Sensor Cell Network for Pressure, Temperature and Position Detection on Wheelchair Users
Abstract
:1. Introduction
2. Sensor Cells Sensing Principle and Design
3. Sensor Cell Characterization and Calibration
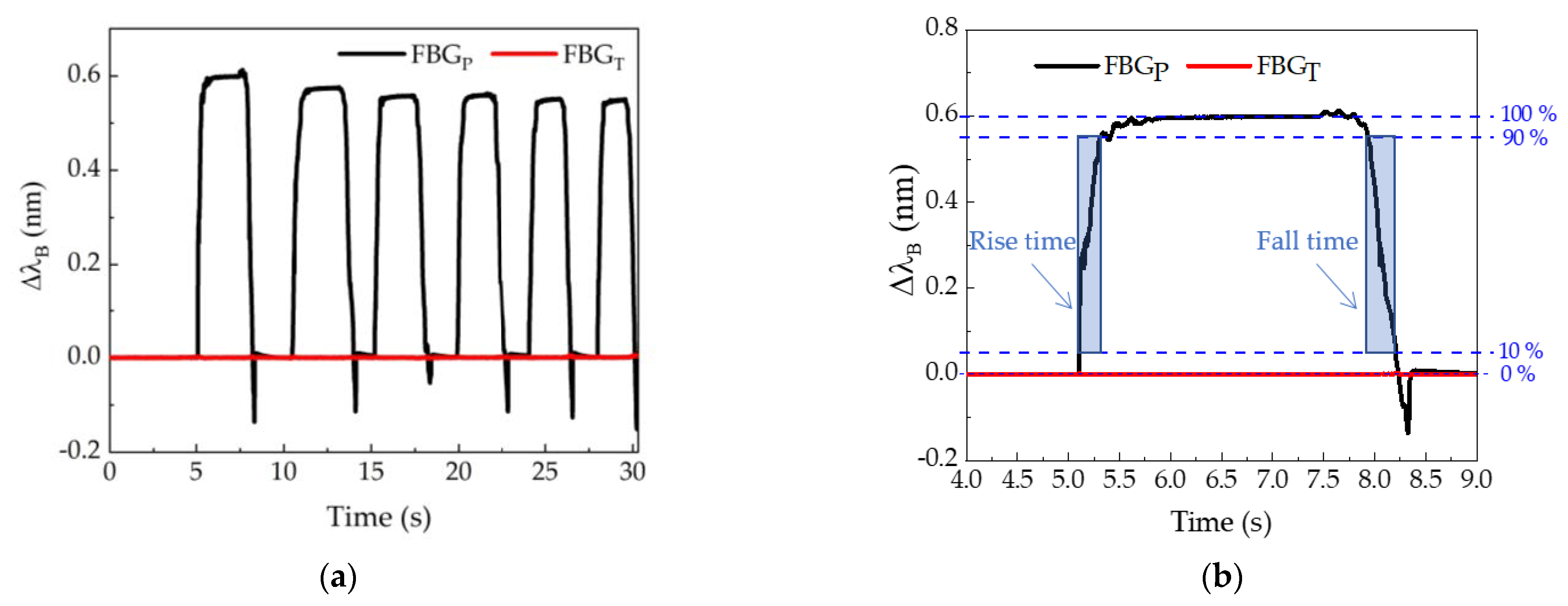
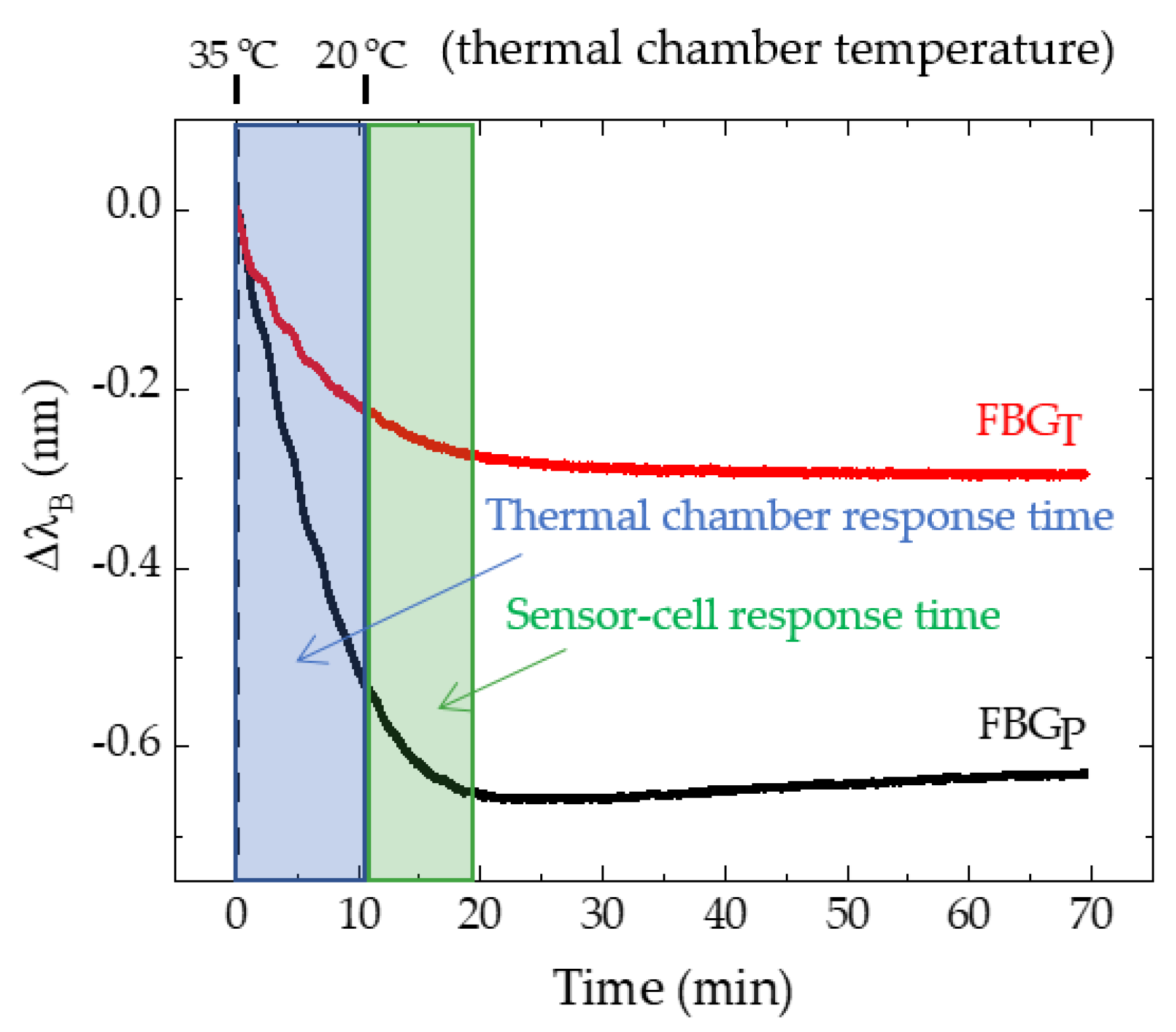
3.1. Response Time of the Sensor Cell to Pressure and Temperature Variations
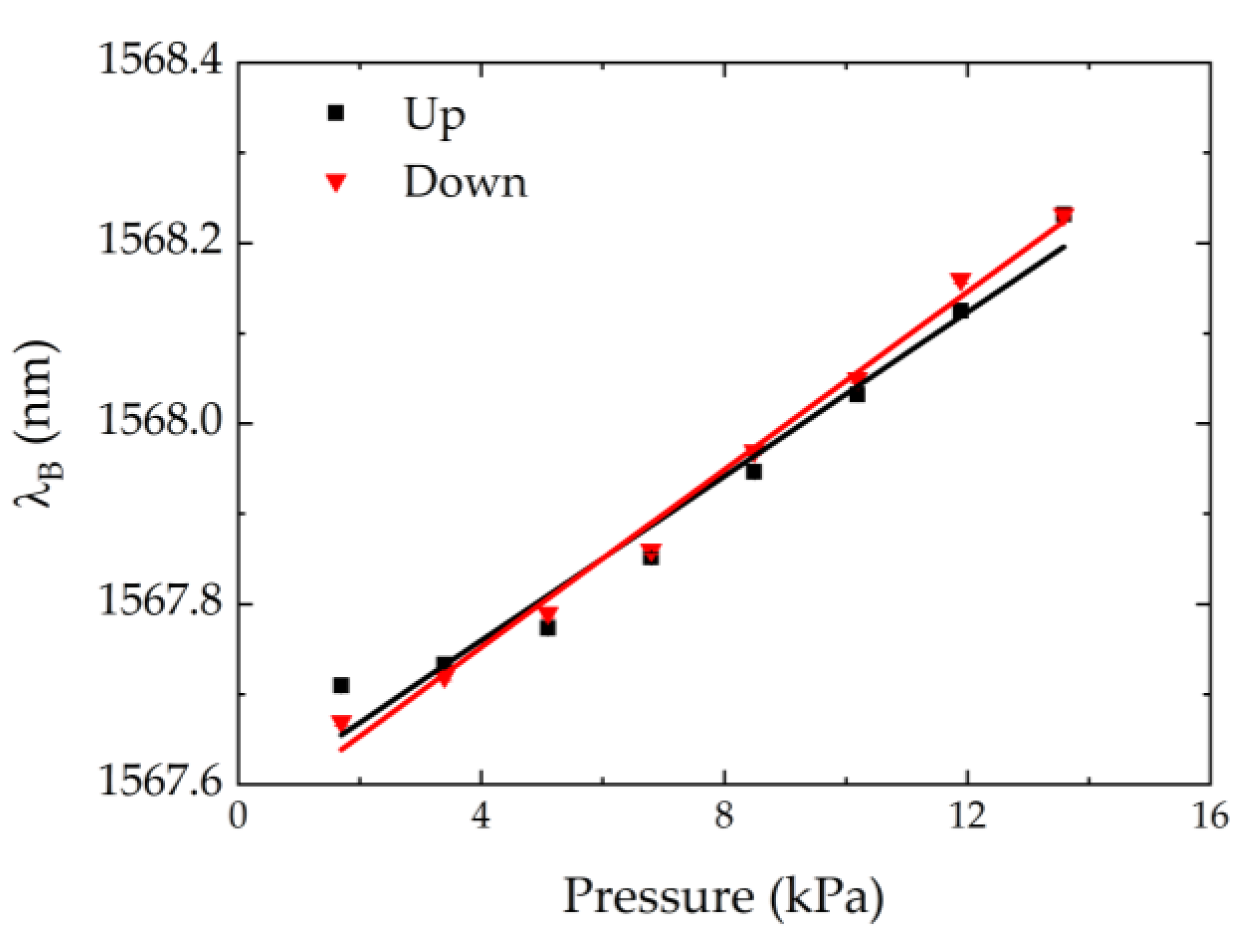
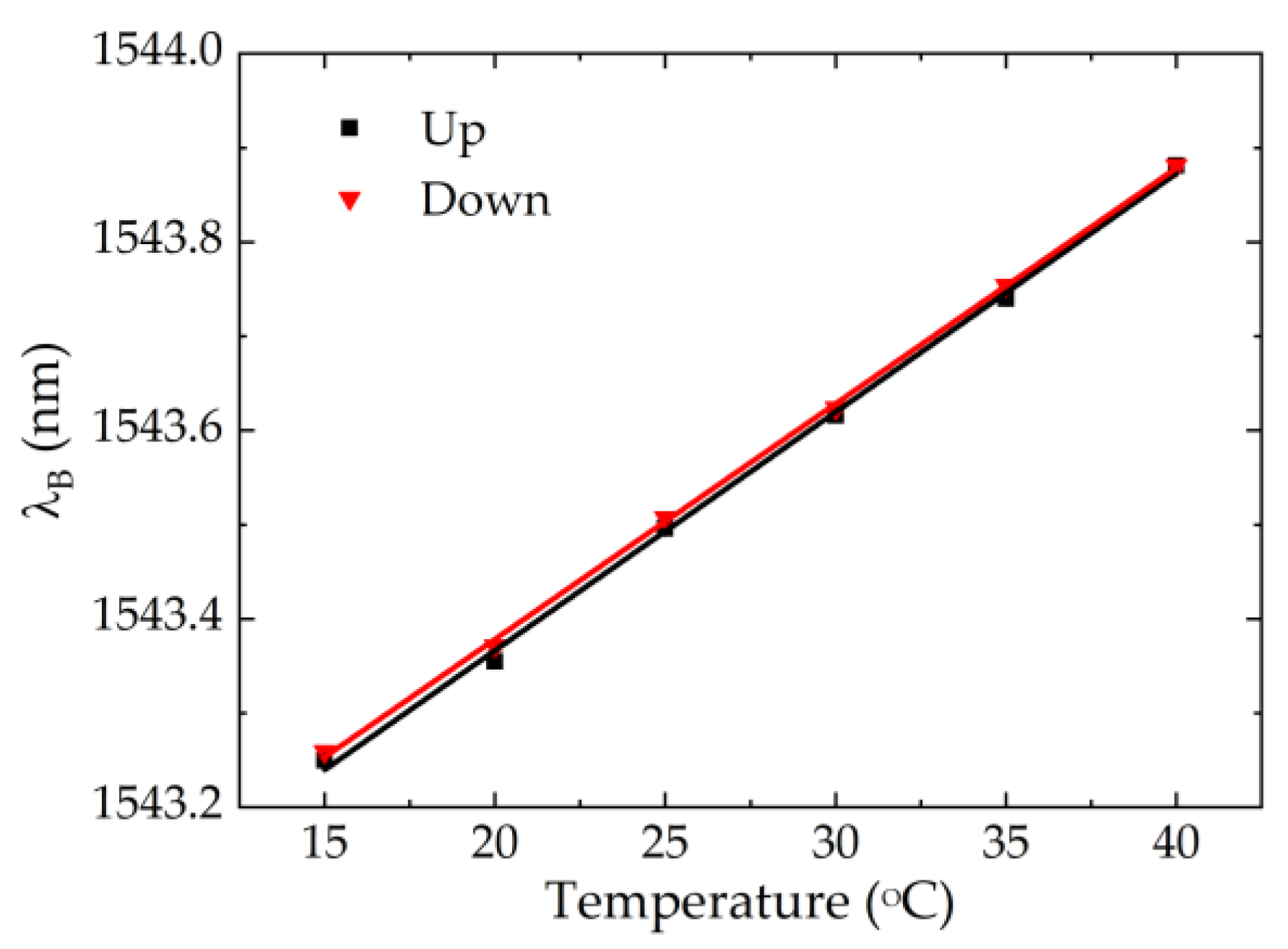
3.2. Calibration to Pressure and Temperature
3.3. Compensation for the Temperature Effect
4. Implementation of Sensor Cells in the Wheelchair
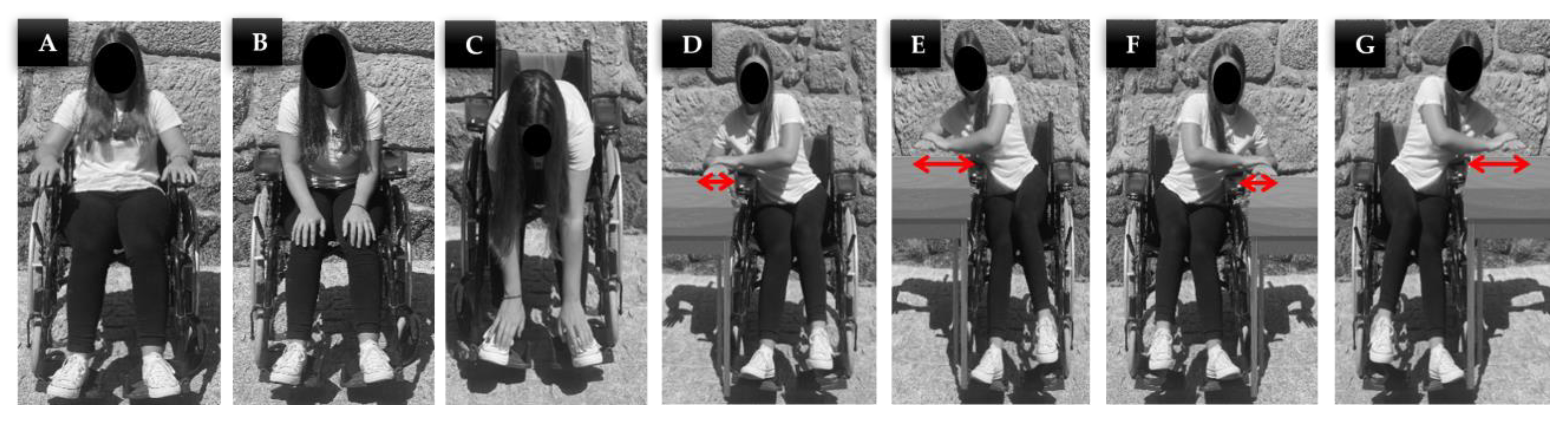
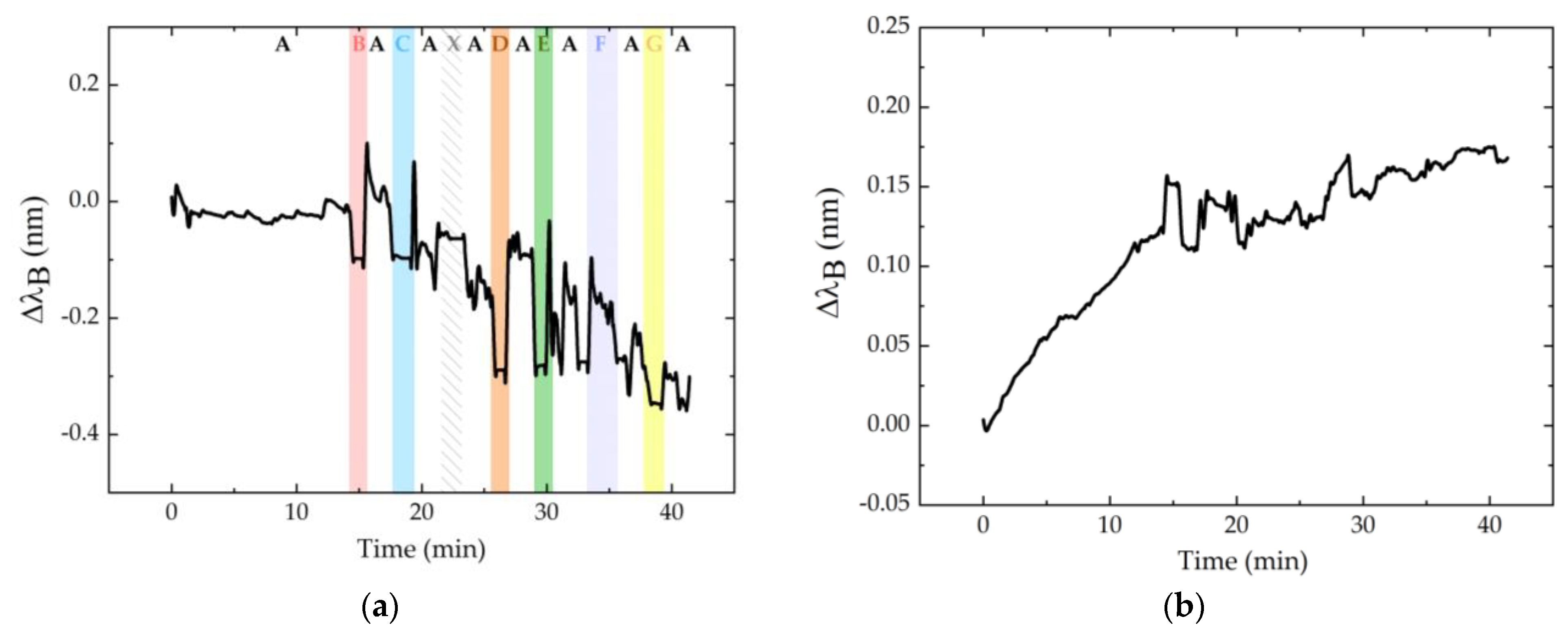
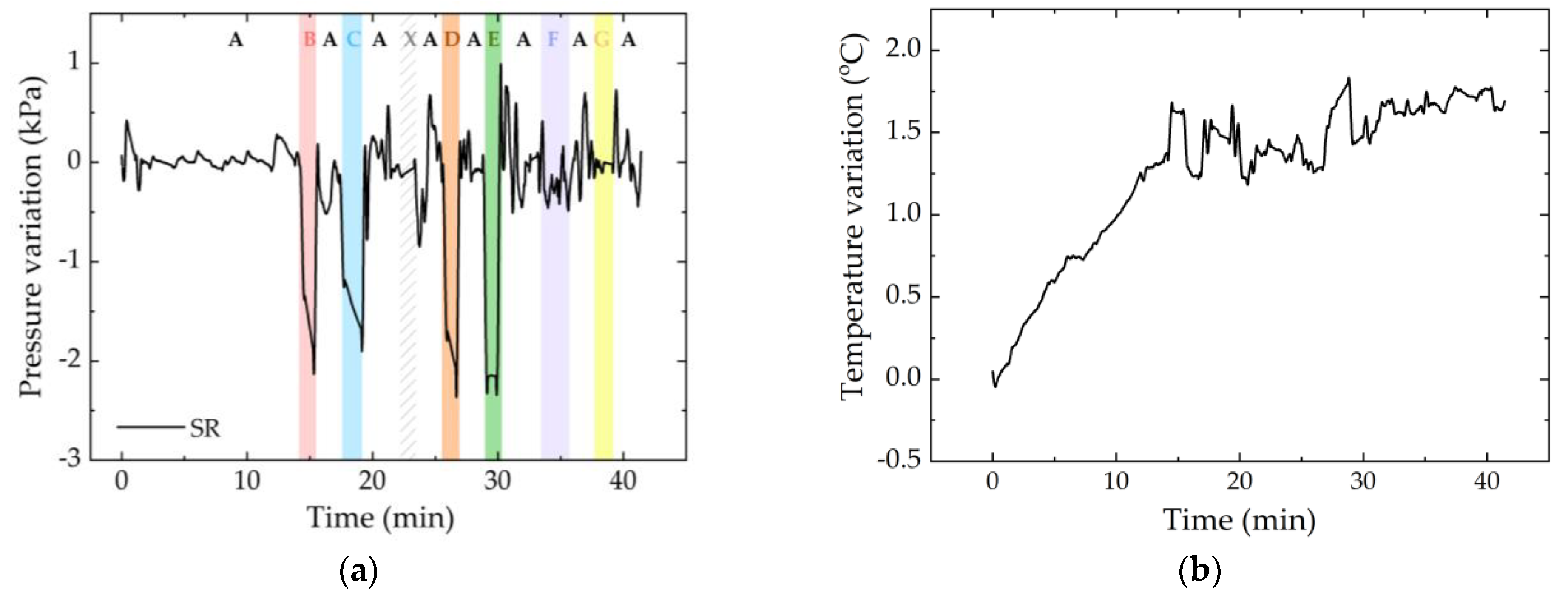
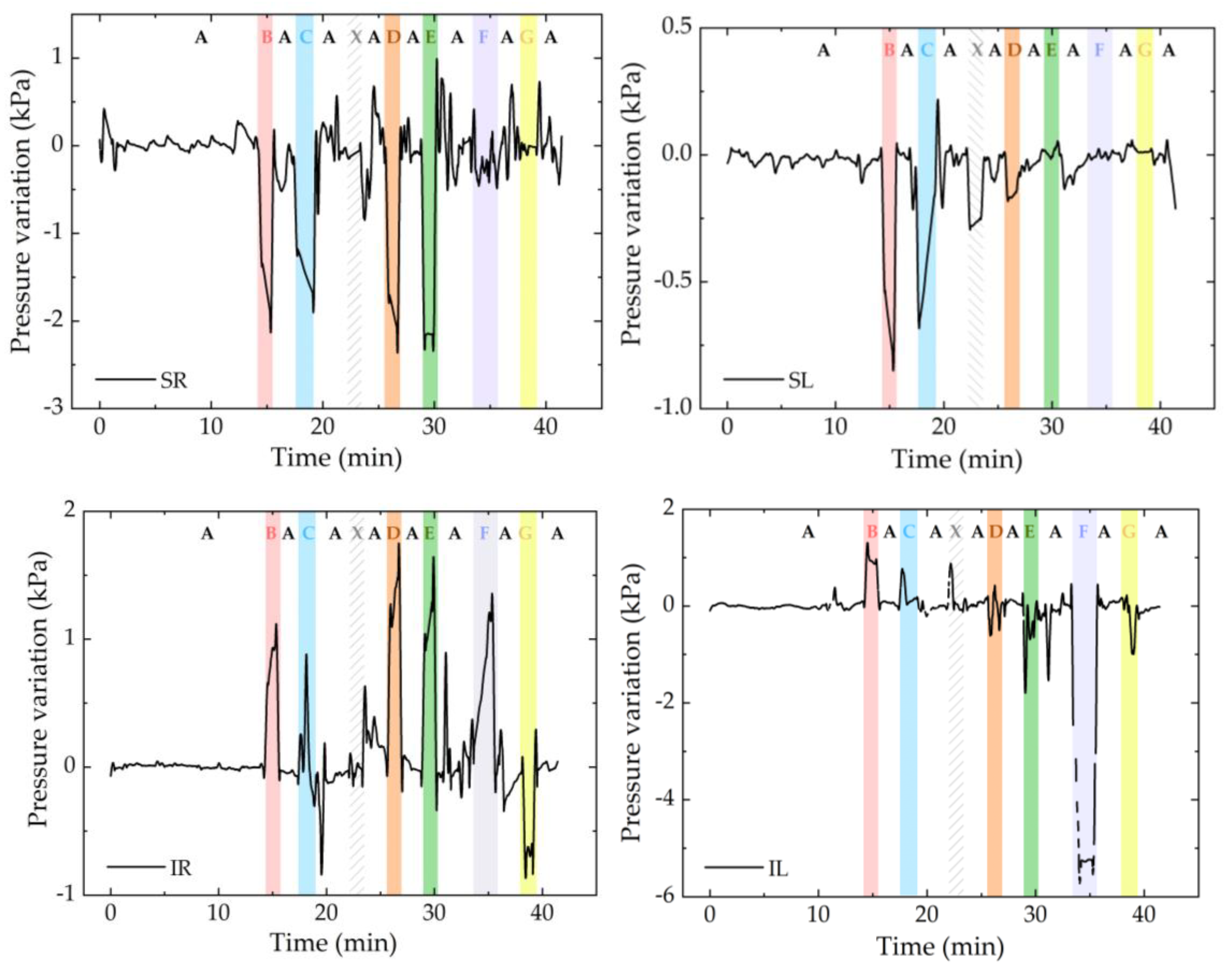
4.1. First Test: Sequence of Pressure Relief Positions
4.2. Second Test: Random of Pressure Relief Positions
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Han, D.K.; Kim, J.M.; Cha, E.J.; Lee, T.S. Wheelchair type biomedical system with event-recorder function. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, CB, Canada, 21–24 August 2008. [Google Scholar]
- Kim, J.M.; Hong, J.H.; Cho, M.C.; Cha, E.J.; Lee, T.S. Wireless biomedical signal monitoring device on wheelchair using noncontact electro-mechanical film sensor. In Proceedings of the 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007. [Google Scholar]
- Gassara, H.E.; Almuhamed, S.; Moukadem, A.; Schacher, L.; Dieterlen, A.; Adolphe, D. Smart wheelchair: Integration of multiple sensors. In Proceedings of the IOP Conference Series: Materials Science and Engineering, Putrajaya, Malaysia, 20–22 October 2017. [Google Scholar]
- Dai, R.; Sonenblum, S.E.; Sprigle, S. A robust wheelchair pressure relief monitoring system. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012. [Google Scholar]
- Brem, H.; Maggi, J.; Nierman, D.; Rolnitzky, L.; Bell, D.; Rennert, R.; Golinko, M.; Yan, A.; Lyder, C.; Vladeck, B. High cost of stage IV pressure ulcers. Am. J. Surg. 2010, 200, 473–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Presti, D.L.; Massaroni, C.; Leitão, C.; Domingues, M.F.; Sypabekova, M.; Barrera, D.; Floris, I.; Massari, L.; Oddo, C.; Sales, S.; et al. Fiber Bragg gratings for medical applications and future challenges: A review. IEEE Access 2020, 8, 156863–156888. [Google Scholar] [CrossRef]
- Sonenblum, S.E.; Vonk, T.E.; Janssen, T.W.; Sprigle, S.H. Effects of wheelchair cushions and pressure relief maneuvers on ischial interface pressure and blood flow in people with spinal cord injury. Arch. Phys. Med. Rehabil. 2014, 95, 1350–1357. [Google Scholar] [CrossRef] [PubMed]
- Verbunt, M.; Bartneck, C. Sensing senses: Tactile feedback for the prevention of Decubitus ulcers. Appl. Psychophysiol. Biofeedback 2010, 35, 243–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gadd, M.M. Preventing hospital-acquired pressure ulcers: Improving quality of outcomes by placing emphasis on the braden subscale scores. J. Wound Ostomy Cont. Nurs. 2012, 39, 292–294. [Google Scholar] [CrossRef] [PubMed]
- Demarré, L.; Van Lancker, A.; Van Hecke, A.; Verhaeghe, S.; Grypdonck, M.; Lemey, J.; Annemans, L.; Beeckman, D. The cost of prevention and treatment of pressure ulcers: A systematic review. Int. J. Nurs. Stud. 2015, 52, 1754–1774. [Google Scholar] [CrossRef] [PubMed]
- Sprigle, S.; Sonenblum, S. Assessing evidence supporting redistribution of pressure for pressure ulcer prevention: A review. J. Rehabil. Res. Dev. 2011, 48, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Chenu, O.; Vuillerme, N.; Bucki, M.; Diot, B.; Cannard, F.; Payan, Y. TexiCare: An innovative embedded device for pressure ulcer prevention. Preliminary results with a paraplegic volunteer. J. Tissue Viability 2013, 22, 83–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sonenblum, S.E.; Sprigle, S.H.; Martin, J.S. Everyday sitting behavior of full-time wheelchair users. J. Rehabil. Res. Dev. 2016, 53, 585–598. [Google Scholar] [CrossRef]
- Yang, Y.S.; Pan, C.T.; Ho, W.H. Sensor-based remote temperature and humidity monitoring device embedded in wheelchair cushion. Sens. Mater. 2018, 30, 1807–1814. [Google Scholar] [CrossRef]
- Tavares, C.; Domingues, M.F.; Paixão, T.; Alberto, N.; Silva, H.; Antunes, P. Wheelchair pressure ulcer prevention using FBG based sensing devices. Sensors 2020, 20, 212. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, K.; Chauhan, N. Pressure ulcers: Back to the basics. Indian J. Plast. Surg. 2012, 45, 244–254. [Google Scholar] [CrossRef] [PubMed]


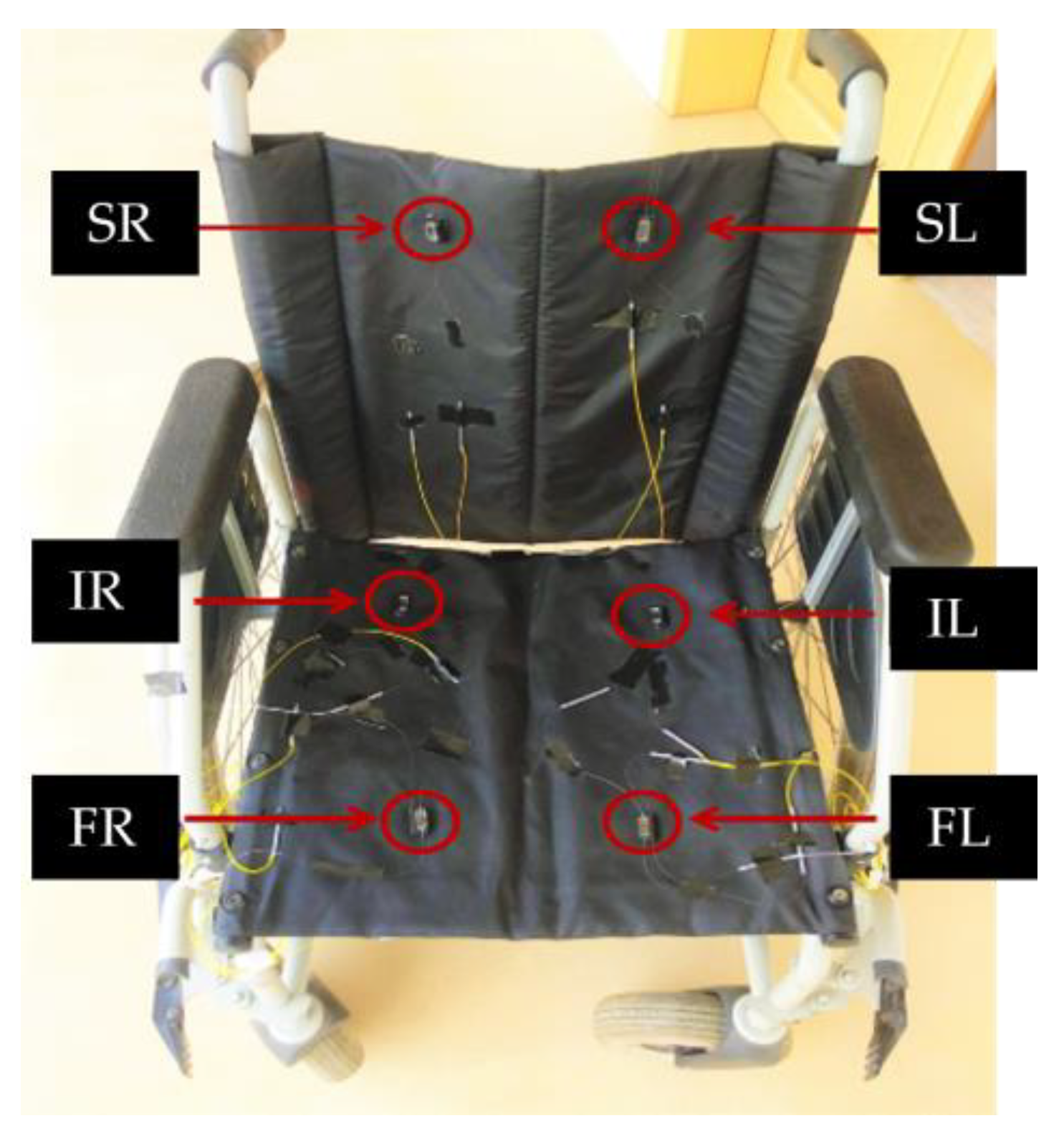



| Sensitivity Coefficient | SR Scapula Right | SL Scapula Left | IR Ischium Right | IL Ischium Left | FR Femur Right | FL Femur Left |
|---|---|---|---|---|---|---|
| 𝑆P,FBGP (pm/kPa) | 87.0 ± 8.0 | 46.0 ± 3.0 | 83.7 ± 0.7 | 16.0 ± 1.0 | 89.0 ± 6.0 | 163.0 ± 11.0 |
| 𝑆P,FBGT (pm/kPa) | −4.5 ± 0.4 | −2.7 ± 0.3 | −1.5 ± 0.3 | −10.0 ± 1.0 | −11.4 ± 0.4 | −0.2 ± 0.1 |
| 𝑆𝑇,FBGP (pm/°C) | 22.0 ± 0.2 | 54.0 ± 5.0 | 21.5 ± 0.2 | 15.0 ± 0.3 | 18.2 ± 0.1 | 21.6 ± 0.2 |
| 𝑆𝑇,FBGT (pm/°C) | 89.0 ± 1.0 | 19.6 ± 0.1 | 27.1 ± 0.7 | 25.3 ± 0.4 | 116.0 ± 2.0 | 9.3 ± 0.1 |
| Sensor Cells | Expected Results |
|---|---|
| SR and SL | After the initial position A, in general, there should be a negative variation of the Bragg wavelength in the periods corresponding to positions B, C, D, E, F, and G, since the body is no longer in contact with the sensors when these relief positions are exercised. |
| IR and FR | Increased Bragg wavelength shift in the period corresponding to positions B, C, D, and E. Decrease in the periods corresponding to positions F and G, with the latter being more accentuated. In position C, a greater variation on the FR sensor cell than the IR sensor cell is expected. |
| IL and FL | Increased Bragg wavelength shift in the periods corresponding to positions B, C, F, and G. Decrease in the positions D and E (more accentuated in this case). In position C, a greater variation on the FL sensor cell than on the IL sensor cell is expected. |
| Sensor Cell Behavior and Predicted Position | Real Position |
|---|---|
| In the first 2 min, there was a positive pressure variation in FR and IL, and a decrease in SR, that is, the user did not have the shoulder blades supported on the wheelchair structure and there was pressure in both the femoral and ischial areas (left and right), corresponding only to position B. | B |
| The pressure in SR was maintained, increased even more in relation to the previous position in FR, and decreased abruptly in IL. This was only verified when the wheelchair user was too inclined to the right, corresponding to position E. | E |
| There was a positive variation in SR corresponding to the position in which the wheelchair user supported the shoulder blades in the area where the sensor cell was located. This variation occurred exclusively for position A, and was confirmed by the variations observed in the remaining sensor cells. | A |
| There was a null variation in SR for the rest of the test, that is, position A was not checked again. As there was an abrupt negative variation in FR and a positive variation in IL, it was concluded that the wheelchair user was excessively tilted to the left, being in the G position. | G |
| The pressure increased in FR and decreased in IL, that is, the wheelchair user was not only exercising pressure on the sensor cells positioned on the left side. As the pressure was higher in the femur area, the user should have been in position C. | C |
| There was again a pressure decrease in the FR sensor cell and an increase in IL; however, this was not so pronounced, corresponding to position F. | F |
| There was an increase in the pressure felt by the FR and a decrease in IL; however, both were slight variations, corresponding to position D. | D |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tavares, C.; Real, D.; Domingues, M.d.F.; Alberto, N.; Silva, H.; Antunes, P. Sensor Cell Network for Pressure, Temperature and Position Detection on Wheelchair Users. Int. J. Environ. Res. Public Health 2022, 19, 2195. https://doi.org/10.3390/ijerph19042195
Tavares C, Real D, Domingues MdF, Alberto N, Silva H, Antunes P. Sensor Cell Network for Pressure, Temperature and Position Detection on Wheelchair Users. International Journal of Environmental Research and Public Health. 2022; 19(4):2195. https://doi.org/10.3390/ijerph19042195
Chicago/Turabian StyleTavares, Cátia, Daniela Real, Maria de Fátima Domingues, Nélia Alberto, Hugo Silva, and Paulo Antunes. 2022. "Sensor Cell Network for Pressure, Temperature and Position Detection on Wheelchair Users" International Journal of Environmental Research and Public Health 19, no. 4: 2195. https://doi.org/10.3390/ijerph19042195
APA StyleTavares, C., Real, D., Domingues, M. d. F., Alberto, N., Silva, H., & Antunes, P. (2022). Sensor Cell Network for Pressure, Temperature and Position Detection on Wheelchair Users. International Journal of Environmental Research and Public Health, 19(4), 2195. https://doi.org/10.3390/ijerph19042195










