An Exploratory Study on the Physical Activity Health Paradox—Musculoskeletal Pain and Cardiovascular Load during Work and Leisure in Construction and Healthcare Workers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Independent Variable: Composition of Physical Activity during Work and Leisure
2.2. Dependent Variable: Overall Musculoskeletal Pain
2.3. Additional Descriptive Information
2.4. Data Analyses
2.5. Visualization of the Regression Analyses
3. Results
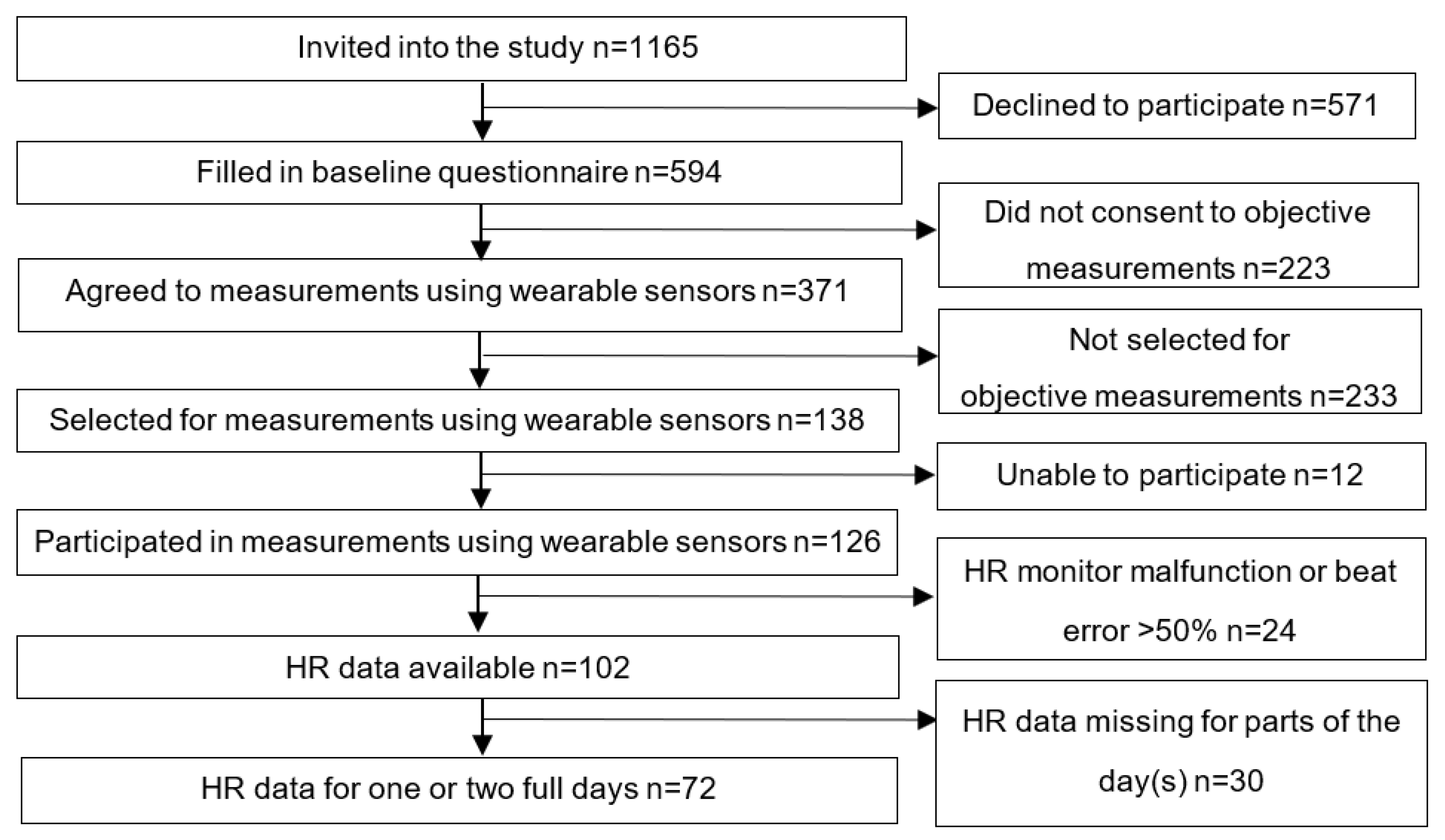
3.1. Sample Characteristics
3.2. Exposure Compositions
3.3. Physical Activity in Relation to Overall Musculoskeletal Pain
4. Discussion
4.1. Strengths and Weaknesses
4.2. Interpretation of the Findings
4.3. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Holtermann, A.; Hansen, J.V.; Burr, H.; Sogaard, K.; Sjogaard, G. The health paradox of occupational and leisure-time physical activity. Br. J. Sports Med. 2012, 46, 291–295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cillekens, B.; Huysmans, M.A.; Holtermann, A.; van Mechelen, W.; Straker, L.; Krause, N.; van der Beek, A.J.; Coenen, P. Physical activity at work may not be health enhancing. A systematic review with meta-analysis on the association between occupational physical activity and cardiovascular disease mortality covering 23 studies with 655,892 participants. Scand. J. Work Environ. Health 2021. [Google Scholar] [CrossRef] [PubMed]
- Cillekens, B.; Lang, M.; van Mechelen, W.; Verhagen, E.; Huysmans, M.A.; Holtermann, A.; van der Beek, A.J.; Coenen, P. How does occupational physical activity influence health? An umbrella review of 23 health outcomes across 158 observational studies. Br. J. Sports Med. 2020, 54, 1474–1481. [Google Scholar] [CrossRef]
- Li, J.; Loerbroks, A.; Angerer, P. Physical activity and risk of cardiovascular disease: What does the new epidemiological evidence show? Curr. Opin. Cardiol. 2013, 28, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Rana, B.; Hu, L.; Harper, A.; Cao, C.; Peters, C.; Brenner, D.; Yang, L. Occupational Physical Activity and Lung Cancer Risk: A Systematic Review and Meta-Analysis. Sports Med. 2020, 50, 1637–1651. [Google Scholar] [CrossRef]
- Coenen, P.; Huysmans, M.A.; Holtermann, A.; Krause, N.; van Mechelen, W.; Straker, L.M.; van der Beek, A.J. Do highly physically active workers die early? A systematic review with meta-analysis of data from 193,696 participants. Br. J. Sports Med. 2018, 52, 1320–1326. [Google Scholar] [CrossRef] [Green Version]
- Ezzatvar, Y.; Calatayud, J.; Andersen, L.L.; Casana, J. Are Moderate and Vigorous Leisure-Time Physical Activity Associated with Musculoskeletal Pain? A Cross-Sectional Study among 981 Physical Therapists. Am. J. Health Promot. 2020, 34, 67–70. [Google Scholar] [CrossRef]
- Andersen, L.L.; Christensen, K.B.; Holtermann, A.; Poulsen, O.M.; Sjogaard, G.; Pedersen, M.T.; Hansen, E.A. Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: A one-year randomized controlled trial. Man. Ther. 2010, 15, 100–104. [Google Scholar] [CrossRef]
- Searle, A.; Spink, M.; Ho, A.; Chuter, V. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin. Rehabil. 2015, 29, 1155–1167. [Google Scholar] [CrossRef]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 4, CD011279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hallman, D.M.; Birk Jorgensen, M.; Holtermann, A. Objectively measured physical activity and 12-month trajectories of neck-shoulder pain in workers: A prospective study in DPHACTO. Scand. J. Public Health 2017, 45, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Lotters, F.; Burdorf, A.; Kuiper, J.; Miedema, H. Model for the work-relatedness of low-back pain. Scand. J. Work Environ. Health 2003, 29, 431–440. [Google Scholar] [CrossRef] [Green Version]
- Coenen, P.; Gouttebarge, V.; van der Burght, A.S.; van Dieen, J.H.; Frings-Dresen, M.H.; van der Beek, A.J.; Burdorf, A. The effect of lifting during work on low back pain: A health impact assessment based on a meta-analysis. Occup. Environ. Med. 2014, 71, 871–877. [Google Scholar] [CrossRef] [Green Version]
- Hulshof, C.T.J.; Pega, F.; Neupane, S.; Colosio, C.; Daams, J.G.; Kc, P.; Kuijer, P.; Mandic-Rajcevic, S.; Masci, F.; van der Molen, H.F.; et al. The effect of occupational exposure to ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 150, 106349. [Google Scholar] [CrossRef]
- Holtermann, A.; Straker, L.; Lee, I.M.; van der Beek, A.J.; Stamatakis, E. Long overdue remarriage for better physical activity advice for all: Bringing together the public health and occupational health agendas. Br. J. Sports Med. 2020, 54, 1377–1378. [Google Scholar] [CrossRef] [PubMed]
- Korshoj, M.; Krustrup, P.; Jespersen, T.; Sogaard, K.; Skotte, J.H.; Holtermann, A. A 24-h assessment of physical activity and cardio-respiratory fitness among female hospital cleaners: A pilot study. Ergonomics 2013, 56, 935–943. [Google Scholar] [CrossRef]
- Holtermann, A.; Krause, N.; van der Beek, A.J.; Straker, L. The physical activity paradox: Six reasons why occupational physical activity (OPA) does not confer the cardiovascular health benefits that leisure time physical activity does. Br. J. Sports Med. 2018, 52, 149–150. [Google Scholar] [CrossRef] [Green Version]
- Webb, H.E.; Weldy, M.L.; Fabianke-Kadue, E.C.; Orndorff, G.R.; Kamimori, G.H.; Acevedo, E.O. Psychological stress during exercise: Cardiorespiratory and hormonal responses. Eur. J. Appl. Physiol. 2008, 104, 973–981. [Google Scholar] [CrossRef]
- Lang, J.; Ochsmann, E.; Kraus, T.; Lang, J.W. Psychosocial work stressors as antecedents of musculoskeletal problems: A systematic review and meta-analysis of stability-adjusted longitudinal studies. Soc. Sci. Med. 2012, 75, 1163–1174. [Google Scholar] [CrossRef] [PubMed]
- Taibi, Y.; Metzler, Y.A.; Bellingrath, S.; Muller, A. A systematic overview on the risk effects of psychosocial work characteristics on musculoskeletal disorders, absenteeism, and workplace accidents. Appl. Ergon. 2021, 95, 103434. [Google Scholar] [CrossRef]
- Hallman, D.M.; Mathiassen, S.E.; van der Beek, A.J.; Jackson, J.A.; Coenen, P. Calibration of Self-Reported Time Spent Sitting, Standing and Walking among Office Workers: A Compositional Data Analysis. Int. J. Environ. Res. Public Health 2019, 16, 3111. [Google Scholar] [CrossRef] [Green Version]
- Koch, M.; Lunde, L.K.; Gjulem, T.; Knardahl, S.; Veiersted, K.B. Validity of Questionnaire and Representativeness of Objective Methods for Measurements of Mechanical Exposures in Construction and Health Care Work. PLoS ONE 2016, 11, e0162881. [Google Scholar] [CrossRef]
- White, R.L.; Parker, P.D.; Lubans, D.R.; MacMillan, F.; Olson, R.; Astell-Burt, T.; Lonsdale, C. Domain-specific physical activity and affective wellbeing among adolescents: An observational study of the moderating roles of autonomous and controlled motivation. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 87. [Google Scholar] [CrossRef]
- Gupta, N.; Dencker-Larsen, S.; Lund Rasmussen, C.; McGregor, D.; Rasmussen, C.D.N.; Thorsen, S.V.; Jorgensen, M.B.; Chastin, S.; Holtermann, A. The physical activity paradox revisited: A prospective study on compositional accelerometer data and long-term sickness absence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 93. [Google Scholar] [CrossRef]
- Hallman, D.M.; Gupta, N.; Bergamin Januario, L.; Holtermann, A. Work-Time Compositions of Physical Behaviors and Trajectories of Sick Leave Due to Musculoskeletal Pain. Int. J. Environ. Res. Public Health 2021, 18, 1508. [Google Scholar] [CrossRef] [PubMed]
- Oakman, J.; Ketels, M.; Clays, E. Low back and neck pain: Objective and subjective measures of workplace psychosocial and physical hazards. Int. Arch. Occup. Environ. Health 2021, 94, 1637–1644. [Google Scholar] [CrossRef] [PubMed]
- Krause, N.; Arah, O.A.; Kauhanen, J. Physical activity and 22-year all-cause and coronary heart disease mortality. Am. J. Ind. Med. 2017, 60, 976–990. [Google Scholar] [CrossRef] [PubMed]
- Korshoj, M.; Lund Rasmussen, C.; de Oliveira Sato, T.; Holtermann, A.; Hallman, D. Heart rate during work and heart rate variability during the following night: A day-by-day investigation on the physical activity paradox among blue-collar workers. Scand. J. Work Environ. Health 2021, 47, 387–394. [Google Scholar] [CrossRef]
- Karvonen, J.; Vuorimaa, T. Heart rate and exercise intensity during sports activities. Practical application. Sports Med. 1988, 5, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Ilmarinen, J. Job design for the aged with regard to the decline in their maximal aerobic capacity: Part i-guidelines for the practitioner. Int. J. Ind. Ergonom. 1992, 10, 53–63. [Google Scholar] [CrossRef]
- Coenen, P.; Korshoj, M.; Hallman, D.M.; Huysmans, M.A.; van der Beek, A.J.; Straker, L.M.; Holtermann, A. Differences in heart rate reserve of similar physical activities during work and in leisure time-A study among Danish blue-collar workers. Physiol. Behav. 2018, 186, 45–51. [Google Scholar] [CrossRef]
- Van Poel, E.; Ketels, M.; Clays, E. The association between occupational physical activity, psychosocial factors and perceived work ability among nurses. J. Nurs. Manag. 2020, 28, 1696–1703. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, M.M.; Veronesi, G.; Roncaioli, M.; Holtermann, A.; Krause, N.; Clays, E.; Borchini, R.; Grassi, G.; Cesana, G.; The Cohorts Collaborative Study in Northern Italy (CCSNI) Research Group. Exploring the interplay between job strain and different domains of physical activity on the incidence of coronary heart disease in adult men. Eur. J. Prev. Cardiol. 2019, 26, 1877–1885. [Google Scholar] [CrossRef] [PubMed]
- Amiri, S.; Behnezhad, S. Sleep disturbances and back pain: Systematic review and meta-analysis. Neuropsychiatrie 2020, 34, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Rasmussen, C.L.; Holtermann, A.; Mathiassen, S.E. Time-Based Data in Occupational Studies: The Whys, the Hows, and Some Remaining Challenges in Compositional Data Analysis (CoDA). Ann. Work Expo. Health 2020, 64, 778–785. [Google Scholar] [CrossRef]
- Dumuid, D.; Pedisic, Z.; Palarea-Albaladejo, J.; Martin-Fernandez, J.A.; Hron, K.; Olds, T. Compositional Data Analysis in Time-Use Epidemiology: What, Why, How. Int. J. Environ. Res. Public Health 2020, 17, 2220. [Google Scholar] [CrossRef] [Green Version]
- Aitchison, J. The statistical analysis of compositional data. J. R. Statist. Soc. B 1982, 44, 139–177. [Google Scholar] [CrossRef]
- Dumuid, D.; Stanford, T.E.; Martin-Fernandez, J.A.; Pedisic, Z.; Maher, C.A.; Lewis, L.K.; Hron, K.; Katzmarzyk, P.T.; Chaput, J.P.; Fogelholm, M.; et al. Compositional data analysis for physical activity, sedentary time and sleep research. Stat. Methods Med. Res. 2018, 27, 3726–3738. [Google Scholar] [CrossRef] [Green Version]
- Gupta, N.; Mathiassen, S.E.; Mateu-Figueras, G.; Heiden, M.; Hallman, D.M.; Jorgensen, M.B.; Holtermann, A. A comparison of standard and compositional data analysis in studies addressing group differences in sedentary behavior and physical activity. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 53. [Google Scholar] [CrossRef]
- Lunde, L.K.; Koch, M.; Knardahl, S.; Waersted, M.; Mathiassen, S.E.; Forsman, M.; Holtermann, A.; Veiersted, K.B. Musculoskeletal health and work ability in physically demanding occupations: Study protocol for a prospective field study on construction and health care workers. BMC Public Health 2014, 14, 1075. [Google Scholar] [CrossRef] [Green Version]
- Lunde, L.K.; Koch, M.; Veiersted, K.B.; Moen, G.H.; Waersted, M.; Knardahl, S. Heavy Physical Work: Cardiovascular Load in Male Construction Workers. Int. J. Environ. Res. Public Health 2016, 13, 356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brage, S.; Brage, N.; Ekelund, U.; Luan, J.; Franks, P.W.; Froberg, K.; Wareham, N.J. Effect of combined movement and heart rate monitor placement on physical activity estimates during treadmill locomotion and free-living. Eur. J. Appl. Physiol. 2006, 96, 517–524. [Google Scholar] [CrossRef]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef] [Green Version]
- Caljouw, S.R.; de Vries, R.; Withagen, R. RAAAF’s office landscape the End of Sitting: Energy expenditure and temporary comfort when working in non-sitting postures. PLoS ONE 2017, 12, e0187529. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.C.; Wang, M.J. Relationship between maximum acceptable work time and physical workload. Ergonomics 2002, 45, 280–289. [Google Scholar] [CrossRef] [PubMed]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Veiersted, K.B.; Hanvold, T.N.; Lunde, L.K.; Koch, M.; Knardahl, S.; Waersted, M. Do intensity of pain alone or combined with pain duration best reflect clinical signs in the neck, shoulder and upper limb? Scand. J. Pain 2021, 21, 266–273. [Google Scholar] [CrossRef]
- Mannion, A.F.; Balague, F.; Pellise, F.; Cedraschi, C. Pain measurement in patients with low back pain. Nat. Clin. Pract. Rheumatol. 2007, 3, 610–618. [Google Scholar] [CrossRef]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sorensen, F.; Andersson, G.; Jorgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Ware, J.E., Jr. SF-36 health survey update. Spine (Phila Pa 1976) 2000, 25, 3130–3139. [Google Scholar] [CrossRef]
- Dallner, M.; Elo, A.-L.; Gamberale, F.; Hottinen, V.; Knardahl, S.; Lindstrom, K.; Skogstad, A.; Ørhede, E. Validation of the General Nordic Questionnaire (QPSNordic) for Psychological and Social Factors at Work; Nordic Council of Ministers: Copenhagen, Denmark, 2000; p. 171. [Google Scholar]
- Ahlstrom, L.; Grimby-Ekman, A.; Hagberg, M.; Dellve, L. The work ability index and single-item question: Associations with sick leave, symptoms, and health–A prospective study of women on long-term sick leave. Scand. J. Work Environ. Health 2010, 36, 404–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Astrand, P.O.; Rodahl, K.; Dahl, H.; Stromme, S. Textbook of Work Physiology: Physiological Bases of Exercise, 4th ed.; Human Kinetics: Champaign, IL, USA, 2003; p. 649. [Google Scholar]
- Astrand, P.O.; Ryhming, I. A nomogram for calculation of aerobic capacity (physical fitness) from pulse rate during sub-maximal work. J. Appl. Physiol. 1954, 7, 218–221. [Google Scholar] [CrossRef] [PubMed]
- Astrand, I. Aerobic work capacity in men and women with special reference to age. Acta Physiol. Scand. Suppl. 1960, 49, 1–92. [Google Scholar] [PubMed]
- Chastin, S.F.; Palarea-Albaladejo, J.; Dontje, M.L.; Skelton, D.A. Combined Effects of Time Spent in Physical Activity, Sedentary Behaviors and Sleep on Obesity and Cardio-Metabolic Health Markers: A Novel Compositional Data Analysis Approach. PLoS ONE 2015, 10, e0139984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dumuid, D.; Martin-Fernandez, J.A.; Ellul, S.; Kenett, R.S.; Wake, M.; Simm, P.; Baur, L.; Olds, T. Analysing body composition as compositional data: An exploration of the relationship between body composition, body mass and bone strength. Stat. Methods Med. Res. 2021, 30, 331–346. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, C.L.; Palarea-Albaladejo, J.; Bauman, A.; Gupta, N.; Nabe-Nielsen, K.; Jorgensen, M.B.; Holtermann, A. Does Physically Demanding Work Hinder a Physically Active Lifestyle in Low Socioeconomic Workers? A Compositional Data Analysis Based on Accelerometer Data. Int. J. Environ. Res. Public Health 2018, 15, 1306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, N.; Korshoj, M.; Dumuid, D.; Coenen, P.; Allesoe, K.; Holtermann, A. Daily domain-specific time-use composition of physical behaviors and blood pressure. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 4. [Google Scholar] [CrossRef] [Green Version]
- Health Profile Institute. Maximal Oxygen Uptake Reference Values for the Ekblom Bak Test. Available online: https://www.gih.se/Global/3_forskning/fysiologi/elinekblombak/Reference_values_180319_en.pdf (accessed on 2 August 2021).
- Jakobsen, M.D.; Sundstrup, E.; Persson, R.; Andersen, C.H.; Andersen, L.L. Is Borg′s perceived exertion scale a useful indicator of muscular and cardiovascular load in blue-collar workers with lifting tasks? A cross-sectional workplace study. Eur. J. Appl. Physiol. 2014, 114, 425–434. [Google Scholar] [CrossRef] [Green Version]
- Balogh, I.; Orbaek, P.; Ohlsson, K.; Nordander, C.; Unge, J.; Winkel, J.; Hansson, G.A.; Malmo Shoulder/Neck Study Group. Self-assessed and directly measured occupational physical activities–Influence of musculoskeletal complaints, age and gender. Appl. Ergon. 2004, 35, 49–56. [Google Scholar] [CrossRef]
- Hanvold, T.N.; Lunde, L.K.; Koch, M.; Waersted, M.; Veiersted, K.B. Multisite musculoskeletal pain among young technical school students entering working life. BMC Musculoskelet. Disord. 2016, 17, 82. [Google Scholar] [CrossRef] [Green Version]
- Coggon, D.; Ntani, G.; Palmer, K.T.; Felli, V.E.; Harari, R.; Barrero, L.H.; Felknor, S.A.; Gimeno, D.; Cattrell, A.; Vargas-Prada, S.; et al. Patterns of multisite pain and associations with risk factors. Pain 2013, 154, 1769–1777. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neupane, S.; Leino-Arjas, P.; Nygard, C.H.; Oakman, J.; Virtanen, P. Developmental pathways of multisite musculoskeletal pain: What is the influence of physical and psychosocial working conditions? Occup. Environ. Med. 2017, 74, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Holtermann, A.; Mortensen, O.S.; Burr, H.; Sogaard, K.; Gyntelberg, F.; Suadicani, P. Physical demands at work, physical fitness, and 30-year ischaemic heart disease and all-cause mortality in the Copenhagen Male Study. Scand. J. Work Environ. Health 2010, 36, 357–365. [Google Scholar] [CrossRef] [Green Version]
- Ketels, M.; Rasmussen, C.L.; Korshoj, M.; Gupta, N.; De Bacquer, D.; Holtermann, A.; Clays, E. The Relation between Domain-Specific Physical Behaviour and Cardiorespiratory Fitness: A Cross-Sectional Compositional Data Analysis on the Physical Activity Health Paradox Using Accelerometer-Assessed Data. Int. J. Environ. Res. Public Health 2020, 17, 7929. [Google Scholar] [CrossRef] [PubMed]
- Seaman, D.R. Body mass index and musculoskeletal pain: Is there a connection? Chiropr. Man. Therap. 2013, 21, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okifuji, A.; Hare, B.D. The association between chronic pain and obesity. J. Pain Res. 2015, 8, 399–408. [Google Scholar] [CrossRef] [Green Version]
- Chin, S.H.; Huang, W.L.; Akter, S.; Binks, M. Obesity and pain: A systematic review. Int. J. Obes. (Lond.) 2020, 44, 969–979. [Google Scholar] [CrossRef]
- Mathiassen, S.E. The influence of exercise/rest schedule on the physiological and psychophysical response to isometric shoulder-neck exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1993, 67, 528–539. [Google Scholar] [CrossRef]
- Coenen, P.; Healy, G.N.; Winkler, E.A.H.; Dunstan, D.W.; Owen, N.; Moodie, M.; LaMontagne, A.D.; Eakin, E.A.; O’Sullivan, P.B.; Straker, L.M. Associations of office workers’ objectively assessed occupational sitting, standing and stepping time with musculoskeletal symptoms. Ergonomics 2018, 61, 1187–1195. [Google Scholar] [CrossRef]
- Hallman, D.M.; Mathiassen, S.E.; Gupta, N.; Korshoj, M.; Holtermann, A. Differences between work and leisure in temporal patterns of objectively measured physical activity among blue-collar workers. BMC Public Health 2015, 15, 976. [Google Scholar] [CrossRef] [Green Version]
- Shah, J.P.; Gilliams, E.A. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: An application of muscle pain concepts to myofascial pain syndrome. J. Bodyw. Mov. Ther. 2008, 12, 371–384. [Google Scholar] [CrossRef] [PubMed]
- Minerbi, A.; Vulfsons, S. Challenging the Cinderella Hypothesis: A New Model for the Role of the Motor Unit Recruitment Pattern in the Pathogenesis of Myofascial Pain Syndrome in Postural Muscles. Rambam Maimonides Med. J. 2018, 9, e0021. [Google Scholar] [CrossRef]
- Generaal, E.; Vogelzangs, N.; Penninx, B.W.; Dekker, J. Insomnia, Sleep Duration, Depressive Symptoms, and the Onset of Chronic Multisite Musculoskeletal Pain. Sleep 2017, 40, 1–10. [Google Scholar] [CrossRef]
- Chun, M.Y.; Cho, B.J.; Yoo, S.H.; Oh, B.; Kang, J.S.; Yeon, C. Association between sleep duration and musculoskeletal pain: The Korea National Health and Nutrition Examination Survey 2010–2015. Medicine (Baltimore) 2018, 97, e13656. [Google Scholar] [CrossRef] [PubMed]
- Trinkoff, A.M.; Le, R.; Geiger-Brown, J.; Lipscomb, J.; Lang, G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. Am. J. Ind. Med. 2006, 49, 964–971. [Google Scholar] [CrossRef]


| Total (n = 72) | ||||
|---|---|---|---|---|
| n | (%) | mean | (sd) | |
| Age (years) | 42.5 | (11.1) | ||
| Seniority (years) | 17 | (11.2) | ||
| Work hours (per week) | 36.7 | (4.4) | ||
| Gender | ||||
| Male | 43 | (60) | ||
| Female | 29 | (40) | ||
| Sector | ||||
| Construction | 35 | (49) | ||
| Healthcare | 37 | (51) | ||
| BMI (kg/m2) | 25.6 | (3.5) | ||
| BMI | ||||
| Normal (<25 kg/m2) | 35 | (49) | ||
| Overweight/obese (≥25 kg/m2) | 37 | (51) | ||
| VO2max (ml/min/kg) | 35.6 | (10.5) | ||
| Smoking | ||||
| Yes (current smoker) | 20 | (28) | ||
| No (never or quit smoking) | 52 | (72) | ||
| Work ability (scale 0–10) | 8.9 | (1.4) | ||
| Control of work pacing at baseline (score 1–5) | 2.8 | (0.8) | ||
| General health | ||||
| Poor or fair | 11 | (15) | ||
| Good | 28 | (39) | ||
| Very good or excellent | 33 | (46) | ||
| Overall musculoskeletal pain at baseline (0–27) | 5.6 | (5.0) | ||
| Mean Time in a Day (Minutes) | Proportion of the Day (% Time) | |||
|---|---|---|---|---|
| n = 72 | n = 72 | |||
| 20 %HRR | mean | (sd) | mean | (sd) |
| ≥20 %HRR Work | 327 | (132) | 22.7 | (9.1) |
| <20 %HRR Work | 145 | (115) | 10.0 | (8.0) |
| ≥20 %HRR Leisure | 305 | (152) | 21.2 | (10.5) |
| <20 %HRR Leisure | 269 | (133) | 18.7 | (9.2) |
| Sleep | 394 | (80) | 27.4 | (5.6) |
| Total | 1440 | 100 | ||
| 30 %HRR | ||||
| ≥30 %HRR Work | 154 | (107) | 10.6 | (7.4) |
| <30 %HRR Work | 318 | (133) | 22.1 | (9.3) |
| ≥30 %HRR Leisure | 131 | (93) | 9.1 | (6.5) |
| <30 %HRR Leisure | 443 | (130) | 30.8 | (9.0) |
| Sleep | 394 | (80) | 27.4 | (5.6) |
| Total | 1440 | 100 | ||
| 40 %HRR | ||||
| ≥40 %HRR Work | 43 | (52) | 3.0 | (3.6) |
| <40 %HRR Work | 429 | (120) | 29.7 | (8.3) |
| ≥40 %HRR Leisure | 47 | (50) | 3.3 | (3.4) |
| <40 %HRR Leisure | 527 | (138) | 36.6 | (9.6) |
| Sleep | 394 | (80) | 27.4 | (5.6) |
| Total | 1440 | 100 | ||
| %HRR threshold | ß | (95% CI) |
|---|---|---|
| 20 %HRR | ||
| Intercept | 4.06 | (1.67–6.45) |
| Time | 0.01 | (−0.22–0.23) |
| Awake/Sleep (ilr1) | −1.18 | (−5.08–2.72) |
| Work/Leisure (ilr2) | −0.53 | (−2.43–1.38) |
| ≥20 %HRR Work/<20 %HRR Work (ilr3) | 1.01 | (−0.35–2.36) |
| ≥20 %HRR Leisure/<20 %HRR Leisure (ilr4) | −1.56 | (−3.29–0.17) |
| 30 %HRR | ||
| Intercept | 5.22 | (2.33–8.10) |
| Time | 0.01 | (−0.22–0.23) |
| Awake/Sleep (ilr1) | −0.56 | (−4.88–3.75) |
| Work/Leisure (ilr2) | −0.27 | (−2.26–1.71) |
| ≥30 %HRR Work/<30 %HRR Work (ilr3) | 0.92 | (−0.63–2.48) |
| ≥30 %HRR Leisure/<30 %HRR Leisure (ilr4) | −0.57 | (−2.59–1.45) |
| 40 %HRR | ||
| Intercept | 6.08 | (2.77–9.36) |
| Time | 0.01 | (−0.22–0.23) |
| Awake/Sleep (ilr1) | −1.02 | (−5.60–3.54) |
| Work/Leisure (ilr2) | −0.32 | (−2.47–1.84) |
| ≥40 %HRR Work/<40 %HRR Work (ilr3) | 0.98 | (−1.28–3.24) |
| ≥40 %HRR Leisure/<40 %HRR Leisure (ilr4) | −0.15 | (−2.23–1.94) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Merkus, S.L.; Coenen, P.; Forsman, M.; Knardahl, S.; Veiersted, K.B.; Mathiassen, S.E. An Exploratory Study on the Physical Activity Health Paradox—Musculoskeletal Pain and Cardiovascular Load during Work and Leisure in Construction and Healthcare Workers. Int. J. Environ. Res. Public Health 2022, 19, 2751. https://doi.org/10.3390/ijerph19052751
Merkus SL, Coenen P, Forsman M, Knardahl S, Veiersted KB, Mathiassen SE. An Exploratory Study on the Physical Activity Health Paradox—Musculoskeletal Pain and Cardiovascular Load during Work and Leisure in Construction and Healthcare Workers. International Journal of Environmental Research and Public Health. 2022; 19(5):2751. https://doi.org/10.3390/ijerph19052751
Chicago/Turabian StyleMerkus, Suzanne Lerato, Pieter Coenen, Mikael Forsman, Stein Knardahl, Kaj Bo Veiersted, and Svend Erik Mathiassen. 2022. "An Exploratory Study on the Physical Activity Health Paradox—Musculoskeletal Pain and Cardiovascular Load during Work and Leisure in Construction and Healthcare Workers" International Journal of Environmental Research and Public Health 19, no. 5: 2751. https://doi.org/10.3390/ijerph19052751
APA StyleMerkus, S. L., Coenen, P., Forsman, M., Knardahl, S., Veiersted, K. B., & Mathiassen, S. E. (2022). An Exploratory Study on the Physical Activity Health Paradox—Musculoskeletal Pain and Cardiovascular Load during Work and Leisure in Construction and Healthcare Workers. International Journal of Environmental Research and Public Health, 19(5), 2751. https://doi.org/10.3390/ijerph19052751








