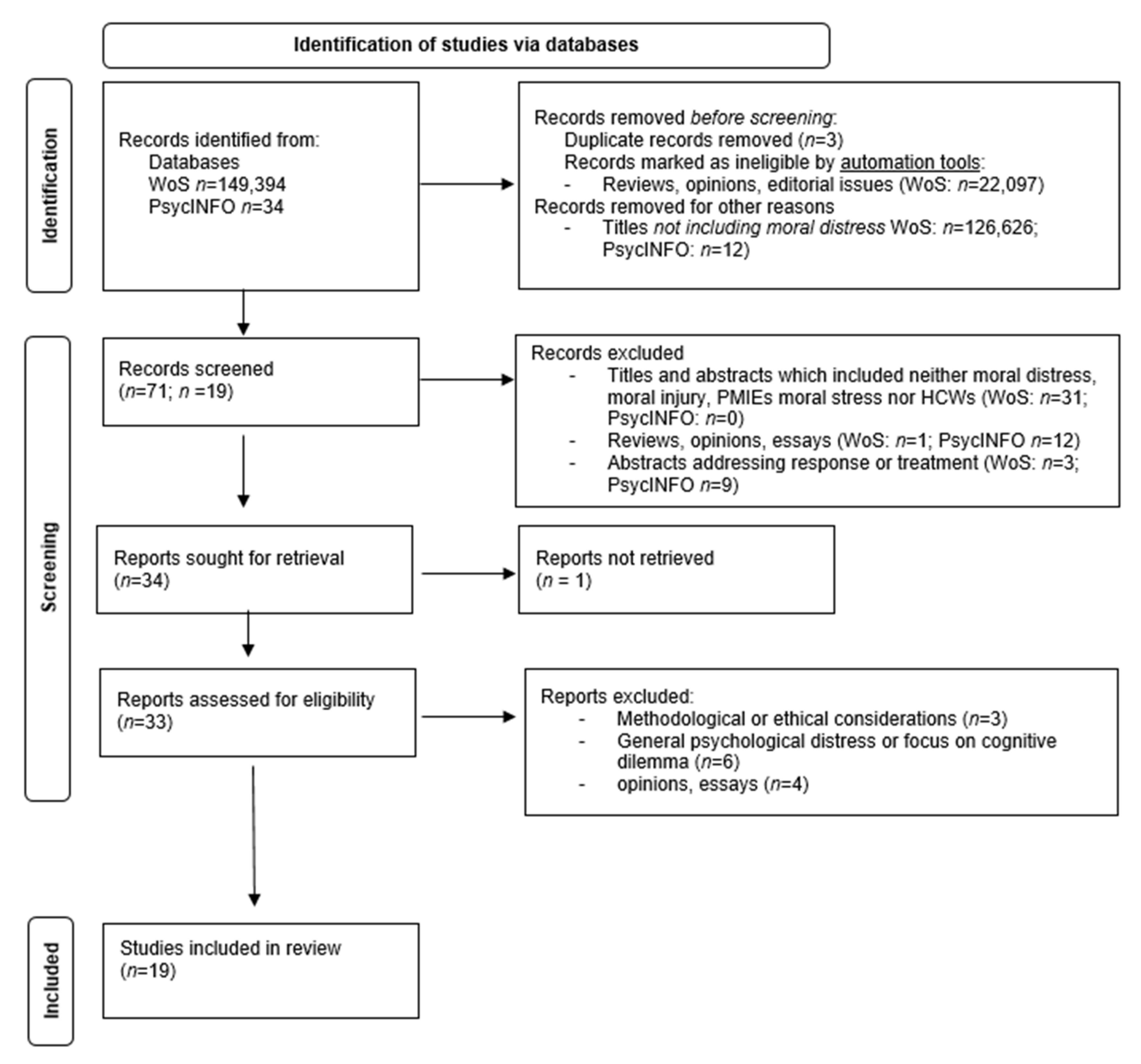
2.1. Literature Research
2.2. Identification
2.3. Screening and Selection
3. Results
3.1. Study Selection
3.2. General Characteristics of Studies
3.3. Synthesis of Results
3.3.1. Moral Stressors during COVID-19
3.3.2. Moral Distress and Moral Injury during COVID-19
3.3.3. Vulnerability Indicators for Moral Distress and Moral Injury in Healthcare Workers during COVID-19
4. Discussion
4.1. Moral Stressors during COVID-19
4.2. Moral Distress and Moral Injury during COVID-19
4.3. Consequences of Moral Distress and Moral Injury
4.4. Vulnerability Indicators for Moral Distress and Moral Injury in Healthcare Workers during COVID-19
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liberati, E.; Richards, N.; Willars, J.; Scott, D.; Boydell, N.; Parker, J.; Pinfold, V.; Martin, G.; Dixon-Woods, M.; Jones, P.B. A qualitative study of experiences of NHS mental healthcare workers during the COVID-19 pandemic. BMC Psychiatry 2021, 21, 250. [Google Scholar] [CrossRef]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H.; Wang, C.; Wang, Z.; You, Y.; et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control 2020, 48, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Williamson, V.; Murphy, D.; Greenberg, N. COVID-19 and Experiences of Moral Injury in Front-Line Key Workers; Oxford University Press: Oxford, UK, 2020. [Google Scholar]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Sadavoy, J.; Verhaeghe, L.M.; Steinberg, R.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003, 168, 1245–1251. [Google Scholar] [PubMed]
- Ramos, A.M.; Barlem, E.L.D.; Barlem, J.G.T.; Rocha, L.P.; Dalmolin, G.d.L.; Figueira, A.B. Cross-cultural adaptation and validation of the Moral Distress Scale-Revised for nurses. Rev. Bras. Enferm. 2017, 70, 1011–1017. [Google Scholar] [CrossRef] [Green Version]
- Sharif Nia, H.; Shafipour, V.; Allen, K.-A.; Heidari, M.R.; Yazdani-Charati, J.; Zareiyan, A. A Second-Order Confirmatory Factor Analysis of the Moral Distress Scale-Revised for Nurses. Nurs. Ethics 2019, 26, 1199–1210. [Google Scholar] [CrossRef] [PubMed]
- Silverman, H.J.; Kheirbek, R.E.; Moscou-Jackson, G.; Day, J. Moral distress in nurses caring for patients with COVID-19. Nurs. Ethics 2021, 9697330211003217. [Google Scholar] [CrossRef] [PubMed]
- Soleimani, M.A.; Sharif, S.P.; Yaghoobzadeh, A.; Panarello, B. Psychometric evaluation of the Moral Distress Scale-Revised among Iranian Nurses. Nurs. Ethics 2019, 26, 1226–1242. [Google Scholar] [CrossRef]
- Liu, X.; Xu, Y.; Chen, Y.; Chen, C.; Wu, Q.; Xu, H.; Zhu, P.; Waidley, E. Ethical dilemmas faced by frontline support nurses fighting COVID-19. Nurs. Ethics 2021, XX, 1–12. [Google Scholar] [CrossRef]
- Wang, Z.; Harold, K.G.; Tong, Y.; Wen, J.; Sui, M.; Liu, H.; Zaben, F.A.; Liu, G. Moral injury in Chinese health professionals during the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 2021, 14, 250–257. [Google Scholar] [CrossRef]
- Mantri, S.; Lawson, J.M.; Wang, Z.; Koenig, H.G. Identifying moral injury in healthcare professionals: The moral injury symptom scale-HP. J. Relig. Health 2020, 59, 2323–2340. [Google Scholar] [CrossRef]
- Kok, N.; van Gurp, J.; van der Hoeven, J.G.; Fuchs, M.; Hoedemaekers, C.; Zegers, M. Complex interplay between moral distress and other risk factors of burnout in ICU professionals: Findings from a cross-sectional survey study. BMJ Qual. Saf. 2021, 1–10. [Google Scholar] [CrossRef]
- Smallwood, N.; Pascoe, A.; Karimi, L.; Willis, K. Moral distress and perceived community views are associated with mental health symptoms in frontline health workers during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 8723. [Google Scholar] [CrossRef]
- Miljeteig, I.; Forthun, I.; Hufthammer, K.O.; Engelund, I.E.; Schanche, E.; Schaufel, M.; Onarheim, K.H. Priority-setting dilemmas, moral distress and support experienced by nurses and physicians in the early phase of the COVID-19 pandemic in Norway. Nurs. Ethics 2021, 28, 66–81. [Google Scholar] [CrossRef]
- Norman, S.B.; Feingold, J.H.; Kaye-Kauderer, H.; Kaplan, C.A.; Hurtado, A.; Kachadourian, L.; Feder, A.; Murrough, J.W.; Charney, D.; Southwick, S.M. Moral distress in frontline healthcare workers in the initial epicenter of the COVID-19 pandemic in the United States: Relationship to PTSD symptoms, burnout, and psychosocial functioning. Depress. Anxiety 2021, 38, 1007–1017. [Google Scholar] [CrossRef]
- Donkers, M.A.; Gilissen, V.J.H.S.; Candel, M.J.J.M.; van Dijk, N.M.; Kling, H.; Heijnen-Panis, R.; Pragt, E.; van der Horst, I.; Pronk, S.A.; van Mook, W.N.K.A. Moral distress and ethical climate in intensive care medicine during COVID-19: A nationwide study. BMC Med. Ethics 2021, 22, 73. [Google Scholar] [CrossRef]
- Patterson, J.E.; Edwards, T.M.; Griffith, J.L.; Wright, S. Moral distress of medical family therapists and their physician colleagues during the transition to COVID-19. J. Marital Fam. Ther. 2021, 47, 289–303. [Google Scholar] [CrossRef]
- Maftei, A.; Holman, A.-C. The prevalence of exposure to potentially morally injurious events among physicians during the COVID-19 pandemic. Eur. J. Psychotraumatol. 2021, 12, 1898791. [Google Scholar] [CrossRef]
- French, L.; Hanna, P.; Huckle, C. “If I die, they do not care”: UK National Health Service staff experiences of betrayal-based moral injury during COVID-19. Psychol. Trauma Theory Res. Pract. Policy 2021, 1–6. [Google Scholar] [CrossRef]
- Wilson, C.A.; Metwally, H.; Heavner, S.; Kennedy, A.B.; Britt, T.W. Chronicling moral distress among healthcare providers during the COVID-19 pandemic: A longitudinal analysis of mental health strain, burnout, and maladaptive coping behaviours. Int. J. Ment. Health Nurs. 2021. [Google Scholar] [CrossRef]
- Hines, S.E.; Chin, K.H.; Glick, D.R.; Wickwire, E.M. Trends in Moral Injury, Distress, and Resilience Factors among Healthcare Workers at the Beginning of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 488. [Google Scholar] [CrossRef]
- Kreh, A.; Brancaleoni, R.; Magalini, S.C.; Chieffo, D.P.R.; Flad, B.; Ellebrecht, N.; Juen, B. Ethical and psychosocial considerations for hospital personnel in the COVID-19 crisis: Moral injury and resilience. PLoS ONE 2021, 16, e0249609. [Google Scholar]
- Billings, J.; Biggs, C.; Ching, B.C.F.; Gkofa, V.; Singleton, D.; Bloomfield, M.; Greene, T. Experiences of mental health professionals supporting front-line health and social care workers during COVID-19: Qualitative study. BJPsych Open 2021, 7, 1–8. [Google Scholar] [CrossRef]
- World Health Organization. The World Health Report 2006: Working Together for Health; World Health Organization: Geneva, Switzerland, 2006; ISBN 9241563176. [Google Scholar]
- Lake, E.T.; Narva, A.M.; Holland, S.; Smith, J.G.; Cramer, E.; Rosenbaum, K.E.F.; French, R.; Clark, R.R.S.; Rogowski, J.A. Hospital nurses’ moral distress and mental health during COVID-19. J. Adv. Nurs. 2021, 1–11. [Google Scholar] [CrossRef]
- Walton, M.; Murray, E.; Christian, M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 241–247. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Litz, B.T.; Kerig, P.K. Introduction to the Special Issue on Moral Injury: Conceptual Challenges, Methodological Issues, and Clinical Applications. J. Trauma. Stress 2019, 32, 341–349. [Google Scholar] [CrossRef]
- Epstein, E.G.; Whitehead, P.B.; Prompahakul, C.; Thacker, L.R.; Hamric, A.B. Enhancing Understanding of Moral Distress: The Measure of Moral Distress for Health Care Professionals. AJOB Empir. Bioeth. 2019, 10, 113–124. [Google Scholar] [CrossRef]
- Jameton, A. Dilemmas of moral distress: Moral responsibility and nursing practice. AWHONNS Clin. Issues Perinat. Womens Health Nurs. 1993, 4, 542–551. [Google Scholar]
- Lamiani, G.; Dordoni, P.; Argentero, P. Value congruence and depressive symptoms among critical care clinicians: The mediating role of moral distress. Stress Health 2018, 34, 135–142. [Google Scholar] [CrossRef]
- Abdolmaleki, M.; Lakdizaji, S.; Ghahramanian, A.; Allahbakhshian, A.; Behshid, M. Relationship between autonomy and moral distress in emergency nurses. Indian J. Med. Ethics 2019, 4, 20–25. [Google Scholar] [CrossRef]
- Fruet, I.M.A.; Dalmolin, G.d.L.; Barlem, E.L.D.; Silva, R.M.d.; Andolhe, R. Aplicabilidade da Moral Distress Scale adaptada no cenário da enfermagem em hemato-oncologia. Rev. Gaucha Enferm. 2018, 38, e63060. [Google Scholar] [CrossRef] [PubMed]
- Hamaideh, S.H. Moral distress and its correlates among mental health nurses in Jordan. Int. J. Ment. Health Nurs. 2014, 23, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Bartholdson, C.; Molewijk, B.; Lützén, K.; Blomgren, K.; Pergert, P. Ethics case reflection sessions: Enablers and barriers. Nurs. Ethics 2018, 25, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Litz, B.T.; Stein, N.; Delaney, E.; Lebowitz, L.; Nash, W.P.; Silva, C.; Maguen, S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clin. Psychol. Rev. 2009, 29, 695–706. [Google Scholar] [CrossRef]
- Griffin, B.J.; Purcell, N.; Burkman, K.; Litz, B.T.; Bryan, C.J.; Schmitz, M.; Villierme, C.; Walsh, J.; Maguen, S. Moral Injury: An Integrative Review. J. Trauma. Stress 2019, 32, 350–362. [Google Scholar] [CrossRef]
- Frankfurt, S.B.; Frazier, P.; Engdahl, B. Indirect relations between transgressive acts and general combat exposure and moral injury. Mil. Med. 2017, 182, e1950–e1956. [Google Scholar] [CrossRef] [Green Version]
- Flipse Vargas, A.; Hanson, T.; Kraus, D.; Drescher, K.; Foy, D. Moral injury themes in combat veterans’ narrative responses from the National Vietnam Veterans’ Readjustment Study. Traumatology 2013, 19, 243–250. [Google Scholar] [CrossRef] [Green Version]
- Schorr, Y.; Stein, N.R.; Maguen, S.; Barnes, J.B.; Bosch, J.; Litz, B.T. Sources of moral injury among war veterans: A qualitative evaluation. J. Clin. Psychol. 2018, 74, 2203–2218. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013; ISBN 978-0-89042-557-2. [Google Scholar]
- Shay, J. Moral injury. Psychoanal. Psychol. 2014, 31, 182. [Google Scholar] [CrossRef]
- Corley, M.C. Nurse moral distress: A proposed theory and research agenda. Nurs. Ethics 2002, 9, 636–650. [Google Scholar] [CrossRef]
- Schwartz, M.S. Universal moral values for corporate codes of ethics. J. Bus. Ethics 2005, 59, 27–44. [Google Scholar] [CrossRef]
- Schwartz, S.H. Are there universal aspects in the structure and contents of human values? J. Soc. Issues 1994, 50, 19–45. [Google Scholar] [CrossRef]
- Epstein, E.G.; Delgado, S. Understanding and addressing moral distress. Online J. Issues Nurs. 2010, 15. Manuscript 1. [Google Scholar]
- Hamric, A.B.; Epstein, E.G. A health system-wide moral distress consultation service: Development and evaluation. In HEC Forum; Springer: Berlin/Heidelberg, Germany, 2017; pp. 127–143. ISBN 1572-8498. [Google Scholar]
- Rider, E.A.; Kurtz, S.; Slade, D.; Longmaid, H.E., III; Ho, M.-J.; Pun, J.K.-h.; Eggins, S.; Branch, W.T., Jr. The International Charter for Human Values in Healthcare: An interprofessional global collaboration to enhance values and communication in healthcare. Patient Educ. Couns. 2014, 96, 273–280. [Google Scholar] [CrossRef] [Green Version]
- Shahriari, M.; Mohammadi, E.; Abbaszadeh, A.; Bahrami, M. Nursing ethical values and definitions: A literature review. Iran J. Nurs. Midwifery Res. 2013, 18, 1–8. [Google Scholar]
- Epstein, E.G.; Hamric, A.B. Moral distress, moral residue, and the crescendo effect. J. Clin. Ethics 2009, 20, 330–342. [Google Scholar]
- Farnsworth, J.K.; Drescher, K.D.; Nieuwsma, J.A.; Walser, R.B.; Currier, J.M. The role of moral emotions in military trauma: Implications for the study and treatment of moral injury. Rev. Gen. Psychol. 2014, 18, 249–262. [Google Scholar] [CrossRef] [Green Version]
- Bryan, C.J.; Bryan, A.O.; Roberge, E.; Leifker, F.R.; Rozek, D.C. Moral injury, posttraumatic stress disorder, and suicidal behavior among National Guard personnel. Psychol. Trauma Theory Res. Pract. Policy 2018, 10, 36. [Google Scholar] [CrossRef]
- Currier, J.M.; Holland, J.M.; Malott, J. Moral injury, meaning making, and mental health in returning veterans. J. Clin. Psychol. 2015, 71, 229–240. [Google Scholar] [CrossRef]
- Evans, W.R.; Stanley, M.A.; Barrera, T.L.; Exline, J.J.; Pargament, K.I.; Teng, E.J. Morally injurious events and psychological distress among veterans: Examining the mediating role of religious and spiritual struggles. Psychol. Trauma Theory Res. Pract. Policy 2018, 10, 360. [Google Scholar] [CrossRef]
- Carey, L.B.; Hodgson, T.J. Chaplaincy, spiritual care and moral injury: Considerations regarding screening and treatment. Front. Psychiatry 2018, 9, 619. [Google Scholar] [CrossRef] [PubMed]
- Jinkerson, J.D. Defining and assessing moral injury: A syndrome perspective. Traumatology 2016, 22, 122. [Google Scholar] [CrossRef]
- Shoorideh, F.A.; Ashktorab, T.; Yaghmaei, F.; Alavi Majd, H. Relationship between ICU nurses’ moral distress with burnout and anticipated turnover. Nurs. Ethics 2015, 22, 64–76. [Google Scholar] [CrossRef] [PubMed]
- Lomis, K.D.; Carpenter, R.O.; Miller, B.M. Moral distress in the third year of medical school; a descriptive review of student case reflections. Am. J. Surg. 2009, 197, 107–112. [Google Scholar] [CrossRef]
- Oh, Y.; Gastmans, C. Moral distress experienced by nurses: A quantitative literature review. Nurs. Ethics 2015, 22, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Van der Colff, J.J.; Rothmann, S. Occupational stress, sense of coherence, coping, burnout and work engagement of registered nurses in South Africa. SA J. Ind. Psychol. 2009, 35, 1–10. [Google Scholar]
- Lamiani, G.; Ciconali, M.; Argentero, P.; Vegni, E. Clinicians’ moral distress and family satisfaction in the intensive care unit. J. Health Psychol. 2020, 25, 1894–1904. [Google Scholar] [CrossRef] [PubMed]
- De Veer, A.J.E.; Francke, A.L.; Struijs, A.; Willems, D.L. Determinants of moral distress in daily nursing practice: A cross sectional correlational questionnaire survey. Int. J. Nurs. Stud. 2013, 50, 100–108. [Google Scholar] [CrossRef] [Green Version]
- Ohnishi, K.; Ohgushi, Y.; Nakano, M.; Fujii, H.; Tanaka, H.; Kitaoka, K.; Nakahara, J.; Narita, Y. Moral distress experienced by psychiatric nurses in Japan. Nurs. Ethics 2010, 17, 726–740. [Google Scholar] [CrossRef]
- Bégat, I.; Ellefsen, B.; Severinsson, E. Nurses’ satisfaction with their work environment and the outcomes of clinical nursing supervision on nurses’ experiences of well-being -- a Norwegian study. J. Nurs. Manag. 2005, 13, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Pauly, B.; Varcoe, C.; Storch, J.; Newton, L. Registered nurses’ perceptions of moral distress and ethical climate. Nurs. Ethics 2009, 16, 561–573. [Google Scholar] [CrossRef]
- Lamiani, G.; Borghi, L.; Argentero, P. When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. J. Health Psychol. 2017, 22, 51–67. [Google Scholar]
- McAndrew, N.S.; Leske, J.S.; Garcia, A. Influence of moral distress on the professional practice environment during prognostic conflict in critical care. J. Trauma Nurs. 2011, 18, 221–230. [Google Scholar] [CrossRef]
- Karanikola, M.N.K.; Albarran, J.W.; Drigo, E.; Giannakopoulou, M.; Kalafati, M.; Mpouzika, M.; Tsiaousis, G.Z.; Papathanassoglou, E.D.E. Moral distress, autonomy and nurse–physician collaboration among intensive care unit nurses in Italy. J. Nurs. Manag. 2014, 22, 472–484. [Google Scholar] [CrossRef]
- Dean, W.; Simon Talbot, A.D. Reframing clinician distress: Moral injury not burnout. Fed. Pract. 2019, 36, 400. [Google Scholar]
- Williamson, V.; Stevelink, S.a.; Greenberg, N. Occupational moral injury and mental health: Systematic review and meta-analysis. Br. J. Psychiatry 2018, 212, 339–346. [Google Scholar] [CrossRef] [Green Version]
- Williams, R.D.; Brundage, J.A.; Williams, E.B. Moral injury in times of COVID-19. J. health Serv. Psychol. 2020, 46, 65–69. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Hawkins, D.T.; Wagers, R. Online Bibliographic Search Strategy Development. Online 1982, 6, 12–19. [Google Scholar]
- Hamric, A.B.; Borchers, C.T.; Epstein, E.G. Development and Testing of an Instrument to Measure Moral Distress in Healthcare Professionals. AJOB Prim. Res. 2012, 3, 1–9. [Google Scholar] [CrossRef]
- Wocial, L.D.; Weaver, M.T. Development and psychometric testing of a new tool for detecting moral distress: The Moral Distress Thermometer. J. Adv. Nurs. 2013, 69, 167–174. [Google Scholar] [PubMed]
- Nash, W.P.; Marino Carper, T.L.; Mills, M.A.; Au, T.; Goldsmith, A.; Litz, B.T. Psychometric evaluation of the Moral Injury Events Scale. Mil. Med. 2013, 178, 646–652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rathert, C.; May, D.R.; Chung, H.S. Nurse moral distress: A survey identifying predictors and potential interventions. Int. J. Nurs. Stud. 2016, 53, 39–49. [Google Scholar] [CrossRef]
- Zerach, G.; Levi-Belz, Y. Moral injury and mental health outcomes among Israeli health and social care workers during the COVID-19 pandemic: A latent class analysis approach. Eur. J. Psychotraumatol. 2021, 12, 1945749. [Google Scholar] [CrossRef]
- Dean, W.; Talbot, S.G.; Caplan, A. Clarifying the language of clinician distress. JAMA 2020, 323, 923–924. [Google Scholar] [CrossRef]
- Carey, L.B.; Hodgson, T.J.; Krikheli, L.; Soh, R.Y.; Armour, A.-R.; Singh, T.K.; Impiombato, C.G. Moral injury, spiritual care and the role of chaplains: An exploratory scoping review of literature and resources. J. Relig. health 2016, 55, 1218–1245. [Google Scholar] [CrossRef]
| Authors (Year) | Country | Time of Measurement | Study Design | Sample | Measures | Main Results |
| Wang et al., (2021) | China | March to April 2020 | Validation study | 3006 doctors and nurses | Moral Injury Symptoms Scale-Health Professional (MISS-HP; [11]) | Scores of MISS-HP were positively correlated with depression (r = 0.44), anxiety (r = 0.41), low well-being(r = −0.50), and emotional exhaustion (r = 0.41); 41% of HCWs experience MI. |
| Mantri et al., (2020) | USA | November 2019 and March 2020 | Validation study | 181 HCWs (doctors, nurses and “other”) | MISS-HP [11] | Validation of dimensions betrayal, guilt, shame, moral concerns, religious struggle, loss of religious/spiritual faith, loss of meaning/purpose, difficulty forgiving, loss of trust, and self-condemnation as components of MI in HCWs; internal reliability was at 0.75. Discriminant validity was shown by moderate positive correlation of scores with low religiosity, depression, and anxiety symptoms (r’s = 0.25–0.37). Convergent validity was indicated by strong correlations with burnout (r = 0.57). |
| Kok et al., (2021) | Netherlands | October to December 2019 and May to June 2020 | Quantitative longitudinal study | 233 physicians and nurses in intensive care units of two different hospitals | Moral distress scale-revised (MDS-R; [75]) | Differences in the presence of moral stressors before and during COVID-19 prevalent in the context of COVID-19 were hindered care due to a lack of financial support, resources of time or staff; working with colleagues not following safety guidelines or acting unsafely; and working with doctors or nurses who lacked professional competence. |
| Smallwood et al., (2021) | Australia | August to October 2020 | Quantitative study | 7846 HCWs, nurses, doctors, and allied health workers | Four self-developed items | Moral distress due to family exclusion; resource constraints; fear of abandoning colleagues in the wake of their own infection; and wearing personal protective equipment (PPE). |
| Miljeteig et al., (2021) | Norway | April to May 2020 | Quantitative study | 1606 nurses, managers, and doctors | Moral distress thermometer (MDT; [76] ) | Moral distress due to priority setting dilemmas and resource shortages. |
| Norman et al., (2021) | USA | Spring 2020 | Quantitative study | 2579 frontline HCWs (physicians, nurse social workers, physician assistants, pastors, and dietitians) | Self-developed 11 Item scale | Moral stressors were present in fears of infecting one’s family; dilemmas between the desire to help one’s family and the duty to help patients; and the effect of COVID-19 on personal relationships and work-related concerns. |
| Donkers et al., (2021) | Netherlands | April and June 2020 | Quantitative study | 84 intensive care units in the Netherlands including 355 nurses, 40 intensivists, and 103 supporting staff | Measure of Moral Distress for Healthcare Professionals (MMD-HP; [29]) | Experiences of stress for all groups of HCWs included the inability to provide emotional support to patients when they or their relatives were anxious and stressed as well as the inability to provide a dignified death for patients’ relatives. MD scores during COVID-19 were lower for ICU nurses and intensivists compared to one year before COVID-19. |
| Lake et al., (2021) | USA | September 2020 | Quantitative study | 307 caregivers | COVID-19 Moral Distress Scale [25] | A lack of protective equipment and the anticipated risk of infecting family members were identified as moral stressors. MD in nurses was negatively associated with effective communication and availability of protective materials and positively associated with number of COVID-19 patients. |
| Lui et al., (2021) | China | Post deployment to working in Wuhan with COVID-19 patients | Qualitative study | 10 nurses working with COVID 19- patients | Semi-structured interviews | Ethical dilemmas were revealed at the level of clinical care, interpersonal relationships, and care management. |
| Silverman et al., (2021) | USA | April to May 2020 | Qualitative study | 31 critical care nurses caring for COVID-19 patients | Focus groups and in-depth interviews | Moral stressors were mentioned in terms of lack of knowledge and uncertainty regarding the novel virus; being overwhelmed by COVID disease; and a fear of the virus leading to suboptimal care. |
| Patterson et al., (2021) | USA | May and July 2020 | Qualitative study | 34 primary care clinicians | Informal questionnaire | Problems balancing personal needs with the demands of the workplace to meet the needs of patients. Feelings of helplessness, cynicism, disengagement from work, and a desire to change career direction were stated as PMIEs. |
| Liberati et al., (2021) | England | June and August 2020 | Qualitative study | 35 mental health care workers (psychiatrists, nurses, caregivers, psychotherapists, and clinical psychologists) | Semi-structured interviews | Dilemmas existed in clinical decision-making, priority setting, care decisions, trade-offs in therapy delivery and role performance, balancing human contact needs, and infection control as well as low organizational support. Psychosocial consequences included sadness, helplessness, isolation, distress, and burnout. |
| Maftei & Holman, (2021) | Romania | April 2020 | Quantitative study | 114 doctors | Adopted version of the Moral Injury Events Scale (MIES; [77]) | 47% of respondents reported high exposure to PMIEs. No associations between PMIE exposure, demographic characteristics or workplace environment (COVID-19 or non-COVID-19) were found. Exposure to PMIEs was associated with physical and emotional impacts. |
| Zerach & Levi-Belz, (2021) | Israel | February to March 2021 | Quantitative study | 296 Israeli social workers and hospital staff | MIES; [77] and MISS-HP; [11] | 55% reported being betrayed by their leadership, 46% felt they witnessed things that were morally wrong, 32% felt betrayed by people outside the hospital, 32% reported their own moral transgressions, 49% reported having experienced at least one transgression by others, and 62% had experienced betrayal by others. “High Exposure” and “betrayal-only” classes show higher levels of depressive, anxiety, posttraumatic, and more moral injury symptoms compared to the “minimal exposure” class. “High exposure” and “betrayal-only” classes state lower levels of self-compassion and higher levels of self-criticism, relative to participants in the “minimal exposure” class. |
| French, Hanna, & Huckle, (2021) | England | No date | Qualitative study | 16 HCWs (nurses, doctors, therapists, paramedics, head of nursing) | Interviews | Respondents reported experiences of betrayal by management during COVID-19. Staff lacked management support, perceived treatment during the pandemic as dehumanizing, and reported being treated as a replaceable resource. Employees reported a lack of empathy, appreciation, and respect from supervisors; and emotions of frustration, anger, and loss of trust. |
| Kreh et al., (2021) | Italy and Austria | March to May 2020 | Qualitative study | 13 key informants (doctors, nurses, psychologists in leading positions) | Interviews | Moral Injury (MI) was represented by feelings of anxiety, blame, frustration, loss of confidence, and exhaustion. |
| Billings et al., (2021) | England | July 2020 | Qualitative study | 28 mental health workers from different settings | Interviews | Identification of PMIEs in additional responsibility and increased workload; confidence building with limited visibility of facial expressions due to PPE; isolation, insecurities, and fears due to lack of knowledge; inconsistency in delivery of own services; and blurred roles occurring when colleagues became clients as PMIEs. Identification of MI in feelings of guilt towards patients. |
| Wilson et al., (2021) | 6 countries (not specified) | April and December 2020 | Quantitative longitudinal study | 378 HCWs (massage therapists, nurses, physicians, and other healthcare personnel) | Single-item Moral Distress Questionnaire [78] | Negative association of MD with mental health and MD was found as a predictor of burnout. |
| Hines et al., (2021) | USA | March to July 2020 | Quantitative longitudinal study | 77 critical care staff (90% physicians) | MIES [77]) | A supportive workplace environment was associated with low MI; and stressful and less supportive working conditions were associated higher MI. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riedel, P.-L.; Kreh, A.; Kulcar, V.; Lieber, A.; Juen, B. A Scoping Review of Moral Stressors, Moral Distress and Moral Injury in Healthcare Workers during COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 1666. https://doi.org/10.3390/ijerph19031666
Riedel P-L, Kreh A, Kulcar V, Lieber A, Juen B. A Scoping Review of Moral Stressors, Moral Distress and Moral Injury in Healthcare Workers during COVID-19. International Journal of Environmental Research and Public Health. 2022; 19(3):1666. https://doi.org/10.3390/ijerph19031666
Chicago/Turabian StyleRiedel, Priya-Lena, Alexander Kreh, Vanessa Kulcar, Angela Lieber, and Barbara Juen. 2022. "A Scoping Review of Moral Stressors, Moral Distress and Moral Injury in Healthcare Workers during COVID-19" International Journal of Environmental Research and Public Health 19, no. 3: 1666. https://doi.org/10.3390/ijerph19031666
APA StyleRiedel, P.-L., Kreh, A., Kulcar, V., Lieber, A., & Juen, B. (2022). A Scoping Review of Moral Stressors, Moral Distress and Moral Injury in Healthcare Workers during COVID-19. International Journal of Environmental Research and Public Health, 19(3), 1666. https://doi.org/10.3390/ijerph19031666






