Attributes of Organizational Health Literacy in Health Care Centers in Iran: A Qualitative Content Analysis Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Participants
2.4. Data Collection Tools and Procedures
2.5. Research Questions
- How do we involve the management of the organization in HL?
- How do employees prepare to carry out HL activities in the organization?
- How can people participate in the organization?
- What features do you think the media should have that are easy for people to read, understand and practice?
- How can we be sure that people have understood our content?
- How is HL the focus of an organization’s activities?
- How to use HL skills to meet people’s needs?
- What factors or conditions do you think facilitate access to health information and services?
- How can the organization improve the HL of people in dangerous medical and nursing conditions?
- How can HL be useful for information on health insurance and health care coverage and costs?
2.6. Data Processing and Analysis
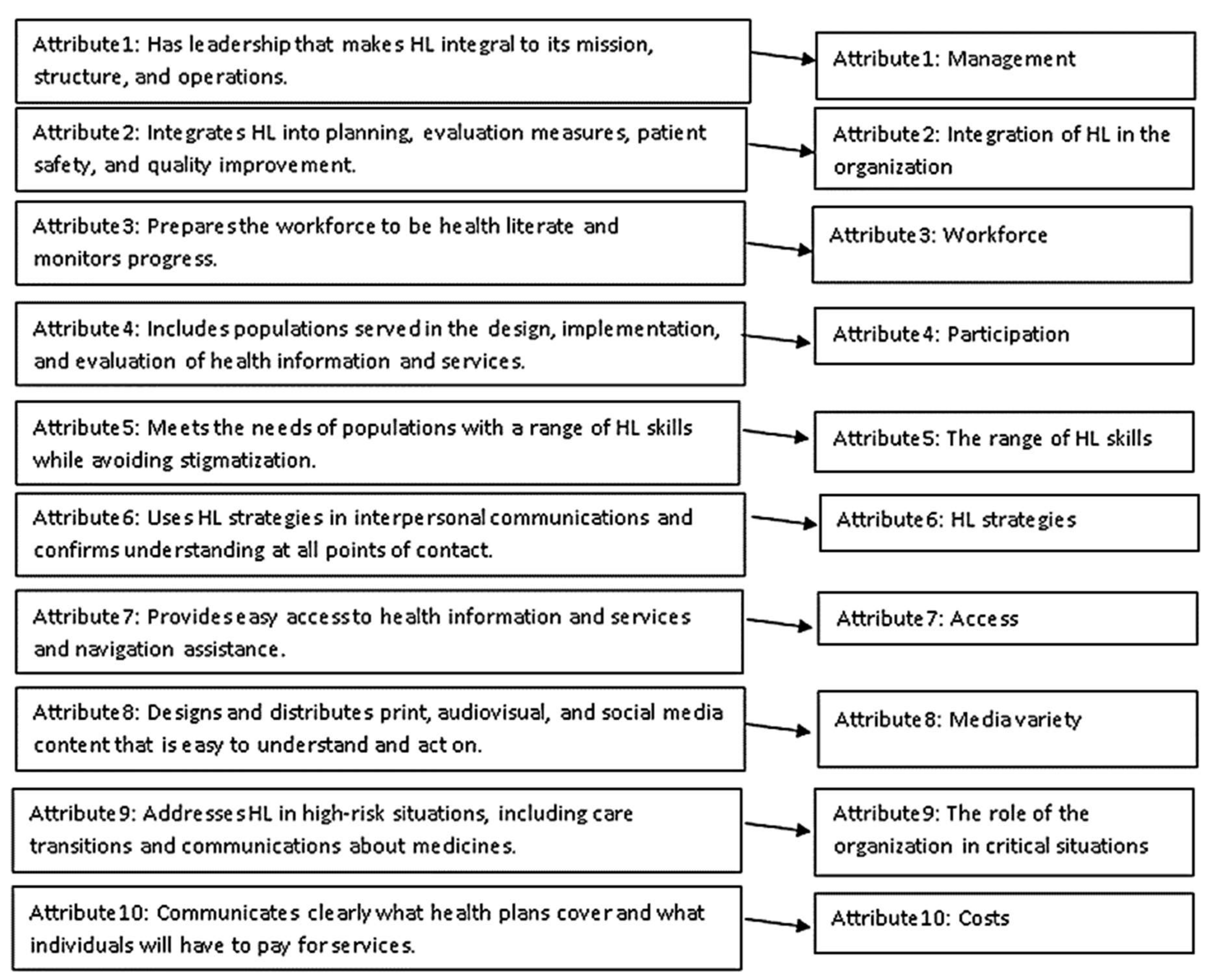
3. Results
4. Discussion
4.1. Manengment
4.2. Integration of HL in the Organization
4.3. Workforce
4.4. Participation
4.5. The Range of HL Skills
4.6. HL Strategies
4.7. Access
4.8. Media Variety
4.9. The Role of the Organization in Critical Situations
4.10. Costs
4.11. Essential Work for the Future
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OHL | Organizational Health Literacy |
| HL | Health Literacy |
References
- Simonds, S.K. Health education as social policy. Health Educ.Monogr. 1974, 2 (Suppl. S1), 1–10. [Google Scholar] [CrossRef]
- Frisch, A.; Camerini, L.; Diviani, N.; Schulz, P.J. Defining and measuring health literacy: How can we profit from other literacy domains? Health Promot. Int. 2012, 27, 117–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brach, C.; Keller, D.; Hernandez, L.M.; Baur, C.; Parker, R.; Dreyer, B.; Schyve, P.; Lemerise, A.J.; Schillinger, D.; Agency for Healthcare Research and Quality. Ten Attributes of Health Literate Health Care Organizations; NAM Perspectives: Washington, DC, USA, 2012; pp. 1–26. [Google Scholar]
- Tehrani Banihashemi, S.-A.; Haghdoost, A.A.; Amirkhani, M.A.; Alavian, S.-M.; Asgharifard, H.; Baradaran, H.; Barghamdi, M.; Parsinia, S.; Fathi Ranjbar, S. Health literacy and the influencing factors: A study in five provinces of Iran. Strides Dev. Med. Educ. 2007, 4, 1–9. [Google Scholar]
- Jafari, A.; Sany, S.B.T.; Peyman, N. The Status of Health Literacy in Students Aged 6 to 18 Old Years: A Systematic Review Study. Iran. J. Public Health 2021, 50, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Mahdifar, M.; Sany, S.B.T.; Ghavami, V.; Vahedian-Shahroodi, M. Health Literacy and Body Image Concern Among Healthcare Employees in Binaloud, Iran. J. Health Lit. 2021, 6, 31–40. [Google Scholar] [CrossRef]
- Tavakoly Sany, S.B.; Doosti, H.; Mahdizadeh, M.; Orooji, A.; Peyman, N. The Health Literacy Status and Its Role in Interventions in Iran: A Systematic and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4260. [Google Scholar] [CrossRef] [PubMed]
- Sany, S.B.T.; Behzhad, F.; Ferns, G.; Peyman, N. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: A randomized controlled trial. BMC Health Serv. Res. 2020, 20, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Charoghchian Khorasani, E.; Peyman, N.; Tehrani, H. Model Design of Health Literacy Organization in Health Care Centers in Iran Mashhad, in Mashhad University of Medical Sciences; Mashhad University of Medical Sciences: Mashhad, Iran, 2021. [Google Scholar]
- Peyman, N.; Rezai-Rad, M.; Tehrani, H.; Gholian-Aval, M.; Vahedian-Shahroodi, M.; Miri, H.H. Digital Media-based Health Intervention on the promotion of Women’s physical activity: A quasi-experimental study. BMC Public Health 2018, 18, 1–7. [Google Scholar] [CrossRef]
- Dadipoor, S.; Ramezankhani, A.; Aghamolaei, T.; Rakhshani, F.; Safari-Moradabadi, A. Evaluation of Health Literacy in the Iranian Population. Health Scope 2018, 7, 62212. [Google Scholar] [CrossRef] [Green Version]
- Khorasani, E.C.; Sany, S.B.T.; Orooji, A.; Ferns, G.; Peyman, N. Health Literacy in Iranian Women: A Systematic Review and Meta-Analysis. Iran. J. Public Health 2020, 49, 860. [Google Scholar] [CrossRef]
- Farmanova, E. Organization of Health Services for Minority Populations: The Role of Organizational Health Literacy and an Active Offer of Health Services in French in Ontario. Ph.D. Thesis, Université d’Ottawa/University of Ottawa, ON, Canada, 2017. [Google Scholar]
- Palumbo, R.; Annarumma, C. The importance of being health literate: An organizational health literacy approach. In Proceedings of the EISIC-Ex Toulon-Verona Conference, Liverpool, UK, 28–29 August 2014; pp. 247–262. [Google Scholar]
- Charoghchian Khorasani, E.; Tavakoly Sany, S.B.; Tehrani, H.; Doosti, H.; Peyman, N. Review of Organizational Health Literacy Practice at Health Care Centers: Outcomes, Barriers and Facilitators. Int. J. Environ. Res. Public Health 2020, 17, 7544. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.W. The meaning and the measure of health literacy. J. Gen. Intern. Med. 2006, 21, 878–883. [Google Scholar] [CrossRef] [Green Version]
- Eslami, V.; Tavakkoli-Sani, S.; Ghavami, V.; Peyman, N. The Relationship of Health literacy with Preventive Behaviors of Urinary Tract Infection in Pregnant Women. J. Health Lit. 2021, 2, 65–69. [Google Scholar] [CrossRef]
- Graneheim, U.H.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today 2004, 24, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Nancy Borkowski, D.B.A.; Meese, K.A. Organizational Behavior in Health Care, 2nd ed.; Jones and Bartlett Publishers: Sudbury, ON, Canada, 2011. [Google Scholar]
- Palumbo, R.; Annarumma, C.; Manna, R.; Musella, M.; Adinolfi, P. Improving quality by involving patient. The role of health literacy in influencing patients’ behaviors. Int. J. Healthc. Manag. 2019, 14, 144–152. [Google Scholar]
- Kaper, M.; Sixsmith, J.; Meijering, L.; Vervoordeldonk, J.; Doyle, P.; Barry, M.M.; De Winter, A.F.; Reijneveld, S.A. Implementation and Long-Term Outcomes of Organisational Health Literacy Interventions in Ireland and The Netherlands: A Longitudinal Mixed-Methods Study. Int. J. Environ. Res. Public Health 2019, 16, 4812. [Google Scholar] [CrossRef] [Green Version]
- Abrams, M.A.; Kurtz-Rossi, S.; Riffenburgh, A.; Savage, B.A. Building health literate organizations: A guidebook to achieving organizational change. J. Res. Pract. Adult Lit. Second. Basic Educ. 2015, 4, 1–74. [Google Scholar]
- Prince, L. Assessing Organizational Health Literacy at an Academic Health Center: A Quantitative Research Study; University of Arkansas: Arkansas, AR, USA, 2017. [Google Scholar]
- Cormier, C.M.; Kotrlik, J.W. Health literacy knowledge and experiences of senior baccalaureate nursing students. J. Nurs. Educ. 2009, 48, 237–248. [Google Scholar]
- McCleary-Jones, V. A Systematic Review of the Literature on Health Literacy in Nursing Education. Nurse Educ. 2016, 41, 93–97. [Google Scholar] [CrossRef]
- Brega, A.; Barnard, J.; Mabachi, N.; Weiss, B.; DeWalt, D.; Brach, C.; West, D. AHRQ Health Literacy Universal Precautions Toolkit, 2nd ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2015; Volume 20, pp. 12–67. [Google Scholar]
- Adams, R.J. Improving health outcomes with better patient understanding and education. Risk Manag. Health Policy 2010, 3, 61–72. [Google Scholar] [CrossRef] [Green Version]
- Palumbo, R. Leveraging Organizational Health Literacy to Enhance Health Promotion and Risk Prevention: A Narrative and Interpretive Literature Review. Yale J. Biol. Med. 2021, 94, 115–128. [Google Scholar] [PubMed]
- Wynia, M.K.; Osborn, C.Y. Health Literacy and Communication Quality in Health Care Organizations. J. Health Commun. 2010, 15, 102–115. [Google Scholar] [CrossRef] [Green Version]
- Andrulis, D.P.; Brach, C. Integrating Literacy, Culture, and Language to Improve Health Care Quality for Diverse Populations. Am. J. Health Behav. 2007, 31, 122–133. [Google Scholar] [CrossRef] [Green Version]
- Coleman, C.A.; Appy, S. Health literacy teaching in US medical schools, 2010. Fam. Med. 2012, 44, 504–507. [Google Scholar] [PubMed]
- Kaphingst, K.A.; Weaver, N.L.; Wray, R.J.; Brown, M.L.R.; Buskirk, T.; Kreuter, M.W. Effects of patient health literacy, patient engagement and a system-level health literacy attribute on patient-reported outcomes: A representative statewide survey. BMC Health Serv. Res. 2014, 14, 475. [Google Scholar] [CrossRef] [Green Version]
- Hibbard, J.H.; Greene, J.; Overton, V. Patients with lower activation associated with higher costs: Delivery systems should know their patients’ scores. Health Aff. 2013, 32, 216–222. [Google Scholar] [CrossRef]
- Koh, H.K.; Brach, C.; Harris, L.M.; Parchman, M.L. A proposed “health literate care model’ would constitute a systems approach to improving patients” engagement in care. Health Aff. 2013, 32, 357–367. [Google Scholar] [CrossRef] [Green Version]
- Paasche-Orlow, M.; Wolf, M.S. Evidence does not support clinical screening of literacy. J. Gen. Intern. Med. 2007, 23, 100–102. [Google Scholar] [CrossRef] [Green Version]
- Behzad, F.; Taghipour, A.H.E. Promoting Level of Health Literacy & Self Efficacy of Chronic Patients Referred to Health Centers through Educating Health Literacy for the Staffs of Health Centers in Mashhad Mashhad University of Medical Sciences, Mashhad. 2013, 5, 11–45. [Google Scholar]
- Imani, J.H. Ashnaie ba ravesh Delphi va karborde an dar tasmimgiri. Faslnameh Modiriat Shahri 2000, 1, 9–35. [Google Scholar]
- Julie, M.; Cooper, B.S. Health Literacy in Practice Program, Evaluation Report. Western Michigan University; School of Social Work: Michigan, MI, USA, 2011; pp. 1–156. [Google Scholar]
- McCarthy, D.M.; Waite, K.R.; Curtis, L.M.; Engel, K.G.; Baker, D.W.; Wolf, M.S. What Did the Doctor Say? Health Literacy and Recall of Medical Instructions. Med. Care 2012, 50, 277–282. [Google Scholar] [CrossRef] [Green Version]
- Center for Health Literacy. Little Rock, A.R. Academic Health Center. 2014, pp. 11–23. Available online: http://healthliteracy.ahc.edu (accessed on 1 June 2017).
- Pignone, M.; DeWalt, D.A.; Sheridan, S.; Berkman, N.; Lohr, K.N. Interventions to improve health outcomes for patients with low literacy. J. Gen. Intern. Med. 2005, 20, 185–192. [Google Scholar] [CrossRef] [Green Version]
- Otal, D.; Wizowski, L.; Pemberton, J.; Nagel, K.; Fitzgerald, P.; Walton, J.M. Parent health literacy and satisfaction with plain language education materials in a pediatric surgery outpatient clinic: A pilot study. J. Pediatr. Surg. 2012, 47, 964–969. [Google Scholar] [CrossRef] [PubMed]
- Cloonan, P.; Wood, J.; Riley, J.B. Reducing 30-Day Readmissions. JONA: J. Nurs. Adm. 2013, 43, 382–387. [Google Scholar] [CrossRef]
- Frosch, D.L.; Elwyn, G. Don’t Blame Patients, Engage Them: Transforming Health Systems to Address Health Literacy. J. Health Commun. 2014, 19, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.; Orr, M.; Warren, J. Health literacy and patient portals. J. Prim. Health Care 2015, 7, 172–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeWalt, D.A.; Broucksou, K.A.; Hawk, V.; Brach, C.; Hink, A.; Rudd, R.; Callahan, L. Developing and testing the health literacy universal precautions toolkit. Nurs. Outlook 2011, 59, 85–94. [Google Scholar] [CrossRef] [Green Version]
- Weiss, B.D. Reading level: Not the only determinant of readability. Fam.Med. 2014, 46, 563. [Google Scholar]
- Parnell, T.A.; McCulloch, E.C.; Mieres, J.H.; Edwards, F. North Shore Long Island Jewish Health System Health Literacy as an Essential Component to Achieving Excellent Patient Outcomes. NAM Perspect. 2014, 4, 41–49. [Google Scholar] [CrossRef]
- Ryan, L.; Logsdon, M.C.; McGill, S.; Stikes, R.; Senior, B.; Helinger, B.; Small, B.; Davis, D.W. Evaluation of Printed Health Education Materials for Use by Low-Education Families. J. Nurs. Sch. 2014, 46, 218–228. [Google Scholar] [CrossRef]
- Mayer, G.; Villaire, M. Enhancing written communication to address health literacy. Online J. Issues Nurs. 2009, 14, 3. [Google Scholar] [CrossRef]
- Somers, S.A.; Mahadevan, R. Health Literacy Implications of the Affordable Care Act; Center for Health Care Strategies: Washington, DC, USA, 2010; Volume 4, pp. 112–129. Available online: https://www.chcs.org/media/Health_Literacy_Implications_of_the_Affordable_Care_Act.pdf (accessed on 1 December 2021).
- Siuki, H.A.; Peyman, N.; Vahedian-Shahroodi, M.; Gholian-Aval, M.; Tehrani, H. Health Education Intervention on HIV/AIDS Prevention Behaviors among Health Volunteers in Healthcare Centers: An Applying the Theory of Planned Behavior. J. Soc. Serv. Res. 2019, 45, 582–588. [Google Scholar] [CrossRef]
- Parker, R. What an Informed Patient Means for the Future of Healthcare. PharmacoEconomics 2006, 24, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Villaire, M.; Mayer, G. Health literacy: The low-hanging fruit in health care reform. J. Health Care Financ. 2009, 36, 55–59. [Google Scholar]
- Ginsburg, J. Controlling Health Care Costs while Promoting the Best Possible Health Outcomes; American College of Physicians: Philadelphia, PA, USA, 2009; Volume 4, pp. 34–39. Available online: https://www.acponline.org/system/files/documents/advocacy/current_policy_papers/assets/controlling_healthcare_costs.pdf (accessed on 1 December 2021).
- Eichler, K.; Wieser, S.; Brügger, U. The costs of limited health literacy: A systematic review. Int. J. Public Health 2009, 54, 313–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tavakoly Sany, S.B.; Peyman, N.; Behzhad, F.; Esmaily, H.; Taghipoor, A.; Ferns, G. Health providers’ communication skills training affects hypertension outcomes. Med. Teach. 2017, 40, 154–163. [Google Scholar] [CrossRef]
| Participant Characteristics (n = 26) | Number (%) | |
|---|---|---|
| Gender | Male | 13 (50) |
| Female | 13 (50) | |
| Profession | Faculty members | 13 (50) |
| physicians | 2 (7.6) | |
| Pharmacist | 1 (3.8) | |
| Midwife | 2 (7.6) | |
| Nurse | 2 (7.6) | |
| Health care providers | 5 (13.8) | |
| Security guards | 1 (3.8) | |
| Education | PhD | 15 (57.6) |
| Doctor | 1 (3.8) | |
| Master | 5 (19.2) | |
| Bachelor | 4 (15.3) | |
| Diploma | 1 (3.8) | |
| Major | Health education | 8 (30.7) |
| Health promotion | 2 (7.6) | |
| Community Health | 1 (3.8) | |
| Nursing | 2 (7.6) | |
| Midwifery | 2 (7.6) | |
| Health services management | 2 (7.6) | |
| Pediatrician | 1 (3.8) | |
| Public health | 3 (11.5) | |
| General Practitioner | 1 (3.8) | |
| PhD in Traditional Medicine | 1 (3.8) | |
| Pharmacology | 1 (3.8) | |
| Diploma of Welfare | 1 (3.8) | |
| Accounting | 1 (3.8) | |
| Work experience (years) | 3–13 | 9 (34.6) |
| 14–24 | 11 (42.3) | |
| 25–35 | 6 (23) | |
| Sub-Theme | Subcategory | Codes | Meaning Unit |
|---|---|---|---|
| Management | Manager Properties | Appreciate employees who implement HL in the organization | “The most important thing is that someone is at the top who cares about this work, understands this work, values this work, he should be valued, if the manager does not do this, the staff will not do HL.” (Participant12, PhD) |
| Encourage other organizations to use HL | “The manager of the organization should collect the results of their work and submit them to other organizations to encourage them to take action to implement HL. By carrying out such activities, we can have a healthy society.” (Participant 26, Expert) | ||
| Tasks of the manager | Appointment to supervise the implementation of HL | “It is necessary that in the centers that work in the name of OHL, there must be a person as a supervisor to ensure that HL is implemented in order to supervise the staff for the implementation of HL.” (Participant 22, MA) | |
| Handling people’s complaints | “Complaints of employees and clients to the OHL should be heard by the management of the organization and he should address the problems and complaints so that the OHL can be promoted.” (Participant 26, Expert) | ||
| Integration of HL in the organization | Integrate HL into the structure of the organization | HL in goals and statements | “First of all, the mission of an OHL must be HL. If you see this, the next steps will be taken.” (Participant 15, MA) |
| Guidelines for promoting employee HL | “In an OHL, it is necessary to have a specific structure. This structure defines a series of frameworks and standards for them, and can formulate appropriate HL plans for them, and design specific guidelines for improving employees’ HL.” (Participant 10, PhD) | ||
| Guidelines for promoting people HL | “The OHL is an organization in which HL is practiced. In an OHL, there are guidelines to promote the HL of people in the organization.” (Participant 5, PhD) | ||
| Integrate HL into the functioning of the organization | Documents on the implementation of HL | “The implementation of HL in an OHL should become a culture and be implemented, and the documents for these activities must be prepared and exist in the organization.” (Participant 21, MA) | |
| Documents for assessment of HL activities | “In the OHL, there should be a special program for assessing HL activities, so that there is no specific application, it cannot be assessed how much HL has been upgraded in the community.” (Participant 26, Expert) | ||
| Work force | Education | HL education to employees | “All the organization’s employees need to train from the lowest level to the highest level, each with their own language, with a simple language.” (Participant 7, PhD) |
| Individuals are responsible for the HL education of employees | “In view of the fact that education has been forgotten in our health center and even in our health education department, there must be a person responsible for educating employees on OHL and continuing employee training.” (Participant 21, MA) | ||
| Train communication strategies to employees | “The workforce before you hire, you need to talk about HL and related communication strategies for these.” (Participant 3, PhD) | ||
| Staff access to HL content | “Another issue is the employees’ access to HL training materials, for example, in the hospital wards have a series of summarized trainings using HL strategies that nurse study and teach her patient.” (Participant 18, Expert) | ||
| Workforce | Employment | Employing staff fluent in the clients’ common languages | “Due to the spoken language of the client, the organization must have persons who can facilitate these exchanges, so it is necessary to hire Multilingual employees.” (Participant 24, PhD). |
| Employing staff familiar with HL | “The first characteristic of an OHL is that it is the foundation of HL, which means that if I want to employ labor for my clinic, I have to select people whose ability is to promote the HL of the organization and its clients.” (Participant 5, PhD). | ||
| Existence of HL in the job description of employees | “First of all, it should be included in the job descriptions of all health literacy staff.” (Participant 9, PhD). | ||
| Participation | People’s participation | Survey of clients regarding the choice of treatment methods | “Unfortunately, the patient’s participation in the treatment is not monitored, while if the patient’s participation in the choice of treatment is attractive, the treatment responds better.” (Participant 18, Expert). |
| Planning to employ volunteers and health liaisons | “At the OHL, we must harness the potential of volunteers to assist staff in training.” (Participant 13, PhD) | ||
| Employee participation | Existence of instructions for employee participation in HL planning | “When the employees of the organization are involved in planning the activities and their implementation, the work is done better, and if the employees of the organization themselves participate in the evaluation of the works, they can do the previous two steps better, so the employees of the organization should do it. There should be clear guidelines for staff involvement in these cases.” (Participant 20, Expert) | |
| Existence of instructions for employee participation in implementing HL | |||
| Existence of instructions for employee participation in HL assessments | |||
| The range of HL skills | Essential HL skills in relation to clients | Welcoming and evaluating the needs of clients upon entering the organization | “At the beginning of the client’s entry into the organization, we should welcome the client and assess the needs and assess his level of HL and make sure that his needs are met when leaving? There should be instructions for all this.” (Participant 25, MA) |
| Ensuring that the client’s needs are met when leaving the organization | |||
| Needs assessment using HL skills | Gather essential information from clients (only once in the organization) | “Identity, demographic and routine information that is taken from clients to organizations should be taken once that is not boring for clients.” (Participant 21, MA) | |
| Identify and guide clients in need of additional assistance | “Such patients who need extra help also need more follow-up. For example, when we see that this patient is illiterate, we should pay more attention to him than educated people. Hence, these issues should be addressed in the OHL.” (Participant 25, MA) | ||
| Determining the HL status of clients | “Determining the health literacy status of clients must be done, because sometimes, what we teach may be too trivial and superficial for the client and he may not listen, and we must first monitor, to see how much his previous information and what are its flaws and misinformation? Then, we will teach people based on it.” (Participant 22, MA) | ||
| HL strategies | Observance of HL strategies by employees in the field of verbal interaction with clients | Use simple, clear and understandable language | “It is best to talk to the clients in simple language. If you need to use professional terms, please use the translation of these terms and explain to him, so that he can understand.” (Participant 21, MA) |
| Talk to clients with appropriate voice and medium speed | “The tone of the voice should be neither too loud nor too slow. It should be such that it can hear the other side of the voice well, and it should be gentle and at the same time speak in a counted way so that the other side understands what it is saying.” (Participant 25, MA) | ||
| Ensure you understand the content provided by clients by getting feedback | “We have techniques in health education that are good techniques, one of them is feedback, that is, when you explain to a person, ask, see if he understands how much he understands your content? From this simple technique, we can use it in the OHL.” (Participant 13, PhD) | ||
| Answering clients’ questions and encouraging them to ask questions | “Clients’ questions should be answered in a good manner in the OHL, and clients should be encouraged to ask questions so that they can raise their knowledge through the question and subsequently increase their HL.” (Participant 21, MA) | ||
| Allocate enough time for each interaction | “Setting the right time for each interaction allows the patient to raise and answer their problems and needs and at the same time remain to teach him, so there must be proper communication with the patient and enough time for each interaction in the OHL.” (Participant 26, Expert) | ||
| Provide training clearly by stating the main and important points | “Sometimes the trainings are so detailed and things are said that are not useful for the trainee, that is, they are not useful, so in the OHL, it should be noted that the trainings are practical and the main and important points are stated in them.” (Participant 15, MA) | ||
| Observance of HL strategies by employees in the field of support and writing with clients | Provide training according to the economic ability of clients | “For example, we do not tell people living in low-income areas to eat protein three times a day, while he may not be able to eat protein once a month. The information we provide is appropriate for their economic situation.” (Participant 14, MA) | |
| Provide written training to clients according to their characteristics | “In written training, attention must be paid to HL issues, and these trainings must be diversified in the organization so that we can provide them according to the characteristics of the audience.” (Participant 26, Expert) | ||
| Access | Access to services and buildings | Easy access to information about the organization and services provided | “That is, the OHL should be such that people are aware of its location and the type of services it provides, and that the needs of the people are met there.” (Participant 14, MA) |
| Use understandable boards and guides in the organization | “In designing boards in the OHL, more care must be taken so that people with different characteristics can easily use the boards in navigation.” (Participant 20, Expert) | ||
| Appropriate number and arrangement of chairs in the organization | “There should be enough seats for the client to use.” (Participant 21, MA) | ||
| Easy access to appointment scheduling methods and their accuracy | “OHLs should make it easy for clients to accept visit appointments, and people in the organization should not be delayed.” (Participant 24, PhD) | ||
| Access | Considering a suitable space for parking vehicles | “In an OHL, a suitable parking space should be considered so that clients will not have a hard time finding a parking place.” (Participant 21, MA) | |
| Possibility of clients’ access to valid educational resources | “An OHL is an organization that has access to health information resources, credible sources of HL, it is possible to obtain this information.” (Participant 3, PhD) | ||
| Sending the needy to help and charity centers | “In OHLs, more help should be provided to people with financial difficulties, and there should be special instructions in this regard.” (Participant 20, Expert) | ||
| Access to understandable and executable information | Design all forms and documents in simple and understandable language | “I think the forms in the OHL should be in simple language and understandable, it is much easier for the clients.” (Participant 16, Diploma) | |
| Evaluate all content distributed in the organization by getting feedback from clients | “Before they want to publish their information and media, they need to check to see if their audience understands it or not, that is, to make sure it is understandable.” (Participant 2, PhD) | ||
| Preparation of forms and documents in the common language of the clients | “It is better to prepare the forms in the common language of the clients and implement HL strategies in them, and then get feedback from them about whether the contents are understandable for them.” (Participant 21, MA) | ||
| Media variety | Media design and distribution | Preparation of educational materials using HL strategies in different formats and their distribution through several channels | “In the OHL, there should be educational media in the common languages of those who refer to the centers, and the principle of diversity should be considered in these media, especially if it is in line with HL strategies.” (Participant 15, MA) |
| Availability of various media for clients with different levels of HL | |||
| Existence of educational media in the common languages of the clients | “In the OHL, there should be educational media in the common languages of those who refer to the centers, and the principle of diversity should be considered in these media, especially if it is in line with HL strategies.” (Participant 26, Expert) | ||
| Optimal media features | Limited number of messages and use of short sentences | “Messages should be short and concise according to the needs of the people, according to the level of information of the people.” (Participant 25, MA) | |
| Clear and understandable messages | “Too simple and schematic, clear and understandable, and too fast for the other person to sit down and read a long text.” (Participant 19, General Practitioner) | ||
| Use images | “In designing media, use images that people can understand better, because images tell everything. But the explanation may not be like the image.” (Participant 4, PhD) | ||
| Media variety | Optimal media features | Economic cost-effectiveness of the media | “Another point that should be considered in the preparation of the media is that the media produced in the organization should be as economical and cost-effective as possible, but it should be borne in mind that this cost-effectiveness should not reduce the capabilities of the media or it should question the other characteristics of the desired media, but in addition to observing other points, it should also be considered economically viable.” (Participant 26, Expert) |
| Prepare based on HL strategies | “Another feature is the preparation of this medium based on HL strategies, which, especially in terms of writing, the items that are considered HL have been observed in it.” (Participant 9, PhD) | ||
| Fits the characteristics of the audience | “In media design, understand this, take into account what psychological characteristics, characteristics and differences the target group may have in terms of demographics and social needs, and the media should be appropriate to the characteristics of the audience.” (Participant 10, PhD) | ||
| Be reliable | “An OHL is an organization that can access health information resources, effective resources, and creditable resources. It means that there are credulous media in the OHL.” (Participant 3, PhD) | ||
| Create attention | “You watch TV commercials, about a junk food item like puffs, they usually use the best commercials, then for HL training, nothing attractive is used that one wants to follow the training.” (Participant 1, PhD). | ||
| Up to date | “The media in the HL organization must be up to date, we do not use modern methods at all.” (Participant 1, PhD). | ||
| The role of the organization in critical situations | Provide understandable information | Continuous and transparent information in critical situations | “The mission of an OHL in dangerous situations is to provide continuous and transparent information about dangerous situations so that it can take steps to win the trust of the audience.” (Participant 15, MA) |
| Ensure that informed consent forms are comprehensible to clients | “In the OHL, it must be ensured that the forms, especially the informed consent forms, are such that a person with low information and low HL can understand.” (Participant 23, Expert) | ||
| Supplies | Existence and use of teaching aids | “We should use teaching aids in our training, especially in cases where there are special conditions, for example, a box of pills can be used to teach when to take pills, and it is very helpful.” (Participant 21, MA) | |
| Providing facilities based on the needs of individuals | “We must provide services to those who are most in need, away from the considerations of kinship, ethnicity, ethnicity, religion, and nationality....” (Participant 6, PhD) | ||
| Provide training | Educate employees about critical situations | “In critical situations, there should be a review in each position, i.e., the health education unit of the health center shall determine retraining courses for its health education experts.” (Participant 10, PhD) | |
| Educate clients in critical situations | “For example, in critical situations such as corona, we need to teach customers how to protect themselves from viruses.” (Participant 14, MA) | ||
| Preparation and distribution of media appropriate to critical situations | “OHLs should use appropriate media in critical situations, for example, in the event of a corona epidemic, a video of a corona patient should be shown. This is much more effective than someone talking about the disease for two hours…” (Participant 4, PhD) | ||
| Costs | Information about costs | Clearly inform clients about costs before providing any service | “As people become more aware of costs and use different resources to meet their health needs, people will find better management and decision-making methods, and ultimately become more satisfied with the service.” (Participant 15, MA) |
| Providing information to clients about the amount of insurance coverage | “The amount of insurance costs should be clear to the individual, i.e., depending on the insurance that the person is covered, this information should be given to him how much he insures and how much he has to pay out of pocket.” (Participant 21, MA) | ||
| The provision of necessary funds for HL activities in the organization | Allocate specific budgets to support HL activities | “Allocating a specific budget to support HL activities in the organization is one of the ways to provide the necessary funding for HL activities.” (Participant 26, Expert) | |
| Existence of forms of attracting public aid in order to finance HL | “In the areas where we worked, before in the south of Zahedan province, the housing of the people was unsuitable, but the mosques were very, very stylish, because there was public aid for the mosques. As for the OHL, if the people’s help is attracted in a proper way, the necessary funds will be provided for HL activities.” (Participant 6, PhD). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charoghchian Khorasani, E.; Tavakoly Sany, S.B.; Mahdizadeh, M.; Doosti, H.; Tehrani, H.; Moghzi, M.; Jafari, A.; Peyman, N. Attributes of Organizational Health Literacy in Health Care Centers in Iran: A Qualitative Content Analysis Study. Int. J. Environ. Res. Public Health 2022, 19, 2310. https://doi.org/10.3390/ijerph19042310
Charoghchian Khorasani E, Tavakoly Sany SB, Mahdizadeh M, Doosti H, Tehrani H, Moghzi M, Jafari A, Peyman N. Attributes of Organizational Health Literacy in Health Care Centers in Iran: A Qualitative Content Analysis Study. International Journal of Environmental Research and Public Health. 2022; 19(4):2310. https://doi.org/10.3390/ijerph19042310
Chicago/Turabian StyleCharoghchian Khorasani, Elham, Seyedeh Belin Tavakoly Sany, Mehrsadat Mahdizadeh, Hassan Doosti, Hadi Tehrani, Mohammad Moghzi, Alireza Jafari, and Nooshin Peyman. 2022. "Attributes of Organizational Health Literacy in Health Care Centers in Iran: A Qualitative Content Analysis Study" International Journal of Environmental Research and Public Health 19, no. 4: 2310. https://doi.org/10.3390/ijerph19042310







