Older Adults’ Perceptions and Recommendations Regarding a Falls Prevention Self-Management Plan Template Based on the Health Belief Model: A Mixed-Methods Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participant Sampling
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Sample Description
3.2. Perceptions Regarding the Falls-Prevention Self-Management Plan
3.3. Discrete Rankings of Items in the Falls Prevention Self-Management Plan
3.4. Recommend Revisions to the Plan
“a lot of times, a personality is something people cannot grasp on their own unless they see something that really points it out. And if you had a graphic showing how many, what the risk of falls were on an age line or something like that, to where they would see that there’s an urgency here, they can place themselves within this data.”
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moreland, B.; Kakara, R.; Henry, A. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years—United States, 2012–2018. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 875–881. [Google Scholar] [CrossRef]
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.; Stevens, J.; Drake, C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.H.; Yu, S. Effectiveness of multifactorial interventions in preventing falls among older adults in the community: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2020, 106, 103564. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; E Lamb, S.; Gates, S.; Cumming, R.G.; Rowe, B.H. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2008, 9, 1–373. [Google Scholar] [CrossRef]
- Stevens, J.A.; Burns, E. A CDC Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults;Centers for Disease Control and Prevention. National Center for Injury Prevention and Control. Division of Unintentional Injury Prevention. 2015. Available online: https://www.cdc.gov/homeandrecreationalsafety/pdf/falls/cdc_falls_compendium-2015-a.pdf (accessed on 24 November 2021).
- Stevens, J.A.; Lee, R. The Potential to Reduce Falls and Avert Costs by Clinically Managing Fall Risk. Am. J. Prev. Med. 2018, 55, 290–297. [Google Scholar] [CrossRef]
- Sjösten, N.M.; Salonoja, M.; Piirtola, M.; Vahlberg, T.J.; Isoaho, R.; Hyttinen, H.K.; Aarnio, P.T.; Kivelä, S.-L. A multifactorial fall prevention programme in the community-dwelling aged: Predictors of adherence. Eur. J. Public Health 2007, 17, 464–470. [Google Scholar] [CrossRef] [Green Version]
- Nithman, R.W.; Vincenzo, J.L. How steady is the STEADI? Inferential analysis of the CDC fall risk toolkit. Arch. Gerontol. Geriatr. 2019, 83, 185–194. [Google Scholar] [CrossRef]
- Nyman, S.R.; Victor, C.R. Older people’s participation in and engagement with falls prevention interventions in community settings: An augment to the Cochrane systematic review. Age Ageing 2011, 41, 16–23. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, R.; Dennis, S.; Hasan, I.; Slewa, J.; Chen, W.; Tian, D.; Bobba, S.; Zwar, N. A systematic review of chronic disease management interventions in primary care. BMC Fam. Pract. 2018, 19, 11. [Google Scholar] [CrossRef]
- Hessler, D.M.; Fisher, L.; Bowyer, V.; Dickinson, L.M.; Jortberg, B.T.; Kwan, B.; Fernald, D.H.; Simpson, M.; Dickinson, W.P. Self-management support for chronic disease in primary care: Frequency of patient self-management problems and patient reported priorities, and alignment with ultimate behavior goal selection. BMC Fam. Pract. 2019, 20, 120. [Google Scholar] [CrossRef] [Green Version]
- Royal College of Physicians. Shared Decision-Making: Information and Resources. Available online: https://www.rcplondon.ac.uk/projects/outputs/shared-decision-making-information-and-resource (accessed on 10 January 2022).
- Radecki, B.; Keen, A.; Miller, J.; McClure, J.K.; Kara, A. Innovating fall safety: Engaging patients as experts. J. Nurs. Care Qual. 2020, 35, 220–226. [Google Scholar] [CrossRef]
- Dykes, P.C.; Burns, Z.; Adelman, J.; Benneyan, J.; Bogaisky, M.; Carter, E.; Ergai, A.; Lindros, M.E.; Lipsitz, S.R.; Scanlan, M. Evaluation of a patient-centered fall-prevention tool kit to reduce falls and injuries: A nonrandomized controlled trial. JAMA Netw. Open 2020, 3, e2025889. [Google Scholar] [CrossRef]
- Vonnes, C.; Wolf, D. Fall risk and prevention agreement: Engaging patients and families with a partnership for patient safety. BMJ Open Qual. 2017, 6, e000038. [Google Scholar] [CrossRef] [Green Version]
- Szanton, S.L.; Leff, B.; Wolff, J.L.; Roberts, L.; Gitlin, L.N. Home-Based Care Program Reduces Disability And Promotes Aging In Place. Health Aff. 2016, 35, 1558–1563. [Google Scholar] [CrossRef]
- Taylor, J.L.; Roberts, L.; Hladek, M.D.; Liu, M.; Nkimbeng, M.; Boyd, C.M.; Szanton, S.L. Achieving self-management goals among low income older adults with functional limitations. Geriatr. Nurs. 2019, 40, 424–430. [Google Scholar] [CrossRef]
- Szanton, S.L.; Wolff, J.; Leff, B.; Thorpe, R.; Tanner, E.; Boyd, C.; Xue, Q.; Guralnik, J.; Bishai, D.; Gitlin, L. CAPABLE trial: A randomized controlled trial of nurse, occupational therapist and handyman to reduce disability among older adults: Rationale and design. Contemp. Clin. Trials 2014, 38, 102–112. [Google Scholar] [CrossRef] [Green Version]
- Haas, R.; Mason, W.; Haines, T.P. Difficulties Experienced in Setting and Achieving Goals by Participants of a Falls Prevention Programme: A Mixed-Methods Evaluation. Physiother. Can. 2014, 66, 413–422. [Google Scholar] [CrossRef] [Green Version]
- Reuben, D.B.; Gazarian, P.; Alexander, N.; Araujo, K.; Baker, D.; Bean, J.F.; Boult, C.; Charpentier, P.; Duncan, P.; Latham, N.; et al. The Strategies to Reduce Injuries and Develop Confidence in Elders Intervention: Falls Risk Factor Assessment and Management, Patient Engagement, and Nurse Co-management. J. Am. Geriatr. Soc. 2017, 65, 2733–2739. [Google Scholar] [CrossRef] [Green Version]
- Bhasin, S.; Gill, T.; Reuben, D.B.; Latham, N.K.; Gurwitz, J.H.; Dykes, P.; McMahon, S.; Storer, T.W.; Duncan, P.W.; A Ganz, D.; et al. Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE): A Cluster-Randomized Pragmatic Trial of a Multifactorial Fall Injury Prevention Strategy: Design and Methods. J. Gerontol. Ser. A 2017, 73, 1053–1061. [Google Scholar] [CrossRef]
- Peek, K.; Carey, M.; MacKenzie, L.; Sanson-Fisher, R. Characteristics associated with high levels of patient-reported adherence to self-management strategies prescribed by physiotherapists. Int. J. Ther. Rehabil. 2020, 27, 1–15. [Google Scholar] [CrossRef]
- Pinnock, H.; Barwick, M.; Carpenter, C.; Eldridge, S.; Grandes, G.; Griffiths, C.J.; Rycroft-Malone, J.; Meissner, P.; Murray, E.; Patel, A.; et al. Standards for Reporting Implementation Studies (StaRI) Statement. BMJ 2017, 356, i6795. [Google Scholar] [CrossRef] [Green Version]
- Sheeran, P.; Maki, A.; Montanaro, E.; Avishai-Yitshak, A.; Bryan, A.; Klein, W.M.P.; Miles, E.; Rothman, A.J. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychol. 2016, 35, 1178–1188. [Google Scholar] [CrossRef]
- Hagger, M.S.; Weed, M. DEBATE: Do interventions based on behavioral theory work in the real world? Int. J. Behav. Nutr. Phys. Act. 2019, 16, 36. [Google Scholar] [CrossRef] [Green Version]
- Janz, N.K.; Becker, M.H. The Health Belief Model: A Decade Later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef] [Green Version]
- Davidhizar, R. Critique of the health-belief model. J. Adv. Nurs. 1983, 8, 467–472. [Google Scholar] [CrossRef]
- Glanz, K.; Bishop, D.B. The Role of Behavioral Science Theory in Development and Implementation of Public Health Interventions. Annu. Rev. Public Health 2010, 31, 399–418. [Google Scholar] [CrossRef] [Green Version]
- Jones, C.; Smith, H.; Llewellyn, C. Evaluating the effectiveness of health belief model interventions in improving adherence: A systematic review. Heal. Psychol. Rev. 2013, 8, 253–269. [Google Scholar] [CrossRef]
- Kaushal, N.; Preissner, C.; Charles, K.; Knäuper, B. Differences and similarities of physical activity determinants between older adults who have and have not experienced a fall: Testing an extended health belief model. Arch. Gerontol. Geriatr. 2021, 92, 104247. [Google Scholar] [CrossRef]
- Huang, S.F.; Tzeng, Y.M.; Chen, S.F. Validation of a Prediction Model for Likelihood of Fall Prevention Actions in Community-Dwelling Older Adults: Application of the Health Belief Model. Int. J. Gerontol. 2021, 15, 34–38. [Google Scholar]
- Ahn, S.; Oh, J. Effects of a health-belief-model-based osteoporosis- and fall-prevention program on women at early old age. Appl. Nurs. Res. 2021, 59, 151430. [Google Scholar] [CrossRef]
- The STRIDE Study, Strategies to Reduce Injuries and Develop Confidence in Elders. Available online: https://www.stride-study.org/ (accessed on 10 January 2022).
- Krueger, R.A. Focus Groups: A Practical Guide for Applied Research; Sage Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Bailey, C.A. A Guide to Qualitative Field Research; Sage Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Laing, S.S.; Silver, I.F.; York, S.; Phelan, E.A. Fall Prevention Knowledge, Attitude, and Practices of Community Stakeholders and Older Adults. J. Aging Res. 2011, 2011, 395357. [Google Scholar] [CrossRef] [Green Version]
- Stevens, J.A.; Sleet, D.A.; Rubenstein, L.Z. The Influence of Older Adults’ Beliefs and Attitudes on Adopting Fall Prevention Behaviors. Am. J. Lifestyle Med. 2018, 12, 324–330. [Google Scholar] [CrossRef]
- Hill, K.D.; Day, L.; Haines, T.P. What factors influence community-dwelling older people’s intent to undertake multifactorial fall prevention programs? Clin. Interv. Aging 2014, 9, 2045–2053. [Google Scholar] [CrossRef] [Green Version]
- French, D.P.; Olander, E.K.; Chisholm, A.; Sharry, J.M. Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review. Ann Behav. Med. 2014, 48, 225–234. [Google Scholar] [CrossRef] [Green Version]
- Sulat, J.S.; Prabandari, Y.S.; Sanusi, R.; Hapsari, E.D.; Santoso, B. The validity of health belief model variables in predicting behavioral change: A scoping review. Health Educ. J. 2018, 6, 499–512. [Google Scholar] [CrossRef]

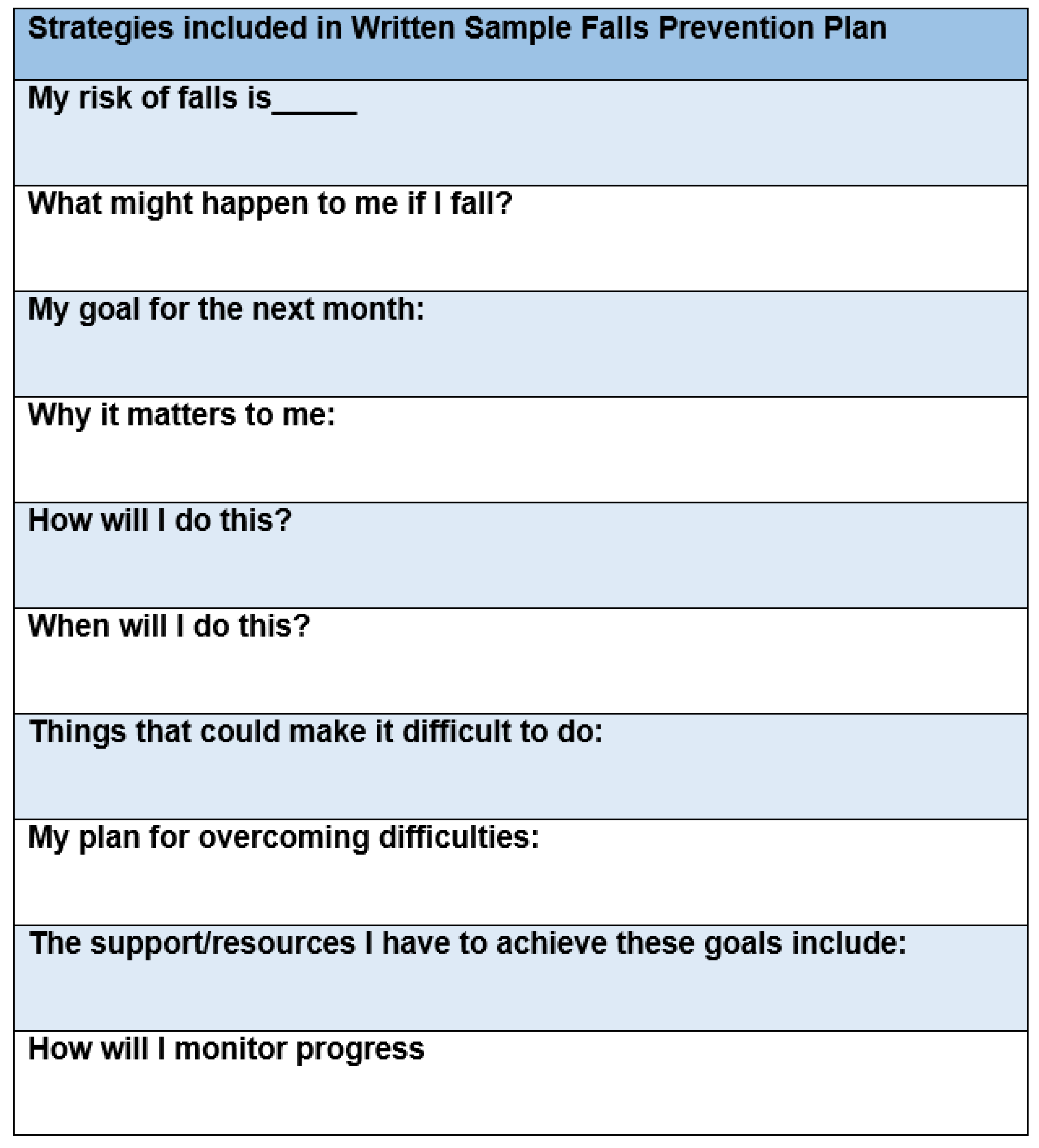
| Items Included in Written Health Belief Model-Informed Falls Prevention Self-Management Plan | Questions: We Are Seeking Your Opinion on the Following: How Does or Does Not This Sample Falls Prevention Plan Help Older Adults: | Constructs of the Health Belief Model |
|---|---|---|
| My risk of falls is_____ | Understand and acknowledge their falls risk? | Knowledge, perceived susceptibility |
| What might happen to me if I fall? | Understand what may happen if they suffer a fall? | Perceived threat, perceived severity |
| My goal for the next month: | Promote engagement and goals? | Self-efficacy, cues to action |
| Why it matters to me: | See the personal benefit to falls prevention? | Benefit, personal relevance |
| How will I do this? | Promote engagement and goals? | Perceived facilitators and barriers, self-efficacy |
| When will I do this? | Make a plan? | Cues to action, likelihood to take action |
| Things that could make it difficult to do: | Address barriers to undergoing falls prevention? | Perceived barriers |
| My plan for overcoming difficulties: | Provide facilitators to undergoing falls prevention? | Perceived facilitators, self-efficacy |
| The support/resources I have to achieve these goals include: | Provide resources and social support to achieve goals? | Cues to action, self-efficacy, social support |
| How will I monitor progress | Provide accountability to goals? | Cues to action, self-efficacy, social support |
| Characteristic | n (27) |
|---|---|
| Sex | |
| Male | 13 |
| Female | 14 |
| Age a | |
| Male | 79.4 |
| Female | 76.1 |
| Race/Ethnicity | |
| Non-Hispanic—white | 21 |
| Did not state | 6 |
| Educational level | |
| Less than a high school diploma | 2 |
| High school degree or equivalent (GED) | 0 |
| Some college, no degree | 11 |
| Associate’s degree | 2 |
| Bachelor’s degree | 5 |
| Master’s degree | 3 |
| Professional degree (MD, DDS, DVM) | 0 |
| Doctorate (PhD, EdD) | 2 |
| No answer | 2 |
| Yearly income | |
| Less than $20,000 | 3 |
| $20,000 to $34,999 | 6 |
| $35,000 to $49,999 | 2 |
| $50,000 to $74,999 | 5 |
| $75,000 to $99,999 | 7 |
| Over $100,000 | 3 |
| No answer | 1 |
| Marital Status | |
| Married, or in a domestic partnership | 19 |
| Widowed | 8 |
| Experienced a fall in the last year | |
| Yes | 10 |
| No | 17 |
| Number of falls in the last year | |
| None | 17 |
| 1 | 2 |
| 2 | 2 |
| ≥3 | 3 |
| No answer | 3 |
| Falls resulting in injury | |
| Yes | 7 |
| No | 6 |
| No answer | 14 |
| Falls Prevention Self-Management Plan Item | Ranking Each Item on the Plan with Respect to One Another with a Discrete Number (1–10); 1 Being the Most Important Item and 10 Being the Least (n = 27) |
|---|---|
| My risk of falls is_____ | Range = 1–9 Mean = 3.0 ± 2.8 Mode = 1 |
| What might happen to me if I fall? | Range = 1–10 Mean = 2.6 ± 1.0 Mode = 2 |
| My goal for the next month: | Range = 1–10 Mean = 5.7 ± 3.0 Mode = 8 |
| Why it matters to me: | Range = 1–9 Mean = 4.3 ± 2.2 Mode = 3 |
| How will I do this? | Range = 1–10 Mean = 4.6 ± 2.5 Mode = 4 |
| When will I do this? | Range = 2–10 Mean = 5.1 ± 2.3 Mode = 5 |
| Things that could make it difficult to do: | Range = 1–10 Mean = 5.5 ± 3.1 Mode = 9 |
| My plan for overcoming difficulties: | Range = 1–10 Mean = 5.4 ± 2.9 Mode = 5 |
| The support/resources I have to achieve these goals include: | Range = 1–10 Mean = 5.3 ± 3.4 Mode = 3 |
| How will I monitor progress | Range = 1–10 Mean = 6.6 ± 3.8 Mode = 10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vincenzo, J.L.; Patton, S.K.; Lefler, L.L.; McElfish, P.A.; Wei, J.; Curran, G.M. Older Adults’ Perceptions and Recommendations Regarding a Falls Prevention Self-Management Plan Template Based on the Health Belief Model: A Mixed-Methods Study. Int. J. Environ. Res. Public Health 2022, 19, 1938. https://doi.org/10.3390/ijerph19041938
Vincenzo JL, Patton SK, Lefler LL, McElfish PA, Wei J, Curran GM. Older Adults’ Perceptions and Recommendations Regarding a Falls Prevention Self-Management Plan Template Based on the Health Belief Model: A Mixed-Methods Study. International Journal of Environmental Research and Public Health. 2022; 19(4):1938. https://doi.org/10.3390/ijerph19041938
Chicago/Turabian StyleVincenzo, Jennifer L., Susan K. Patton, Leanne L. Lefler, Pearl A. McElfish, Jeanne Wei, and Geoffrey M. Curran. 2022. "Older Adults’ Perceptions and Recommendations Regarding a Falls Prevention Self-Management Plan Template Based on the Health Belief Model: A Mixed-Methods Study" International Journal of Environmental Research and Public Health 19, no. 4: 1938. https://doi.org/10.3390/ijerph19041938







