Physical Fitness—Not Physical Activity Levels—Influence Quality of Life in Anorexia Nervosa
Abstract
:1. Introduction
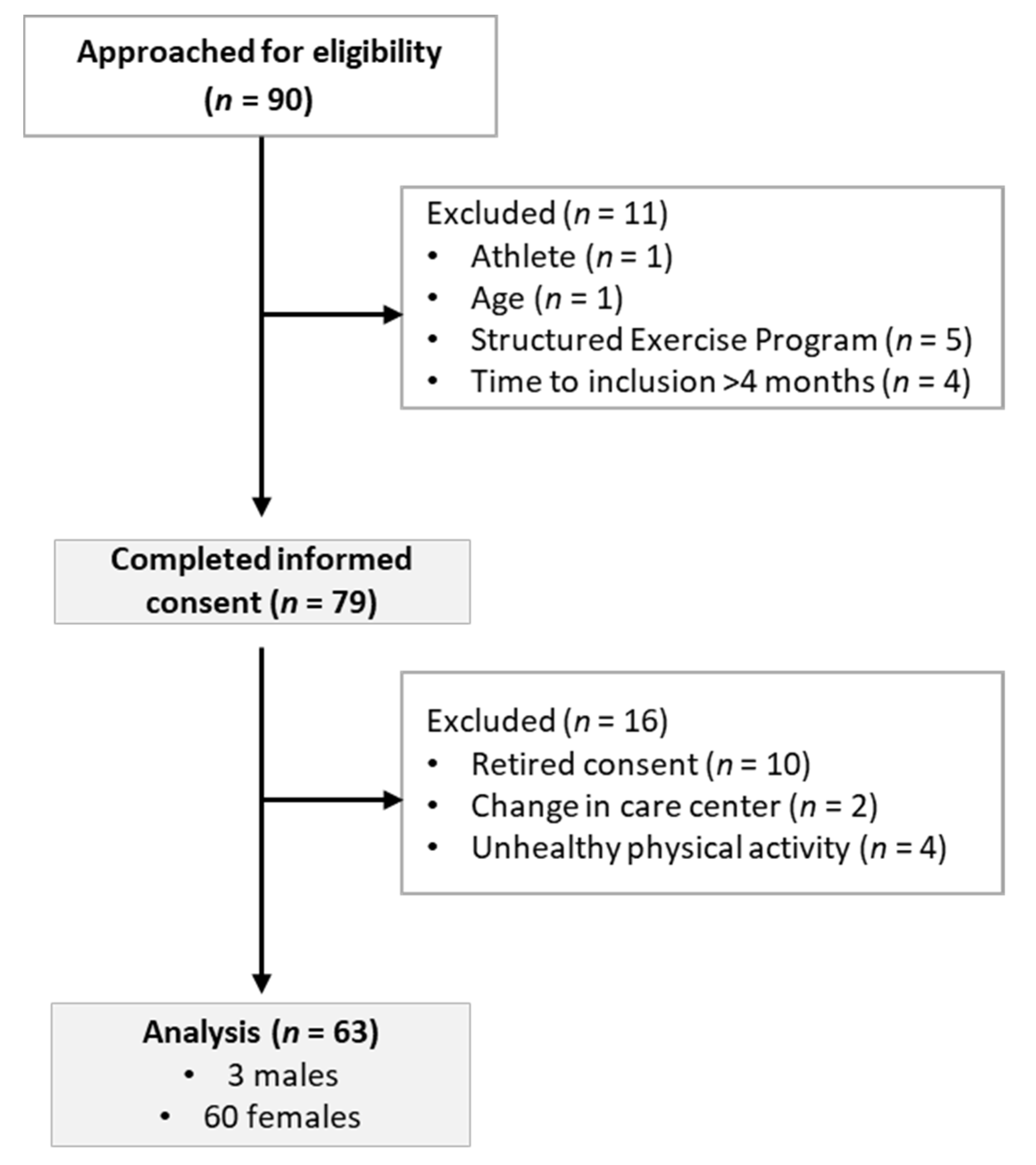
2. Materials and Methods
2.1. Physical Activity Assessment
2.2. Physical Fitness Assessments
2.2.1. Cardiorespiratory Fitness
2.2.2. Muscular Strength and Functional Mobility
2.2.3. Body Composition
2.2.4. Diet Management
2.3. Quality of Life Assessment
2.4. Statistical Analysis
3. Results
3.1. Physical Activity
3.2. Physical Fitness
3.3. Body Composition
3.4. Quality of Life
3.5. Association Analyses
3.6. Logistic Regression Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Edakubo, S.; Fushimi, K. Mortality and risk assessment for anorexia nervosa in acute-care hospitals: A nationwide administrative database analysis. BMC Psychiatry 2020, 20, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti, M.; Galvani, C.; Capelli, C.; Lanza, M.; El Ghoch, M.; Calugi, S.; Dalle Grave, R. Physical fitness before and after weight restoration in anorexia nervosa. J. Sports Med. Phys. Fitness 2013, 53, 396–402. [Google Scholar] [PubMed]
- Dalle Grave, R. Excessive and Compulsive Exercise in Eating Disorders: Prevalence, Associated Features, and Management. Dir. Psychiatry 2008, 28, 273–282. [Google Scholar]
- Melissa, R.; Lama, M.; Laurence, K.; Sylvie, B.; Jeanne, D.; Odile, V.; Nathalie, G. Physical Activity in Eating Disorders: A Systematic Review. Nutrients 2020, 12, 183. [Google Scholar] [CrossRef] [Green Version]
- Berends, T.; Boonstra, N.; Van Elburg, A. Relapse in anorexia nervosa: A systematic review and meta-analysis. Curr. Opin. Psychiatry 2018, 31, 445–455. [Google Scholar] [CrossRef]
- Ibrahim, A.; Cutinha, D.; Ayton, A. What is the evidence for using bed rest as part of hospital treatment of severe anorexia nervosa? Evid. Based. Ment. Health 2019, 22, 77–82. [Google Scholar] [CrossRef]
- DiVasta, A.D.; Feldman, H.A.; Quach, A.E.; Balestrino, M.; Gordon, C.M. The effect of bed rest on bone turnover in young women hospitalized for anorexia nervosa: A pilot study. J. Clin. Endocrinol. Metab. 2009, 94, 1650–1655. [Google Scholar] [CrossRef] [Green Version]
- DiVasta, A.D.; Feldman, H.A.; Rubin, C.T.; Gallagher, J.S.; Stokes, N.; Kiel, D.P.; Snyder, B.D.; Gordon, C.M. The ability of low-magnitude mechanical signals to normalize bone turnover in adolescents hospitalized for anorexia nervosa. Osteoporos. Int. 2017, 28, 1255–1263. [Google Scholar] [CrossRef]
- Touyz, S.W.; Beumont, P.J.V.; Glaun, D. A comparison of lenient and strict operant conditioning programmes in refeeding patients with anorexia nervosa. Br. J. Psychiatry 1984, 144, 517–520. [Google Scholar] [CrossRef]
- Griffiths, R.; Gross, G.; Russell, J.; Thornton, C.; Beumont, P.; Schotte, D.; Touyz, S. Perceptions of bed rest by anorexic patients. Int. J. Eat. Disord. 1998, 23, 443–447. [Google Scholar] [CrossRef]
- Parry, S.M.; Puthucheary, Z.A. The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extrem. Physiol. Med. 2015, 4, 16. [Google Scholar] [CrossRef] [Green Version]
- Achamrah, N.; Coëffier, M.; Reviews, P.D.-N. Physical activity in patients with anorexia nervosa. Nutr. Rev. 2016, 74, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Quesnel, D.A.; Libben, M.D.; Oelke, N.I.; Clark, M.; Willis-Stewart, S.; Caperchione, C.M. Is abstinence really the best option? Exploring the role of exercise in the treatment and management of eating disorders. Eat. Disord. 2018, 26, 290–310. [Google Scholar] [CrossRef]
- Szabo, C.P.; Green, K. Hospitalized anorexics and resistance training: Impact on body composition and psychological well-being. A preliminary study. Eat. Weight Disord. 2002, 7, 293–297. [Google Scholar] [CrossRef]
- Fernandez-del-Valle, M.; Larumbe-Zabala, E.; Villaseñor-Montarroso, A.; Cardona Gonzalez, C.; Diez-Vega, I.; Lopez Mojares, L.M.; Perez Ruiz, M. Resistance training enhances muscular performance in patients with anorexia nervosa: A randomized controlled trial. Int. J. Eat. Disord. 2014, 47, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-del-Valle, M.; Larumbe-Zabala, E.; Morande-Lavin, G.; Perez Ruiz, M. Muscle function and body composition profile in adolescents with restrictive anorexia nervosa: Does resistance training help? Disabil. Rehabil. 2016, 38, 346–353. [Google Scholar] [CrossRef]
- Chantler, I.; Szabo, C.P.; Green, K. Muscular strength changes in hospitalized anorexic patients after an eight week resistance training program. Int. J. Sport. Med. 2006, 27, 660–665. [Google Scholar] [CrossRef]
- Cook, B.; Leininger, L. The ethics of exercise in eating disorders: Can an ethical principles approach guide the next generation of research and clinical practice? J. Sport Health Sci. 2017, 6, 295–298. [Google Scholar] [CrossRef]
- Cook, B.; Hausenblas, H.; Tuccitto, D.; Giacobbi, P.R. Eating disorders and exercise: A structural equation modelling analysis of a conceptual model. Eur. Eat. Disord. Rev. 2011, 19, 216–225. [Google Scholar] [CrossRef]
- Ng, L.W.C.; Ng, D.P.; Wong, W.P. Is supervised exercise training safe in patients with anorexia nervosa? A meta-analysis. Physiotherapy 2013, 99, 1–11. [Google Scholar] [CrossRef]
- Vancampfort, D.; Vanderlinden, J.; De Hert, M.; Soundy, A.; Adámkova, M.; Skjaerven, L.H.; Catalán-Matamoros, D.; Lundvik Gyllensten, A.; Gómez-Conesa, A.; Probst, M. A systematic review of physical therapy interventions for patients with anorexia and bulemia nervosa. Disabil. Rehabil. 2014, 36, 628–634. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Misra, M.; Klibanski, A. Anorexia nervosa and bone. J. Endocrinol. 2014, 221, R163–R176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prince, S.A.; Adamo, K.B.; Hamel, M.E.; Hardt, J.; Gorber, S.C.; Tremblay, M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 56. [Google Scholar] [CrossRef] [Green Version]
- Alberti, M.; Galvani, C.; El Ghoch, M.; Capelli, C.; Lanza, M.; Calugi, S.; Dalle Grave, R. Assessment of physical activity in anorexia nervosa and treatment outcome. Med. Sci. Sports Exerc. 2013, 45, 1643–1648. [Google Scholar] [CrossRef] [Green Version]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults a systematic review and meta-analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef]
- Martinez-Gomez, D.; Ortega, F.B.; Ruiz, J.R.; Vicente-Rodriguez, G.; Veiga, O.L.; Widhalm, K.; Manios, Y.; Béghin, L.; Valtueña, J.; Kafatos, A.; et al. Excessive sedentary time and low cardiorespiratory fitness in European adolescents: The HELENA study. Arch. Dis. Child. 2011, 96, 240–246. [Google Scholar] [CrossRef] [Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, 1623–1627. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®), 5th ed.; American Psychiatric Association: Arlington, TX, USA, 2013. [Google Scholar]
- Beumont, P.J.V.; Arthur, B.; Russell, J.D.; Touyz, S.W. Excessive physical activity in dieting disorder patients: Proposals for a supervised exercise program. Int. J. Eat. Disord. 1994, 15, 21–36. [Google Scholar] [CrossRef]
- Fewell, L.K.; Nickols, R.; Schlitzer Tierney, A.; Levinson, C.A. Strength and power improvements in athlete and non-athletes during intensive eating disorder treatment. J. Clin. Sport Psychol. 2018, 12, 562–577. [Google Scholar] [CrossRef]
- Rich, C.; Geraci, M.; Griffiths, L.; Sera, F.; Dezateux, C.; Cortina-Borja, M. Quality Control Methods in Accelerometer Data Processing: Defining Minimum Wear Time. PLoS ONE 2013, 8, e67206. [Google Scholar] [CrossRef]
- Andersen, L.B.; Harro, M.; Sardinha, L.B.; Froberg, K.; Ekelund, U.; Brage, S.; Anderssen, S.A. Physical activity and clustered cardiovascular risk in children: A cross-sectional study (The European Youth Heart Study). Lancet 2006, 368, 299–304. [Google Scholar] [CrossRef]
- Freedson, P.; Melanson, E.; Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef] [PubMed]
- Marfell-Jones, M.J.; Stewart, A.D.; de Ridder, J.H. International Standards for Anthorpometric Assessment; International Society for the Advancement of Kinanthropometry (ISAK): Glasgow, Scotland, 2012; ISBN 0868037125. [Google Scholar]
- Heyward, V. ASEP Methods Recommendation: Body Composition Assessment. Int. Electron. J. 2001, 4, 1–12. [Google Scholar]
- Poortmans, J.R.; Boisseau, N.; Moraine, J.J.; Moreno-Reyes, R.; Goldman, S. Estimation of total-body skeletal muscle mass in children and adolescents. Med. Sci Sport. Exerc. 2005, 37, 316. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; McManus, C.; Smith, J.; Stevens, V.; Nixon, D.W. Anthropometric measurement of muscle mass: Revised equations for calculating bone-free arm muscle area. Am. J. Clin. Nutr. 1982, 36, 680–690. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Snow, K.K.; Kosinski, M.; Gandek, B. SF-36 Health Survey: Manual and Interpretation Guide; New England Medical Center: Boston, MA, USA, 1993. [Google Scholar]
- Bar-Or, O.; Rowland, T.W. Pediatric Exercise Medicine: From Physiologic Principles to Health Care Application; Human Kinetics Publishers: Champaign, IL, USA, 2004; ISBN 0880115971. [Google Scholar]
- Marchese, V.G.; Oriel, K.N.; Fry, J.A.; Kovacs, J.L.; Weaver, R.L.; Reilly, M.M.; Ginsberg, J.P. Development of reference values for the Functional Mobility Assessment. Pediatr. Phys. Ther. 2012, 24, 224–230. [Google Scholar] [CrossRef]
- Moreno, L.A.; Mesana, M.I.; González-Gross, M.; Gil, C.M.; Fleta, J.; Wärnberg, J.; Ruiz, J.R.; Sarría, A.; Marcos, A.; Bueno, M.; et al. Anthropometric body fat composition reference values in Spanish adolescents. The AVENA Study. Eur. J. Clin. Nutr. 2006, 60, 191–196. [Google Scholar] [CrossRef] [Green Version]
- Addo, O.Y.; Himes, J.H.; Zemel, B.S. Reference ranges for midupper arm circumference, upper arm muscle area, and upper arm fat area in US children and adolescents aged 1–20 y. Am. J. Clin. Nutr. 2017, 105, 111–120. [Google Scholar] [CrossRef] [Green Version]
- Ward, N.; Stiller, K.; Holland, A.E. Exercise as a therapeutic intervention for people with cystic fibrosis. Expert Rev. Respir. Med. 2019, 13, 449–458. [Google Scholar] [CrossRef]
- Verschuren, O.; Peterson, M.D.; Balemans, A.C.J.; Hurvitz, E.A. Exercise and physical activity recommendations for people with cerebral palsy. Dev. Med. Child Neurol. 2016, 58, 798–808. [Google Scholar] [CrossRef]
- Whooten, R.; Kerem, L.; Stanley, T. Physical Activity in Adolescents and Children and Relationship to Metabolic Health. Curr. Opin. Endocrinol. Diabetes. Obes. 2019, 26, 25. [Google Scholar] [CrossRef] [PubMed]
- Wurz, A.; Mclaughlin, E.; Lategan, C.; Ellis, K.; Culos-Reed, S.N. Synthesizing the literature on physical activity among children and adolescents affected by cancer: Evidence for the international Pediatric Oncology Exercise Guidelines (iPOEG). Transl. Behav. Med. 2021, 11, 699–708. [Google Scholar] [CrossRef] [PubMed]
- Skinner, J.S.; McLellan, T.H. The Transition from Aerobic to Anaerobic Metabolism. Res. Q. Exerc. Sport 1980, 51, 234–248. [Google Scholar] [CrossRef]
- Eisenmann, J.C.; Laurson, K.R.; Welk, G.J. Aerobic fitness percentiles for U.S. adolescents. Am. J. Prev. Med. 2011, 41, S106–S110. [Google Scholar] [CrossRef] [PubMed]
- Cook, B.; Engel, S.; Crosby, R.; Hausenblas, H.; Wonderlich, S.; Mitchell, J. Pathological motivations for exercise and eating disorder specific health-related quality of life. Int. J. Eat. Disord. 2014, 47, 268–272. [Google Scholar] [CrossRef] [Green Version]
- Jenkins, P.E.; Hoste, R.R.; Meyer, C.; Blissett, J.M. Eating disorders and quality of life: A review of the literature. Clin. Psychol. Rev. 2011, 31, 113–121. [Google Scholar] [CrossRef]
- Kane, C.; Tomotake, M.; Hamatani, S.; Chiba, S.; Ohmori, T. Clinical Factors Influencing Quality of Life in Anorexia Nervosa Patients. Open J. Psychiatry 2018, 08, 50–60. [Google Scholar] [CrossRef] [Green Version]
- Bermejo-Cantarero, A.; Álvarez-Bueno, C.; Martínez-Vizcaino, V.; Redondo-Tébar, A.; Pozuelo-Carrascosa, D.P.; Sánchez-López, M. Relationship between both cardiorespiratory and muscular fitness and health-related quality of life in children and adolescents: A systematic review and meta-analysis of observational studies. Health Q. Life Outcomes 2021, 19, 127. [Google Scholar] [CrossRef]
- Deenik, J.; Kruisdijk, F.; Tenback, D.; Braakman-Jansen, A.; Taal, E.; Hopman-Rock, M.; Beekman, A.; Tak, E.; Hendriksen, I.; van Harten, P. Physical activity and quality of life in long-term hospitalized patients with severe mental illness: A cross-sectional study. BMC Psychiatry 2017, 17, 298. [Google Scholar] [CrossRef] [Green Version]
- Van Eeden, A.E.; Van Hoeken, D.; Hoek, H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatry 2021, 34, 515. [Google Scholar] [CrossRef] [PubMed]

| n | Mean | SD | ||
|---|---|---|---|---|
| Age (years) | 63 | 13.5 | ± | 1.15 |
| BWlowest (kg) | 63 | 39.9 | ± | 6.3 |
| BMIlowest (kg/m2) | 63 | 15.8 | ± | 1.6 |
| Time to inclusion (days) | 63 | 49.5 | ± | 22.2 |
| BWgain (kg) | 63 | 5.6 | ± | 3.6 |
| n | Total | Weekdays | Weekends | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||||
| LPA (min/day) | 63 | 113.1 | ± | 57.7 | 110.3 | ± | 55.9 | 117.3 | ± | 63.0 |
| MPA (min/day) | 63 | 24.3 | ± | 13.4 | 24.0 | ± | 14.8 | 24.8 | ± | 16.5 |
| VPA (min/day) | 63 | 14.0 | ± | 11.0 | 13.8 | ± | 11.6 | 14.4 | ± | 12.9 |
| vVPA (min/day) | 63 | 7.1 | ± | 13.3 | 6.0 | ± | 8.9 | 8.6 | ± | 27.9 |
| MVPA (min/day) | 63 | 45.4 | ± | 22.5 | 43.8 | ± | 23.3 | 47.8 | ± | 34.6 |
| AT (min/day) | 63 | 156.5 | ± | 63.9 | 154.2 | ± | 63.0 | 160.1 | ± | 71.1 |
| ST (min/day) | 63 | 530.3 | ± | 99.3 | 546.7 | ± | 109.7 | 505.8 | ± | 108.2 |
| Relative ST (%) | 63 | 77.0 | ± | 10.1 | 77.7 | ± | 10.0 | 75.7 | ± | 11.2 |
| Wear time (min/day) | 63 | 686.9 | ± | 78.4 | 700.9 | ± | 91.0 | 665.9 | ± | 89.9 |
| n | Mean | SD | Min | Max | ||
|---|---|---|---|---|---|---|
| Muscular Strength | ||||||
| 6RM-BP (kg) | 63 | 43.5 | ± | 7.3 | 31.8 | 65.8 |
| 6RM-LP (kg) | 63 | 84.1 | ± | 17.1 | 29.5 | 113.4 |
| 6RM-LR (kg) | 63 | 43.1 | ± | 8.7 | 25.0 | 63.5 |
| Cardiorespiratory Fitness | ||||||
| SBP (mmHg) | 63 | 98.1 | ± | 11.1 | 80.0 | 120.0 |
| DBP (mmHg) | 63 | 59.2 | ± | 6.9 | 50.0 | 75.0 |
| Time-end-test (min) | 63 | 7.9 | ± | 1.4 | 5.7 | 12.8 |
| Speed-end-test (km/h) | 63 | 7.1 | ± | 0.7 | 5.1 | 9.3 |
| Incline-end-test (%) | 63 | 12.1 | ± | 1.3 | 8.5 | 16.5 |
| rVO2peak (mL/kg/min) | 63 | 38.7 | ± | 6.3 | 26.8 | 54.3 |
| aVO2peak (L/min) | 63 | 1.8 | ± | 0.4 * | 1.1 | 3.0 |
| HRpeak (bpm) | 63 | 187.4 | ± | 9.4 | 167.0 | 213.0 |
| VEpeak (L/min) | 63 | 67.2 | ± | 16.7 | 35.4 | 118.3 |
| %VO2 at VT1 | 63 | 51.7 | ± | 11.2 * | 31.9 | 86.0 |
| %VO2 at VT2 | 41 | 83.8 | ± | 9.9 ** | 51.7 | 99.6 |
| Functional Mobility | ||||||
| TUG-3m (seconds) | 63 | 4.2 | ± | 0.3 | 3.5 | 4.9 |
| TUG-10m (seconds) | 63 | 9.5 | ± | 0.8 | 7.9 | 11.1 |
| TUDS (seconds) | 63 | 6.2 | ± | 0.7 * | 4.8 | 9.7 |
| n | Mean | SD | Min | Max | ||
|---|---|---|---|---|---|---|
| Height (m) | 63 | 1.6 | ± | 0.8 | 1.4 | 1.9 |
| BW (kg) | 63 | 45.4 | ± | 7.5 | 29.3 | 71.6 |
| BMI (kg/m2) | 63 | 18.0 | ± | 2.1 | 13.4 | 23.1 |
| SMM (kg) | 63 | 17.8 | ± | 3.6 | 11.1 | 32.2 |
| %BF | 63 | 20.2 | ± | 3.9 | 11.5 | 28.4 |
| Sum6-SK (mm) | 63 | 66.9 | ± | 21.6 | 29.8 | 111.0 |
| Abdominal-SK (mm) | 63 | 14.2 | ± | 5.5 | 2.4 | 25.5 |
| Arm-C relaxed (cm) | 63 | 22.9 | ± | 2.4 | 17.0 | 29.7 |
| Arm-C contracted (cm) | 63 | 23.7 | ± | 2.0 | 18.2 | 27.7 |
| Upper-Thigh-C (cm) | 63 | 49.4 | ± | 5.0 | 32.7 | 59.0 |
| Mid-Thigh-C (cm) | 63 | 47.2 | ± | 5.0 | 32.7 | 55.0 |
| Calf-C relaxed (cm) | 63 | 32.3 | ± | 2.8 | 25.5 | 37.7 |
| Calf-C contracted (cm) | 63 | 32.8 | ± | 3.0 | 25.5 | 38.8 |
| Arm CSA (cm2) | 63 | 23.1 | ± | 6.3 | 11.5 | 51.3 |
| Mid-Thigh CSA (cm2) | 63 | 136.3 | ± | 27.2 | 53.2 | 208.4 |
| Calf CSA (cm2) | 63 | 58.6 | ± | 11.6 | 24.8 | 87.2 |
| n | Mean | SD | Min | Max | ||
|---|---|---|---|---|---|---|
| PF | 63 | 83.6 | ± | 21.7 * | 0.0 | 100.0 |
| RP | 63 | 66.8 | ± | 26.0 * | 0.0 | 100.0 |
| BP | 63 | 74.4 | ± | 23.2 * | 10.0 | 100.0 |
| GH | 63 | 64.9 | ± | 19.0 * | 18.8 | 100.0 |
| VT | 63 | 62.4 | ± | 22.3 * | 0.0 | 100.0 |
| SF | 63 | 65.5 | ± | 28.3 * | 12.5 | 100.0 |
| RE | 63 | 71.6 | ± | 25.7 * | 0.0 | 100.0 |
| MH | 63 | 57.9 | ± | 24.7 * | 0.0 | 100.0 |
| PCS | 63 | 51.3 | ± | 7.9 | 28.8 | 64.6 |
| MCS | 63 | 41.1 | ± | 13.5 * | 6.2 | 67.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agne, A.; Olmedillas, H.; Pérez Ruiz, M.; del Valle Soto, M.; Fernandez-del-Valle, M. Physical Fitness—Not Physical Activity Levels—Influence Quality of Life in Anorexia Nervosa. Int. J. Environ. Res. Public Health 2022, 19, 2678. https://doi.org/10.3390/ijerph19052678
Agne A, Olmedillas H, Pérez Ruiz M, del Valle Soto M, Fernandez-del-Valle M. Physical Fitness—Not Physical Activity Levels—Influence Quality of Life in Anorexia Nervosa. International Journal of Environmental Research and Public Health. 2022; 19(5):2678. https://doi.org/10.3390/ijerph19052678
Chicago/Turabian StyleAgne, Alexa, Hugo Olmedillas, Margarita Pérez Ruiz, Miguel del Valle Soto, and Maria Fernandez-del-Valle. 2022. "Physical Fitness—Not Physical Activity Levels—Influence Quality of Life in Anorexia Nervosa" International Journal of Environmental Research and Public Health 19, no. 5: 2678. https://doi.org/10.3390/ijerph19052678
APA StyleAgne, A., Olmedillas, H., Pérez Ruiz, M., del Valle Soto, M., & Fernandez-del-Valle, M. (2022). Physical Fitness—Not Physical Activity Levels—Influence Quality of Life in Anorexia Nervosa. International Journal of Environmental Research and Public Health, 19(5), 2678. https://doi.org/10.3390/ijerph19052678









