Relationship between Using Fibrate and Open-Angle Glaucoma in Hyperlipidemic Patients: A Population-Based Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Database
2.2. Study Participants
2.3. Ethical Considerations
2.4. Statistical Analysis
3. Results
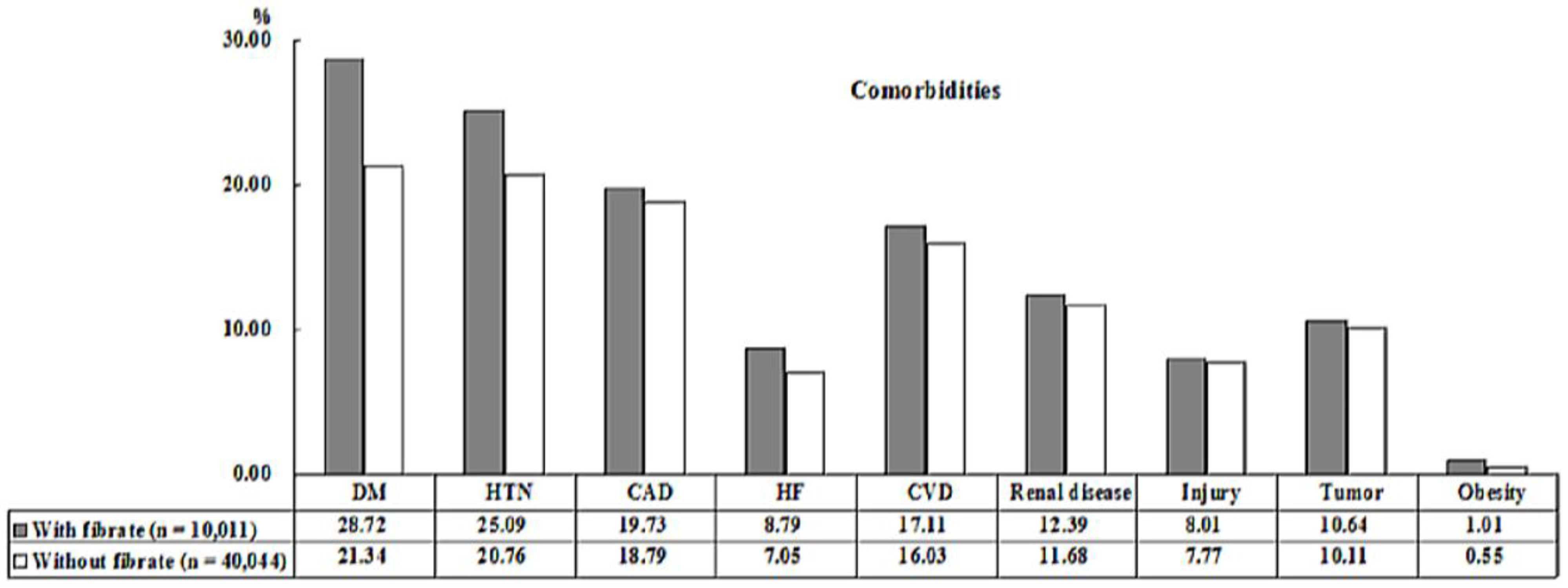
3.1. Baseline Characteristics of the Subjects
3.2. Fibrate Lowers the Risk of Developing OAG
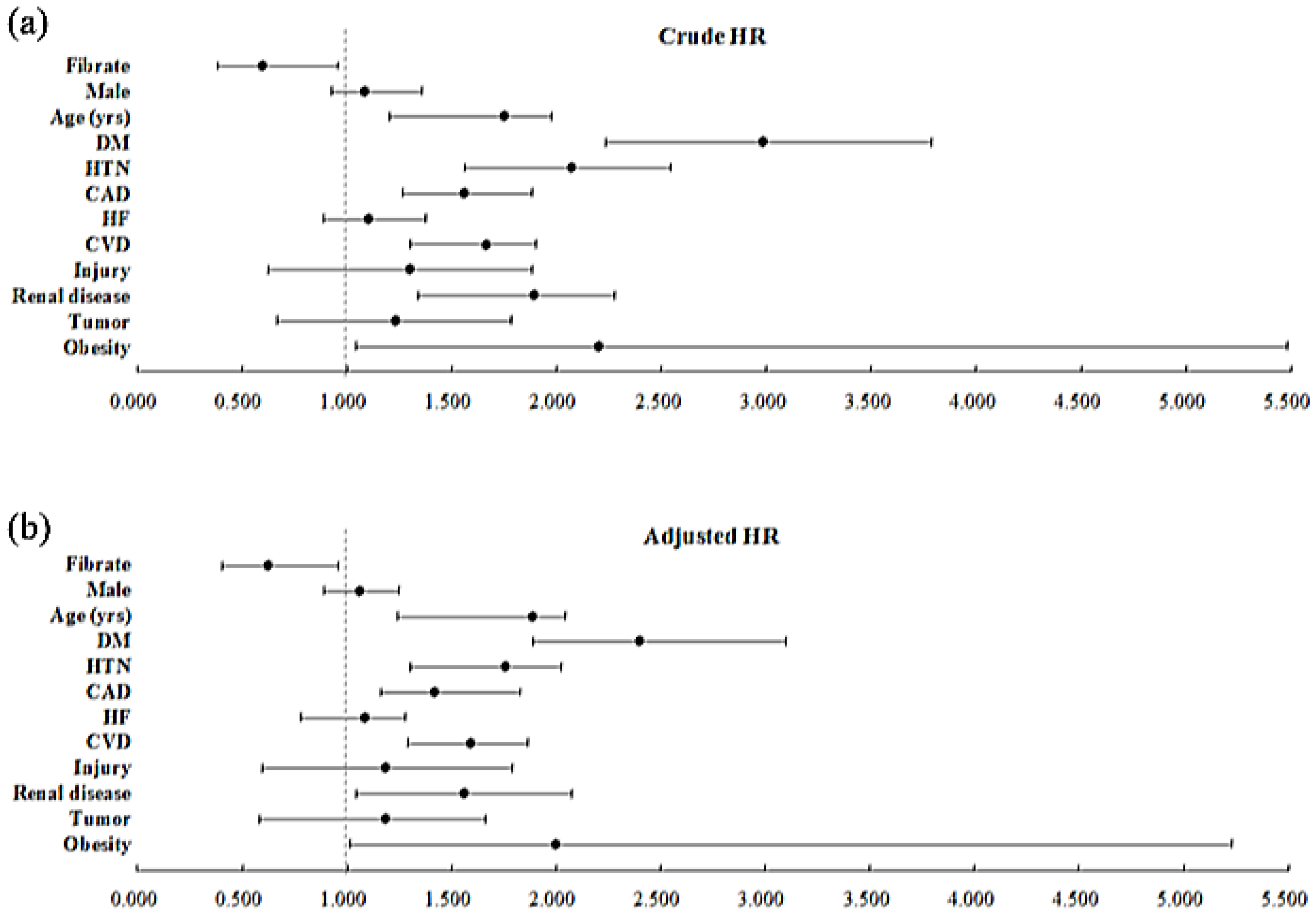
3.3. The Risk Factors for OAG
3.4. The Total Incidence of OAG with and without Using Fibrate in the Subgroup Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chan, E.W.; Li, X.; Tham, Y.-C.; Liao, J.; Wong, T.Y.; Aung, T.; Cheng, C.-Y. Glaucoma in Asia: Regional prevalence variations and future projections. Br. J. Ophthalmol. 2016, 100, 8–85. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Bao, X. Hyperlipidemia, blood lipid level, and the risk of glaucoma: A meta-analysis. Investig. Ophthalmol. Vis. Sci. 2019, 60, 1028–1043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogdanov, P.; Herna´ndez, C.; Corraliza, L.; Carvalho, A.R.; Simo, R. Effect of fenofibrate on retinal neurodegeneration in an experimental model of type 2 diabetes. Acta Diabetol. 2015, 52, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Escandon, P.; Vasini, B.; Whelchel, A.E.; Nicholas, S.E.; Matlock, H.G.; Ma, J.-X.; Karamichos, D. The role of peroxisome proliferator-activated receptors in healthy and diseased eyes. Exp. Eye Res. 2021, 208, 108617. [Google Scholar] [CrossRef] [PubMed]
- Bordet, R.; Ouk, T.; Petrault, O.; Gelé, P.; Gautier, S.; Laprais, M.; Deplanque, D.; Duriez, P.; Staels, B.; Fruchart, J.C.; et al. PPAR: A new pharmacological target for neuroprotection in stroke and neurodegenerative diseases. Biochem. Soc. Trans. 2006, 34, 1341–1346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, M.C.; Khosla, P.; Garg, K.N. Evaluation of effects of clofibrate, an antilipaemic agent on intraocular pressure in experimental glaucoma. Ind. J. Ophthalmol. 1985, 33, 313–315. [Google Scholar]
- Marrs, J.M.; Rowe, K.W., Jr. The effect of clofibrate on open-angle glaucoma. Arch. Ophthalmol. 1969, 82, 19–20. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.; Han, K.; Park, H.-Y.L.; Park, C.K. Type 2 diabetes mellitus and risk of open-angle glaucoma development in Koreans: An 11-year nationwide propensity-score-matched study. Diabetes Metab. 2018, 44, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Kuang, T.M.; Xirasagar, S.; Kao, Y.-W.; Shia, B.-C.; Lin, H.-C. Association of systemic hypertension with primary open-angle glaucoma: A population based case-control study. Am. J. Ophthalmol. 2020, 218, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-Y.; Hu, H.-Y.; Chu, D.; Chen, H.-H.; Chang, C.-K.; Chou, P. Patients with primary open-angle glaucoma may develop ischemic heart disease more often than those without glaucoma: An 11-year population-based cohort study. PLoS ONE 2016, 11, e0163210. [Google Scholar] [CrossRef] [PubMed]
- De Escalona-Rojas, J.E.M.; Cantero-Hinojosa, J.; Garrido-Pareja, F.; García-Serrano, J.L.; Padilla-Torres, J.F. Hemodynamic component in glaucoma and its association with risk factors and cardiovascular disease. Med. Clin. 2014, 143, 157–160. [Google Scholar]
- Park, S.J.; Byun, S.J.; Park, J.Y.; Kim, M. Primary open-angle glaucoma and increased risk of chronic kidney disease. J. Glaucoma 2019, 28, 1067–1073. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.; Han, K.; Park, H.-Y.L.; Lee, S.H.; Park, C.K. Metabolic health, obesity, and the risk of developing open-angle glaucoma: Metabolically healthy obese patients versus metabolically unhealthy but normal weight patients. Diabetes Metab. J. 2020, 44, 414–425. [Google Scholar] [CrossRef]
- Staels, B.; Dallongeville, J.; Auwerx, J.; Schoonjans, K.; Leitersdorf, E.; Fruchart, J.C. Mechanism of action of fibrates on lipid and lipoprotein metabolism. Circulation 1998, 98, 2088–2093. [Google Scholar] [CrossRef] [Green Version]
- Kersten, S. Peroxisome proliferator activated receptors and lipoprotein metabolism. PPAR Res. 2008, 2008, 132960. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castelli, V.; d’Angelo, M.; Antonosante, A.; Catanesi, M.; Benedetti, E.; Desideri, G.; Cimini, A. Physiology and pathophysiology of PPARs in the eye. Nucl. Recept. Res. 2018, 5, 101370. [Google Scholar] [CrossRef]
- Wu, T.Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef] [Green Version]


| Fibrate | Total | With | Without | p | |||
|---|---|---|---|---|---|---|---|
| Variables | n | % | n | % | n | % | |
| Total | 50,055 | 10,011 | 20.00 | 40,044 | 80.00 | ||
| Gender | 0.999 | ||||||
| Male | 27,855 | 55.65 | 5571 | 55.65 | 22,284 | 55.65 | |
| Female | 22,200 | 44.35 | 4440 | 44.35 | 17,760 | 44.35 | |
| Age (years) | 49.76 ± 18.07 | 49.98 ± 18.25 | 49.71 ± 18.03 | 0.181 | |||
| DM | <0.001 | ||||||
| Without | 38,636 | 77.19 | 7136 | 71.28 | 31,500 | 78.66 | |
| With | 11,419 | 22.81 | 2875 | 28.72 | 8544 | 21.34 | |
| HTN | <0.001 | ||||||
| Without | 39,231 | 78.38 | 7499 | 74.91 | 31,732 | 79.24 | |
| With | 10,824 | 21.62 | 2512 | 25.09 | 8312 | 20.76 | |
| CAD | 0.032 | ||||||
| Without | 40,557 | 81.02 | 8036 | 80.27 | 32,521 | 81.21 | |
| With | 9498 | 18.98 | 1975 | 19.73 | 7523 | 18.79 | |
| HF | <0.001 | ||||||
| Without | 46,350 | 92.60 | 9131 | 91.21 | 37,219 | 92.95 | |
| With | 3705 | 7.40 | 880 | 8.79 | 2825 | 7.05 | |
| CVD | 0.009 | ||||||
| Without | 41,922 | 83.75 | 8298 | 82.89 | 33,624 | 83.97 | |
| With | 8133 | 16.25 | 1713 | 17.11 | 6420 | 16.03 | |
| Renal disease | 0.049 | ||||||
| Without | 44,138 | 88.18 | 8771 | 87.61 | 35,367 | 88.32 | |
| With | 5917 | 11.82 | 1240 | 12.39 | 4677 | 11.68 | |
| Injury | 0.424 | ||||||
| Without | 46,141 | 92.18 | 9209 | 91.99 | 36,932 | 92.23 | |
| With | 3914 | 7.82 | 802 | 8.01 | 3112 | 7.77 | |
| Tumor | 0.119 | ||||||
| Without | 44,941 | 89.78 | 8946 | 89.36 | 35,995 | 89.89 | |
| With | 5114 | 10.22 | 1065 | 10.64 | 4049 | 10.11 | |
| Obesity | <0.001 | ||||||
| Without | 49,732 | 99.35 | 9910 | 98.99 | 39,822 | 99.45 | |
| With | 323 | 0.65 | 101 | 1.01 | 222 | 0.55 | |
| CCI_R | 1.00 ± 1.19 | 1.06 ± 1.24 | 0.99 ± 1.18 | <0.001 | |||
| Location | <0.001 | ||||||
| Northern Taiwan | 15,118 | 30.20 | 3012 | 30.09 | 12,106 | 30.23 | |
| Middle Taiwan | 13,522 | 27.01 | 2511 | 25.08 | 11,011 | 27.50 | |
| Southern Taiwan | 14,683 | 29.33 | 2804 | 28.01 | 11,879 | 29.66 | |
| Eastern Taiwan | 5256 | 10.50 | 1375 | 13.73 | 3881 | 9.69 | |
| Outlets islands | 1476 | 2.95 | 309 | 3.09 | 1167 | 2.91 | |
| Urbanization level | 0.083 | ||||||
| 1 (The highest) | 14,644 | 29.26 | 2886 | 28.83 | 11,758 | 29.36 | |
| 2 | 15,284 | 30.53 | 3015 | 30.12 | 12,269 | 30.64 | |
| 3 | 9974 | 19.93 | 1988 | 19.86 | 7986 | 19.94 | |
| 4 (The lowest) | 10,153 | 20.28 | 2122 | 21.20 | 8031 | 20.06 | |
| Level of care | <0.001 | ||||||
| Medical center | 10,389 | 20.76 | 2024 | 20.22 | 8365 | 20.89 | |
| Regional hospital | 11,874 | 23.72 | 1988 | 19.86 | 9886 | 24.69 | |
| Local hospital | 12,622 | 25.22 | 2498 | 24.95 | 10,124 | 25.28 | |
| Physician Clinics | 15,170 | 30.31 | 3501 | 34.97 | 11,669 | 29.14 | |
| Variables | Crude HR | 95% CI | 95% CI | p | Adjusted HR | 95% CI | 95% CI | p |
|---|---|---|---|---|---|---|---|---|
| Fibrate | ||||||||
| Without | Reference | Reference | ||||||
| With | 0.602 | 0.387 | 0.955 | 0.001 | 0.624 | 0.401 | 0.960 | 0.007 |
| Gender | ||||||||
| Male | 1.088 | 0.927 | 1.356 | 0.186 | 1.065 | 0.894 | 1.246 | 0.203 |
| Female | Reference | Reference | ||||||
| Age (yrs) | 1.752 | 1.201 | 1.976 | <0.001 | 1.892 | 1.244 | 2.045 | <0.001 |
| DM | ||||||||
| Without | Reference | Reference | ||||||
| With | 2.989 | 2.235 | 3.786 | <0.001 | 2.401 | 1.888 | 3.097 | <0.001 |
| HTN | ||||||||
| Without | Reference | Reference | ||||||
| With | 2.075 | 1.562 | 2.544 | <0.001 | 1.762 | 1.301 | 2.026 | <0.001 |
| CAD | ||||||||
| Without | Reference | Reference | ||||||
| With | 1.562 | 1.268 | 1.885 | <0.001 | 1.420 | 1.165 | 1.831 | <0.001 |
| HF | ||||||||
| Without | Reference | Reference | ||||||
| With | 1.103 | 0.892 | 1.378 | 0.188 | 1.086 | 0.781 | 1.279 | 0.276 |
| CVD | ||||||||
| Without | Reference | Reference | ||||||
| With | 1.664 | 1.304 | 1.904 | <0.001 | 1.594 | 1.289 | 1.862 | <0.001 |
| Injury | ||||||||
| Without | Reference | Reference | ||||||
| With | 1.303 | 0.624 | 1.880 | 0.486 | 1.186 | 0.597 | 1.789 | 0.571 |
| Renal disease | ||||||||
| Without | Reference | Reference | ||||||
| With | 1.894 | 1.341 | 2.275 | <0.001 | 1.562 | 1.048 | 2.076 | 0.002 |
| Tumor | ||||||||
| Without | Reference | Reference | ||||||
| With | 1.234 | 0.670 | 1.786 | 0.611 | 1.189 | 0.583 | 1.660 | 0.679 |
| Obesity | ||||||||
| Without | Reference | Reference | ||||||
| With | 2.201 | 1.046 | 5.484 | 0.005 | 2.000 | 1.017 | 5.231 | 0.034 |
| Fibrate | With | Without (Reference) | With vs. Without (Reference) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Stratified | Events | PYs | Rate (per 105 PYs) | Events | PYs | Rate (per 105 PYs) | Adjusted HR | 95% CI | 95% CI | p |
| Total | 376 | 81,205.68 | 463.02 | 1859 | 324,065.72 | 573.65 | 0.624 | 0.401 | 0.960 | 0.007 |
| Gender | ||||||||||
| Male | 190 | 45,189.96 | 420.45 | 931 | 180,339.64 | 516.25 | 0.630 | 0.406 | 0.969 | 0.014 |
| Female | 186 | 36,015.73 | 516.44 | 928 | 143,726.08 | 645.67 | 0.618 | 0.398 | 0.951 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, Y.-E.; Chen, Y.-H.; Sun, C.-A.; Chung, C.-H.; Chien, W.-C.; Chien, K.-H. Relationship between Using Fibrate and Open-Angle Glaucoma in Hyperlipidemic Patients: A Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 2415. https://doi.org/10.3390/ijerph19042415
Tsai Y-E, Chen Y-H, Sun C-A, Chung C-H, Chien W-C, Chien K-H. Relationship between Using Fibrate and Open-Angle Glaucoma in Hyperlipidemic Patients: A Population-Based Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(4):2415. https://doi.org/10.3390/ijerph19042415
Chicago/Turabian StyleTsai, Yung-En, Yi-Hao Chen, Chien-An Sun, Chi-Hsiang Chung, Wu-Chien Chien, and Ke-Hung Chien. 2022. "Relationship between Using Fibrate and Open-Angle Glaucoma in Hyperlipidemic Patients: A Population-Based Cohort Study" International Journal of Environmental Research and Public Health 19, no. 4: 2415. https://doi.org/10.3390/ijerph19042415
APA StyleTsai, Y.-E., Chen, Y.-H., Sun, C.-A., Chung, C.-H., Chien, W.-C., & Chien, K.-H. (2022). Relationship between Using Fibrate and Open-Angle Glaucoma in Hyperlipidemic Patients: A Population-Based Cohort Study. International Journal of Environmental Research and Public Health, 19(4), 2415. https://doi.org/10.3390/ijerph19042415







