Extreme Heat and Pregnancy Outcomes: A Scoping Review of the Epidemiological Evidence
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
2.3. Study Selection Process
2.4. Extraction and Synthesis
3. Results
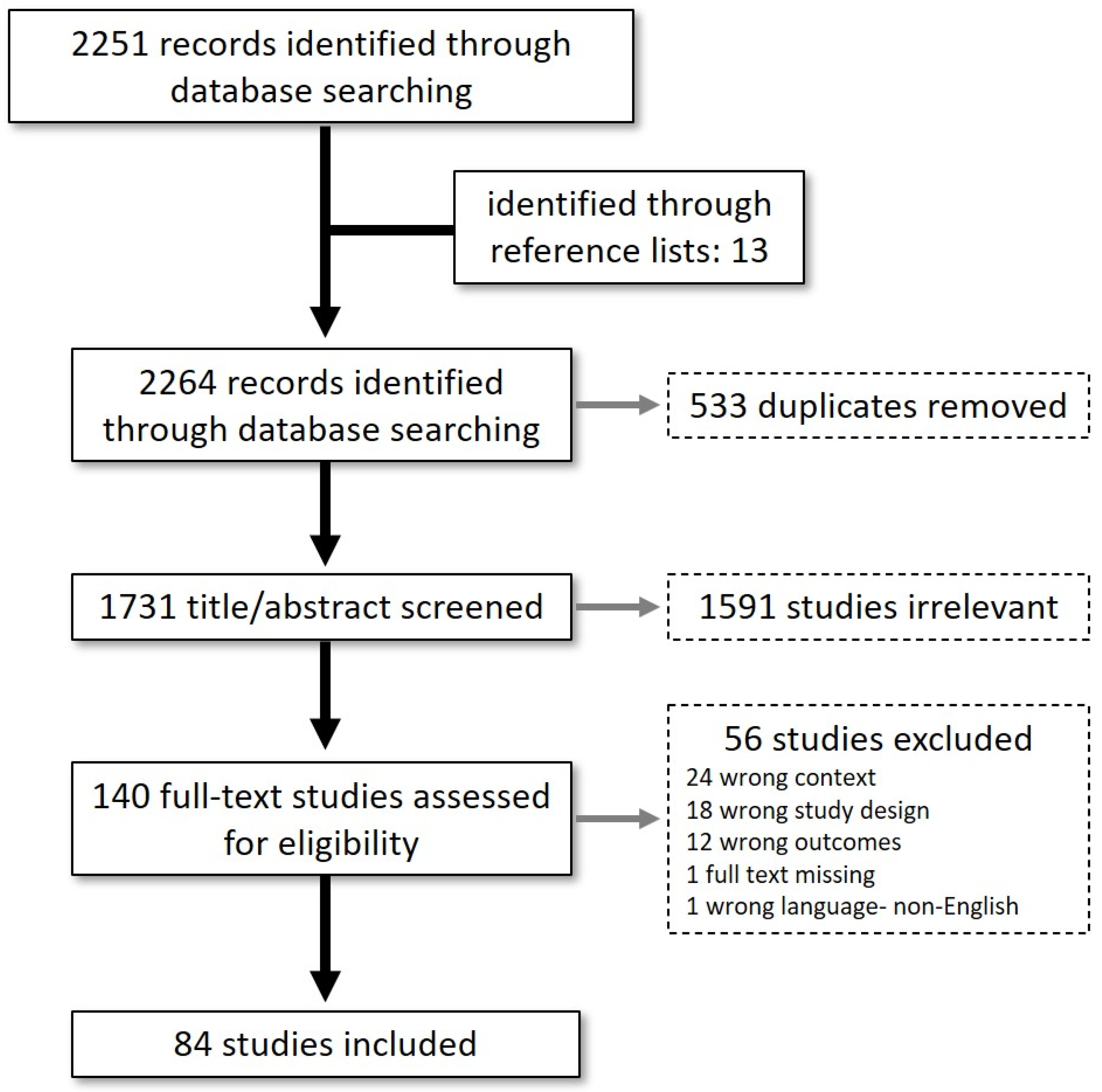
3.1. Literature Search
3.2. Study Characteristics
3.3. Preterm Birth
3.4. Birthweight
3.5. Congenital Anomaly
3.6. Stillbirth
4. Discussion
4.1. Social Gradient of Risk
4.2. Pregnancy Outcomes
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- IPCC. Summary for Policymakers. In Climate Change 2021: The Physical Science Basis; Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Masson-Delmotte, V., Zhai, P., Pirani, A., Connors, S.L., Péan, C., Berger, S., Caud, N., Chen, Y., Goldfarb, L., Gomis, M.I., et al., Eds.; Cambridge University Press: Cambridge, UK, 2021; in press. [Google Scholar]
- Turek-Hankins, L.L.; de Perez, E.C.; Scarpa, G.; Ruiz-Diaz, R.; Schwerdtle, P.N.; Joe, E.T.; Galappaththi, E.K.; French, E.M.; Austin, S.E.; Singh, C.; et al. Climate change adaptation to extreme heat: A global systematic review of implemented action. Oxf. Open Clim. Chang. 2021, 1, kgab005. [Google Scholar] [CrossRef]
- Tong, S.; FitzGerald, G.; Wang, X.Y.; Aitken, P.; Tippett, V.; Chen, D.; Wang, X.; Guo, Y. Exploration of the health risk-based definition for heatwave: A multi-city study. Environ. Res. 2015, 142, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Pascal, M.; Lagarrigue, R.; Tabai, A.; Bonmarin, I.; Camail, S.; Laaidi, K.; Le Tertre, A.; Denys, S. Evolving heat waves characteristics challenge heat warning systems and prevention plans. Int. J. Biometeorol. 2021, 65, 1683–1694. [Google Scholar] [CrossRef] [PubMed]
- Ren, C.; Williams, G.M.; Tong, S. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environ. Health Perspect. 2006, 114, 1690–1696. [Google Scholar] [CrossRef] [Green Version]
- Robine, J.M.; Cheung, S.L.; Le Roy, S.; Van Oyen, H.; Griffiths, C.; Michel, J.P.; Herrmann, F.R. Death toll exceeded 70,000 in Europe during the summer of 2003. C. R. Biol. 2008, 331, 171–178. [Google Scholar] [CrossRef]
- Rylander, C.; Odland, J.Ø.; Sandanger, T.M. Climate change and the potential effects on maternal and pregnancy outcomes: An assessment of the most vulnerable—The mother, fetus, and newborn child. Glob. Health Action 2013, 6, 19538. [Google Scholar] [CrossRef] [Green Version]
- Konkel, L. Taking the heat: Potential fetal health effects of hot temperatures. Environ. Health Perspect. 2019, 127, 102002. [Google Scholar] [CrossRef] [Green Version]
- Ravanelli, N.; Casasola, W.; English, T.; Edwards, K.M.; Jay, O. Heat stress and fetal risk. Environmental limits for exercise and passive heat stress during pregnancy: A systematic review with best evidence synthesis. Br. J. Sports Med. 2019, 53, 799–805. [Google Scholar] [CrossRef] [Green Version]
- Koman, P.D.; Hogan, K.A.; Sampson, N.; Mandell, R.; Coombe, C.M.; Tetteh, M.M.; Hill-Ashford, Y.R.; Wilkins, D.; Zlatnik, M.G.; Loch-Caruso, R.; et al. Examining joint effects of air pollution exposure and social determinants of health in defining “at-risk” populations under the clean air act: Susceptibility of pregnant women to hypertensive disorders of pregnancy. World Med. Health Pol. 2018, 10, 7–54. [Google Scholar] [CrossRef]
- Kuehn, L.; McCormick, S. Heat exposure and maternal health in the face of climate change. Int. J. Environ. Res. Public Health 2017, 14, 853. [Google Scholar] [CrossRef] [Green Version]
- Chersich, M.F.; Pham, M.D.; Areal, A.; Haghighi, M.M.; Manyuchi, A.; Swift, C.P.; Wernecke, B.; Robinson, M.; Hetem, R.; Boeckmann, M.; et al. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: Systematic review and meta-analysis. BMJ 2020, 371, m3811. [Google Scholar] [CrossRef] [PubMed]
- Carolan-Olah, M.; Frankowska, D. High environmental temperature and preterm birth: A review of the evidence. Midwifery 2014, 30, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Method 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Agay-Shay, K.; Friger, M.; Linn, S.; Peled, A.; Amitai, Y.; Peretz, C. Ambient temperature and congenital heart defects. Hum. Reprod. 2013, 28, 2289–2297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andalón, M.; Azevedo, J.P.; Rodríguez-Castelán, C.; Sanfelice, V.; Valderrama-González, D. Weather shocks and health at birth in Colombia. World Dev. 2016, 82, 69–82. [Google Scholar] [CrossRef] [Green Version]
- Arroyo, V.; Díaz, J.; Ortiz, C.; Carmona, R.; Sáez, M.; Linares, C. Short term effect of air pollution, noise and heat waves on preterm births in Madrid (Spain). Environ. Res. 2016, 145, 162–168. [Google Scholar] [CrossRef]
- Asamoah, B.; Kjellstrom, T.; Östergren, P.O. Is ambient heat exposure levels associated with miscarriage or stillbirths in hot regions? A cross-sectional study using survey data from the Ghana Maternal Health Survey 2007. Int. J. Biometeorol. 2018, 62, 319–330. [Google Scholar] [CrossRef] [Green Version]
- Asta, F.; Michelozzi, P.; Cesaroni, G.; De Sario, M.; Badaloni, C.; Davoli, M.; Schifano, P. The modifying role of socioeconomic position and greenness on the short-term effect of heat and air pollution on preterm births in Rome, 2001–2013. Int. J. Environ. Res. Public Health 2019, 16, 2497. [Google Scholar] [CrossRef] [Green Version]
- Auger, N.; Naimi, A.I.; Smargiassi, A.; Lo, E.; Kosatsky, T. Extreme heat and risk of early delivery among preterm and term pregnancies. Epidemiology 2014, 25, 344–350. [Google Scholar] [CrossRef]
- Auger, N.; Fraser, W.D.; Smargiassi, A.; Bilodeau-Bertrand, M.; Kosatsky, T. Elevated outdoor temperatures and risk of stillbirth. Int. J. Epidemiol. 2017, 46, 200–208. [Google Scholar] [CrossRef] [Green Version]
- Auger, N.; Fraser, W.D.; Sauve, R.; Bilodeau-Bertrand, M.; Kosatsky, T. Risk of congenital heart defects after ambient heat exposure early in pregnancy. Environ. Health Perspect. 2017, 125, 8–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Auger, N.; Fraser, W.D.; Arbour, L.; Bilodeau-Bertrand, M.; Kosatsky, T. Elevated ambient temperatures and risk of neural tube defects. Occup. Environ. Med. 2017, 74, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Avalos, L.A.; Chen, H.; Li, D.K.; Basu, R. The impact of high apparent temperature on spontaneous preterm delivery: A case-crossover study. Environ. Health 2017, 16, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baroutis, G.; Mousiolis, A.; Hoffman, D.; Antsaklis, A. Preterm birth seasonality in Greece: An epidemiological study. J. Matern-Fetal Neonatal Med. 2012, 25, 1406–1412. [Google Scholar] [CrossRef]
- Barreca, A.; Deschenes, O.; Guldi, M. Maybe next month? Temperature shocks and dynamic adjustments in birth rates. Demography 2018, 55, 1269–1293. [Google Scholar] [CrossRef]
- Barreca, A.; Schaller, J. The impact of high ambient temperatures on delivery timing and gestational lengths. Nat. Clim. Chang. 2020, 10, 77–82. [Google Scholar] [CrossRef]
- Basu, R.; Malig, B.; Ostro, B. High ambient temperature and the risk of preterm delivery. Am. J. Epidemiol. 2010, 172, 1108–1117. [Google Scholar] [CrossRef] [Green Version]
- Basu, R.; Pearson, D.; Sie, L.; Broadwin, R. A case-crossover study of temperature and infant mortality in California. Paediatr. Perinat. Epidemiol. 2015, 29, 407–415. [Google Scholar] [CrossRef]
- Basu, R.; Sarovar, V.; Malig, B.J. Association between high ambient temperature and risk of stillbirth in California. Am. J. Epidemiol. 2016, 183, 894–901. [Google Scholar] [CrossRef]
- Basu, R.; Chen, H.; Li, D.K.; Avalos, L.A. The impact of maternal factors on the association between temperature and preterm delivery. Environ. Res. 2017, 154, 109–114. [Google Scholar] [CrossRef] [Green Version]
- Basu, R.; Rau, R.; Pearson, D.; Malig, B. Temperature and term low birth weight in California. Am. J. Epidemiol. 2018, 187, 2306–2314. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, S.L.; Cullen, M.R.; Mayo, J.A.; Gould, J.B.; Loftus, P.; Stevenson, D.K.; Wise, P.H.; Shaw, G.M. Population-level correlates of preterm delivery among black and white women in the U.S. PLoS ONE 2014, 9, e94153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Tan, C.M.; Zhang, X.; Zhang, X. The effects of prenatal exposure to temperature extremes on birth outcomes: The case of China. J. Popul. Econ. 2020, 33, 1263–1302. [Google Scholar] [CrossRef]
- Cho, H. Ambient temperature, birth rate, and birth outcomes: Evidence from South Korea. Popul. Environ. 2020, 41, 330–346. [Google Scholar] [CrossRef] [Green Version]
- Cil, G.; Cameron, T.A. Potential climate change health risks from increases in heat waves: Abnormal birth outcomes and adverse maternal health conditions. Risk Anal. 2017, 37, 2066–2079. [Google Scholar] [CrossRef]
- Cox, B.; Vicedo-Cabrera, A.M.; Gasparrini, A.; Roels, H.A.; Martens, E.; Vangronsveld, J.; Forsberg, B.; Nawrot, T.S. Ambient temperature as a trigger of preterm delivery in a temperate climate. J. Epidemiol. Community Health 2016, 70, 1191–1199. [Google Scholar] [CrossRef] [Green Version]
- Dadvand, P.; Basagaña, X.; Sartini, C.; Figueras, F.; Vrijheid, M.; de Nazelle, A.; Sunyer, J.; Nieuwenhuijsen, M.J. Climate extremes and the length of gestation. Environ. Health Perspect. 2011, 119, 1449–1453. [Google Scholar] [CrossRef] [Green Version]
- Dadvand, P.; Ostro, B.; Figueras, F.; Foraster, M.; Basagaña, X.; Valentín, A.; Martinez, D.; Beelen, R.; Cirach, M.; Hoek, G.; et al. Residential proximity to major roads and term low birth weight: The roles of air pollution, heat, noise, and road-adjacent trees. Epidemiology 2014, 25, 518–525. [Google Scholar] [CrossRef]
- Davenport, F.; Dorélien, A.; Grace, K. Investigating the linkages between pregnancy outcomes and climate in sub-Saharan Africa. Popul. Environ. 2020, 41, 397–421. [Google Scholar] [CrossRef]
- Díaz, J.; Arroyo, V.; Ortiz, C.; Carmona, R.; Linares, C. Effect of environmental factors on low weight in non-premature births: A time series analysis. PLoS ONE 2016, 11, e0164741. [Google Scholar] [CrossRef] [Green Version]
- Gronlund, C.J.; Yang, A.J.; Conlon, K.C.; Bergmans, R.S.; Le, H.Q.; Batterman, S.A.; Wahl, R.L.; Cameron, L.; O’Neill, M.S. Time series analysis of total and direct associations between high temperatures and preterm births in Detroit, Michigan. BMJ Open 2020, 10, e032476. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Wang, Y.; Zhang, H.; Zhang, Y.; Zhao, J.; Wang, Y.; Xie, X.; Wang, L.; Zhang, Q.; Liu, D.; et al. The association between ambient temperature and the risk of preterm birth in China. Sci. Total Environ. 2018, 613–614, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.; Liu, D.; Zhu, Y.; Kim, S.S.; Sherman, S.; Mendola, P. Ambient temperature and early delivery of singleton pregnancies. Environ. Health Perspect. 2017, 125, 453–459. [Google Scholar] [CrossRef] [PubMed]
- He, J.R.; Liu, Y.; Xia, X.Y.; Ma, W.J.; Lin, H.L.; Kan, H.D.; Lu, J.H.; Feng, Q.; Mo, W.J.; Wang, P.; et al. Ambient temperature and the risk of preterm birth in Guangzhou, China (2001–2011). Environ. Health Perspect. 2016, 124, 1100–1106. [Google Scholar] [CrossRef] [Green Version]
- He, S.; Kosatsky, T.; Smargiassi, A.; Bilodeau-Bertrand, M.; Auger, N. Heat and pregnancy-related emergencies: Risk of placental abruption during hot weather. Environ. Int. 2018, 111, 295–300. [Google Scholar] [CrossRef]
- Hu, Z.; Li, T. Too hot to handle: The effects of high temperatures during pregnancy on adult welfare outcomes. J. Environ. Econ. Manag. 2019, 94, 236–253. [Google Scholar] [CrossRef]
- Ilango, S.D.; Weaver, M.; Sheridan, P.; Schwarz, L.; Clemesha, R.E.S.; Bruckner, T.; Basu, R.; Gershunov, A.; Benmarhnia, T. Extreme heat episodes and risk of preterm birth in California, 2005–2013. Environ. Int. 2020, 137, 105541. [Google Scholar] [CrossRef]
- Jakpor, O.; Chevrier, C.; Kloog, I.; Benmerad, M.; Giorgis-Allemand, L.; Cordier, S.; Seyve, E.; Vicedo-Cabrera, A.M.; Slama, R.; Heude, B.; et al. Term birthweight and critical windows of prenatal exposure to average meteorological conditions and meteorological variability. Environ. Int. 2020, 142, 105847. [Google Scholar] [CrossRef]
- Jensen, P.M.; Sørensen, M. Differences in human birth weight and corollary attributes as a result of temperature regime. Ann. Hum. Biol. 2013, 40, 385–395. [Google Scholar] [CrossRef]
- Kanner, J.; Williams, A.D.; Nobles, C.; Ha, S.; Ouidir, M.; Sherman, S.; Mendola, P. Ambient temperature and stillbirth: Risks associated with chronic extreme temperature and acute temperature change. Environ. Res. 2020, 189, 109958. [Google Scholar] [CrossRef]
- Kent, S.T.; McClure, L.A.; Zaitchik, B.F.; Smith, T.T.; Gohlke, J.M. Heat waves and health outcomes in Alabama (USA): The importance of heat wave definition. Environ. Health Perspect. 2014, 122, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Kilinc, M.F.; Cakmak, S.; Demir, D.O.; Doluoglu, O.G.; Yildiz, Y.; Horasanli, K.; Dalkilic, A. Does maternal exposure during pregnancy to higher ambient temperature increase the risk of hypospadias? J. Pediatr. Urol. 2016, 12, 407.e1–407.e6. [Google Scholar] [CrossRef] [PubMed]
- Kloog, I.; Melly, S.J.; Coull, B.A.; Nordio, F.; Schwartz, J.D. Using satellite-based spatiotemporal resolved air temperature exposure to study the association between ambient air temperature and birth outcomes in Massachusetts. Environ. Health Perspect. 2015, 123, 1053–1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwag, Y.; Kim, M.H.; Oh, J.; Shah, S.; Ye, S.; Ha, E.H. Effect of heat waves and fine particulate matter on preterm births in Korea from 2010 to 2016. Environ. Int. 2021, 147, 106239. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, J.; Xu, Z.; Wang, X.; Xu, G.; Zhang, J.; Shen, X.; Tong, S. Exploring associations of maternal exposure to ambient temperature with duration of gestation and birth weight: A prospective study. BMC Pregnancy Childbirth 2018, 18, 513. [Google Scholar] [CrossRef]
- Li, S.; Chen, G.; Jaakkola, J.J.K.; Williams, G.; Guo, Y. Temporal change in the impacts of ambient temperature on preterm birth and stillbirth: Brisbane, 1994–2013. Sci. Total Environ. 2018, 634, 579–585. [Google Scholar] [CrossRef]
- Liang, Z.; Lin, Y.; Ma, Y.; Zhang, L.; Zhang, X.; Li, L.; Zhang, S.; Cheng, Y.; Zhou, X.; Lin, H.; et al. The association between ambient temperature and preterm birth in Shenzhen, China: A distributed lag non-linear time series analysis. Environ. Health 2016, 15, 84. [Google Scholar] [CrossRef] [Green Version]
- Lin, G.; Zhang, T. Examining extreme weather effects on birth weight from the individual effect to spatiotemporal aggregation effects. J. Agric. Biol. Env. Stat. 2012, 17, 490–507. [Google Scholar] [CrossRef] [Green Version]
- Lin, S.; Lin, Z.; Ou, Y.; Soim, A.; Shrestha, S.; Lu, Y.; Sheridan, S.; Luben, T.J.; Fitzgerald, E.; Bell, E.; et al. Maternal ambient heat exposure during early pregnancy in summer and spring and congenital heart defects—A large US population-based, case-control study. Environ. Int. 2018, 118, 211–221. [Google Scholar] [CrossRef]
- Madsen, C.; Gehring, U.; Walker, S.E.; Brunekreef, B.; Stigum, H.; Naess, O.; Nafstad, P. Ambient air pollution exposure, residential mobility and term birth weight in Oslo, Norway. Environ. Res. 2010, 110, 363–371. [Google Scholar] [CrossRef]
- Martens, D.S.; Plusquin, M.; Cox, B.; Nawrot, T.S. Early biological aging and fetal exposure to high and low ambient temperature: A birth cohort study. Environ. Health Perspect. 2019, 127, 117001. [Google Scholar] [CrossRef] [PubMed]
- Mathew, S.; Mathur, D.; Chang, A.B.; McDonald, E.; Singh, G.R.; Nur, D.; Gerritsen, R. Examining the effects of ambient temperature on pre-term birth in Central Australia. Int. J. Environ. Res. Public Health 2017, 14, 147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohammadi, D.; Naghshineh, E.; Sarsangi, A.; Zare Sakhvidi, M.J. Environmental extreme temperature and daily preterm birth in Sabzevar, Iran: A time-series analysis. Environ. Health Prev. Med. 2019, 24, 5. [Google Scholar] [CrossRef] [PubMed]
- Molina, O.; Saldarriaga, V. The perils of climate change: In utero exposure to temperature variability and birth outcomes in the Andean region. Econ. Hum. Biol. 2017, 24, 111–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moreira, I.; Linares, C.; Follos, F.; Sánchez-Martínez, G.; Vellón, J.M.; Díaz, J. Short-term effects of Saharan dust intrusions and biomass combustion on birth outcomes in Spain. Sci. Total Environ. 2020, 701, 134755. [Google Scholar] [CrossRef]
- Muresan, D.; Staicu, A.; Zaharie, G.; Marginean, C.; Rotar, I.C. The influence of seasonality and weather changes on premature birth incidence. Clujul Med. 2017, 90, 273–278. [Google Scholar] [CrossRef] [Green Version]
- Ngo, N.S.; Horton, R.M. Climate change and fetal health: The impacts of exposure to extreme temperatures in New York City. Environ. Res. 2016, 144 Pt A, 158–164. [Google Scholar] [CrossRef]
- Poeran, J.; Birnie, E.; Steegers, E.A.; Bonsel, G.J. The impact of extremes in outdoor temperature and sunshine exposure on birth weight. J. Environ. Health 2016, 78, 92–100. [Google Scholar]
- Rammah, A.; Whitworth, K.W.; Han, I.; Chan, W.; Hess, J.W.; Symanski, E. Temperature, placental abruption and stillbirth. Environ. Int. 2019, 131, 105067. [Google Scholar] [CrossRef]
- Schifano, P.; Lallo, A.; Asta, F.; De Sario, M.; Davoli, M.; Michelozzi, P. Effect of ambient temperature and air pollutants on the risk of preterm birth, Rome 2001–2010. Environ. Int. 2013, 61, 77–87. [Google Scholar] [CrossRef]
- Schifano, P.; Asta, F.; Dadvand, P.; Davoli, M.; Basagana, X.; Michelozzi, P. Heat and air pollution exposure as triggers of delivery: A survival analysis of population-based pregnancy cohorts in Rome and Barcelona. Environ. Int. 2016, 88, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.L.; Hardeman, R.R. Association of summer heat waves and the probability of preterm birth in Minnesota: An exploration of the intersection of race and education. Int. J. Environ. Res. Public Health 2020, 17, 6391. [Google Scholar] [CrossRef] [PubMed]
- Soim, A.; Lin, S.; Sheridan, S.C.; Hwang, S.A.; Hsu, W.H.; Luben, T.J.; Shaw, G.M.; Feldkamp, M.L.; Romitti, P.A.; Reefhuis, J.; et al. Population-based case-control study of the association between weather-related extreme heat events and neural tube defects. Birth Defects Res. 2017, 109, 1482–1493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soim, A.; Sheridan, S.C.; Hwang, S.A.; Hsu, W.H.; Fisher, S.C.; Shaw, G.M.; Feldkamp, M.L.; Romitti, P.A.; Reefhuis, J.; Langlois, P.H.; et al. A population-based case-control study of the association between weather-related extreme heat events and orofacial clefts. Birth Defects Res. 2018, 110, 1468–1477. [Google Scholar] [CrossRef]
- Son, J.Y.; Lee, J.T.; Lane, K.J.; Bell, M.L. Impacts of high temperature on adverse birth outcomes in Seoul, Korea: Disparities by individual- and community-level characteristics. Environ. Res. 2019, 168, 460–466. [Google Scholar] [CrossRef]
- Song, J.; Lu, J.; Wang, E.; Lu, M.; An, Z.; Liu, Y.; Zeng, X.; Li, W.; Li, H.; Xu, D.; et al. Short-term effects of ambient temperature on the risk of premature rupture of membranes in Xinxiang, China: A time-series analysis. Sci. Total Environ. 2019, 689, 1329–1335. [Google Scholar] [CrossRef]
- Stingone, J.A.; Luben, T.J.; Sheridan, S.C.; Langlois, P.H.; Shaw, G.M.; Reefhuis, J.; Romitti, P.A.; Feldkamp, M.L.; Nembhard, W.N.; Browne, M.L.; et al. Associations between fine particulate matter, extreme heat events, and congenital heart defects. Environ. Epidemiol. 2019, 3, e071. [Google Scholar] [CrossRef] [Green Version]
- Strand, L.B.; Barnett, A.G.; Tong, S. Maternal exposure to ambient temperature and the risks of preterm birth and stillbirth in Brisbane, Australia. Am. J. Epidemiol. 2012, 175, 99–107. [Google Scholar] [CrossRef] [Green Version]
- Sun, S.; Weinberger, K.R.; Spangler, K.R.; Eliot, M.N.; Braun, J.M.; Wellenius, G.A. Ambient temperature and preterm birth: A retrospective study of 32 million US singleton births. Environ. Int. 2019, 126, 7–13. [Google Scholar] [CrossRef]
- Sun, Y.; Ilango, S.D.; Schwarz, L.; Wang, Q.; Chen, J.C.; Lawrence, J.M.; Wu, J.; Benmarhnia, T. Examining the joint effects of heatwaves, air pollution, and green space on the risk of preterm birth in California. Environ. Res. Lett. 2020, 15, 104099. [Google Scholar] [CrossRef]
- Van Zutphen, A.R.; Lin, S.; Fletcher, B.A.; Hwang, S.A. A population-based case-control study of extreme summer temperature and birth defects. Environ. Health Perspect. 2012, 120, 1443–1449. [Google Scholar] [CrossRef] [Green Version]
- Vicedo-Cabrera, A.M.; Iñíguez, C.; Barona, C.; Ballester, F. Exposure to elevated temperatures and risk of preterm birth in Valencia, Spain. Environ. Res. 2014, 134, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Vicedo-Cabrera, A.M.; Olsson, D.; Forsberg, B. Exposure to seasonal temperatures during the last month of gestation and the risk of preterm birth in Stockholm. Int. J. Environ. Res. Public Health 2015, 12, 3962–3978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walfisch, A.; Kabakov, E.; Friger, M.; Sheiner, E. Trends, seasonality and effect of ambient temperature on preterm delivery. J. Matern-Fetal Neonatal Med. 2017, 30, 2483–2487. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Williams, G.; Guo, Y.; Pan, X.; Tong, S. Maternal exposure to heatwave and preterm birth in Brisbane, Australia. BJOG 2013, 120, 1631–1641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Tong, S.; Williams, G.; Pan, X. Exposure to heat wave during pregnancy and adverse birth outcomes: An exploration of susceptible windows. Epidemiology 2019, 30 (Suppl. 1), S115–S121. [Google Scholar] [CrossRef]
- Wang, Q.; Li, B.; Benmarhnia, T.; Hajat, S.; Ren, M.; Liu, T.; Knibbs, L.D.; Zhang, H.; Bao, J.; Zhang, Y.; et al. Independent and combined effects of heatwaves and PM2.5 on preterm birth in Guangzhou, China: A Survival Analysis. Environ. Health Perspect. 2020, 128, 17006. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Liu, X.; Dong, M.; Sun, X.; Xiao, J.; Zeng, W.; Hu, J.; Li, X.; Guo, L.; Rong, Z.; et al. Associations of maternal ambient temperature exposures during pregnancy with the placental weight, volume and PFR: A birth cohort study in Guangzhou, China. Environ. Int. 2020, 139, 105682. [Google Scholar] [CrossRef]
- Ward, A.; Clark, J.; McLeod, J.; Woodul, R.; Moser, H.; Konrad, C. The impact of heat exposure on reduced gestational age in pregnant women in North Carolina, 2011–2015. Int. J. Biometeorol. 2019, 63, 1611–1620. [Google Scholar] [CrossRef]
- Weng, Y.H.; Yang, C.Y.; Chiu, Y.W. Adverse neonatal outcomes in relation to ambient temperatures at birth: A nationwide survey in Taiwan. Arch. Environ. Occup. Health 2018, 73, 48–55. [Google Scholar] [CrossRef]
- Wolf, J.; Armstrong, B. The association of season and temperature with adverse pregnancy outcome in two German states, a time-series analysis. PLoS ONE 2012, 7, e40228. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Song, L.; Zheng, X.; Zhang, L.; Liu, B.; Wang, L.; Li, H.; Xiong, C.; Cao, Z.; Wang, Y.; et al. Prenatal exposure of diurnal temperature range and preterm birth: Findings from a birth cohort study in China. Sci. Total Environ. 2019, 656, 1102–1107. [Google Scholar] [CrossRef] [PubMed]
- Yitshak-Sade, M.; Novack, L.; Landau, D.; Kloog, I.; Sarov, B.; Hershkovitz, R.; Karakis, I. Relationship of ambient air pollutants and hazardous household factors with birth weight among Bedouin-Arabs. Chemosphere 2016, 160, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Spero, T.L.; Nolte, C.G.; Garcia, V.C.; Lin, Z.; Romitti, P.A.; Shaw, G.M.; Sheridan, S.C.; Feldkamp, M.L.; Woomert, A.; et al. Projected changes in maternal heat exposure during early pregnancy and the associated congenital heart defect burden in the United States. J. Am. Heart Assoc. 2019, 8, e010995. [Google Scholar] [CrossRef] [Green Version]
- Zheng, X.; Zhang, W.; Lu, C.; Norbäck, D.; Deng, Q. An epidemiological assessment of the effect of ambient temperature on the incidence of preterm births: Identifying windows of susceptibility during pregnancy. J. Therm. Biol. 2018, 74, 201–207. [Google Scholar] [CrossRef]
- Zhong, Q.; Lu, C.; Zhang, W.; Zheng, X.; Deng, Q. Preterm birth and ambient temperature: Strong association during night-time and warm seasons. J. Therm. Biol. 2018, 78, 381–390. [Google Scholar] [CrossRef]
- Zhou, G.; Yang, M.; Chai, J.; Sun, R.; Zhang, J.; Huang, H.; Zhang, Y.; Deng, Q.; Jiang, L.; Ba, Y. Preconception ambient temperature and preterm birth: A time-series study in rural Henan, China. Environ. Sci. Pollut. Res. Int. 2021, 28, 9407–9416. [Google Scholar] [CrossRef]
- Hughes, M.M.; Black, R.E.; Katz, J. 2500-g low birth weight cutoff: History and implications for future research and policy. Matern. Child Health J. 2017, 21, 283–289. [Google Scholar] [CrossRef] [Green Version]
- Zare, S.; Hasheminejad, N.; Shirvan, H.E.; Hemmatjo, R.; Sarebanzadeh, K.; Ahmadi, S. Comparing Universal Thermal Climate Index (UTCI) with selected thermal indices/environmental parameters during 12 months of the year. Weather Clim. Extrem. 2018, 19, 49–57. [Google Scholar] [CrossRef]
- Lee, J.B.; Kim, J.H.; Murota, H. Perspiration functions in different ethnic, age, and sex populations: Modification of sudomotor function. Curr. Probl. Dermatol. 2016, 51, 109–119. [Google Scholar] [CrossRef]
- Harrington, L.J.; Otto, F.E.L. Reconciling theory with the reality of African heatwaves. Nat. Clim. Chang. 2020, 10, 796–798. [Google Scholar] [CrossRef]
- Keller, C.A.; Nugent, R.P. Seasonal patterns in perinatal mortality and preterm delivery. Am. J. Epidemiol. 1983, 118, 689–698. [Google Scholar] [CrossRef]
- Cheung, S.S.; McLellan, T.M.; Tenaglia, S. The thermophysiology of uncompensable heat stress. Physiological manipulations and individual characteristics. Sports Med. 2000, 29, 329–359. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, T.; Phillips, K. From SARS to pandemic influenza—The framing of high-risk populations. Nat. Hazards 2019, 98, 103–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thompson, E.; Edjoc, R.; Atchessi, N.; Striha, M.; Gabrani-Juma, I.; Dawson, T. COVID-19: A case for the collection of race data in Canada and abroad. Can. Commun. Dis. Rep. 2021, 47, 300–304. [Google Scholar] [CrossRef]
- Kaplan, J.B.; Bennett, T. Use of race and ethnicity in biomedical publication. JAMA 2003, 289, 2709–2716. [Google Scholar] [CrossRef]
- Poursafa, P.; Keikha, M.; Kelishadi, R. Systematic review on adverse birth outcomes of climate change. J. Res. Med. Sci. 2015, 20, 397–402. [Google Scholar]
- Yackerson, N.; Piura, B.; Sheiner, E. The influence of meteorological factors on the emergence of preterm delivery and preterm premature rupture of membrane. J. Perinatol. 2008, 28, 707–711. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.J.; Power, G.G. Engine and radiator: Fetal and placental interactions for heat dissipation. Exp. Physiol. 1997, 82, 403–414. [Google Scholar] [CrossRef]
- Laburn, H.P.; Faurie, A.; Goelst, K.; Mitchell, D. Effects on fetal and maternal body temperatures of exposure of pregnant ewes to heat, cold, and exercise. J. Appl. Physiol. 2002, 92, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Sharif-Naeini, R.; Ciura, S.; Bourque, C.W. TRPV1 gene required for thermosensory transduction and anticipatory secretion from vasopressin neurons during hyperthermia. Neuron 2008, 58, 179–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akerlund, M. Involvement of oxytocin and vasopressin in the pathophysiology of preterm labor and primary dysmenorrhea. Prog. Brain Res. 2002, 139, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Evers, K.S.; Wellmann, S. Arginine vasopressin and copeptin in perinatology. Front. Pediatr. 2016, 4, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fill Malfertheiner, S.; Bataiosu-Zimmer, E.; Michel, H.; Fouzas, S.; Bernasconi, L.; Bührer, C.; Wellmann, S. Vasopressin but not oxytocin responds to birth stress in infants. Front. Neurosci. 2021, 15, 718056. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.S. The epidemiology of low birthweight. Nestle Nutr. Inst. Workshop Ser. 2013, 74, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silbergeld, E.K.; Patrick, T.E. Environmental exposures, toxicologic mechanisms, and adverse pregnancy outcomes. Am. J. Obstet. Gynecol. 2005, 192 (Suppl. 5), S11–S21. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, W.; Xu, J.; Luo, Z.; Ye, X.; Yan, C.; Liu, Z.; Tong, S. Association between temperature and maternal stress during pregnancy. Environ. Res. 2017, 158, 421–430. [Google Scholar] [CrossRef]
- Kalisch-Smith, J.I.; Ved, N.; Sparrow, D.B. Environmental risk factors for congenital heart disease. Cold Spring Harb. Perspect. Biol. 2020, 12, a037234. [Google Scholar] [CrossRef] [Green Version]
- Hutson, M.R.; Keyte, A.L.; Hernández-Morales, M.; Gibbs, E.; Kupchinsky, Z.A.; Argyridis, I.; Erwin, K.N.; Pegram, K.; Kneifel, M.; Rosenberg, P.B.; et al. Temperature-activated ion channels in neural crest cells confer maternal fever-associated birth defects. Sci Signal. 2017, 10, eaal4055. [Google Scholar] [CrossRef] [Green Version]
- Wilkins-Haug, L. Genetic innovations and our understanding of stillbirth. Hum. Genet. 2020, 139, 1161–1172. [Google Scholar] [CrossRef]
- Filiano, J.J.; Kinney, H.C. A perspective on neuropathologic findings in victims of the sudden infant death syndrome: The triple-risk model. Biol. Neonate 1994, 65, 194–197. [Google Scholar] [CrossRef] [PubMed]
| Count | % | |
|---|---|---|
| Year of Publication | ||
| 2010–2015 | 20 | 24 |
| 2016–2020 | 64 | 76 |
| Study Setting 1 | ||
| Australia | 6 | 7 |
| Eastern Europe | 1 | 1 |
| Northern Europe | 2 | 2 |
| South America | 2 | 2 |
| Southern Europe | 10 | 12 |
| Western Asia | 5 | 6 |
| Western Europe | 5 | 6 |
| East Asia | 16 | 19 |
| Northern America | 34 | 40 |
| West Africa | 2 | 2 |
| Start Dates of Data Collection/Inclusion 2 | ||
| 1931–1949 | 1 | 1 |
| 1950–1974 | 3 | 4 |
| 1975–1999 | 35 | 42 |
| 2000–2020 | 46 | 55 |
| Duration of Data Collection/Inclusion 3 | ||
| less than 5 y | 22 | 26 |
| 5–9 y | 28 | 33 |
| 10–14 y | 18 | 21 |
| 15–19 y | 4 | 5 |
| 20–24 y | 6 | 7 |
| 25+ y | 7 | 8 |
| Count | % | |
|---|---|---|
| Study Design | ||
| Case-Control | 7 | 8 |
| Case-Crossover | 11 | 13 |
| Case-Series | 2 | 2 |
| Cohort | 31 | 37 |
| Cross-sectional | 3 | 4 |
| Population Registry | 16 | 19 |
| Time-series, Registry | 13 | 15 |
| Not Stated | 1 | 1 |
| Statistical Analysis 1 | ||
| Case-Crossover Analysis | 6 | 7 |
| Fixed Effect-Poisson Distribution | 16 | 19 |
| General Linear Model | 9 | 11 |
| Pearson Correlation | 2 | 2 |
| Regression Models | 34 | 40 |
| Survival Analysis-Time | 30 | 36 |
| Temperature Measurements | ||
| Hourly 2 | 7 | 8 |
| Daily | 63 | 75 |
| Monthly | 5 | 6 |
| Seasonal | 1 | 1 |
| Climate 3 | 2 | 2 |
| Heat wave | 6 | 7 |
| Exposure Period | ||
| 1st Trimester | 12 | 14 |
| 2nd + 3rd Trimester 4 | 15 | 18 |
| 3rd Trimester | 8 | 10 |
| All/Any Part of Pregnancy 5 | 35 | 42 |
| Delivery Date | 13 | 15 |
| Count | % | |
| Study Design | ||
| Case-Crossover | 5 | 11 |
| Case-Series | 1 | 2 |
| Cohort | 17 | 39 |
| Population Registry | 10 | 23 |
| Time-Series, Registry | 11 | 25 |
| Setting | ||
| Australia | 5 | 11 |
| Eastern Asia | 12 | 27 |
| Eastern Europe | 1 | 2 |
| Northern America | 14 | 32 |
| Northern Europe | 1 | 2 |
| Southern Asia | 1 | 2 |
| Southern Europe | 7 | 16 |
| Western Asia | 1 | 2 |
| Western Europe | 2 | 5 |
| Exposure Period | ||
| Conception | 1 | 2 |
| 2nd + 3rd Trimester 1 | 11 | 25 |
| 3rd Trimester | 7 | 16 |
| All/Any Part Of Pregnancy 2 | 13 | 30 |
| Delivery Date | 12 | 27 |
| Count | % | |
|---|---|---|
| Study Design | ||
| Cohort | 10 | 48 |
| Cross-sectional | 2 | 10 |
| Population Registry | 4 | 19 |
| Time-series, Registry | 4 | 19 |
| Not stated | 1 | 5 |
| Setting | ||
| Africa | 1 | 5 |
| Australia | 1 | 5 |
| Eastern Asia | 4 | 19 |
| Global | 1 | 5 |
| Northern Europe | 1 | 5 |
| Southern America | 4 | 19 |
| United States | 4 | 19 |
| Western Asia | 1 | 5 |
| Western Europe | 4 | 19 |
| Exposure Period | ||
| All/Any Part of Pregnancy 1 | 17 | 86 |
| Delivery Date | 3 | 14 |
| Count | % | |
|---|---|---|
| Study Design | ||
| Case-Control | 7 | 64 |
| Case-Crossover | 1 | 9 |
| Cohort | 3 | 27 |
| Setting | ||
| Canada | 2 | 18 |
| Israel | 1 | 9 |
| Turkey | 1 | 9 |
| United States | 7 | 64 |
| Exposure Period | ||
| 1st Trimester | 10 | 91 |
| All/Any Part of Pregnancy | 1 | 9 |
| Type of Congenital Anomaly 1 | ||
| Congenital Heart Defect | 5 | 45 |
| Hypospadias | 1 | 9 |
| Neural Tube Defect | 2 | 18 |
| Orofacial Clefts | 1 | 9 |
| Various | 2 | 18 |
| Count | % | |
|---|---|---|
| Study Design | ||
| Case-Crossover | 4 | 40 |
| Cohort | 2 | 20 |
| Cross-Sectional | 2 | 20 |
| Population Registry | 2 | 20 |
| Setting | ||
| Australia | 3 | 30 |
| Canada | 1 | 10 |
| Sub-Saharan Africa | 2 | 20 |
| Taiwan | 1 | 10 |
| United States | 3 | 30 |
| Exposure Period | ||
| 1st Trimester | 1 | 10 |
| 2nd/3rd Trimester | 2 | 20 |
| 3rd Trimester | 1 | 10 |
| Delivery Date | 1 | 10 |
| All/Any Part of Pregnancy 1 | 5 | 50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Syed, S.; O’Sullivan, T.L.; Phillips, K.P. Extreme Heat and Pregnancy Outcomes: A Scoping Review of the Epidemiological Evidence. Int. J. Environ. Res. Public Health 2022, 19, 2412. https://doi.org/10.3390/ijerph19042412
Syed S, O’Sullivan TL, Phillips KP. Extreme Heat and Pregnancy Outcomes: A Scoping Review of the Epidemiological Evidence. International Journal of Environmental Research and Public Health. 2022; 19(4):2412. https://doi.org/10.3390/ijerph19042412
Chicago/Turabian StyleSyed, Sarah, Tracey L. O’Sullivan, and Karen P. Phillips. 2022. "Extreme Heat and Pregnancy Outcomes: A Scoping Review of the Epidemiological Evidence" International Journal of Environmental Research and Public Health 19, no. 4: 2412. https://doi.org/10.3390/ijerph19042412
APA StyleSyed, S., O’Sullivan, T. L., & Phillips, K. P. (2022). Extreme Heat and Pregnancy Outcomes: A Scoping Review of the Epidemiological Evidence. International Journal of Environmental Research and Public Health, 19(4), 2412. https://doi.org/10.3390/ijerph19042412






