Oncological Outcomes of Primary vs. Salvage OPHL Type II: A Systematic Review
Abstract
:1. Introduction
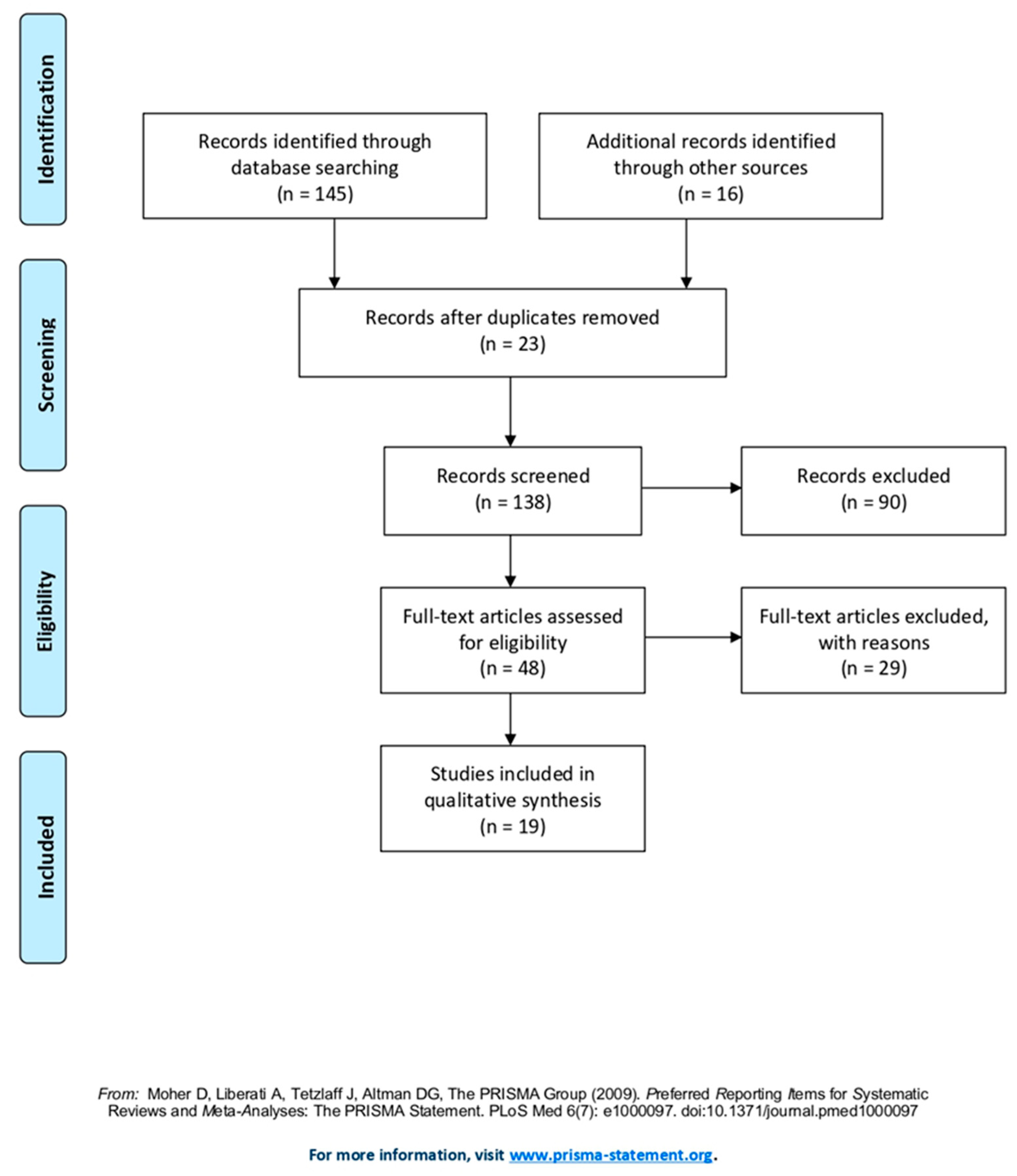
2. Materials and Methods
2.1. Search Methodology
2.2. Eligibility Criteria
2.3. Data Analysis
3. Results
3.1. Selection and Classification of Studies
3.2. Primary OPHL Type II
3.3. Salvage OPHL Type II
3.4. Adjuvant Radiotherapy after Primary OPHL Type II
4. Discussion
4.1. Primary OPHL Type II
4.2. Salvage OPHL Type II
4.3. Adjuvant Radiotherapy after Primary OPHL Type II
4.4. The Old Discussion: Laryngeal Preservation vs. Functional Preservation
4.5. Study Limitation
5. Conclusions
6. Highlights
- OPHL type II has two aims: oncological radicality and organ preservation
- OPHL type II ensures good oncological outcome both in primary and salvage surgery
- OPHL type II performs better results in primary surgery than in salvage surgery
- The main criterion for positive outcomes is the strict selection of patient and tumor stage
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Majer, E.H.; Rieder, W. Technic of laryngectomy permitting the conservation of respiratory permeability (cricohyoidopexy). Les Ann. D’oto-Laryngol. 1959, 76, 677–681. [Google Scholar]
- Piquet, J.J.; Desaulty, A.; Decroix, G. La crico-hyoïdo-épiglotto-pexie. Technique opératoire et résultats fonctionnels. Ann. Otolaryngol. Chir. Cervicofac. 1974, 91, 681–686. [Google Scholar] [PubMed]
- Karasalihoglu, A.R.; Yagiz, R.; Tas, A.; Uzun, C.; Adali, M.K.; Koten, M. Supracricoid partial laryngectomy with cricohyoidopexy and cricohyoidoepiglottopexy: Functional and oncological results. J. Laryngol. Otol. 2004, 118, 671–675. [Google Scholar] [CrossRef] [PubMed]
- Forastiere, A.A.; Ismaila, N.; Lewin, J.; Nathan, C.A.; Adelstein, D.J.; Eisbruch, A.; Fass, G.; Fisher, S.G.; Laurie, S.A.; Le, Q.-T.; et al. Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2018, 36, 1143–1169. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, K.; Akyildiz, S.; Gode, S.; Turhal, G.; Kirazli, T.; Aysel, A.; Uluoz, U. Post-Surgical and Oncologic Outcomes of Supracricoid Partial Laryngectomy: A Single-Institution Report of Ninety Cases. ORL J. Otorhinolaryngol. Relat. Spec. 2016, 78, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Cuadrado, I.; Castro, A.; Bernáldez, R.; Del Palacio, A.; Gavilán, J. Oncologic Outcomes after Supracricoid Partial Laryngectomy. Otolaryngol. Head Neck Surg. 2011, 144, 910–914. [Google Scholar] [CrossRef] [PubMed]
- Succo, G.; Peretti, G.; Piazza, C.; Remacle, M.; Eckel, H.E.; Chevalier, D.; Simo, R.; Hantzakos, A.G.; Rizzotto, G.; Lucioni, M.; et al. Open partial horizontal laryngectomies: A proposal for classification by the working committee on nomenclature of the European Laryngological Society. Eur. Arch. Oto-Rhino-Laryngol. 2014, 271, 2489–2496. [Google Scholar] [CrossRef]
- Pinar, E.; Imre, A.; Calli, C.; Oncel, S.; Katilmis, H. Supracricoid Partial Laryngectomy: Analyses of oncologic and functional outcomes. Otolaryngol. Head Neck Surg. 2012, 147, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Calearo, C.; Bignardi, L. A personal experience with subtotal and conservation surgery as treatment for laryngeal cancer. Eur. Arch. Oto-Rhino-Laryngol. 1986, 243, 174–179. [Google Scholar] [CrossRef]
- Sperry, S.M.; Rassekh, C.H.; Laccourreye, O.; Weinstein, G.S. Supracricoid Partial Laryngectomy for Primary and Recurrent Laryngeal Cancer. JAMA Otolaryngol. Head Neck Surg. 2013, 139, 1226–1235. [Google Scholar] [CrossRef] [Green Version]
- Nakayama, M.; Okamoto, M.; Hayakawa, K.; Ishiyama, H.; Kotani, S.; Miyamoto, S.; Seino, Y.; Okamoto, T.; Soda, I.; Sekiguchi, A. Clinical outcome of supracricoid laryngectomy with cricohyoidoepiglottopexy: Radiation failure versus previously untreated patients. Auris Nasus Larynx 2013, 40, 207–210. [Google Scholar] [CrossRef]
- Cho, K.J.; Joo, Y.H.; Sun, D.I.; Kim, M.S. Supracricoid laryngectomy: Oncologic validity and functional safety. Eur. Arch. Oto-Rhino-Laryngol. 2010, 267, 1919–1925. [Google Scholar] [CrossRef]
- Basaran, B.; Ünsaler, S.; Ulusan, M.; Aslan, I. The Effect of Arytenoidectomy on Functional and Oncologic Results of Supracricoid Partial Laryngectomy. Ann. Otol. Rhinol. Laryngol. 2015, 124, 788–796. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, F.; Fermi, M.; Molinari, G.; Capriotti, V.; Melegari, G.; Bertolini, F.; D’Angelo, E.; Tirelli, G.; Presutti, L. pT3 N0 Laryngeal Squamous Cell Carcinoma: Oncologic Outcomes and Prognostic Factors of Surgically Treated Patients. Laryngoscope 2021, 131, 2262–2268. [Google Scholar] [CrossRef] [PubMed]
- Crosetti, E.; Bertolin, A.; Molteni, G.; Bertotto, I.; Balmativola, D.; Carraro, M.; Sprio, A.E.; Berta, G.N.; Presutti, L.; Rizzotto, G.; et al. Patterns of recurrence after open partial horizontal laryngectomy types II and III: Univariate and logistic regression analysis of risk factors. Acta Otorhinolaryngol. Ital. 2019, 39, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Page, C.; Mortuaire, G.; Mouawad, F.; Ganry, O.; Darras, J.; Pasquesoone, X.; Chevalier, D. Supracricoid laryngectomy with cricohyoidoepiglottopexy (CHEP) in the management of laryngeal carcinoma: Oncologic results. A 35-year experience. Eur. Arch. Oto-Rhino-Laryngol. 2013, 270, 1927–1932. [Google Scholar] [CrossRef]
- Gong, H.; Zhou, L.; Wu, H.; Tao, L.; Chen, X.; Li, X.; Li, C.; Zhou, J. Long-term clinical outcomes of supracricoid partial laryngectomy with cricohyoidoepiglottopexy for glottic carcinoma. Acta Oto-Laryngol. 2019, 139, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Deganello, A.; Gallo, O.; De Cesare, J.M.; Ninu, M.B.; Gitti, G.; Campora, L.D.; Radici, M.; Campora, E.D. Supracricoid partial laryngectomy as salvage surgery for radiation therapy failure. Head Neck 2008, 30, 1064–1071. [Google Scholar] [CrossRef] [Green Version]
- Pellini, R.; Pichi, B.; Ruscito, P.; Ceroni, A.R.; Caliceti, U.; Rizzotto, G.; Pazzaia, A.; Laudadio, P.; Piazza, C.; Peretti, G.; et al. Supracricoid partial laryngectomies after radiation failure: A multi-institutional series. Head Neck 2008, 30, 372–379. [Google Scholar] [CrossRef]
- Bertolin, A.; Lionello, M.; Ghizzo, M.; Cena, I.; Leone, F.; Valerini, S.; Mattioli, F.; Crosetti, E.; Presutti, L.; Succo, G.; et al. Salvage open partial horizontal laryngectomy after failed radiotherapy: A multicentric study. Laryngoscope 2020, 130, 431–436. [Google Scholar] [CrossRef]
- Gallo, A.; Manciocco, V.; Simonelli, M.; Pagliuca, G.; D’Arcangelo, E.; de Vincentiis, M. Supracricoid Partial Laryngectomy in the Treatment of Laryngeal Cancer: UnIn Proceedings of theivariate and multivariate analysis of prognostic factors. Arch. Otolaryngol.—Head Neck Surg. 2005, 131, 620–625. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Topaloğlu, I.; Bal, M.; Saltürk, Z. Supracricoid laryngectomy with cricohyoidopexy: Oncological results. Eur. Arch. Oto-Rhino-Laryngol. 2011, 269, 1959–1965. [Google Scholar] [CrossRef]
- Rizzotto, G.; Crosetti, E.; Lucioni, M.; Succo, G. Subtotal laryngectomy: Outcomes of 469 patients and proposal of a comprehensive and simplified classification of surgical procedures. Eur. Arch. Oto-Rhino-Laryngol. 2012, 269, 1635–1646. [Google Scholar] [CrossRef]
- Mercante, G.; Grammatica, A.; Battaglia, P.; Cristalli, G.; Pellini, R.; Spriano, G. Supracricoid Partial Laryngectomy in the Management of T3 Laryngeal Cancer. Otolaryngol. Head Neck Surg. 2013, 149, 714–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atallah, I.; Berta, E.; Coffre, A.; Villa, J.; Reyt, E.; Righini, C. Supracricoid partial laryngectomy with crico-hyoido-epiglottopexy for glottic carcinoma with anterior commissure involvement. La laringectomia parziale sopracricoidea con crico-ioido-pessia per il carcinoma della glottide coinvolgente la commissura anteriore. Acta Otorhinolaryngol. Ital. 2017, 37, 188–194. [Google Scholar] [CrossRef]
- Pescetto, B.; Gal, J.; Chamorey, E.; Dassonville, O.; Poissonnet, G.; Bozec, A. Role of supracricoid partial laryngectomy with cricohyoidoepiglottopexy in glottic carcinoma with anterior commissure involvement. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2018, 135, 249–253. [Google Scholar] [CrossRef]
- Pfister, D.G.; Spencer, S.; Adelstein, D.; Adkins, D.; Anzai, Y.; Brizel, D.M.; Bruce, J.Y.; Busse, P.M.; Caudell, J.J.; Cmelak, A.J.; et al. Head and Neck Cancers, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2020, 18, 873–898. [Google Scholar] [CrossRef] [PubMed]
- Succo, G.; Crosetti, E.; Bertolin, A.; Lucioni, M.; Caracciolo, A.; Panetta, V.; Sprio, A.E.; Berta, G.N.; Rizzotto, G. Benefits and drawbacks of open partial horizontal laryngectomies, Part A: Early- to intermediate-stage glottic carcinoma. Head Neck 2016, 38 (Suppl. S1), E333–E340. [Google Scholar] [CrossRef] [Green Version]
- Vella, O.; Blanchard, D.; de Raucourt, D.; Rame, J.E.; Babin, E. Function evaluation of laryngeal reconstruction using infrahyoid muscle after partial laryngectomy in 37 patients. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2020, 137, 7–11. [Google Scholar] [CrossRef]
- Succo, G.; Crosetti, E. Limitations and Opportunities in Open Laryngeal Organ Preservation Surgery: Current Role of OPHLs. Front. Oncol. 2019, 9, 408. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, N.P.; Chi, A.; Betz, M.; Almeida, F.; Vos, P.; Davis, R.; Slane, B.; Ceizyk, M.; Abraham, D.; Smith-Raymond, L.; et al. Feasibility of Intensity-Modulated and Image-Guided Radiotherapy for Functional Organ Preservation in Locally Advanced Laryngeal Cancer. PLoS ONE 2012, 7, e42729. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.N.; Dyer, M.A.; Qureshi, M.M.; Shah, N.K.; Grillone, G.A.; Faden, D.L.; Jalisi, S.M.; Truong, M.T. Hypofractionated radiotherapy and surgery compared to standard radiotherapy in early glottic cancer. Am. J. Otolaryngol. 2020, 41, 102544. [Google Scholar] [CrossRef]
- Luna-Ortiz, K.; Reynoso-Noveron, N.; Zacarias-Ramon, L.C.; Alvarez-Avitia, M.; Luna-Peteuil, Z.; Garcia-Ortega, D.Y. Supracricoid Partial Laryngectomy With and Without Neoadjuvant Chemotherapy in Glottic Cancer. Laryngoscope 2021, 132, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Massaro, N.; Verro, B.; Greco, G.; Chianetta, E.; D’Ecclesia, A.; Saraniti, C. Quality of Life with Voice Prosthesis after Total Laryngectomy. Iran J. Otorhinolaryngol. 2021, 33, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, G.S.; El-Sawy, M.M.; Ruiz, C.; Dooley, P.; Chalian, A.; El-Sayed, M.M.; Goldberg, A. Laryngeal Preservation With Supracricoid Partial Laryngectomy Results in Improved Quality of Life When Compared With Total Laryngectomy. Laryngoscope 2001, 111, 191–199. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. SF-36 Physical and Mental Health Summary Scale: A User Manual; The Health Institute, New England Medical Center: Boston, UK, 1994. [Google Scholar]
- Hogikyan, N.D.; Sethuraman, G. Validation of an instrument to measure voice-related quality of life (V-RQOL). J. Voice 1999, 13, 557–569. [Google Scholar] [CrossRef]
- Fantini, M.; Crosetti, E.; Affaniti, R.; Sprio, A.E.; Bertotto, I.; Succo, G. Preoperative prognostic factors for functional and clinical outcomes after open partial horizontal laryngectomies. Head Neck 2021, 43, 3459–3467. [Google Scholar] [CrossRef]
- Lucioni, M.; Bertolin, A.; Lionello, M.; Giacomelli, L.; Rizzotto, G.; Marioni, G. Salvage transoral laser microsurgery for recurrent glottic carcinoma after primary laser-assisted treatment: Analysis of prognostic factors. Head Neck 2016, 38, 1043–1049. [Google Scholar] [CrossRef]
- Crosetti, E.; Caracciolo, A.; Molteni, G.; Sprio, A.E.; Berta, G.; Presutti, L. Unravelling the risk factors that underlie laryngeal surgery in elderly, Svelare i fattori di rischio che sottendono la chirurgia laringea negli anziani. Acta Otorhinolaryngol. Ital. 2016, 36, 185–193. [Google Scholar] [CrossRef]
- American Society of Clinical Oncology; Pfister, D.G.; Laurie, S.A.; Weinstein, G.S.; Mendenhall, W.M.; Adelstein, D.J.; Ang, K.K.; Clayman, G.L.; Fisher, S.G.; Forastiere, A.A.; et al. American Society of Clinical Oncology Clinical Practice Guideline for the Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer. J. Clin. Oncol. 2006, 24, 3693–3704. [Google Scholar] [CrossRef]
- Saraniti, C.; Montana, F.; Chianetta, E.; Greco, G.; Verro, B. Impact of resection margin status and revision transoral laser microsurgery in early glottic cancer: Analysis of organ preservation and disease local control on a cohort of 153 patients. Braz. J. Otorhinolaryngol. 2020, 1808. [Google Scholar] [CrossRef] [PubMed]
- Makeieff, M.; Venegoni, D.; Mercante, G.; Crampette, L.; Guerrier, B. Supracricoid Partial Laryngectomies after Failure of Radiation Therapy. Laryngoscope 2005, 115, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Schindler, A.; Pizzorni, N.; Mozzanica, F.; Fantini, M.; Ginocchio, D.; Bertolin, A.; Crosetti, E.; Succo, G. Functional outcomes after supracricoid laryngectomy: What do we not know and what do we need to know? Eur. Arch. Oto-Rhino-Laryngol. 2015, 273, 3459–3475. [Google Scholar] [CrossRef]
- Schindler, A.; Mozzanica, F.; Ginocchio, D.; Invernizzi, A.; Peri, A.; Ottaviani, F. Voice-related quality of life in patients after total and partial laryngectomy. Auris Nasus Larynx 2012, 39, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, A.; Bertelli, A.; Malavasi, T.; Kikuchi, W.; Rodrigues, A.; Menezes, M. Results after supracricoid horizontal partial laryngectomy. Auris Nasus Larynx 2010, 37, 84–88. [Google Scholar] [CrossRef]
- Saraniti, C.; Speciale, R.; Santangelo, M.; Massaro, N.; Maniaci, A.; Gallina, S. Functional outcomes after supracricoid modified partial laryngectomy. J. Biol. Regul. Homeost. Agents 2019, 33, 1903–1907. [Google Scholar]
- Thomas, L.; Drinnan, M.; Natesh, B.; Mehanna, H.; Jones, T.; Paleri, V. Open conservation partial laryngectomy for laryngeal cancer: A systematic review of English language literature. Cancer Treat. Rev. 2012, 38, 203–211. [Google Scholar] [CrossRef]
| Authors (Year of Publication) | N° Patients | pT Treated | Follow-Up | OS | DSS | DFS | LP | LC |
|---|---|---|---|---|---|---|---|---|
| Karasalihoglu AR et al. (2004) [3] | 68 | T1-T4 | 62 months (median) | 78.6% (5 years) | 93.9% (5 years) | / | 89.7% (5 years) | 95.6% (5 years) |
| Sánchez-Cuadrado I et al. (2011) [6] | 41 | T1-T3 | 43 months (median) | 69% (5 years) | 81% (5 years) | / | 85% (5 years) | 80% (5 years) |
| Nakayama M et al. (2013) [11] | 43 | T1-T4 | 38 months (median) | 81% (5 years) [salvage]—87% (5 years) [virgin] | / | / | 94% (5 years) [salvage]—91% (5 years) [virgin] | / |
| Page C et al. (2013) [15] | 291 | T1-T3 | 56 months (mean) | 80% (5 years) | / | / | / | 93.94% (5 years) |
| Ozturk K et al. (2016) [5] | 90 | T1b—T2—selected T3 | 55 months (median) | 80.4% (5 years) | / | 76.7% (5 years) | / | / |
| Gong H et al. (2019) [16] | 164 | T1b—T2—selected T3 | 85 months (median) | 86.9% (5 years) | 87.6% (5 years) | 82.4% (5 years) | / | / |
| Number of treated patients, stage of tumor (pT), period of follow up, overall survival (OS), disease-specific survival (DSS), disease-free survival (DFS), laryngeal preservation (LP), and local control (LC). | ||||||||
| Authors (Year of Publication) | N° Patients | pT Treated | Follow-Up | OS | DSS | DFS | LP | LC |
|---|---|---|---|---|---|---|---|---|
| Deganello A et al. (2008) [19] | 31 | T1-T4 | 45 months (mean) | 60% (5 years) | / | / | 90% (5 years) | 75% (5 years) |
| Pellini R et al. (2008) [20] | 78 | T1-T4 | 70 months (median) | 81.8% (5 years) | / | 95.5% (5 years) | / | / |
| Nakayama M et al. (2013) [11] | 30 | T1-T4 | 38 months (median) | 81% (5 years) [salvage]—87% (5 years) [primary] | / | / | 94% (5 years) [salvage]—91% (5 years) [primary] | / |
| Sperry SM et al. (2013) [10] | 42 | T1-T3 | 61 months (mean) | 75% (5 years) | 85% (5 years) | / | 95% (5 years) | 98% (5 years) |
| Bertolin A et al. (2020) [21] | 50 | T1-T4 | 50.1 months (mean) | 82% (5 years) | 88% (5 years) | 86% (5 years) | / | / |
| Number of treated patients, stage of tumor (pT), period of follow up, overall survival (OS), disease-specific survival (DSS), disease-free survival (DFS), laryngeal preservation (LP), and local control (LC). | ||||||||
| Authors (Year of Publication) | N° Patients | pT Treated | Follow-Up | OS | DSS | DFS | LP | LC | LR | Criteria for Adjuvant RT |
|---|---|---|---|---|---|---|---|---|---|---|
| Gallo A et al. (2005) [20] | 253 | T1-T4 | 51.6 months (mean) | 79.1% (5 years) | / | / | / | / | 8.7% (5 years) | Positive resection margin, >N1, extracapsular spread |
| Pinar et al. (2012) [8] | 56 | T1-T4 | 58 months (median) | 82.1% (5 years) | 86.5% (5 years) | / | / | 92.5% (5 years) | / | Positive resection margin, >N1, extracapsular spread, thyroid cartilage invasion |
| Topaloglu I et al. (2012) [23] | 44 | T2-T3 | 53.2 months (mean) | 84.1% (5 years) | 92.5% (5 years) | / | / | / | / | Positive resection margin, >N1, extracapsular spread, thyroid cartilage invasion |
| Rizzotto G et al. (2012) [24] | 399 | T1-T4 | 97 months (mean) | 95.6% (5 years) | / | 90.9% (5 years) | / | / | 3.2% (5 years) | Positive resection margin, >N1, extracapsular spread |
| Mercante G et al. (2013) [25] | 32 | T3 | 47.3 months (median) | 87.3% (5 years) | / | 78.2% (5 years) | / | 96.2% (5 years) | / | >N1, extracapsular spread, T4a |
| Basaran B et al. (2015) [13] | 68 | T2-T3 | 52.4 months (mean) | 81.2% (5 years) [BASCL]—85% (5 years [OASCL] p-value 0.66 | 93% (5 years) [BASCL]—89.5% (5 years [OASCL] p-value 0.49 | / | 88.7% (5 years) [BASCL]—89.2% (5 years [OASCL] p-value 0.59 | 86.8% (5 years) [BASCL]—84.2% (5 years [OASCL] p-value 0.42 | / | >N1, extracapsular spread |
| Atallah I et al. (2017) [26] | 53 | T1-T2 | 96 months (median) | 93.7% (5 years) | 95.6% (5 years) | 87.7% (5 years) | / | / | 11.3% (5 years) | Positive resection margin |
| Pescetto B et al. (2018) [27] | 53 | T1-T3 | 40.8 months (median) | 86% (3 years) | 95% (3 years) | 80% (3 years) | / | / | / | / |
| Number of treated patients, stage of tumor (pT), period of follow up, overall survival (OS), disease-specific survival (DSS), disease-free survival (DFS), laryngeal preservation (LP), and local control (LC), local recurrence (LR), OASCL, both arytenoids preserved SCPL (BASCL), one arytenoid preserved SCPL (OASCL). | ||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saraniti, C.; Verro, B.; Ciodaro, F.; Galletti, F. Oncological Outcomes of Primary vs. Salvage OPHL Type II: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 1837. https://doi.org/10.3390/ijerph19031837
Saraniti C, Verro B, Ciodaro F, Galletti F. Oncological Outcomes of Primary vs. Salvage OPHL Type II: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(3):1837. https://doi.org/10.3390/ijerph19031837
Chicago/Turabian StyleSaraniti, Carmelo, Barbara Verro, Francesco Ciodaro, and Francesco Galletti. 2022. "Oncological Outcomes of Primary vs. Salvage OPHL Type II: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 3: 1837. https://doi.org/10.3390/ijerph19031837
APA StyleSaraniti, C., Verro, B., Ciodaro, F., & Galletti, F. (2022). Oncological Outcomes of Primary vs. Salvage OPHL Type II: A Systematic Review. International Journal of Environmental Research and Public Health, 19(3), 1837. https://doi.org/10.3390/ijerph19031837






