Thirty Minutes Identified as the Threshold for Development of Pain in Low Back and Feet Regions, and Predictors of Intensity of Pain during 1-h Laboratory-Based Standing in Office Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Procedure
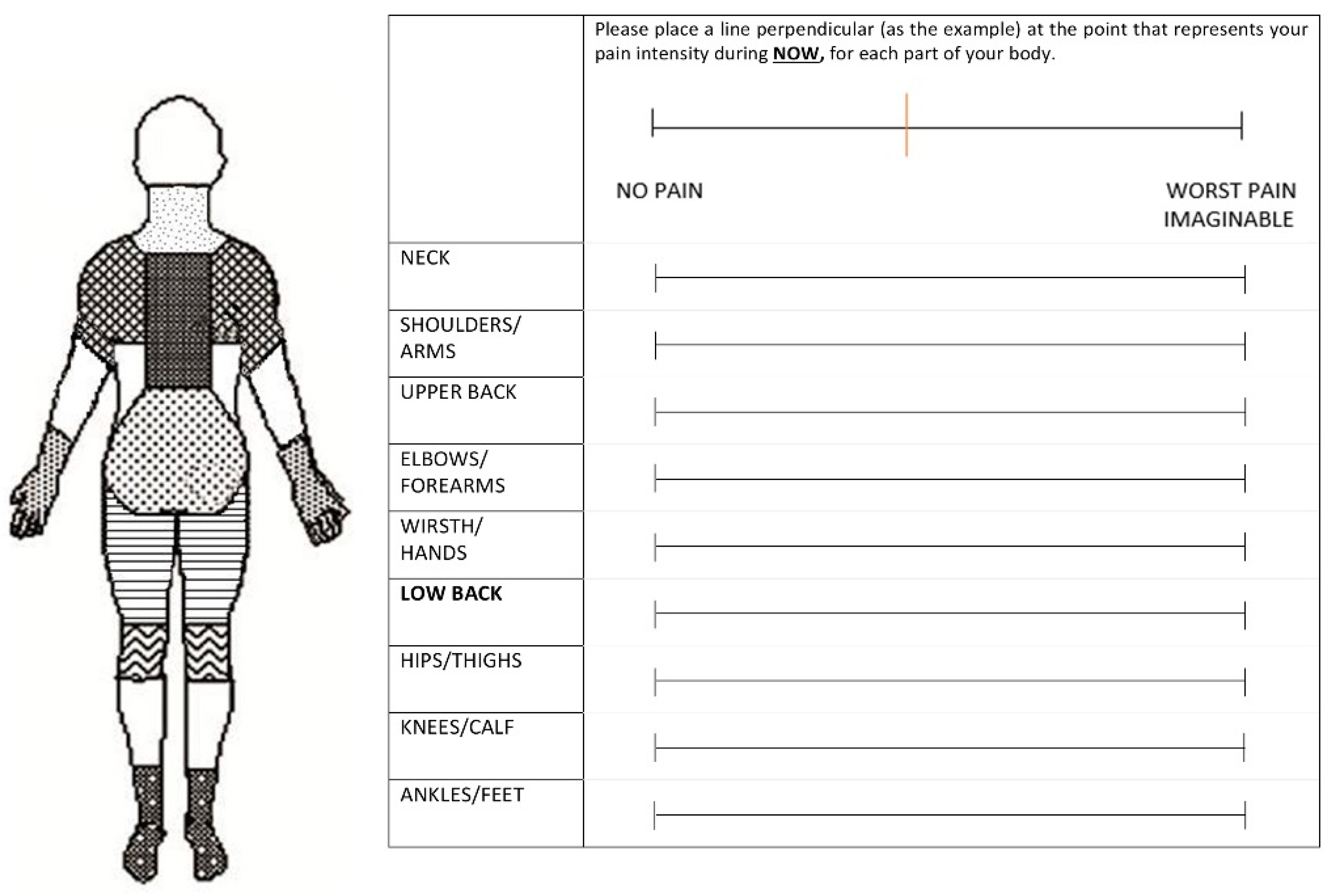
2.3. Measurements
2.4. Statistical Analysis
3. Results
3.1. Standing-Time Effect on Pain Status: Any Reported Pain
3.2. Standing-Time Effect on Pain Status: Intensity of Pain
3.3. Association of Individual, Physical and Psychosocial Factors with Pain Ratings over Time
3.4. Regression Analysis-Predicting the Magnitude of Low-Back Pain throughout of 1-h Standing Task
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dutheil, F.; Duclos, M.; Esquirol, Y. Editorial: Sedentary Behaviors at Work. Front. Public Health 2020, 8, 57. [Google Scholar] [CrossRef] [PubMed]
- Roffey, D.M.; Wai, E.K.; Bishop, P.; Kwon, B.K.; Dagenais, S. Causal Assessment of Occupational Standing or Walking and Low Back Pain: Results of a Systematic Review. Spine J. 2010, 10, 262–272. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, D.E.; de Luca, K.; Funabashi, M.; Breen, A.; Wong, A.Y.L.; Johansson, M.S.; Ferreira, M.L.; Swab, M.; Neil Kawchuk, G.; Adams, J.; et al. Association of Exposures to Seated Postures With Immediate Increases in Back Pain: A Systematic Review of Studies With Objectively Measured Sitting Time. J. Manip. Physiol. Ther. 2020, 43, 1–12. [Google Scholar] [CrossRef]
- Korshøj, M.; Hallman, D.M.; Mathiassen, S.E.; Aadahl, M.; Holtermann, A.; Jørgensen, M.B. Is Objectively Measured Sitting at Work Associated with Low-Back Pain? A Cross Sectional Study in the DPhacto Cohort. Scand. J. Work. Environ. Health 2018, 44, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Bu, W.; Chen, Y.; Chen, X. The Dose-Response Associations of Sedentary Time with Chronic Diseases and the Risk for All-Cause Mortality Affected by Different Health Status: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2020, 24, 63–70. [Google Scholar] [CrossRef]
- Buckley, J.P.; Hedge, A.; Yates, T.; Copeland, R.J.; Loosemore, M.; Hamer, M.; Bradley, G.; Dunstan, D.W. The Sedentary Office: An Expert Statement on the Growing Case for Change towards Better Health and Productivity. Br. J. Sport. Med. 2015, 49, 1357–1362. [Google Scholar] [CrossRef]
- Shrestha, N.; Kukkonen-Harjula, K.T.; Verbeek, J.H.; Ijaz, S.; Hermans, V.; Pedisic, Z. Workplace Interventions for Reducing Sitting at Work. Cochrane Database Syst. Rev. 2018, 6, CD010912. [Google Scholar]
- Coenen, P.; Parry, S.; Willenberg, L.; Shi, J.W.; Romero, L.; Blackwood, D.M.; Healy, G.N.; Dunstan, D.W.; Straker, L.M. Associations of Prolonged Standing with Musculoskeletal Symptoms-A Systematic Review of Laboratory Studies. Gait Posture 2017, 58, 310–318. [Google Scholar] [CrossRef]
- Coenen, P.; Willenberg, L.; Parry, S.; Shi, J.W.; Romero, L.; Blackwood, D.M.; Maher, C.G.; Healy, G.N.; Dunstan, D.W.; Straker, L.M. Associations of Occupational Standing with Musculoskeletal Symptoms: A Systematic Review with Meta-Analysis. Br. J. Sports Med. 2018, 52, 174–181. [Google Scholar] [CrossRef]
- Takala, E.-P. Lack of “Statistically Significant” Association Does Not Exclude Causality. Spine J. 2010, 10, 944. [Google Scholar] [CrossRef]
- Marshall, P.W.M.; Patel, H.; Callaghan, J.P. Gluteus Medius Strength, Endurance, and Co-Activation in the Development of Low Back Pain during Prolonged Standing. Hum. Mov. Sci. 2011, 30, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Viggiani, D.; Callaghan, J.P. Hip Abductor Fatigability and Recovery Are Related to the Development of Low Back Pain During Prolonged Standing. J. Appl. Biomech. 2018, 34, 39–46. [Google Scholar] [CrossRef]
- Rodríguez-Romero, B.; Smith, M.D.; Quintela-Del-Rio, A.; Johnston, V. What Psychosocial and Physical Characteristics Differentiate Office Workers Who Develop Standing-Induced Low Back Pain? A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 7104. [Google Scholar] [CrossRef] [PubMed]
- Nelson-Wong, E.; Callaghan, J.P. Is Muscle Co-Activation a Predisposing Factor for Low Back Pain Development during Standing? A Multifactorial Approach for Early Identification of at-Risk Individuals. J. Electromyogr. Kinesiol. 2010, 20, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, C.J.; Johnson, M.B.; Norton, B.J.; Callaghan, J.P.; Van Dillen, L.R. Asymmetry of Lumbopelvic Movement Patterns during Active Hip Abduction Is a Risk Factor for Low Back Pain Development during Standing. Hum. Mov. Sci. 2016, 50, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Nelson Wong, E.; Flynn, T.; Callaghan, J.P. Development of Active Hip Abduction Screening Test for Identifying Occupational Low Back Pain. J. Orthop. Sports Phys. Ther. 2009, 39, 649–657. [Google Scholar] [CrossRef]
- Nelson-Wong, E.; Gregory, D.E.; Winter, D.A.; Callaghan, J.P. Gluteus Medius Muscle Activation Patterns as a Predictor of Low Back Pain during Standing. Clin. Biomech. 2008, 23, 545–553. [Google Scholar] [CrossRef]
- Antle, D.M.; Côté, J.N. Relationships between Lower Limb and Trunk Discomfort and Vascular, Muscular and Kinetic Outcomes during Stationary Standing Work. Gait Posture 2013, 37, 615–619. [Google Scholar] [CrossRef]
- Andersen, J.H.; Haahr, J.P.; Frost, P. Risk Factors for More Severe Regional Musculoskeletal Symptoms: A Two-Year Prospective Study of a General Working Population. Arthritis Rheum. 2007, 56, 1355–1364. [Google Scholar] [CrossRef]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic Questionnaires for the Analysis of Musculoskeletal Symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Von Korff, M.; Jensen, M.P.; Karoly, P. Assessing Global Pain Severity by Self-Report in Clinical and Health Services Research. Spine 2000, 25, 3140–3151. [Google Scholar] [CrossRef] [PubMed]
- Silsbury, Z.; Goldsmith, R.; Rushton, A. Systematic Review of the Measurement Properties of Self-Report Physical Activity Questionnaires in Healthy Adult Populations. BMJ Open 2015, 5, e008430. [Google Scholar] [CrossRef] [PubMed]
- Jancey, J.; Tye, M.; McGann, S.; Blackford, K.; Lee, A.H. Application of the Occupational Sitting and Physical Activity Questionnaire (OSPAQ) to Office Based Workers. BMC Public Health 2014, 14, 762. [Google Scholar] [CrossRef] [PubMed]
- Karasek, R.; Brisson, C.; Kawakami, N.; Houtman, I.; Bongers, P.; Amick, B. The Job Content Questionnaire (JCQ): An Instrument for Internationally Comparative Assessments of Psychosocial Job Characteristics. J. Occup Health Psychol. 1998, 3, 322–355. [Google Scholar] [CrossRef]
- Sullivan, M.J.; Bishop, S.R.; Pivik, J. The Pain Catastrophizing Scale: Development and Validation. Psychol. Assess. 1995, 74, 524–532. [Google Scholar] [CrossRef]
- Gandek, B.; Ware, J.E.; Aaronson, N.K.; Apolone, G.; Bjorner, J.B.; Brazier, J.E.; Bullinger, M.; Kaasa, S.; Leplege, A.; Prieto, L.; et al. Cross-Validation of Item Selection and Scoring for the SF-12 Health Survey in Nine Countries: Results from the IQOLA Project. International Quality of Life Assessment. J. Clin. Epidemiol. 1998, 51, 1171–1178. [Google Scholar] [CrossRef]
- Davis, A.M.; Bridge, P.; Miller, J.; Nelson-Wong, E. Interrater and Intrarater Reliability of the Active Hip Abduction Test. J. Orthop. Sport. Phys. Ther. 2011, 41, 953–960. [Google Scholar] [CrossRef]
- Mens, J.M.; Vleeming, A.; Snijders, C.J.; Koes, B.W.; Stam, H.J. Reliability and Validity of the Active Straight Leg Raise Test in Posterior Pelvic Pain since Pregnancy. Spine 2001, 26, 1167–1171. [Google Scholar] [CrossRef]
- McGill, S.M.; Childs, A.; Liebenson, C. Endurance Times for Low Back Stabilization Exercises: Clinical Targets for Testing and Training from a Normal Database. Arch. Phys. Med. Rehabil. 1999, 80, 941–944. [Google Scholar] [CrossRef]
- Schellenberg, K.L.; Lang, J.M.; Chan, K.M.; Burnham, R.S. A Clinical Tool for Office Assessment of Lumbar Spine Stabilization Endurance: Prone and Supine Bridge Maneuvers. Am. J. Phys. Med. Rehabil. 2007, 86, 380–386. [Google Scholar] [CrossRef]
- Van Cant, J.; Dumont, G.; Pitance, L.; Demoulin, C.; Feipel, V. Test-Retest Reliability of Two Clinical Tests for the Assessment of Hip Abductor Endurance in Healthy Females. Int. J. Sports Phys. Ther. 2016, 11, 24–33. [Google Scholar]
- Sorensen, C.J.; Johnson, M.B.; Callaghan, J.P.; George, S.Z.; Van Dillen, L.R. Validity of a Paradigm for Low Back Pain Symptom Development During Prolonged Standing. Clin. J. Pain 2015, 31, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.; Prescott, R. Applied Mixed Models in Medicine.; John Wiley & Sons: New York, NY, USA, 1999. [Google Scholar]
- Gregory, D.E.; Callaghan, J.P. Prolonged Standing as a Precursor for the Development of Low Back Discomfort: An Investigation of Possible Mechanisms. Gait Posture 2008, 28, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.D.; Vicentino, B.; Brown, W.; Gilson, N.; Gane, E.M.; Johnston, V. Characteristics of Symptoms Experienced by Individuals during a Prolonged Standing Task: An Office-Based Study. Brazilian J. Phys. Ther. 2022; in press. [Google Scholar]
- Ostelo, R.W.; Deyo, R.A.; Stratford, P.; Waddell, G.; Croft, P.; Von Korff, M.; Bouter, L.M.; de Vet, H.C. Interpreting Change Scores for Pain and Functional Status in Low Back Pain: Towards International Consensus Regarding Minimal Important Change. Spine 2008, 33, 90–94. [Google Scholar] [CrossRef]
- Saarinen, A.J.; Uimonen, M.M.; Sandelin, H.; Toom, A.; Richter, M.; Repo, J.P. Minimal Important Change for the Visual Analogue Scale Foot and Ankle (VAS-FA). Foot Ankle Surg. Off. J. Eur. Soc. Foot Ankle Surg. 2021, 27, 196–200. [Google Scholar] [CrossRef]
- Hwang, U.-J.; Kwon, O.-Y.; Jung, S.-H.; Ahn, S.-H.; Kim, H.-A. Predictors of Pain Intensity and Oswestry Disability Index in Prolonged Standing Service Workers with Nonspecific Chronic Low Back Pain Subclassified as Active Extension Pattern. Musculoskelet. Sci. Pract. 2019, 40, 58–64. [Google Scholar] [CrossRef]
- Øverås, C.K.; Johansson, M.S.; de Campos, T.F.; Ferreira, M.L.; Natvig, B.; Mork, P.J.; Hartvigsen, J. Distribution and Prevalence of Musculoskeletal Pain Co-Occurring with Persistent Low Back Pain: A Systematic Review. BMC Musculoskelet. Disord. 2021, 22, 91. [Google Scholar] [CrossRef]
- Taylor, J.B.; Goode, A.P.; George, S.Z.; Cook, C.E. Incidence and Risk Factors for First-Time Incident Low Back Pain: A Systematic Review and Meta-Analysis. Spine J. 2014, 14, 2299–2319. [Google Scholar] [CrossRef]
- Butterworth, P.A.; Landorf, K.B.; Smith, S.E.; Menz, H.B. The Association between Body Mass Index and Musculoskeletal Foot Disorders: A Systematic Review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2012, 13, 630–642. [Google Scholar] [CrossRef]
- Sullivan, J.; Pappas, E.; Burns, J. Role of Mechanical Factors in the Clinical Presentation of Plantar Heel Pain: Implications for Management. Foot 2020, 42, 101636. [Google Scholar] [CrossRef] [PubMed]
- Neumann, D.A. Kinesiology of the Hip: A Focus on Muscular Actions. J. Orthop. Sports Phys. Ther. 2010, 40, 82–94. [Google Scholar] [CrossRef] [PubMed]
- McCann, R.S.; Crossett, I.D.; Terada, M.; Kosik, K.B.; Bolding, B.A.; Gribble, P.A. Hip Strength and Star Excursion Balance Test Deficits of Patients with Chronic Ankle Instability. J. Sci. Med. Sport 2017, 20, 992–996. [Google Scholar] [CrossRef]
- Khalaj, N.; Vicenzino, B.; Smith, M.D. Hip and Knee Muscle Torque and Its Relationship with Dynamic Balance in Chronic Ankle Instability, Copers and Controls. J. Sci. Med. Sport 2021, 24, 647–652. [Google Scholar] [CrossRef]
- Willson, J.D.; Dougherty, C.P.; Ireland, M.L.; Davis, I.M. Core Stability and Its Relationship to Lower Extremity Function and Injury. J. Am. Acad. Orthop. Surg. 2005, 13, 316–325. [Google Scholar] [CrossRef] [PubMed]
- De Blaiser, C.; De Ridder, R.; Willems, T.; Vanden Bossche, L.; Danneels, L.; Roosen, P. Impaired Core Stability as a Risk Factor for the Development of Lower Extremity Overuse Injuries: A Prospective Cohort Study. Am. J. Sports Med. 2019, 47, 1713–1721. [Google Scholar] [CrossRef]
- Goulet, J.L.; Buta, E.; Bathulapalli, H.; Gueorguieva, R.; Brandt, C.A. Statistical Models for the Analysis of Zero-Inflated Pain Intensity Numeric Rating Scale Data. J. Pain 2017, 18, 340–348. [Google Scholar] [CrossRef]
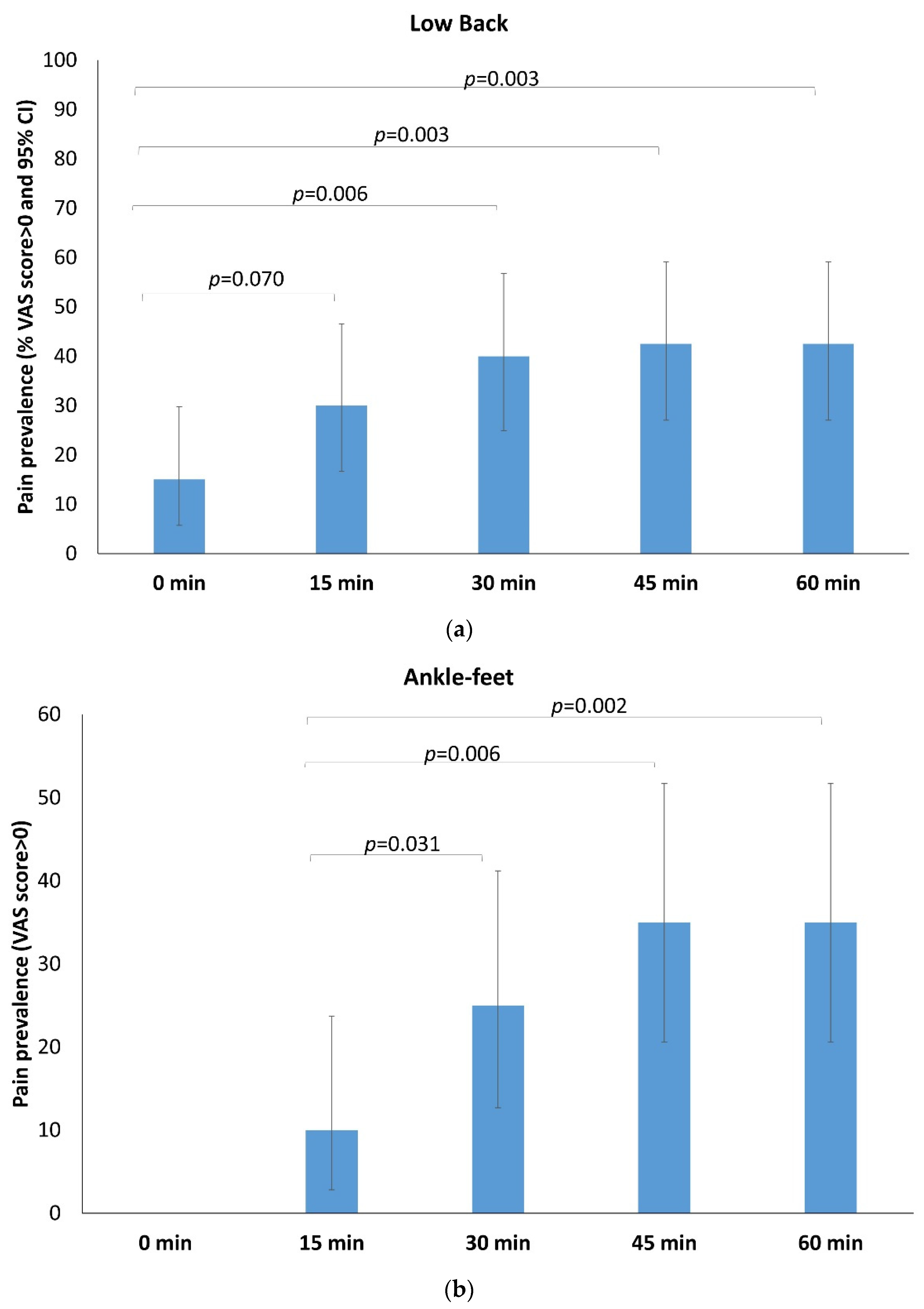
| Low Back | ||||||||||
| Pain | 0 min | 15 min | 30 min | 45 min | 60 min | |||||
| n | % | n | % | n | % | n | % | n | % | |
| No | 34 | 85.0 | 28 | 70.0 | 24 | 60.0 | 23 | 57.5 | 23 | 57.5 |
| Yes | 6 | 15.0 | 12 | 30.0 | 16 | 40.0 | 17 | 42.5 | 17 | 42.5 |
| Total | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 |
| Hip-Thigh | ||||||||||
| Pain | 0 min | 15 min | 30 min | 45 min | 60 min | |||||
| n | % | n | % | n | n | % | n | % | ||
| No | 39 | 97.5 | 39 | 97.5 | 35 | 87.5 | 34 | 85.0 | 34 | 85.0 |
| Yes | 1 | 2.5 | 1 | 2.5 | 5 | 12.5 | 6 | 15.0 | 6 | 15.0 |
| Total | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 |
| Knee-Calf | ||||||||||
| Pain | 0 min | 15 min | 30 min | 45 min | 60 min | |||||
| n | % | n | % | n | n | % | n | % | ||
| No | 38 | 95.0 | 36 | 90.0 | 33 | 82.5 | 30 | 75.0 | 29 | 72.5 |
| Yes | 2 | 5.0 | 4 | 10.0 | 7 | 17.5 | 10 | 25.0 | 11 | 27.5 |
| Total | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 |
| Ankle-feet | ||||||||||
| Pain | 0 min | 15 min | 30 min | 45 min | 60 min | |||||
| n | % | n | % | n | % | n | % | n | % | |
| No | 40 | 100 | 36 | 90.0 | 30 | 75.0 | 26 | 65.0 | 26 | 65.0 |
| Yes | - | - | 4 | 10.0 | 10 | 25.0 | 14 | 35.0 | 14 | 35.0 |
| Total | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 | 40 | 100.0 |
| Low Back | |||||
|---|---|---|---|---|---|
| VAS Scores (0–100 mm) | VAS Scores Increase from Baseline (0–100 mm) # | ||||
| Mean ± SD | Median | Mean ± SD | Median | p * | |
| Total (n = 40) | |||||
| 0 min | 1.63 ± 4.5 | 0 | - | - | |
| 15 min | 3.57 ± 8.7 | 0 | 1.94 ± 6.4 | 0 | 0.050 |
| 30 min | 7.54 ± 13.2 | 0 | 5.90 ± 11.8 | 0 | 0.004 |
| 45 min | 10.01 ± 17.6 | 0 | 8.38 ± 16.4 | 0 | 0.002 |
| 60 min | 11.64 ± 19.0 | 0 | 9.97 ± 17.5 | 0 | 0.001 |
| PD (n = 14) | |||||
| 0 min | 2.9 ± 5.9 | 0.0 | - | - | - |
| 15 min | 8.7 ± 13.3 | 4.0 | 5.9 ± 8.1 | 3.0 | 0.050 |
| 30 min | 20.5 ± 15.5 | 19.0 | 17.6 ± 12.7 | 19.0 | 0.004 |
| 45 min | 27.0 ± 21.1 | 18.0 | 24.1 ± 19.0 | 18.0 | 0.002 |
| 60 min | 30.8 ± 20.5 | 23.5 | 27.9 ± 18.1 | 23.5 | 0.001 |
| NPD (n = 26) | |||||
| 0 min | 1.0 ± 3.5 | 0.0 | - | - | - |
| 15 min | 0.8 ± 2.1 | 0.0 | −0.2 ± 4.0 | 0.0 | 0.999 |
| 30 min | 0.6 ± 1.6 | 0.0 | −0.4 ± 3.9 | 0.0 | 0.684 |
| 45 min | 0.9 ± 2.1 | 0.0 | −0.1 ± 4.1 | 0.0 | 0.916 |
| 60 min | 0.9 ± 3.1 | 0.0 | −0.1 ± 3.6 | 0.0 | 0.715 |
| Ankle-feet | |||||
| Total (n = 40) | |||||
| 0 min | 0.0 ± 0.0 | 0 | - | - | |
| 15 min | 1.5 ± 5.4 | 0 | 1.5 ± 5.4 | 0.0 | 0.068 |
| 30 min | 3.2 ± 6.3 | 0 | 3.2 ± 6.3 | 0.0 | 0.005 |
| 45 min | 5.0 ± 7.9 | 0 | 5.0 ± 7.9 | 0.0 | 0.001 |
| 60 min | 5.8 ± 70.4 | 0 | 5.8 ± 10.4 | 0.0 | 0.001 |
| PD (n = 9) | |||||
| 0 min | 0.0 ± 0.0 | 0.0 | - | - | - |
| 15 min | 6.8 ± 10.1 | 0.0 | 6.8 ± 10.1 | 0.0 | 0.068 |
| 30 min | 11.6 ± 7.2 | 12.0 | 11.6 ± 7.2 | 12.0 | 0.012 |
| 45 min | 15.7 ± 4.6 | 17.0 | 15.7 ± 4.6 | 17.0 | 0.008 |
| 60 min | 22.6 ± 9.7 | 21.0 | 22.6 ± 9.7 | 21.0 | 0.008 |
| NPD (n = 31) | |||||
| 0 min | 0.0 ± 0.0 | 0.0 | - | - | - |
| 15 min | 0.0 ± 0.0 | 0.0 | 0.0 ± 0.0 | 0.0 | 0.999 |
| 30 min | 0.8 ± 3.3 | 0.0 | 0.8 ± 3.3 | 0.0 | 0.180 |
| 45 min | 1.8 ± 5.5 | 0.0 | 1.8 ± 5.5 | 0.0 | 0.027 |
| 60 min | 0.9 ± 2.3 | 0.0 | 0.9 ± 2.3 | 0.0 | 0.026 |
| Low Back | Ankle-Feet | |||
|---|---|---|---|---|
| Total n = 40 | Total n = 40 | |||
| Rho | p | Rho | p | |
| Age (years) | 0.162 | 0.318 | −0.008 | 0.961 |
| BMI (kg/m2) | −0.098 | 0.546 | 0.379 * | 0.016 |
| IPAQ, during de last 7 days, how much time did you usually spend sitting on a weekend day (minutes) | −0.002 | 0.988 | 0.284 | 0.076 |
| IPAQ, during de last 7 days, how much time did you usually spend sitting on a weekday (minutes) | 0.142 | 0.381 | 0.025 | 0.878 |
| IPAQ, MET min/week | 0.005 | 0.975 | 0.067 | 0.690 |
| LBP severity, last 7 days (0–100) | 0.538 * | 0.000 | −0.046 | 0.777 |
| OSPAQ, minutes sitting at work per week | −0.268 | 0.094 | 0.283 | 0.077 |
| OSPAQ, minutes standing at work per week | 0.028 | 0.862 | −0.009 | 0.956 |
| OSPAQ, minutes walking at work per week | −0.083 | 0.612 | −0.208 | 0.198 |
| JCQ, Job Control | −0.085 | 0.601 | −0.068 | 0.679 |
| JCQ, Psychological Job Demands | −0.140 | 0.390 | −0.220 | 0.172 |
| JCQ, Social Support | 0.009 | 0.957 | 0.104 | 0.523 |
| JCQ, Physical Demands | 0.158 | 0.329 | 0.010 | 0.953 |
| PCS, Rumination | 0.222 | 0.168 | −0.121 | 0.455 |
| PCS, Magnification | 0.141 | 0.386 | −0.224 | 0.164 |
| PCS, Helplessness | 0.263 | 0.101 | 0.041 | 0.801 |
| PCS-total | 0.249 | 0.122 | −0.121 | 0.458 |
| SF-12, Mental Component Summary | 0.278 | 0.083 | −0.387 * | 0.014 |
| SF-12, Physical Component Summary | −0.345 * | 0.029 | 0.168 | 0.299 |
| ASLR, total examiner-score (0–10) | 0.210 | 0.193 | 0.051 | 0.755 |
| ASLR, total participant-score (0–10) | 0.346 * | 0.029 | −0.058 | 0.724 |
| AHAbd, right side, examiner-score (0–3) | 0.038 | 0.816 | 0.025 | 0.881 |
| AHAbd, left side, examiner-score (0–3) | 0.129 | 0.426 | 0.033 | 0.839 |
| AHAbd, right side, participant-score (0–5) | 0.226 | 0.162 | 0.115 | 0.479 |
| AHAbd, left side, participant-score (0–5) | 0.325 * | 0.041 | 0.008 | 0.960 |
| Abdominal (s) | −0.269 | 0.094 | −0.156 | 0.337 |
| Side Bridge right side (s) | −0.254 | 0.114 | −0.097 | 0.550 |
| Side Bridge left side (s) | −0.246 | 0.126 | −0.069 | 0.671 |
| Supine Bridge (s) | −0.298 | 0.062 | −0.327 * | 0.040 |
| Isometric hip abduction (right leg) (s) | −0.472 * | 0.002 | −0.003 | 0.985 |
| Isometric hip abduction (left leg) (s) | −0.484 * | 0.002 | 0.045 | 0.782 |
| Sorensen (s) | −0.290 | 0.070 | −0.315 * | 0.048 |
| Lineal Regression Analysis | |||||
|---|---|---|---|---|---|
| Model | B | SE | p | 95% CI | |
| Lower | Upper | ||||
| Intercept | 74.661 | 15.375 | 0.000 | 43.507 | 105.814 |
| Isometric Hip Abduction endurance test | −0.233 | 0.081 | 0.007 | −0.397 | −0.069 |
| Physical Component Summary (SF-12) | −0.864 | 0.309 | 0.008 | −1.489 | −0.239 |
| Mixed Regression Analysis | |||||
| B | SE | p | |||
| Fixed effects | |||||
| Intercept | −8.07 | 6.31 | 0.203 | ||
| Time | 0.79 | 0.42 | 0.068 | ||
| Age | 0.076 | 0.076 | 0.322 | ||
| Time×Age | 0.009 | 0.005 | 0.078 | ||
| Isometric Hip Abduction endurance test | −0.002 | 0.025 | 0.939 | ||
| Time*Isometric Hip Abduction endurance test | −0.004 | 0.002 | 0.022 | ||
| Physical Component Summary (SF-12) | 0.132 | 0.098 | 0.177 | ||
| Time*Physical Component Summary (SF-12) | −0.012 | 0.006 | 0.062 | ||
| Estimate | SE | ||||
| Random effects | |||||
| Linear slope (time) | 0.073 | 0.270 | |||
| Residual | 32.30 | 5.68 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Romero, B.; Smith, M.D.; Pértega-Díaz, S.; Quintela-del-Rio, A.; Johnston, V. Thirty Minutes Identified as the Threshold for Development of Pain in Low Back and Feet Regions, and Predictors of Intensity of Pain during 1-h Laboratory-Based Standing in Office Workers. Int. J. Environ. Res. Public Health 2022, 19, 2221. https://doi.org/10.3390/ijerph19042221
Rodríguez-Romero B, Smith MD, Pértega-Díaz S, Quintela-del-Rio A, Johnston V. Thirty Minutes Identified as the Threshold for Development of Pain in Low Back and Feet Regions, and Predictors of Intensity of Pain during 1-h Laboratory-Based Standing in Office Workers. International Journal of Environmental Research and Public Health. 2022; 19(4):2221. https://doi.org/10.3390/ijerph19042221
Chicago/Turabian StyleRodríguez-Romero, Beatriz, Michelle D. Smith, Sonia Pértega-Díaz, Alejandro Quintela-del-Rio, and Venerina Johnston. 2022. "Thirty Minutes Identified as the Threshold for Development of Pain in Low Back and Feet Regions, and Predictors of Intensity of Pain during 1-h Laboratory-Based Standing in Office Workers" International Journal of Environmental Research and Public Health 19, no. 4: 2221. https://doi.org/10.3390/ijerph19042221
APA StyleRodríguez-Romero, B., Smith, M. D., Pértega-Díaz, S., Quintela-del-Rio, A., & Johnston, V. (2022). Thirty Minutes Identified as the Threshold for Development of Pain in Low Back and Feet Regions, and Predictors of Intensity of Pain during 1-h Laboratory-Based Standing in Office Workers. International Journal of Environmental Research and Public Health, 19(4), 2221. https://doi.org/10.3390/ijerph19042221







