Parental Illness and Life Satisfaction among Young People: A Cross-Sectional Study of the Importance of School Factors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Life Satisfaction (Outcome)
2.2.2. Parental Illness (Exposure)
2.2.3. School-Related Factors
2.2.4. Combined Variables
2.2.5. Socioeconomic and Illness Characteristics
2.3. Statistical Analyses
3. Results
3.1. Association between Parental Illness, School-Related Factors, and Life Satisfaction
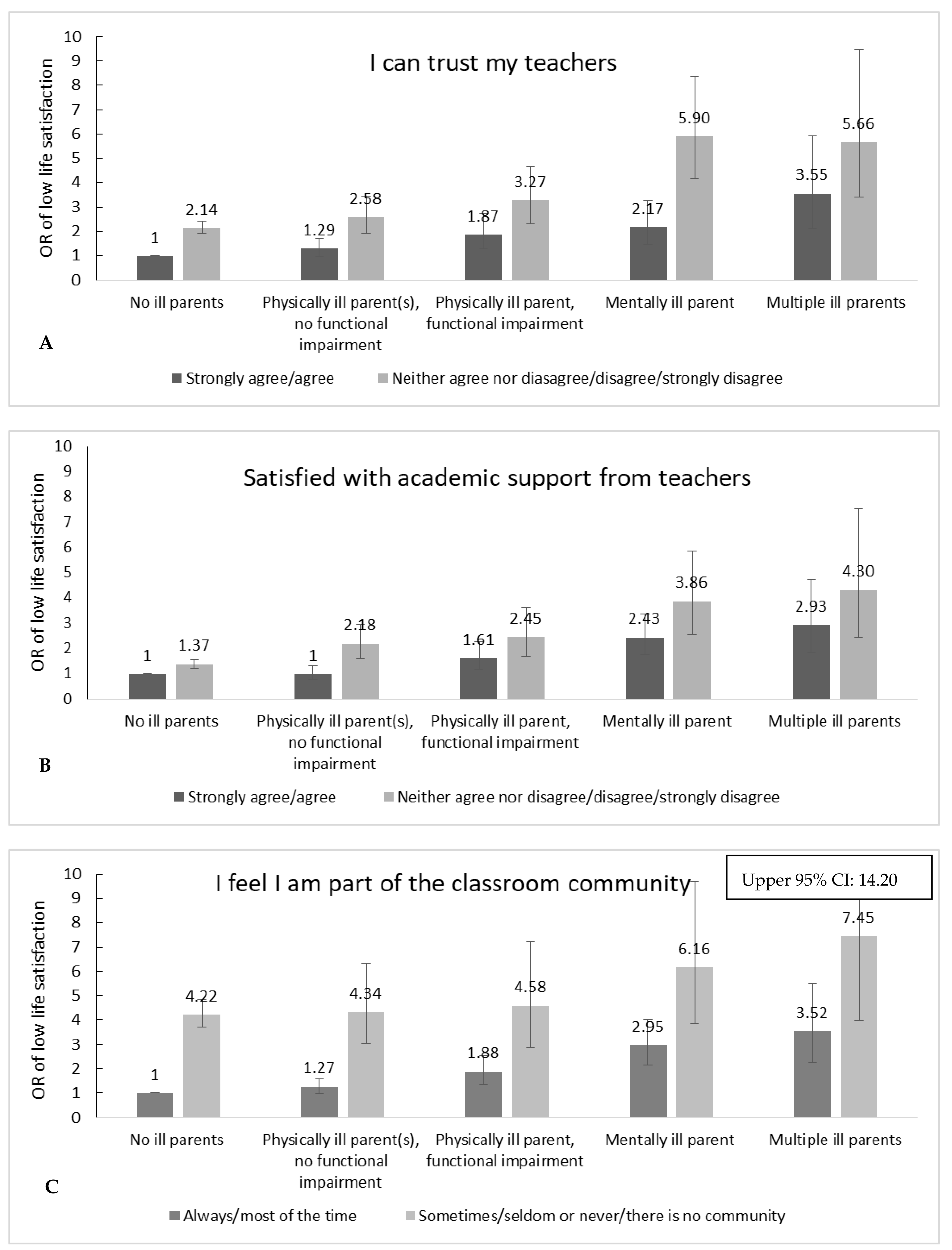
3.2. Joint Effect of School-Related Factors and Parental Illness on Life Satisfaction
3.3. Students’ Experiences with Student Counsellors
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barkmann, C.; Romer, G.; Watson, M.; Schulte-Markwort, M. Parental Physical Illness as a Risk for Psychosocial Maladjustment in Children and Adolescents: Epidemiological Findings from a National Survey in Germany. J. Psychosom. Res. 2007, 48, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Reupert, A.E.; Maybery, J.D.; Kowalenko, N.M. Children whose parents have a mental illness: Prevalence, need and treatment. Med. J. Aust. 2013, 1, 7–9. Available online: https://www.mja.com.au/system/files/issues/001_01_160412_open/reu11200_fm.pdf (accessed on 25 December 2021). [CrossRef] [PubMed] [Green Version]
- Nagl-Cupal, M.; Daniel, M.; Ma, M.M.K.; Ma, M.D. Prevalence and effects of caregiving on children. J. Adv. Nurs. 2014, 70, 2314–2325. [Google Scholar] [CrossRef] [PubMed]
- Stoeckel, M.; Weissbrod, C. Growing up with an ill parent: An examination of family characteristics and parental illness features. Fam. Syst. Health 2015, 33, 356–362. [Google Scholar] [CrossRef]
- Sieh, D.S.; Meijer, A.M.; Oort, F.J.; Visser-Meily, J.M.A.; Van Der Leij, D.A.V. Problem Behavior in Children of Chronically Ill Parents: A Meta-Analysis. Clin. Child Fam. Psychol. Rev. 2010, 13, 384–397. [Google Scholar] [CrossRef] [Green Version]
- Sieh, D.S.; Visser-Meily, J.M.A.; Oort, F.J.; Meijer, A.M. Risk factors for problem behavior in adolescents of parents with a chronic medical condition. Eur. Child Adolesc. Psychiatry 2012, 21, 459–471. [Google Scholar] [CrossRef] [Green Version]
- Houck, C.; Rodrigue, J.R.; Lobato, D. Parent—Adolescent Communication and Psychological Symptoms among Adolescents with Chronically Ill Parents. J. Pediatr. Psychol. 2007, 32, 596–604. [Google Scholar] [CrossRef] [Green Version]
- Dean, K.; Green, M.J.; Laurens, K.R.; Kariuki, M.; Tzoumakis, S.; Sprague, T.; Lenroot, R.; Carr, V.J. The impact of parental mental illness across the full diagnostic spectrum on externalising and internalising vulnerabilities in young offspring. Psychol. Med. 2018, 48, 2257–2263. [Google Scholar] [CrossRef] [Green Version]
- Joergensen, A.C.; Kjaer Urhoj, S.; Nybo Andersen, A.-M. Primary school achievement and socioeconomic attainment in individuals affected by parental cancer in childhood or adolescence: A Danish nationwide register-based study. J. Epidemiol. Community Health 2018. Available online: http://jech.bmj.com/lookup/doi/10.1136/jech-2018-210472 (accessed on 25 December 2021).
- Moberg, J.Y.; Laursen, B.; Koch-Henriksen, N.; Thygesen, L.C.; Brødsgaard, A.; Soelberg Sørensen, P.; Magyari, M. Employment, disability pension and income for children with parental multiple sclerosis. Mult. Scler. J. 2017, 23, 1148–1156. Available online: http://www.ncbi.nlm.nih.gov/pubmed/27682230 (accessed on 25 December 2021). [CrossRef]
- Chikhradze, N.; Knecht, C.; Metzing, S. Young carers: Growing up with chronic illness in the family—A systematic review 2007–2017. J. Compassionate Health Care 2017, 4, 1–16. Available online: https://link.springer.com/content/pdf/10.1186%2Fs40639-017-0041-3.pdf (accessed on 25 December 2021). [CrossRef] [Green Version]
- Lin, A.; Di Prinzio, P.; Young, D.; Jacoby, P.; Whitehouse, A.; Waters, F.; Jablensky, A.; Morgan, V.A. Academic Performance in Children of Mothers With Schizophrenia and Other Severe Mental Illness, and Risk for Subsequent Development of Psychosis: A Population-Based Study. Schizophr. Bull. 2017, 43, 205–213. Available online: http://www.ncbi.nlm.nih.gov/pubmed/27131155 (accessed on 25 December 2021). [CrossRef] [PubMed] [Green Version]
- Tabak, I.; Zabłocka-Żytka, L.; Ryan, P.; Poma, S.Z.; Joronen, K.; Viganò, G.; Simpson, W.; Paavilainen, E.; Scherbaum, N.; Smith, M.; et al. Needs, expectations and consequences for children growing up in a family where the parent has a mental illness. Int. J. Ment. Health Nurs. 2016, 25, 319–329. [Google Scholar] [CrossRef] [Green Version]
- Sieh, D.S.; Visser-Meily, J.M.A.; Meijer, A.M. Differential Outcomes of Adolescents with Chronically Ill and Healthy Parents. J. Child Fam. Stud. 2013, 22, 209–218. [Google Scholar] [CrossRef] [Green Version]
- Van der Werf, H.M.; Luttik, M.L.A.; Francke, A.L. Students growing up with a chronically ill family member; A survey on experienced consequences, background characteristics, and risk factors. BMC Public Health 2019, 19, 1486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leinonen, J.A.; Solantaus, T.S.; Punamaki, R.-L. Parental mental health and children’s adjustment: The quality of marital interaction and parenting as mediating factors. J. Child Psychol. Psychiatry 2003, 44, 227–241. [Google Scholar] [CrossRef] [PubMed]
- Piko, B.F.; Hamvai, C. Parent, school and peer-related correlates of adolescents’ life satisfaction. Child. Youth Serv. Rev. 2010, 32, 1479–1482. [Google Scholar] [CrossRef]
- Thapa, A.; Cohen, J.; Guffey, S.; Higgins-D’Alessandro, A. A Review of School Climate Research. Rev. Educ. Res. 2013, 83, 357–385. [Google Scholar] [CrossRef]
- Aldridge, J.M.; McChesney, K. The relationships between school climate and adolescent mental health and wellbeing: A systematic literature review. Int. J. Educ. Res. 2018, 88, 121–145. [Google Scholar] [CrossRef]
- Wang, M.T.; Degol, J.L. School Climate: A Review of the Construct, Measurement, and Impact on Student Outcomes. Educ. Psychol. Rev. 2016, 28, 315–352. [Google Scholar] [CrossRef]
- Suldo, S.M.; McMahan, M.M.; Chappel, A.M.; Loker, T. Relationships Between Perceived School Climate and Adolescent Mental Health Across Genders. Sch. Ment. Health 2012, 4, 69–80. [Google Scholar] [CrossRef]
- Rathmann, K.; Herke, M.G.; Hurrelmann, K.; Richter, M. Perceived class climate and school-aged children’s life satisfaction: The role of the learning environment in classrooms. PLoS ONE 2018, 13, e0189335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, J.; Mccabe, E.M.; Michelli, N.M. School Climate: Research, Policy, Paratice, and Teacher Education. Teach. Coll. Rec. 2009, 111, 180–213. [Google Scholar] [CrossRef]
- Masten, A.S.; Herbers, J.E.; Cutuli, J.J. Promoting competence and resilience in the school context. Prof. Sch. Couns. 2008, 12, 76–84. [Google Scholar] [CrossRef]
- Gilligan, R. Adversity, resilience and young people: The protective value of positive school and spare time experiences. Child Soc. 2000, 14, 37–47. [Google Scholar] [CrossRef]
- Brooks, J.E. Strengthening Resilience in Children and Youths: Maximizing Opportunities through the Schools. Child. Sch. 2006, 28, 69–76. [Google Scholar] [CrossRef]
- Rak, C.F.; Patterson, L.E. Promoting Resilience in At-Risk Children. J. Couns. Dev. 1996, 74, 368–373. [Google Scholar] [CrossRef]
- O’Malley, M.; Voight, A.; Renshaw, T.L.; Eklund, K. School climate, family structure, and academic achievement: A study of moderation effects. Sch. Psychol. Q. 2015, 30, 142–157. [Google Scholar] [CrossRef]
- Hopson, L.M.; Lee, E. Mitigating the effect of family poverty on academic and behavioral outcomes: The role of school climate in middle and high school. Child. Youth Serv. Rev. 2011, 33, 2221–2229. [Google Scholar] [CrossRef]
- Levin, K.A.; Currie, C. Reliability and Validity of an Adapted Version of the Cantril Ladder for Use with Adolescent Samples. Soc. Indic. Res. 2014, 119, 1047–1063. [Google Scholar] [CrossRef]
- Mazur, J.; Szkultecka-Dębek, M.; Dzielska, A.; Drozd, M.; Małkowska-Szkutnik, A. What does the Cantril Ladder measure in adolescence? Arch. Med. Sci. 2018, 1, 182–189. [Google Scholar] [CrossRef]
- Pförtner, T.-K.; Günther, S.; Levin, A.K.; Torsheim, T.; Richter, M. The use of parental occupation in adolescent health surveys. An application of ISCO-based measures of occupational status. J. Epidemiol. Community Health 2015, 69, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.; The International HBSC Study Group; Freeman, J.; Samdal, O.; Schnohr, C.W.; De Looze, M.E.; Nic Gabhainn, S.; Iannotti, R.; Rasmussen, M. The Health Behaviour in School-aged Children (HBSC) study: Methodological developments and current tensions. Int. J. Public Health 2009, 54, 140–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ungar, M. The Social Ecology of Resilience A Handbook of Theory and Practice; Springer: London, UK, 2012. [Google Scholar]
- Pakenham, I.K.; Bursnall, S. Relations between social support, appraisal and coping and both positive and negative outcomes for children of a parent with multiple sclerosis and comparisons with children of healthy parents. Clin. Rehabil. 2006, 20, 709–723. [Google Scholar] [CrossRef] [PubMed]
- Krattenmacher, T.; Kühne, F.; Halverscheid, S.; Wiegand-Grefe, S.; Bergelt, C.; Romer, G.; Möller, B. A comparison of the emotional and behavioral problems of children of patients with cancer or a mental disorder and their association with parental quality of life. J. Psychosom. Res. 2014, 76, 213–220. [Google Scholar] [CrossRef]
- Assary, E.; Vincent, J.P.; Keers, R.; Pluess, M. Gene-environment interaction and psychiatric disorders: Review and future directions. Semin. Cell Dev. Biol. 2018, 77, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Henderson, C.; Thornicroft, G. Stigma and discrimination in mental illness: Time to Change. Lancet 2009, 373, 1928–1930. [Google Scholar] [CrossRef]
- Pakenham, K.I.; Cox, S. The nature of caregiving in children of a parent with multiple sclerosis from multiple sources and the associations between caregiving activities and youth adjustment overtime. Psychol. Health 2012, 27, 324–346. [Google Scholar] [CrossRef] [Green Version]
- Kallander, E.K.; Weimand, B.M.; Becker, S.; Van Roy, B.; Hanssen-Bauer, K.; Stavnes, K.; Faugli, A.; Kufås, E.; Ruud, T. Children with ill parents: Extent and nature of caring activities. Scand. J. Caring Sci. 2017, 32, 793–804. [Google Scholar] [CrossRef] [Green Version]
- Shen, H.; Magnusson, C.; Rai, D.; Lundberg, M.; Lê-Scherban, F.; Dalman, C.; Lee, B.K. Associations of Parental Depression With Child School Performance at Age 16 Years in Sweden. JAMA Psychiatry 2016, 73, 239–246. [Google Scholar] [CrossRef] [Green Version]
- Abraham, K.; Aldridge, J. Who Cares About Me? Manchester: Manchester, UK, 2010. [Google Scholar]
- Ireland, M.J.; Pakenham, K.I. Youth adjustment to parental illness or disability: The role of illness characteristics, caregiving, and attachment. Psychol. Health Med. 2010, 15, 632–645. [Google Scholar] [CrossRef]
- Hagen, K.A.; Hilsen, M.; Kallander, E.K.; Ruud, T. Health-related quality of life (HRQoL) in children of ill or substance abusing parents: Examining factor structure and sub-group differences. Qual. Life Res. 2018, 28, 1063–1073. Available online: http://dx.doi.org/10.1007/s11136-018-2067-1 (accessed on 25 December 2021). [CrossRef] [PubMed]
- Kallander, E.K.; Weimand, B.M.; Hanssen-Bauer, K.; Van Roy, B.; Ruud, T. Factors associated with quality of life for children affected by parental illness or substance abuse. Scand. J. Caring Sci. 2020, 35, 405–419. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/scs.12868 (accessed on 25 December 2021). [CrossRef] [PubMed]
| No Ill Parents | Physically Ill Parent(s), No Functional Impairment | Physically Ill Parent, Functionally Impaired | Mentally Ill Parent | Multiple Ill Parents | p1 | |
|---|---|---|---|---|---|---|
| Total (% (N)) | 85.1 (8141) | 7.2 (688) | 3.4 (325) | 2.9 (282) | 1.4 (129) | |
| Age (mean (SD)) | 16.9 (1.45) | 16.9 (1.40) | 17.2 (1.59) | 17.0 (1.67) | 17.4 (1.61) | <0.0001 |
| Age range | 12–26 | 12–25 | 12–26 | 13–26 | 13–25 | |
| Age 95% quantile | 19 | 19 | 19 | 20 | 19 | |
| Gender (% female) | 55.3 | 63.8 | 68.6 | 74.6 | 81.4 | <0.0001 |
| Family socioeconomic position (%) | <0.0001 | |||||
| High | 47.7 | 42.0 | 34.5 | 34.4 | 19.4 | |
| Medium | 29.9 | 33.0 | 28.6 | 29.8 | 27.9 | |
| Low | 6.5 | 11.3 | 19.1 | 13.1 | 30.2 | |
| Students/missing/ unclassifiable | 15.9 | 13.7 | 17.9 | 22.7 | 22.5 | |
| Own physical illness (%) | 30.9 | 41.7 | 48.3 | 43.6 | 54.3 | <0.0001 |
| Own mental/behavioural illness (%) | 18.1 | 21.5 | 22.8 | 35.8 | 53.5 | <0.0001 |
| I can trust my teachers (% neither agree nor disagree/disagree/strongly disagree | 40.0 | 37.5 | 45.9 | 51.1 | 49.6 | <0.0001 |
| Satisfied with academic support from teachers (% neither agree nor disagree/disagree/strongly disagree) | 32.7 | 32.3 | 37.9 | 35.1 | 41.9 | 0.0803 |
| I feels I am part of the classroom community (% sometimes/seldom or never/there is no community) | 16.1 | 18.2 | 24.9 | 28.0 | 31.8 | <0.0001 |
| Low life satisfaction (%) | 16.9 | 20.8 | 29.2 | 37.9 | 47.3 | <0.0001 |
| Crude OR (95% CI) | Adjusted OR 1 (95% CI) | |
|---|---|---|
| Parental illness | ||
| No ill parents | 1.00 (ref.) | 1.00 (ref.) |
| Physically ill parent(s), no functional impairment | 1.27 (1.04–1.54) | 1.20 (0.98–1.46) |
| Physically ill parent, functional impairment | 1.98 (1.54–2.53) | 1.70 (1.32–2.20) |
| Mentally ill parent | 2.98 (2.32–3.83) | 2.60 (1.99–3.31) |
| Multiple ill parents | 3.98 (2.79–5.69) | 3.05 (2.12–4.38) |
| I can trust my teachers | ||
| Strongly agree/agree | 1.00 (ref.) | 1.00 (ref.) |
| Neither agree nor disagree/disagree/strongly disagree | 2.28 (2.05–2.54) | 2.13 (1.91–2.37) |
| Satisfied with academic support from teachers | ||
| Neither agree nor disagree/disagree/strongly disagree | 1.00 (ref.) | 1.00 (ref.) |
| Strongly agree/agree | 1.53 (1.37–1.70) | 1.44 (1.29–1.61) |
| I feel I am part of the classroom community | ||
| Always/most of the time | 1.00 (ref.) | 1.00 (ref.) |
| Sometimes/ seldom or never/there is no community | 4.25 (3.78–4.79) | 3.91 (3.47–4.41) |
| % (n) | Adjusted OR 1 (95% CI) | Type III Test, p | |
|---|---|---|---|
| Talked to student counsellor, N = 9280 | <0.0001 | ||
| No ill parents | 17.1 (1342) | 1.00 (ref.) | |
| Physically ill parent(s), no functional impairment | 20.6 (141) | 1.26 (1.03–1.54) | |
| Physically ill parent, functional impairment | 28.6 (92) | 1.74 (1.34–2.26) | |
| Mentally ill parent | 35.7 (99) | 2.52 (1.94–3.29) | |
| Multiple ill parents | 38.3 (49) | 2.42 (1.65–3.54) | |
| Among students who talked to a student counsellor, N = 1725 | |||
| Strongly agree/agree that it was helpful | 0.31 | ||
| No ill parents | 61.2 (820) | 1.00 (ref.) | |
| Physically ill parent(s), no functional impairment | 61.4 (86) | 1.03 (0.72–1.48) | |
| Physically ill parent, functional impairment | 51.1 (47) | 0.71 (0.46–1.09) | |
| Mentally ill parent | 67.7 (67) | 1.36 (0.89–2.12) | |
| Multiple ill parents | 59.2 (29) | 1.01 (0.56–1.82) | |
| Among students who did not talk to a student counsellor, N = 7478 | |||
| Wish to talk to a student counsellor | 0.0003 | ||
| No ill parents | 8.8 (565) | 1.00 (ref.) | |
| Physically ill parent(s), no functional impairment | 6.3 (34) | 0.69 (0.48–1.00) | |
| Physically ill parent, functional impairment | 9.7 (22) | 1.14 (0.72–1.81) | |
| Mentally ill parent | 11.8 (21) | 1.52 (0.94–2.46) | |
| Multiple ill parents | 21.8 (17) | 3.04 (1.69–5.46) | |
| Do not know if they wish to talk to a student counsellor | 0.32 | ||
| No ill parents | 23.6 (1523) | 1.00 (ref.) | |
| Physically ill parent(s), no functional impairment | 22.4 (120) | 0.86 (0.69–1.06) | |
| Physically ill parent, functional impairment | 24.3 (55) | 0.96 (0.70–1.32) | |
| Mentally ill parent | 30.3 (54) | 1.31 (0.93–1.84) | |
| Multiple ill parents | 23.1 (18) | 1.00 (0.57–1.75) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jørgensen, S.E.; Thygesen, L.C.; Andersen, A.; Due, P.; Michelsen, S.I. Parental Illness and Life Satisfaction among Young People: A Cross-Sectional Study of the Importance of School Factors. Int. J. Environ. Res. Public Health 2022, 19, 2719. https://doi.org/10.3390/ijerph19052719
Jørgensen SE, Thygesen LC, Andersen A, Due P, Michelsen SI. Parental Illness and Life Satisfaction among Young People: A Cross-Sectional Study of the Importance of School Factors. International Journal of Environmental Research and Public Health. 2022; 19(5):2719. https://doi.org/10.3390/ijerph19052719
Chicago/Turabian StyleJørgensen, Sanne Ellegård, Lau Caspar Thygesen, Anette Andersen, Pernille Due, and Susan Ishøy Michelsen. 2022. "Parental Illness and Life Satisfaction among Young People: A Cross-Sectional Study of the Importance of School Factors" International Journal of Environmental Research and Public Health 19, no. 5: 2719. https://doi.org/10.3390/ijerph19052719







