Validation and Psychometric Properties of the Polish Version of the Skin Picking Scale-Revised
Abstract
:1. Introduction
2. Materials and Methods
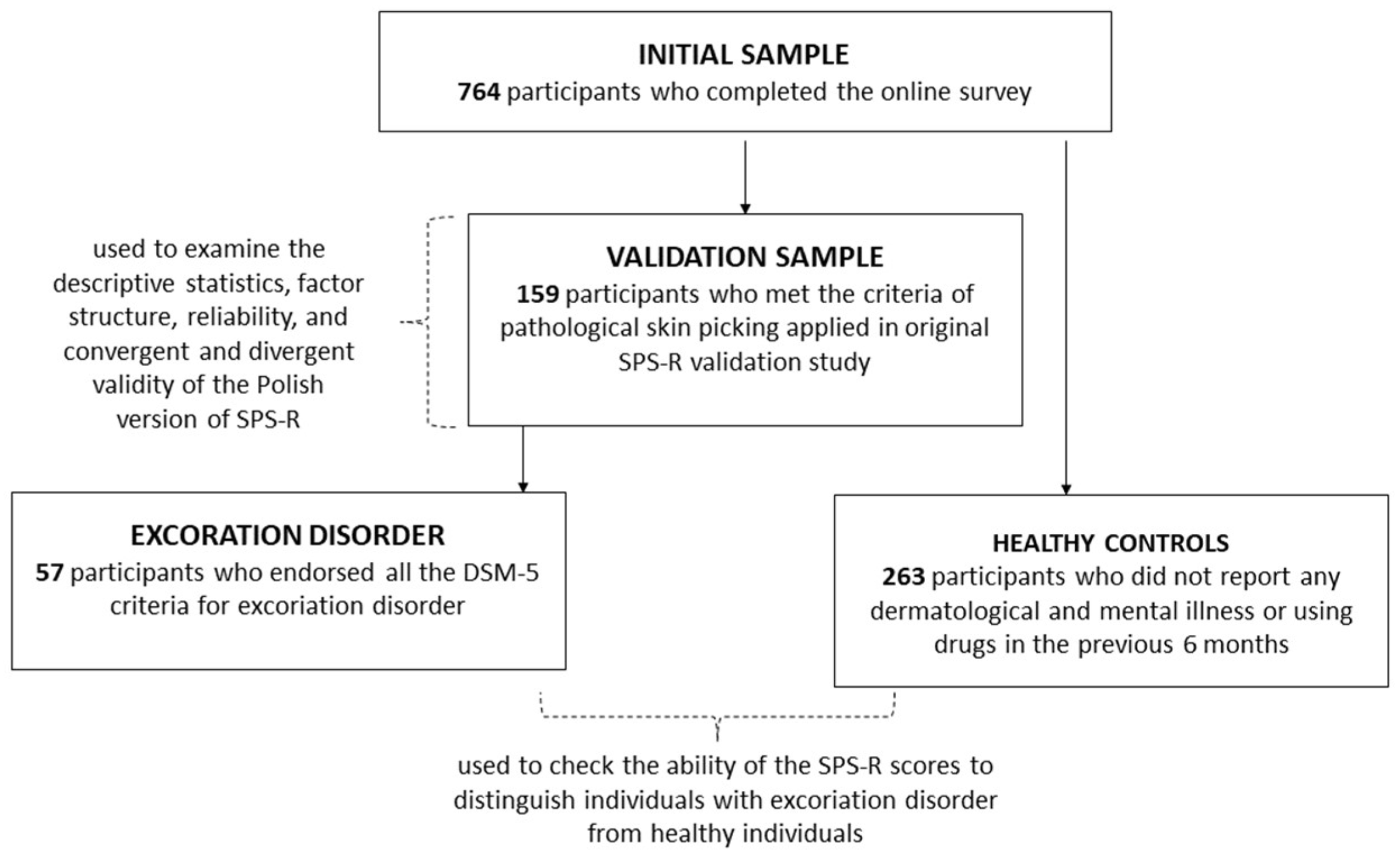
2.1. Participants
2.2. Measures
2.2.1. Skin Picking Scale Revised (SPS-R)
2.2.2. Depression Anxiety Stress Scales 21-Item Version (DASS-21)
2.2.3. Obsessive-Compulsive Inventory-Revised (OCI-R)
2.2.4. Skin Picking Disorder Diagnostic Criteria
2.2.5. Demographic and Illness History Data Sheet
2.3. Procedure
2.4. Determination of the Sample Size
2.5. Analysis Plan
3. Results
3.1. Descriptive Statistics
3.2. Factor Structure
3.3. Reliability
3.4. Convergent and Divergent Reliability
3.5. Diagnostic Accuracy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hayes, S.L.; Storch, E.A.; Berlanga, L. Skin picking behaviors: An examination of the prevalence and severity in a community sample. J. Anxiety Disord. 2009, 23, 314–319. [Google Scholar] [CrossRef] [Green Version]
- Keuthen, N.J.; Koran, L.M.; Aboujaoude, E.; Large, M.D.; Serpe, R.T. The prevalence of pathologic skin picking in US adults. Compr. Psychiatry 2010, 51, 183–186. [Google Scholar] [CrossRef]
- Bohne, A.; Wilhelm, S.; Keuthen, N.J.; Florin, I.; Baer, L.; Jenike, M.A. Prevalence of body dysmorphic disorder in a German college student sample. Psychiatry Res. 2002, 109, 101–104. [Google Scholar] [CrossRef]
- Calikusu, C.; Kucukgoncu, S.; Tecer, Ö.; Bestepe, E. Skin picking in Turkish students: Prevalence, characteristics, and gender differences. Behav. Modif. 2012, 36, 49–66. [Google Scholar] [CrossRef]
- Odlaug, B.L.; Grant, J.E. Clinical characteristics and medical complications of pathologic skin picking. Gen. Hosp. Psychiatry 2008, 30, 61–66. [Google Scholar] [CrossRef]
- Odlaug, B.L.; Grant, J.E. Phenomenology and epidemiology of pathological skin picking. In The Oxford Library of Psychology: Oxford Handbook of Impulse Control Disorders; Grant, J.E., Potenza, M.N., Eds.; Oxford University Press: Oxford, UK, 2011; pp. 186–195. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Arnold, L.M.; Mutasim, D.F.; Dwight, M.M.; Lamerson, C.L.; Morris, E.M.; McElroy, S.L. An open clinical trial of fluvoxamine treatment of psychogenic excoriation. J. Clin. Psychopharmacol. 1999, 19, 15–18. [Google Scholar] [CrossRef]
- Simeon, D.; Stein, D.J.; Gross, S.; Islam, N.; Schmeidler, J.; Hollander, E. A double-blind trial of fluoxetine in pathologic skin picking. J. Clin. Psychiatry 1997, 58, 341–347. [Google Scholar] [CrossRef]
- Keuthen, N.J.; Wilhelm, S.; Deckersbach, T.; Engelhard, I.M.; Forker, A.E.; Baer, L.; Jenike, M.A. The Skin Picking Scale: Scale construction and psychometric analyses. J. Psychosom. Res. 2001, 50, 337–341. [Google Scholar] [CrossRef]
- Snorrason, I.; Olafsson, R.P.; Flessner, C.A.; Keuthen, N.J.; Franklin, M.E.; Woods, D.W. The skin picking scale-revised: Factor structure and psychometric properties. J. Obsess-Compuls. Rel. 2012, 1, 133–137. [Google Scholar] [CrossRef]
- Sheehan, D.V. The Anxiety Disease; Scribner’s: New York, NY, USA, 1983. [Google Scholar]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Foa, E.B.; Huppert, J.D.; Leiberg, S.; Langner, R.; Kichic, R.; Hajcak, G.; Salkovskis, P.M. The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychol. Assess. 2002, 14, 485–496. [Google Scholar] [CrossRef] [PubMed]
- Mojsa-Kaja, J.; Golonka, K.; Gawłowska, M. Preliminary analyses of psychometric characteristics of the Polish version of the Obsessive-Compulsive Inventory-Revised (OCI-R) in a non-clinical sample. Int. J. Occup. Med. Environ. Health. 2016, 29, 1011–1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soper, D.S. A-Priori Sample Size Calculator for Structural Equation Models [Software]. 2021. Available online: https://www.danielsoper.com/statcalc (accessed on 15 January 2021).
- Prochwicz, K.; Kałużna-Wielobób, A.; Kłosowska, J. Skin picking in a non-clinical sample of young Polish adults. Prevalence and characteristics. Compr. Psychiatry 2016, 71, 77–85. [Google Scholar] [CrossRef]
- Cole, D.A. Utility of confirmatory factor analysis in test validation research. J. Consult. Clin. Psychol. 1987, 55, 584–594. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Gallinat, C.; Keuthen, N.J.; Stefini, A.; Backenstrass, M. The assessment of skin picking in adolescence: Psychometric properties of the Skin Picking Scale-Revised (German version). Nord. J. Psychiatry 2017, 71, 145–150. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modelling, 3rd ed.; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Grant, J.E.; Odlaug, B.L.; Kim, S.W. A clinical comparison of pathologic skin picking and obsessive-compulsive disorder. Compr. Psychiatry 2010, 51, 347–352. [Google Scholar] [CrossRef]
- Snorrason, I.; Beard, C.; Peckham, A.D.; Björgvinsson, T. Transdiagnostic dimensions in obsessive-compulsive and related disorders: Associations with internalizing and externalizing symptoms. Psychol. Med. 2021, 51, 1657–1665. [Google Scholar] [CrossRef]
- Snorrason, I.; Conway, C.C.; Falkenstein, M.J.; Kelley, K.N.; Kuckertz, J.M. Higher order compulsivity versus grooming dimensions as treatment targets for the DSM-5 obsessive-compulsive and related disorders. Depress. Anxiety 2021. [Google Scholar] [CrossRef] [PubMed]
- Buchholz, J.; Reuman, L.; Blakey, S.; Abramowitz, J. Psychological Treatment of Obsessive-Compulsive Disorder: Efficacy, Mechanisms and Transdiagnostic Implications. In A Transdiagnostic Approach to Obsessions, Compulsions and Related Phenomena; Fontenelle, L., Yücel, M., Eds.; Cambridge University Press: Cambridge, UK, 2019; pp. 207–216. [Google Scholar] [CrossRef]
- Dixon, L.J.; Snorrason, I. Prevalence and clinical characteristics of skin picking among adults with skin disease symptoms. J. Obsess-Compuls. Rel. 2019, 22, 100454. [Google Scholar] [CrossRef]
- Solley, K.; Turner, C. Prevalence and correlates of clinically significant body-focused repetitive behaviors in a non-clinical sample. Compr. Psychiatry 2018, 86, 9–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | Women (N = 141) | Men (N = 15) | Total (N = 159) | |
|---|---|---|---|---|
| Age | Mean (SD) | 23.46 (5.78) | 25.40 (10.22) | 23.58 (6.29) |
| Marital status | N (%) | |||
| Single | 61 (43.26) | 7 (46.67) | 71 (44.65) | |
| In relationship but not married | 69 (48.94) | 6 (40.00) | 75 (47.17) | |
| Married | 11 (7.80) | 2 (13.33) | 13 (8.18) | |
| Education | N (%) | |||
| Primary school graduate | 2 (1.41) | 0 (0.00) | 2 (1.26) | |
| Secondary school graduate | 3 (2.13) | 0 (0.00) | 3 (1.89) | |
| Higher secondary school graduate | 98 (69.50) | 14 (93.33) | 115 (72.33) | |
| Vocational education | 2 (1.41) | 0 (0.00) | 2 (1.26) | |
| University graduate | 35 (24.82) | 1.00 (6.66) | 36 (22.64) | |
| PhD | 1 (0.71) | 0.00 (0.00) | 1 (0.63) | |
| Employment status b | N (%) | |||
| Student | 110 (78.01) | 5 (33.33) | 115 (72.33) | |
| Employed | 63 (44.68) | 12 (0.80) | 75 (47.17) | |
| Unemployed | 3 (2.13) | 0 (0.00) | 3 (1.89) | |
| Pensioner | 4 (2.84) | 0 (0.00) | 4 (2.52) | |
| Income (PLN) | N (%) | |||
| <2000 | 96 (68.09) | 11(73.33) | 110 (69.18) | |
| 2000–3999 | 38 (26.95) | 3 (20.00) | 41 (25.79) | |
| 4000–5999 | 3 (2.13) | 1 (6.67) | 4 (2.52) | |
| 6000–9999 | 2 (1.41) | 0 (0.00) | 2 (1.26) | |
| >10,000 | 2 (1.41) | 0 (0.00) | 2 (1.26) | |
| Place of residence | N (%) | |||
| Village/rural area | 28 (19.86) | 3 (20.00) | 31 (19.50) | |
| <20,000 inhabitants | 14 (9.93) | 3 (20.00) | 17 (10.69) | |
| 20,000–50,000 inhabitants | 12 (8.51) | 1 (6.67) | 13 (8.18) | |
| 50,000–100,000 inhabitants | 14 (9.93) | 2 (13.33) | 16 (10.06) | |
| 100,000–200,000 inhabitants | 9 (6.38) | 0 (0.00) | 10 (6.29) | |
| 200,000–500,000 inhabitants | 12 (8.51) | 1 (6.67) | 14 (8.81) | |
| >500,000 inhabitants | 52 (36.88) | 5 (33.33) | 58 (36.48) |
| Mean (SD) | |||||||
|---|---|---|---|---|---|---|---|
| Scale | Total Sample | Women/Men | Median | Skewness | Kurtosis | Observed Range | Possible Range |
| SPS-R | 12.062 (4.553) | 12.063 (4.526)/11.733 (5.035) | 11.000 | 0.705 | 0.175 | 5–27 | 0–32 |
| SPS-R severity | 7.863 (2.687) | 7.867 (2.625)/7.400 (2.898) | 8.000 | 0.191 | −0.394 | 2–15 | 0–16 |
| SPS-R impairment | 4.199 (2.487) | 4.196 (2.501)/4.333 (2.664) | 3.000 | 1.416 | 2.231 | 1–14 | 0–16 |
| SPS-R item 1 | 2.037 (0.894) | 2.030 (0.896)/1.930 (0.799) | 2.000 | 0.405 | −0.492 | 0–4 | 0–4 |
| SPS-R item 2 | 2.280 (0.823) | 2.280 (0.817)/ 2.200 (0.941) | 2.000 | −0.288 | 0.018 | 0–4 | 0–4 |
| SPS-R item 3 | 1.584 (0.755) | 1.590 (0.744)/1.400 (0.632) | 1.000 | 0.948 | 0.197 | 0–4 | 0–4 |
| SPS-R item 4 | 1.963 (0.968) | 1.970 (0.911)/1.870 (1.356) | 2.000 | 0.159 | −0.509 | 0–4 | 0–4 |
| SPS-R item 5 | 1.640 (0.926) | 1.680 (0.908)/1.400 (1.121) | 1.000 | 0.492 | −0.358 | 0–4 | 0–4 |
| SPS-R item 6 | 0.739 (0.848) | 0.730 (0.857)/0.930 (0.799) | 1.000 | 1.213 | 1.414 | 0–4 | 0–4 |
| SPS-R item 7 | 0.453 (0.741) | 0.430 (0.707)/0.670 (0.976) | 0.000 | 1.654 | 2.205 | 0–3 | 0–4 |
| SPS-R item 8 | 1.366 (0.677) | 1.360 (0.687)/1.330 (0.617) | 1.000 | 0.497 | 0.188 | 0–3 | 0–4 |
| OCI-R | 17.925 (11.589) | 17.385 (11.523)/20.867 (10.690) | 17.000 | 0.536 | −0.512 | 0–47 | 0–72 |
| DASS-21 total | 27.379 (13.923) | 27.322 (13.626)/25.867 (15.959) | 28.000 | 0.163 | −0.716 | 0–58 | 0–63 |
| DASS-21 depression | 9.366 (5.779) | 9.315 (5.761)/8.800 (5.979) | 9.000 | 0.189 | −1.083 | 0–21 | 0–21 |
| DASS-21 anxiety | 6.988 (5.138) | 7.028 (5.074)/6.200 (5.199) | 6.000 | 0.616 | −0.482 | 0–20 | 0–21 |
| DASS-21 stress | 11.025 (5.017) | 10.979 (4.881)/10.867 (6.300) | 11.000 | −0.119 | −0.759 | 0–21 | 0–21 |
| 95% Confidence Interval | ||||||||
|---|---|---|---|---|---|---|---|---|
| Factor | Item | Estimate | Std. Error | Lower | Upper | z | p | Standardized Estimate |
| Two-factor model | ||||||||
| SPS-R Severity | ||||||||
| Item 1 | 0.678 | 0.060 | 0.561 | 0.795 | 11.352 | <0.001 | 0.757 | |
| Item 2 | 0.677 | 0.058 | 0.563 | 0.791 | 11.648 | <0.001 | 0.818 | |
| Item 3 | 0.472 | 0.054 | 0.366 | 0.578 | 8.735 | <0.001 | 0.624 | |
| Item 4 | 0.543 | 0.067 | 0.411 | 0.676 | 8.053 | <0.001 | 0.562 | |
| SPS-R Impairment | ||||||||
| Item 5 | 0.647 | 0.074 | 0.503 | 0.791 | 8.793 | <0.001 | 0.696 | |
| Item 6 | 0.640 | 0.085 | 0.472 | 0.807 | 7.493 | <0.001 | 0.753 | |
| Item 7 | 0.384 | 0.087 | 0.213 | 0.555 | 4.400 | <0.001 | 0.516 | |
| Item 8 | 0.489 | 0.051 | 0.389 | 0.590 | 9.512 | <0.001 | 0.728 | |
| One-factor model | ||||||||
| SPS-R Total | ||||||||
| Item 1 | 0.630 | 0.059 | 0.515 | 0.744 | 10.745 | <0.001 | 0.703 | |
| Item 2 | 0.639 | 0.055 | 0.531 | 0.748 | 11.588 | <0.001 | 0.772 | |
| Item 3 | 0.443 | 0.052 | 0.340 | 0.545 | 8.437 | <0.001 | 0.585 | |
| Item 4 | 0.524 | 0.065 | 0.396 | 0.652 | 8.024 | <0.001 | 0.542 | |
| Item 5 | 0.567 | 0.072 | 0.425 | 0.710 | 7.830 | <0.001 | 0.611 | |
| Item 6 | 0.546 | 0.081 | 0.386 | 0.705 | 6.715 | <0.001 | 0.643 | |
| Item 7 | 0.314 | 0.077 | 0.162 | 0.465 | 4.060 | <0.001 | 0.422 | |
| Item 8 | 0.418 | 0.050 | 0.320 | 0.515 | 8.409 | <0.001 | 0.622 | |
| Cronbach’s Alpha | Cronbach’s Alpha | |||
|---|---|---|---|---|
| SPS-R | Item | If Item Dropped | Item—Total Correlation | Total Scale |
| Severity | 0.783 | |||
| Item 1 | 0.680 | 0.679 | ||
| Item 2 | 0.707 | 0.636 | ||
| Item 3 | 0.722 | 0.613 | ||
| Item 4 | 0.805 | 0.459 | ||
| Impairment | 0.776 | |||
| Item 5 | 0.759 | 0.529 | ||
| Item 6 | 0.683 | 0.650 | ||
| Item 7 | 0.733 | 0.561 | ||
| Item 8 | 0.713 | 0.614 | ||
| Total | 0.836 | |||
| Item 1 | 0.809 | 0.624 | ||
| Item 2 | 0.803 | 0.673 | ||
| Item 3 | 0.821 | 0.530 | ||
| Item 4 | 0.830 | 0.481 | ||
| Item 5 | 0.819 | 0.557 | ||
| Item 6 | 0.808 | 0.634 | ||
| Item 7 | 0.830 | 0.452 | ||
| Item 8 | 0.814 | 0.606 |
| 95% Confidence Interval | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cutpoint | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Youden’s Index | AUC | SE | Lower | Upper | |
| 1 | 100 | 67.80 | 40.14 | 100 | 0.678 | 0.995 | 0.002 | 0.990 | 1.000 | <0.001 |
| 2 | 100 | 74.62 | 45.97 | 100 | 0.746 | |||||
| 3 | 100 | 82.20 | 54.81 | 100 | 0.822 | |||||
| 4 | 100 | 87.88 | 64.04 | 100 | 0.878 | |||||
| 5 | 100 | 93.94 | 78.08 | 100 | 0.939 | |||||
| 6 | 96.49 | 96.21 | 84.62 | 99.22 | 0.927 | |||||
| 7 | 94.74 | 97.35 | 88.52 | 98.85 | 0.921 | |||||
| 8 | 89.47 | 98.11 | 91.09 | 97.74 | 0.876 | |||||
| 10 c | 85.96 | 98.86 | 94.23 | 97.03 | 0.848 | |||||
| 11 | 84.21 | 99.24 | 96.00 | 96.68 | 0.835 | |||||
| 12 | 77.19 | 99.62 | 97.78 | 95.29 | 0.768 | |||||
| 13 | 75.44 | 99.62 | 97.73 | 94.95 | 0.751 | |||||
| 14 | 70.18 | 99.62 | 97.56 | 93.93 | 0.698 | |||||
| 15 | 57.89 | 100 | 100 | 91.67 | 0.579 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kłosowska, J.; Prochwicz, K.; Sznajder, D.; Antosz-Rekucka, R.; Tuleja, A.; Dembińska, A.; Snorrason, I. Validation and Psychometric Properties of the Polish Version of the Skin Picking Scale-Revised. Int. J. Environ. Res. Public Health 2022, 19, 2578. https://doi.org/10.3390/ijerph19052578
Kłosowska J, Prochwicz K, Sznajder D, Antosz-Rekucka R, Tuleja A, Dembińska A, Snorrason I. Validation and Psychometric Properties of the Polish Version of the Skin Picking Scale-Revised. International Journal of Environmental Research and Public Health. 2022; 19(5):2578. https://doi.org/10.3390/ijerph19052578
Chicago/Turabian StyleKłosowska, Joanna, Katarzyna Prochwicz, Dominika Sznajder, Rachela Antosz-Rekucka, Aleksandra Tuleja, Aleksandra Dembińska, and Ivar Snorrason. 2022. "Validation and Psychometric Properties of the Polish Version of the Skin Picking Scale-Revised" International Journal of Environmental Research and Public Health 19, no. 5: 2578. https://doi.org/10.3390/ijerph19052578
APA StyleKłosowska, J., Prochwicz, K., Sznajder, D., Antosz-Rekucka, R., Tuleja, A., Dembińska, A., & Snorrason, I. (2022). Validation and Psychometric Properties of the Polish Version of the Skin Picking Scale-Revised. International Journal of Environmental Research and Public Health, 19(5), 2578. https://doi.org/10.3390/ijerph19052578








