The Protective Role of Self-Compassion in the Relationship between Perfectionism and Burnout in Portuguese Medicine and Dentistry Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure and Participants
2.2. Measures
2.2.1. Perfectionism
2.2.2. Burnout
2.2.3. Self-Compassion
2.3. Data Analysis
3. Results
3.1. Descriptive and Correlation Analysis
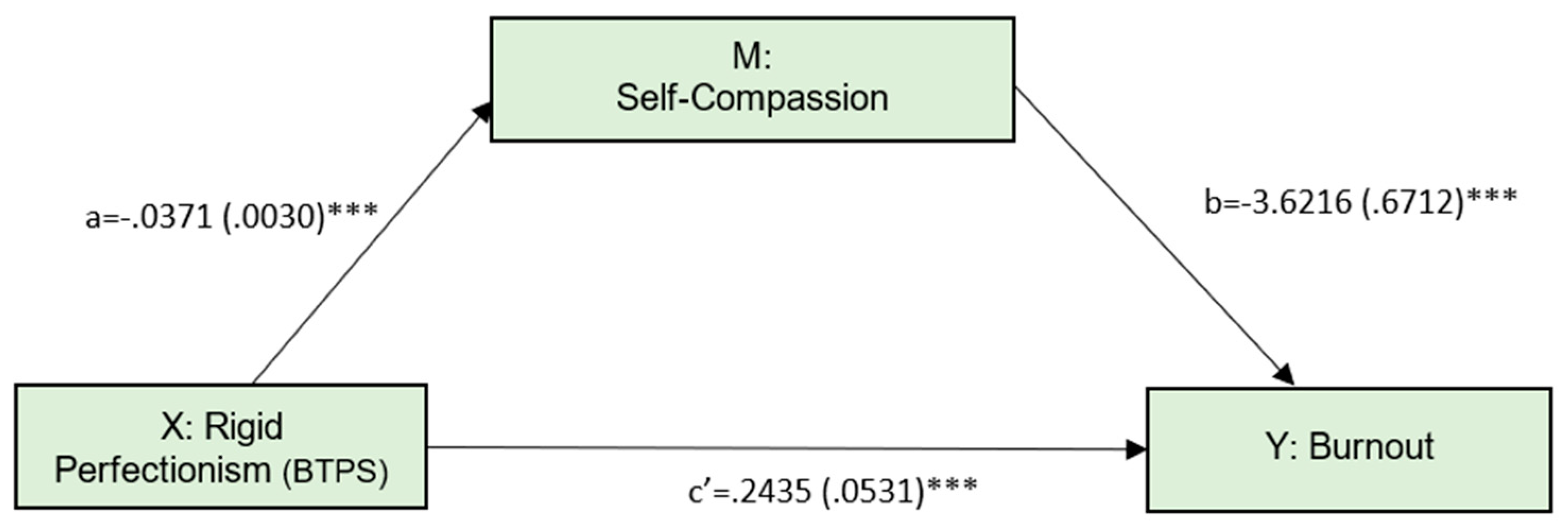
3.2. Mediation Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, A.P.; Curran, T. Multidimensional Perfectionism and Burnout: A Meta-Analysis. Personal. Soc. Psychol. Rev. 2016, 20, 269–288. [Google Scholar] [CrossRef] [PubMed]
- Freudenberger, H.J. Staff burn-out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- LoboPrabhu, S.; Summers, R.F.; Moffic, H.S. Understanding Burnout and its Potential Effects on Clinical Care. In Combating Physician Burnout: A Guide for Psychiatrists; American Psychiatric Pub.: Washington, DC, USA, 2019; pp. 65–84. ISBN 978-1-61537-227-0. [Google Scholar]
- Moffic, H.S.; Levin, R.M.; Rouse, H. The History of Burnout in Society, Medicine, and Psychiatry. In Combating Physician Burnout: A Guide for Psychiatrists; American Psychiatric Pub.: Washington, DC, USA, 2019; pp. 3–26. ISBN 978-1-61537-227-0. [Google Scholar]
- Frajerman, A.; Morvan, Y.; Krebs, M.O.; Gorwood, P.; Chaumette, B. Burnout in medical students before residency: A systematic review and meta-analysis. Eur. Psychiatry 2019, 55, 36–42. [Google Scholar] [CrossRef]
- Boyards, L.; Gullie, C. Burnout among Medical Students and Residents. In Combating Physician Burnout: A Guide for Psychiatrists; American Psychiatric Pub.: Washington, DC, USA, 2019; pp. 193–209. ISBN 978-1-61537-227-0. [Google Scholar]
- Collin, V.; Toon, M.; O’Selmo, E.; Reynolds, L.; Whitehead, P. A survey of stress, burnout and well-being in UK dentists. Br. Dent. J. 2019, 226, 40–49. [Google Scholar] [CrossRef]
- Kwak, E.-J.; Ji, Y.-A.; Baek, S.-H.; Baek, Y.S. High levels of burnout and depression in a population of senior dental students in a school of dentistry in Korea. J. Dent. Sci. 2021, 16, 65–70. [Google Scholar] [CrossRef]
- Picton, A. Work-life balance in medical students: Self-care in a culture of self-sacrifice. BMC Med. Educ. 2021, 21, 8. [Google Scholar] [CrossRef]
- Jackson, E.R.; Shanafelt, T.D.; Hasan, O.; Satele, D.V.; Dyrbye, L.N. Burnout and alcohol abuse/dependence among U.S. Medical Students. Acad. Med. 2016, 91, 1251–1256. [Google Scholar] [CrossRef]
- Lebensohn, P.; Dodds, S.; Benn, R.; Brooks, A.J.; Birch, M. Resident wellness behaviors. Fam. Med. 2013, 45, 541–549. [Google Scholar]
- Van der Heijden, F.; Dillingh, G.; Bakker, A.; Prins, J. Suicidal thoughts among medical residents with burnout. Arch. Suicide Res. 2008, 12, 344–346. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; Thomas, M.R.; Massie, F.S.; Power, D.V.; Eacker, A.; Harper, W.; Durning, S.; Moutier, C.; Szydlo, D.W.; Novotny, P.J.; et al. Burnout and Suicidal Ideation among U.S. Medical Students. Ann. Intern. Med. 2008, 136, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Slavin, S.J. Medical Student Mental Health. JAMA J. Am. Med. Assoc. 2016, 316, 2214–2236. [Google Scholar] [CrossRef]
- Guthrie, E.; Black, D.; Creed, F.; Shaw, C. Stress and Burnout in Medical Students. J. R. Soc. Med. 1998, 91, 237–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, E.S.; Konrad, T.R. Suboptimal patient care: Results from the MEMO study. Health Care Manag. Rev. 2007, 32, 203–212. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Huschka, M.M.; Novotny, P.J.; Sloan, J.A.; Kolars, J.C.; Habermann, T.M.; Shanafelt, T.D. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. J. Am. Med. Assoc. 2006, 296, 1071–1078. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dyrbye, L.N.; Massie, F.S.; Eacker, A.; Harper, W.; Power, D.; Durning, S.J.; Thomas, M.R.; Moutier, C.; Satele, D.; Sloan, J.; et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA J. Am. Med. Assoc. 2010, 304, 1173–1180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, M.R.; Dyrbye, L.N.; Huntington, J.L.; Lawson, K.L.; Novotny, P.J.; Sloan, J.A.; Shanafelt, T.D. How do distress and well-being relate to medical student empathy? A multicenter study. J. Gen. Intern. Med. 2007, 22, 177–183. [Google Scholar] [CrossRef] [Green Version]
- Kelm, Z.; Womer, J.; Walter, J.K.; Feudtner, C. Interventions to cultivate physician empathy: A systematic review. BMC Med. Educ. 2014, 14, 219. [Google Scholar] [CrossRef] [Green Version]
- Trzeciak, S.; Mazzarelli, A.; Booker, C. Compassionomics: The Revolutionary Scientific Evidence That Caring Makes a Difference; Studer Group: Pensacola, FL, USA, 2019; ISBN 1622181069. [Google Scholar]
- Moir, F.; Yielder, J.; Sanson, J.; Chen, Y. Depression in medical students: Current insights. Adv. Med. Educ. Pract. 2018, 9, 323–333. [Google Scholar] [CrossRef] [Green Version]
- Dyrbye, L.N.; Thomas, M.R.; Harper, W.; Massie, F.S.; Power, D.V.; Eacker, A.; Szydlo, D.W.; Novotny, P.J.; Sloan, J.A.; Shanafelt, T.D. The learning environment and medical student burnout: A multicentre study. Med. Educ. 2009, 43, 274–282. [Google Scholar] [CrossRef]
- Mian, A.; Kim, D.; Chen, D.; Ward, W.L. Medical Student and Resident Burnout: A Review of Causes, Effects, and Prevention. J. Fam. Med. Dis. Prev. 2018, 4, 10–17. [Google Scholar] [CrossRef]
- Papapanou, M.; Routsi, E.; Tsamakis, K.; Fotis, L.; Marinos, G.; Lidoriki, I.; Karamanou, M.; Papaioannou, T.G.; Tsiptsios, D.; Smyrnis, N.; et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad. Med. J. 2021, 1–7. [Google Scholar] [CrossRef]
- Farrokhi, F.; Mohebbi, S.Z.; Farrokhi, F.; Khami, M.R. Impact of COVID-19 on dental education—A scoping review. BMC Med. Educ. 2021, 21, 587. [Google Scholar] [CrossRef] [PubMed]
- Vala, N.; Vachhani, M.; Sorani, A. Study of anxiety, stress, and depression level among medical students during COVID-19 pandemic phase in Jamnagar city. Natl. J. Physiol. Pharm. Pharmacol. 2020, 10, 1. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Pereira, A.T.; Cabaços, C.; Araújo, A.; Amaral, A.P.; Carvalho, F.; Macedo, A. COVID-19 psychological impact: The role of perfectionism. Pers. Ind. Diff. 2021, 184, 111160. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Corrigendum to “Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis” [Brain Behav. Immun. 88 (2020) 901–907] (Brain Behavior and Immunity (2020) 88 (901–907). Brain. Behav. Immun. 2021, 92, 247. [Google Scholar] [CrossRef]
- Li, Y.; Wang, A.; Wu, Y.; Han, N.; Huang, H. Impact of the COVID-19 Pandemic on the Mental Health of College Students: A Systematic Review and Meta-Analysis. Front. Psychol. 2021, 12, 669119. [Google Scholar] [CrossRef]
- Lasheras, I.; Gracia-García, P.; Lipnicki, D.M.; Bueno-Notivol, J.; López-Antón, R.; de la Cámara, C.; Lobo, A.; Santabárbara, J. Prevalence of anxiety in medical students during the COVID-19 pandemic: A rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 6603. [Google Scholar] [CrossRef]
- Pereira, A.T.; Cabaços, C.; Araújo, A.; Soares, M.J.; Brito, M.J.; Carvalho, F.; Mota, D.; Bajouco, M.; Madeira, N.; Carneiro, M.; et al. COVID-19 Pandemic: Another Source of Stress for Medical Students. Eur. Psychiatry, 2022, accepted.
- Zis, P.; Artemiadis, A.; Bargiotas, P.; Nteveros, A.; Hadjigeorgiou, G.M. Medical studies during the COVID-19 pandemic: The impact of digital learning on medical students’ Burnout and mental health. Int. J. Environ. Res. Public Health 2021, 18, 349. [Google Scholar] [CrossRef] [PubMed]
- Jezzini-Martinez, S.; Quiroga-Garza, A.; Jacobo-Baca, G.; Guzman-Lopez, S.; Salinas-Alvarez, Y.; Martinez-Garza, J.; Zarate-Garza, P.; de la Fuente-Villarreal, D.; Elizondo-Omaña, R. COVID-19 Causing Burnout Among Medical Students. FASEB J. 2021, 35. [Google Scholar] [CrossRef]
- Chi, D.L.; Randall, C.L.; Hill, C.M. Dental trainees’ mental health and intention to leave their programs during the COVID-19 pandemic. J. Am. Dent. Assoc. 2021, 152, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Al-Rawi, N.H.; Yacoub, A.; Zaouali, A.; Salloum, L.; Afash, N.; Shazli, O.A.; Elyan, Z. Prevalence of Burnout among Dental Students during COVID-19 Lockdown in UAE. J. Contemp. Dent. Pract. 2021, 22, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Myers, M.F.; Gabbard, G.O. The Physician as Patient: A Clinical Handbook for Mental Health Professionals; American Psychiatric Pub.: Washington, DC, USA, 2008; ISBN 1585623121. [Google Scholar]
- Mayer, L.E.S. From Burnout to Impairment: The Slippery Slope. In Combating Physician Burnout: A Guide for Psychiatrists; American Psychiatric Pub.: Washington, DC, USA, 2019; pp. 85–100. ISBN 978-1-61537-227-0. [Google Scholar]
- Flett, G.L.; Hewitt, P.L.; Nepon, T.; Besser, A. Perfectionism cognition theory: The cognitive side of perfectionism. In The Psychology of Perfectionism; Routledge: London, UK, 2017; pp. 89–110. ISBN 1315536250. [Google Scholar]
- Dunkley, D.M.; Zuroff, D.C.; Blankstein, K.R. Self-Critical Perfectionism and Daily Affect: Dispositional and Situational Influences on Stress and Coping. J. Pers. Soc. Psychol. 2003, 84, 234–252. [Google Scholar] [CrossRef]
- Beauregard, T.A. Predicting interference between work and home: A comparison of dispositional and situational antecedents. J. Manag. Psychol. 2006, 21, 244–264. [Google Scholar] [CrossRef] [Green Version]
- Stoeber, J.; Stoeber, F.S. Domains of perfectionism: Prevalence and relationships with perfectionism, gender, age, and satisfaction with life. Pers. Individ. Differ. 2009, 46, 530–535. [Google Scholar] [CrossRef] [Green Version]
- Macedo, A.; Pereira, A.T.; Marques, M.; Soares, M.J.; Valente, J.; Nogueira, V.; Azevedo, M.H. P-931-The portuguese version of the domains of perfectionism scale. Eur. Psychiatry 2012, 27, 1. [Google Scholar] [CrossRef]
- Dunn, J.C.; Whelton, W.J.; Sharpe, D. Maladaptive perfectionism, hassles, coping, and psychological distress in university professors. J. Couns. Psychol. 2006, 53, 511. [Google Scholar] [CrossRef]
- Flett, G.L.; Hewitt, P.L. Perfectionism: Theory, research, and treatment; American Psychological Association: Washington, DC, USA, 2002. [Google Scholar]
- Macedo, A.; Soares, M.J.; Amaral, A.P.; Nogueira, V.; Madeira, N.; Roque, C.; Marques, M.; Maia, B.; Bos, S.; Valente, J. Repetitive negative thinking mediates the association between perfectionism and psychological distress. Pers. Individ. Differ. 2015, 72, 220–224. [Google Scholar] [CrossRef]
- Macedo, A.; Marques, C.; Quaresma, V.; Soares, M.J.; Amaral, A.P.; Araújo, A.I.; Pereira, A.T. Are perfectionism cognitions and cognitive emotion regulation strategies mediators between perfectionism and psychological distress? Pers. Individ. Differ. 2017, 119, 46–51. [Google Scholar] [CrossRef]
- Yu, J.H.; Chae, S.J.; Chang, K.H. The relationship among self-efficacy, perfectionism and academic burnout in medical school students. Korean J. Med. Educ. 2016, 28, 49–55. [Google Scholar] [CrossRef] [Green Version]
- Marques, M.; Macedo, A.; Soares, M.J.; Maia, B.; Pereira, A.T.; Bos, S.; Gomes, A.; Valente, J.; Azevedo, M.H. The premedical syndrome: Does it exist in Portugal? Acta Med. Port. 2009, 22, 789–796. [Google Scholar]
- Madigan, D.J. A Meta-Analysis of Perfectionism and Academic Achievement. Educ. Psychol. Rev. 2019, 31, 967–989. [Google Scholar] [CrossRef] [Green Version]
- Harari, D.; Swider, B.W.; Steed, L.B.; Breidenthal, A.P. Is perfect good? A meta-analysis of perfectionism in the workplace. J. Appl. Psychol. 2018, 103, 1121–1144. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.M.; Saklofske, D.H.; Stoeber, J.; Sherry, S.B. The Big Three Perfectionism Scale: A New Measure of Perfectionism. J. Psychoeduc. Assess. 2016, 34, 670–687. [Google Scholar] [CrossRef]
- Lino, F.; Marques, C.; Pereira, A.T.; Sousa, P.; Amaral, A.P.; Oliveira, P.; Araujo, A.I.; Macedo, A. Confirmatory factor analysis of the big three perfectionism scale in a sample of Portuguese university students. Eur. Psychiatry 2018, 48, S282–S283. [Google Scholar]
- Curran, T.; Hill, A.P. Perfectionism is increasing over time: A meta-analysis of birth cohort differences from 1989 to 2016. Psychol. Bull. 2019, 145, 410. [Google Scholar] [CrossRef] [PubMed]
- Neff, K.D.; Hsieh, Y.-P.; Dejitterat, K. Self-compassion, Achievement Goals, and Coping with Academic Failure. Self Identity 2005, 4, 263–287. [Google Scholar] [CrossRef]
- Hiçdurmaz, D. The Relationship Between Self-Compassion and Multidimensional Perfectionism Levels and Influencing Factors in Nursing Students. J. Psychiatr. Nurs. 2017, 8, 86–94. [Google Scholar] [CrossRef]
- Linnett, R.J.; Kibowski, F. A multidimensional approach to perfectionism and self-compassion. Self Identity 2020, 19, 757–783. [Google Scholar] [CrossRef] [Green Version]
- Tobin, R.; Dunkley, D.M. Self-critical perfectionism and lower mindfulness and self-compassion predict anxious and depressive symptoms over two years. Behav. Res. Ther. 2021, 136, 103780. [Google Scholar] [CrossRef]
- Alaloglu, G.; Bahtiyar, B. The Predictive Roles of Perfectionism, Self-Handicapping and Self-Compassion on Psychological Well-Being. In Psychology Applications & Developments VI; inScience Press: Lisboa, Portugal, 2020; ISBN 9789895481538. [Google Scholar]
- Kemper, K.J.; McClafferty, H.; Wilson, P.M.; Serwint, J.R.; Batra, M.; Mahan, J.D.; Schubert, C.J.; Staples, B.B.; Schwartz, A.; Consortium, P.R.B.-R.S. Do mindfulness and self-compassion predict burnout in pediatric residents? Acad. Med. 2019, 94, 876–884. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Yap, K.; Scott, N.; Einstein, D.A.; Ciarrochi, J. Self-compassion moderates the perfectionism and depression link in both adolescence and adulthood. PLoS ONE 2018, 13, e0192022. [Google Scholar] [CrossRef]
- Abdollahi, A.; Allen, K.A.; Taheri, A. Moderating the Role of Self-Compassion in the Relationship Between Perfectionism and Depression. J. Ration. Emot. Cogn. Behav. Ther. 2020, 38, 459–471. [Google Scholar] [CrossRef]
- Wei, S.; Li, L.; Shi, J.; Liang, H.; Yang, X. Self-compassion mediates the perfectionism and depression link on chinese undergraduates. Ann. Palliat. Med. 2021, 10, 1950–1960. [Google Scholar] [CrossRef]
- Richardson, C.M.E.; Trusty, W.T.; George, K.A. Trainee wellness: Self-critical perfectionism, self-compassion, depression, and burnout among doctoral trainees in psychology. Couns. Psychol. Q. 2020, 33, 187–198. [Google Scholar] [CrossRef]
- Beck, A.R.; Verticchio, H.; Seeman, S.; Milliken, E.; Schaaba, H. A Mindfulness Practice for Communication Sciences and Disorders Undergraduate and Speech-Language Pathology Graduate Students: Effects on Stress, Self-Compassion, and Perfectionism. Am. J. Speech-Lang. Pathol. 2017, 4, 527–534. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Martinez, I.M.; Pinto, A.M.; Salanova, M.; Bakker, A.B. Burnout and engagement in university students: A cross-national study. J. Cross. Cult. Psychol. 2002, 33, 464–481. [Google Scholar] [CrossRef] [Green Version]
- Marôco, J.; Tecedeiro, M. Inventário de burnout de maslach para estudantes portugueses. Psicol. Saúde Doenças 2009, 10, 227–236. [Google Scholar]
- Manão, A.; Carneiro, M.; Carvalho, F.; Barros, M.; Cabaços, C.; Brito, M.J.; Araújo, A.; Azevedo, J.; Marques, M.; Macedo, A.; et al. Maslach Burnout Inventory—Students Survey Validation for Portuguese Medicine Students. In Proceedings of the 21st WPA World Congress of Psychiatry, Virtual, 18–21 October 2021. [Google Scholar]
- Neff, K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity 2003, 2, 85–101. [Google Scholar] [CrossRef] [Green Version]
- Castilho, P.; Pinto-Gouveia, J.; Duarte, J. Evaluating the Multifactor Structure of the Long and Short Versions of the Self-Compassion Scale in a Clinical Sample. J. Clin. Psychol. 2015, 71, 856–870. [Google Scholar] [CrossRef] [Green Version]
- Carvalho, F.; Macedo, A.; Manão, A.; Cabaços, C.; Azevedo, J.; Marques, C.; Marques, M.; Carneiro, M.; Telles, C.D.; Barreto, C.; et al. Further Validation of the Short Form of the Self-Compassion Scale in a sample of Portuguese Medicine Students. Eur. Psychiatry. 2022, accepted.
- Cohen, J. Statistical power analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Hayes, A.F.; Rockwood, N.J. Conditional process analysis: Concepts, computation, and advances in the modeling of the contingencies of mechanisms. Am. Behav. Sci. 2020, 64, 19–54. [Google Scholar] [CrossRef] [Green Version]
- Walburg, V. Burnout among high school students: A literature review. Child. Youth Serv. Rev. 2014, 42, 28–33. [Google Scholar] [CrossRef]
- Smith, M.M.; Vidovic, V.; Sherry, S.B.; Stewart, S.H.; Saklofske, D.H. Are perfectionism dimensions risk factors for anxiety symptoms? A meta-analysis of 11 longitudinal studies. Anxiety Stress Coping 2018, 31, 4–20. [Google Scholar] [CrossRef]
- Seeliger, H.; Harendza, S. Is perfect good?—Dimensions of perfectionism in newly admitted medical students. BMC Med. Educ. 2017, 17, 206. [Google Scholar] [CrossRef] [Green Version]
- Craiovan, P.M. Correlations between Perfectionism, Stress, Psychopathological Symptoms and Burnout in the Medical Field. Procedia Soc. Behav. Sci. 2014, 127, 529–533. [Google Scholar] [CrossRef] [Green Version]
- Sibeoni, J.; Bellon-Champel, L.; Mousty, A.; Manolios, E.; Verneuil, L.; Revah-Levy, A. Physicians’ Perspectives About Burnout: A Systematic Review and Metasynthesis. J. Gen. Intern. Med. 2019, 34, 1578–1590. [Google Scholar] [CrossRef]
- Hewitt, P.L.; Flett, G.L.; Ediger, E. Perfectionism and depression: Longitudinal assessment of a specific vulnerability hypothesis. J. Abnorm. Psychol. 1996, 105, 276–280. [Google Scholar] [CrossRef]
- Chunming, W.M.; Harrison, R.; MacIntyre, R.; Travaglia, J.; Balasooriya, C. Burnout in medical students: A systematic review of experiences in Chinese medical schools. BMC Med. Educ. 2017, 17, 217. [Google Scholar] [CrossRef] [Green Version]
- Stoeber, J. How other-oriented perfectionism differs from self-oriented and socially prescribed perfectionism. J. Psychopathol. Behav. Assess. 2014, 36, 329–338. [Google Scholar] [CrossRef]
- Yarnell, L.M.; Neff, K.D.; Davidson, O.A.; Mullarkey, M. Gender Differences in Self-Compassion: Examining the Role of Gender Role Orientation. Mindfulness 2019, 10, 1136–1152. [Google Scholar] [CrossRef]
- Backović, D.V.; Živojinović, J.I.; Maksimović, J.; Maksimović, M. Gender differences in academic stress and burnout among medical students in final years of education. Psychiatr. Danub. 2012, 24, 175–181. [Google Scholar]
- Smith, M.M.; Saklofske, D.H.; Yan, G. Perfectionism, trait emotional intelligence, and psychological outcomes. Pers. Individ. Differ. 2015, 85, 155–158. [Google Scholar] [CrossRef]
- Yanes, A. The Culture of Perfection: A Barrier to Medical Student Wellness and Development. Acad. Med. 2017, 92, 900–901. [Google Scholar] [CrossRef]
- Kilmen, S.; Arikan, S. The Big Three Perfectionism Scale: Factor Structure and Measurement Invariance in a Turkish Sample. J. Psychoeduc. Assess. 2020, 38, 53–68. [Google Scholar] [CrossRef]
- Flett, G.L.; Sherry, S.B.; Hewitt, P.L.; Nepon, T. Understanding the narcissistic perfectionists among us: Grandiosity, vulnerability, and the quest for the perfect self. In Handbook of Psychology Narcissism: Diverse Perspectives; Nova Science Publishers: Hauppauge, NY, USA, 2014; pp. 43–66. [Google Scholar]
- Schwarzkopf, K.; Straus, D.; Porschke, H.; Znoj, H.; Conrad, N.; Schmidt-Trucksäss, A.; Känel, R. Von Empirical evidence for a relationship between narcissistic personality traits and job burnout. Burn. Res. 2016, 3, 25–33. [Google Scholar] [CrossRef] [Green Version]
- Barnett, M.D.; Flores, J. Narcissus, exhausted: Self-compassion mediates the relationship between narcissism and school burnout. Pers. Individ. Differ. 2016, 97, 102–108. [Google Scholar] [CrossRef]
- James, W. The Principles of Psychology; Harvard University Press: Cambridge, MA, USA, 1983. [Google Scholar]
- Kohut, H. The Analysis of the Self: A Systematic Approach to the Psychoanalytic Treatment of Narcissistic Personality Disorders; University of Chicago Press: Chicago, IL, USA, 2013. [Google Scholar]
- Neff, K.D.; Vonk, R. Self-compassion versus global self-esteem: Two different ways of relating to oneself. J. Pers. 2009, 77, 23–50. [Google Scholar] [CrossRef]
- Nealis, L.J.; Sherry, S.B.; Sherry, D.L.; Stewart, S.H.; Macneil, M.A. Toward a better understanding of narcissistic perfectionism: Evidence of factorial validity, incremental validity, and mediating mechanisms. J. Res. Pers. 2015, 57, 11–25. [Google Scholar] [CrossRef]
- Leary, M.R.; Tate, E.B.; Adams, C.E.; Allen, A.B.; Hancock, J. Self-compassion and reactions to unpleasant self-relevant events: The implications of treating oneself kindly. J. Pers. Soc. Psychol. 2007, 92, 887–904. [Google Scholar] [CrossRef] [Green Version]
- Beaumont, E.; Durkin, M.; Hollins Martin, C.J.; Carson, J. Compassion for others, self-compassion, quality of life and mental well-being measures and their association with compassion fatigue and burnout in student midwives: A quantitative survey. Midwifery 2016, 34, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Dev, V.; Fernando, A.T.; Lim, A.G.; Consedine, N.S. Does self-compassion mitigate the relationship between burnout and barriers to compassion? A cross-sectional quantitative study of 799 nurses. Int. J. Nurs. Stud. 2018, 81, 81–88. [Google Scholar] [CrossRef]
- Hashem, Z.; Zeinoun, P. Self-Compassion Explains Less Burnout Among Healthcare Professionals. Mindfulness 2020, 11, 2542–2551. [Google Scholar] [CrossRef] [PubMed]
- Joeng, J.R.; Turner, S.L. Mediators between self-criticism and depression: Fear of compassion, self-compassion, and importance to others. J. Couns. Psychol. 2015, 62, 453–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilbert, P.; Procter, S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clin. Psychol. Psychother. 2006, 13, 353–379. [Google Scholar] [CrossRef]
- Beaumont, E.; Irons, C.; Rayner, G.; Dagnall, N. Does compassion-focused therapy training for health care educators and providers increase self-compassion and reduce self-persecution and self-criticism? J. Contin. Educ. Health Prof. 2016, 36, 4–10. [Google Scholar] [CrossRef]
- Halamová, J.; Jurková, V.; Kanovský, M.; Kupeli, N. Effect of a Short-Term Online Version of a Mindfulness-Based Intervention on Self-criticism and Self-compassion in a Nonclinical Sample. Stud. Psychol. 2018, 60, 259–273. [Google Scholar] [CrossRef]


| 2 | 3 | 4 | 5 | Mean | SD | α | |
|---|---|---|---|---|---|---|---|
| 1 SCritPerf | 0.75 ** | 0.31 ** | −0.68 ** | 0.42 ** | 570.02 | 140.17 | 0.86 |
| 2 RigPerf | 1 | 0.46 ** | −0.47 ** | 0.32 ** | 270.10 | 80.93 | 0.85 |
| 3 NarcPerf | 1 | −0.17 ** | 0.13 ** | 300.88 | 90.11 | 0.85 | |
| 4 Self-Comp | 1 | −0.34 ** | 20.90 | 0.71 | 0.73 | ||
| 5 Burnout | 1 | 400.68 | 100.43 | 0.73 |
| Bootstrapping BC 95% CI | ||||||
|---|---|---|---|---|---|---|
| MODEL | Coefficient | SE | p | Lower | Upper | |
| 1 | PREDICTOR: Self-critical perfectionism | |||||
| Covariate: Gender | Direct effect c′ | 0.2608 | 0.0401 | <0.001 | 0.1820 | 3395 |
| Indirect effect c | 0.0532 | 0.0255 | 0.0029 | 0.1030 | ||
| 2 | PREDICTOR: Rigid perfectionism | |||||
| Direct effect c′ | 0.2435 | 0.0531 | <0.001 | 0.1392 | 0.3479 | |
| Indirect effect c | 0.1343 | 0.0258 | 0.0859 | 0.1868 | ||
| 3 | PREDICTOR: Narcissistic perfectionism | |||||
| Direct effect c′ | 0.0849 | 0.0475 | 0.0747 | −0.0085 | 0.1782 | |
| Indirect effect c | 0.0654 | 0.0168 | 0.0332 | 0.0989 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira, A.T.; Brito, M.J.; Cabaços, C.; Carneiro, M.; Carvalho, F.; Manão, A.; Araújo, A.; Pereira, D.; Macedo, A. The Protective Role of Self-Compassion in the Relationship between Perfectionism and Burnout in Portuguese Medicine and Dentistry Students. Int. J. Environ. Res. Public Health 2022, 19, 2740. https://doi.org/10.3390/ijerph19052740
Pereira AT, Brito MJ, Cabaços C, Carneiro M, Carvalho F, Manão A, Araújo A, Pereira D, Macedo A. The Protective Role of Self-Compassion in the Relationship between Perfectionism and Burnout in Portuguese Medicine and Dentistry Students. International Journal of Environmental Research and Public Health. 2022; 19(5):2740. https://doi.org/10.3390/ijerph19052740
Chicago/Turabian StylePereira, Ana Telma, Maria João Brito, Carolina Cabaços, Mário Carneiro, Frederica Carvalho, Andreia Manão, Ana Araújo, Daniela Pereira, and António Macedo. 2022. "The Protective Role of Self-Compassion in the Relationship between Perfectionism and Burnout in Portuguese Medicine and Dentistry Students" International Journal of Environmental Research and Public Health 19, no. 5: 2740. https://doi.org/10.3390/ijerph19052740







