A Pilot Study on the Feasibility of Developing and Implementing a Mobile App for the Acquisition of Clinical Knowledge and Competencies by Medical Students Transitioning from Preclinical to Clinical Years
Abstract
:1. Introduction
2. Materials and Methods
- –
- Enrollment in the subject “General Pathology” from the second year of Medicine Degree in our University;
- –
- Voluntary provision of explicit consent;
- –
- Owning an Android® device connected to the internet.
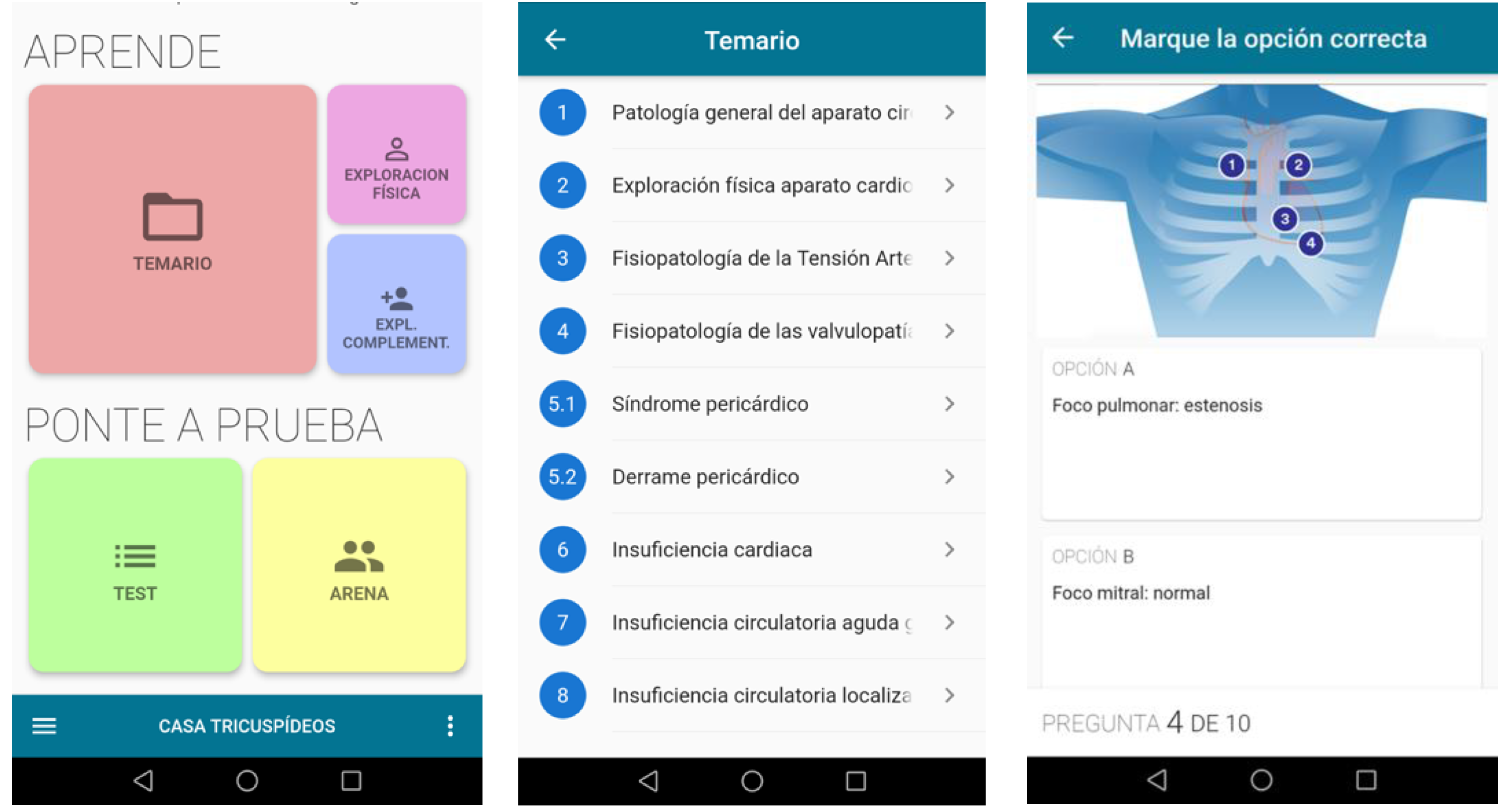
- (i)
- Lectures and slides covering different topics in PDF format;
- (ii)
- Physical exploration guide with an interactive auscultation module;
- (iii)
- Main investigations in cardiovascular pathology with resources in various formats;
- (iv)
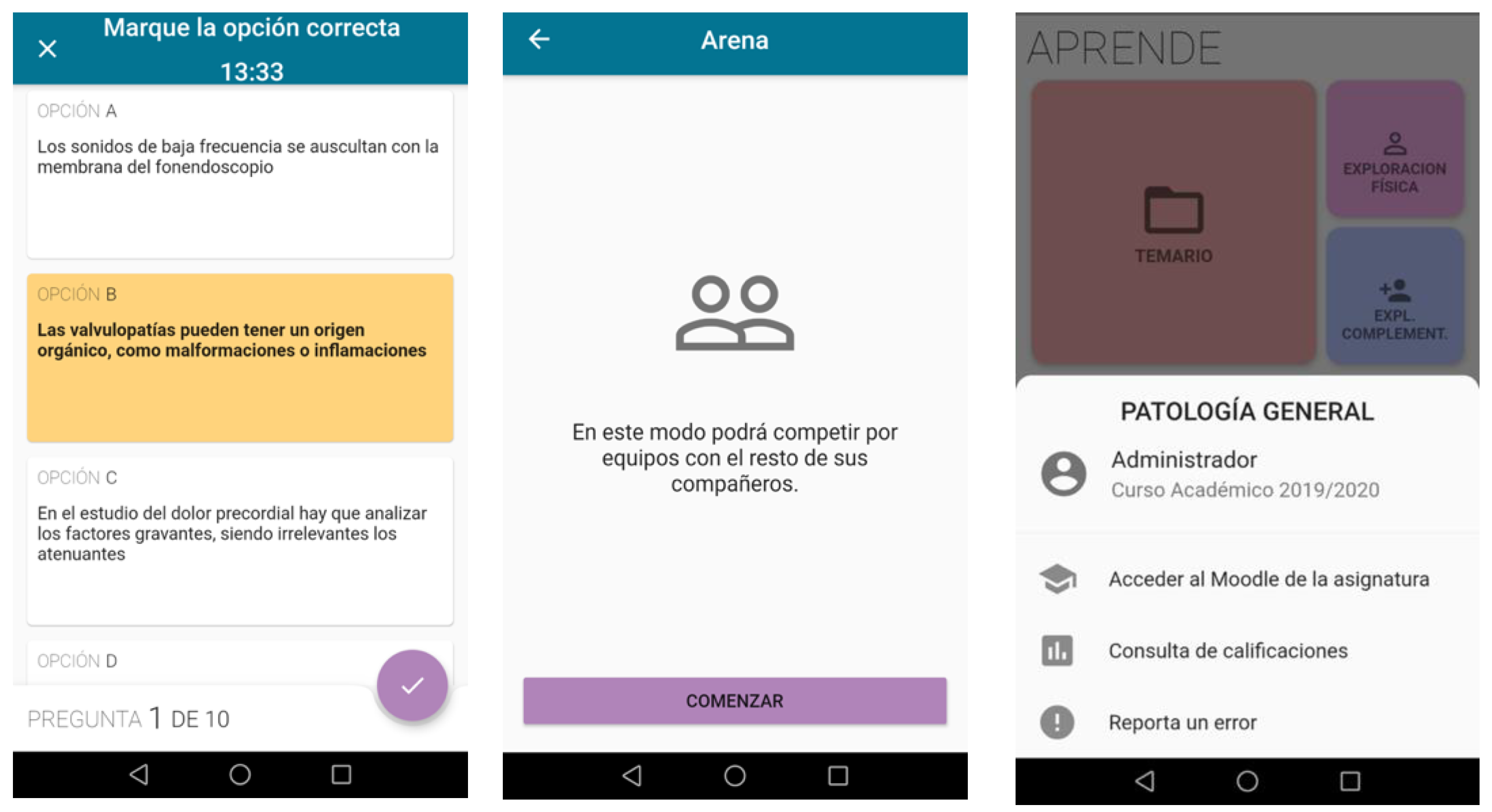
- Tests for self-assessment;
- (v)
- Arena: programmed team-based competition encouraging students to answer multiple-choice questions, thus reinforcing learning through the teaching period by engaging among peers.
- (vi)
- Others: quick access to the university platform, results from tests, technical support, etc.
- (a)
- For comparing quantitative variables, we used:
- –
- Contrasts between two groups with independent/unpaired data: Student t-test (parametric) or Mann–Whitney U-test (nonparametric);
- –
- Contrasts between two groups with paired data: Student t-test for paired data (parametric) or Wilcoxon test (nonparametric).
- (b)
- For correlating quantitative variables, Pearson’s linear correlation coefficient (r) was used.
3. Results
3.1. Participants’ Demographics and Previous Digital Competency
3.2. Team-Based Competition and App-Use Data
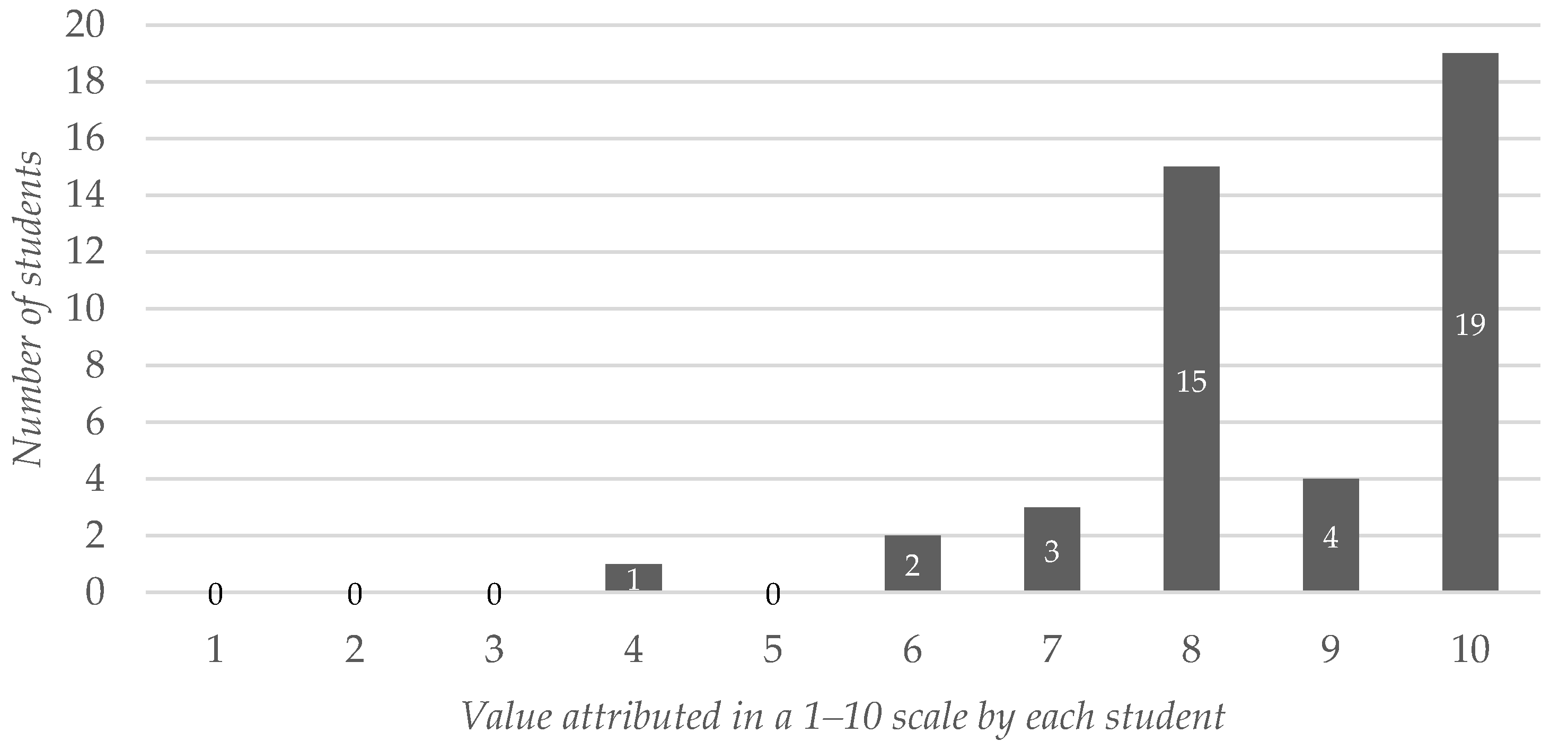
3.3. Learning Value Attributed to the App
3.4. Influence of Self-Reported Digital Competence on the Learning Value Attributed to the App
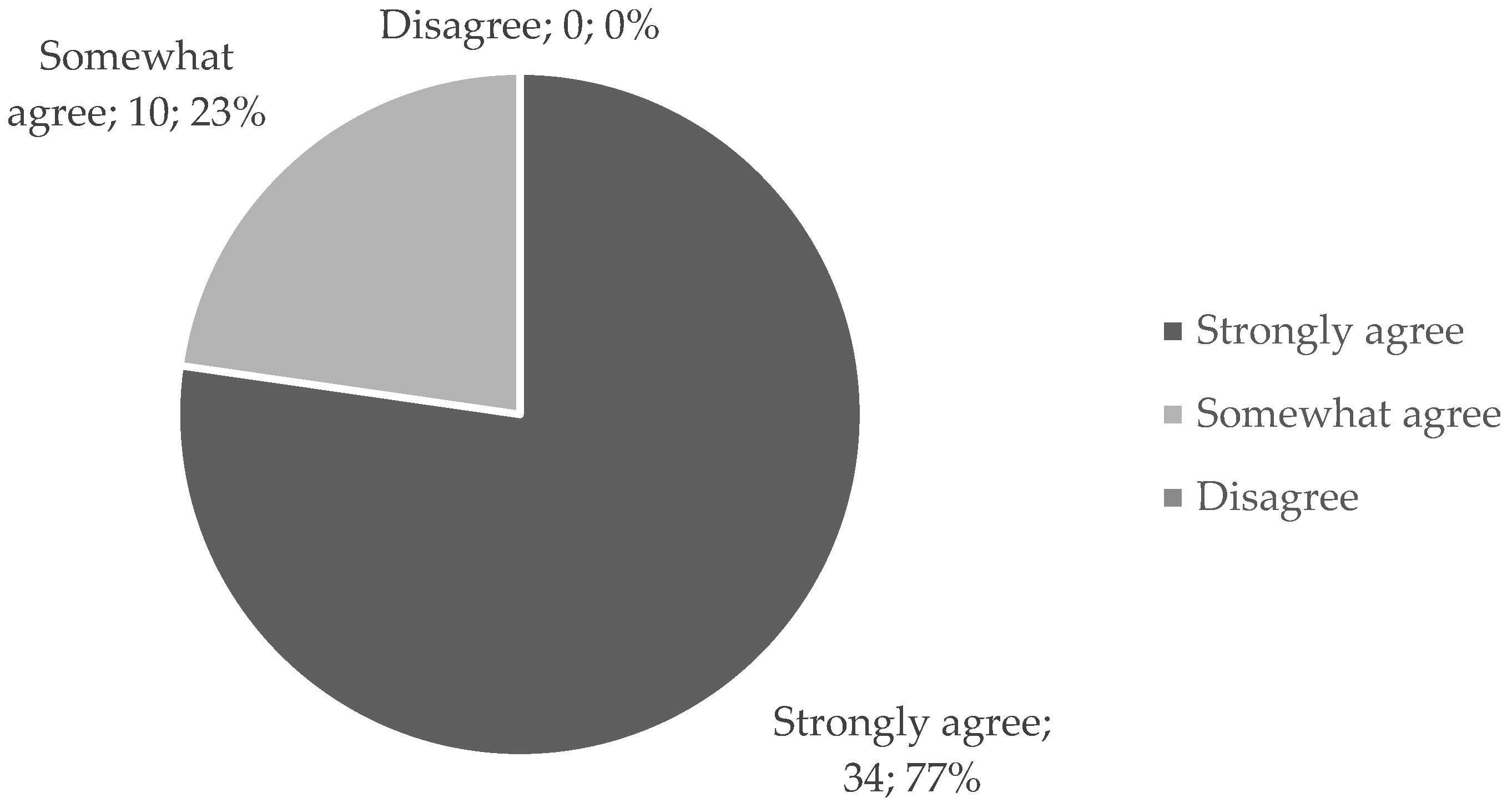
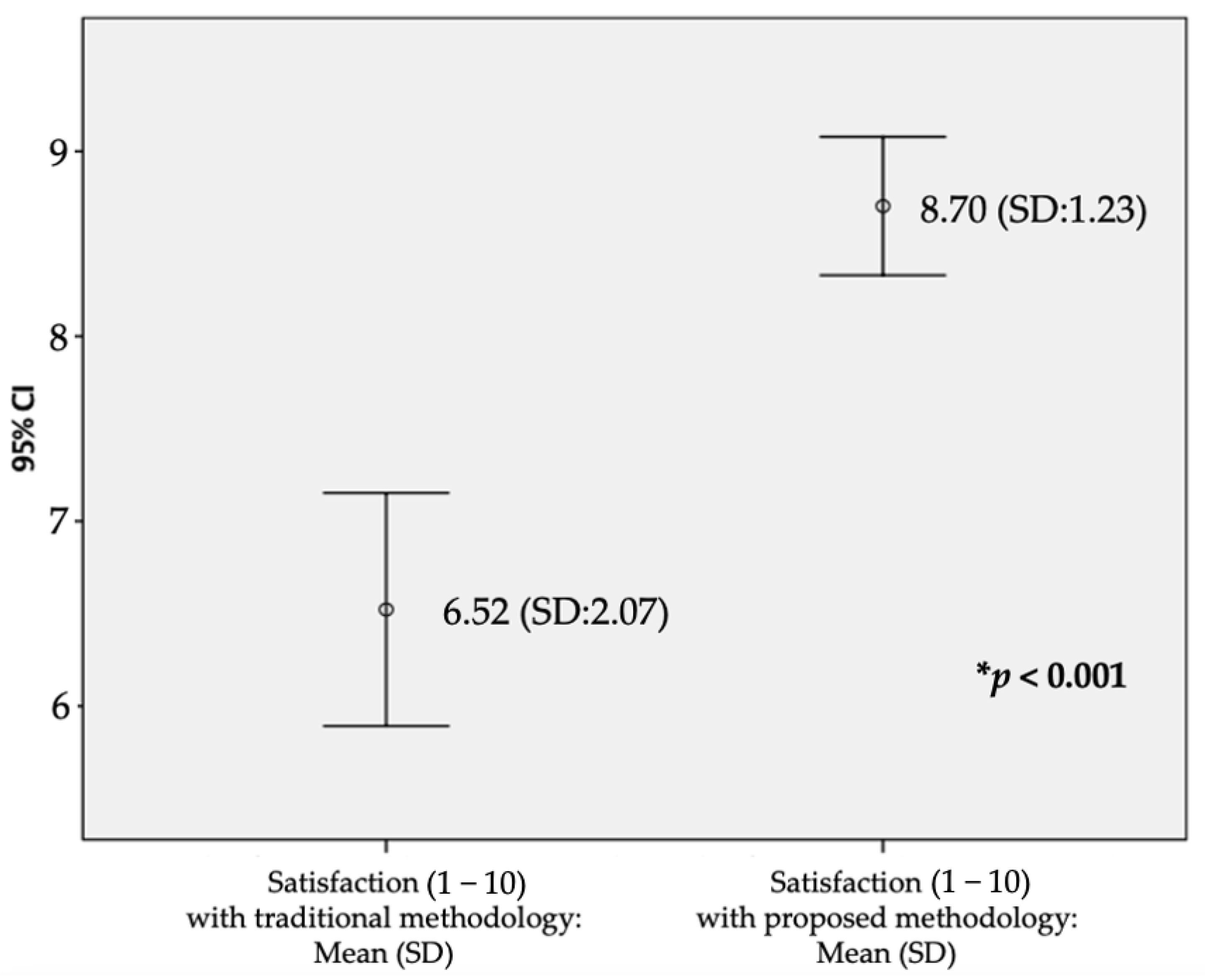
3.5. Acceptability of the App
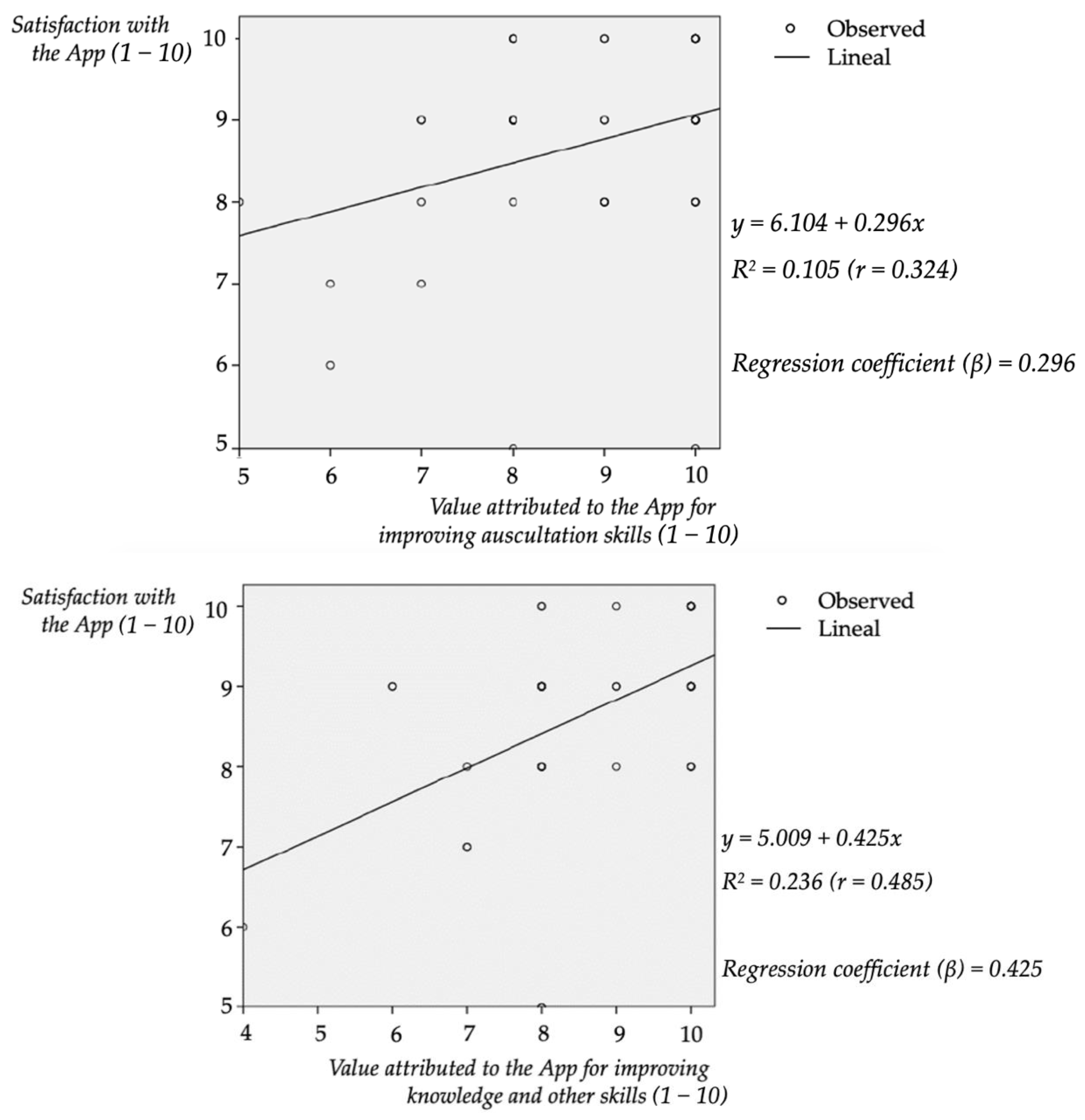
3.6. Correlation between Satisfaction and Learning Value Attributed to the app
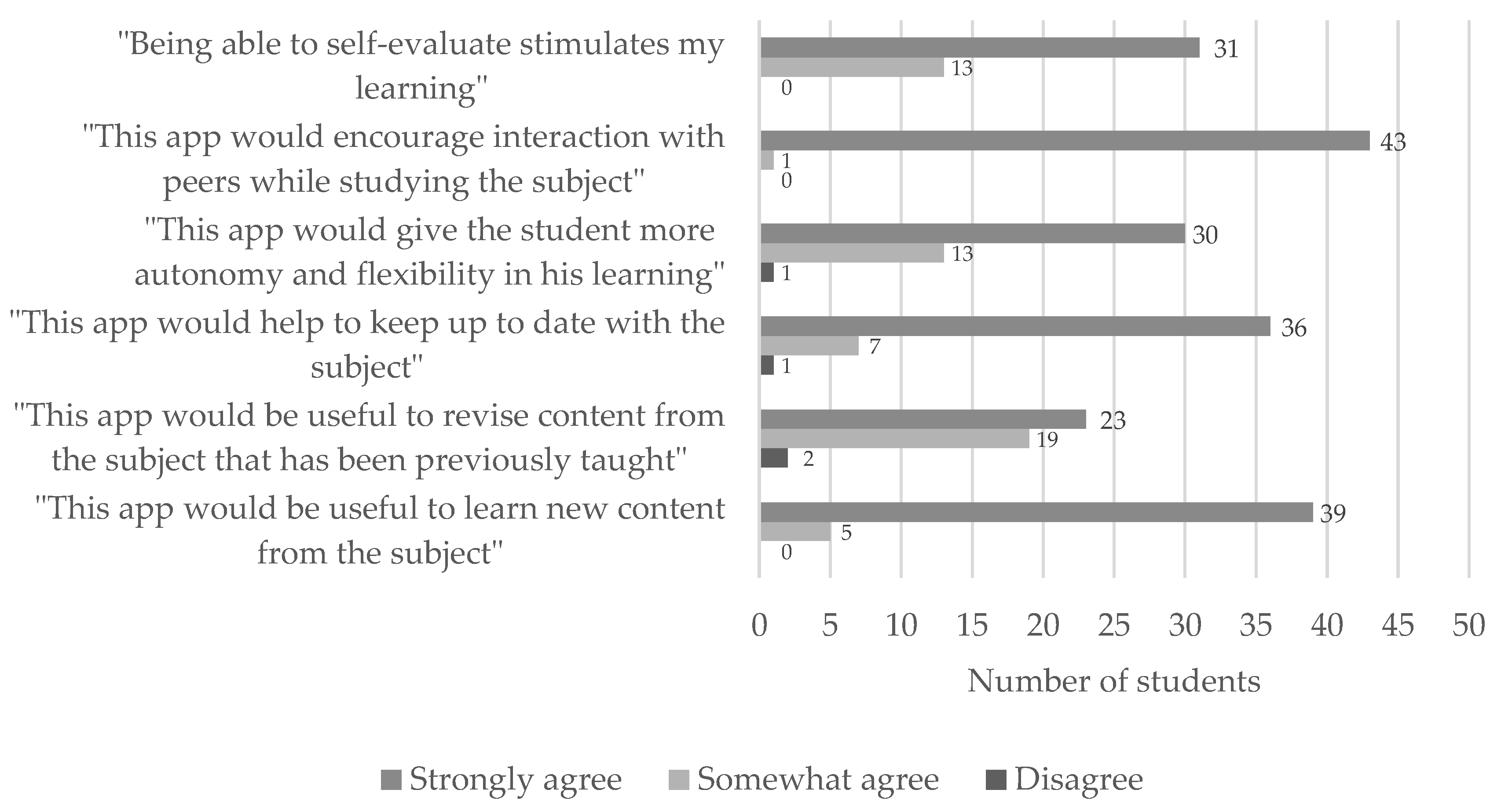
3.7. Feedback from Participants
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
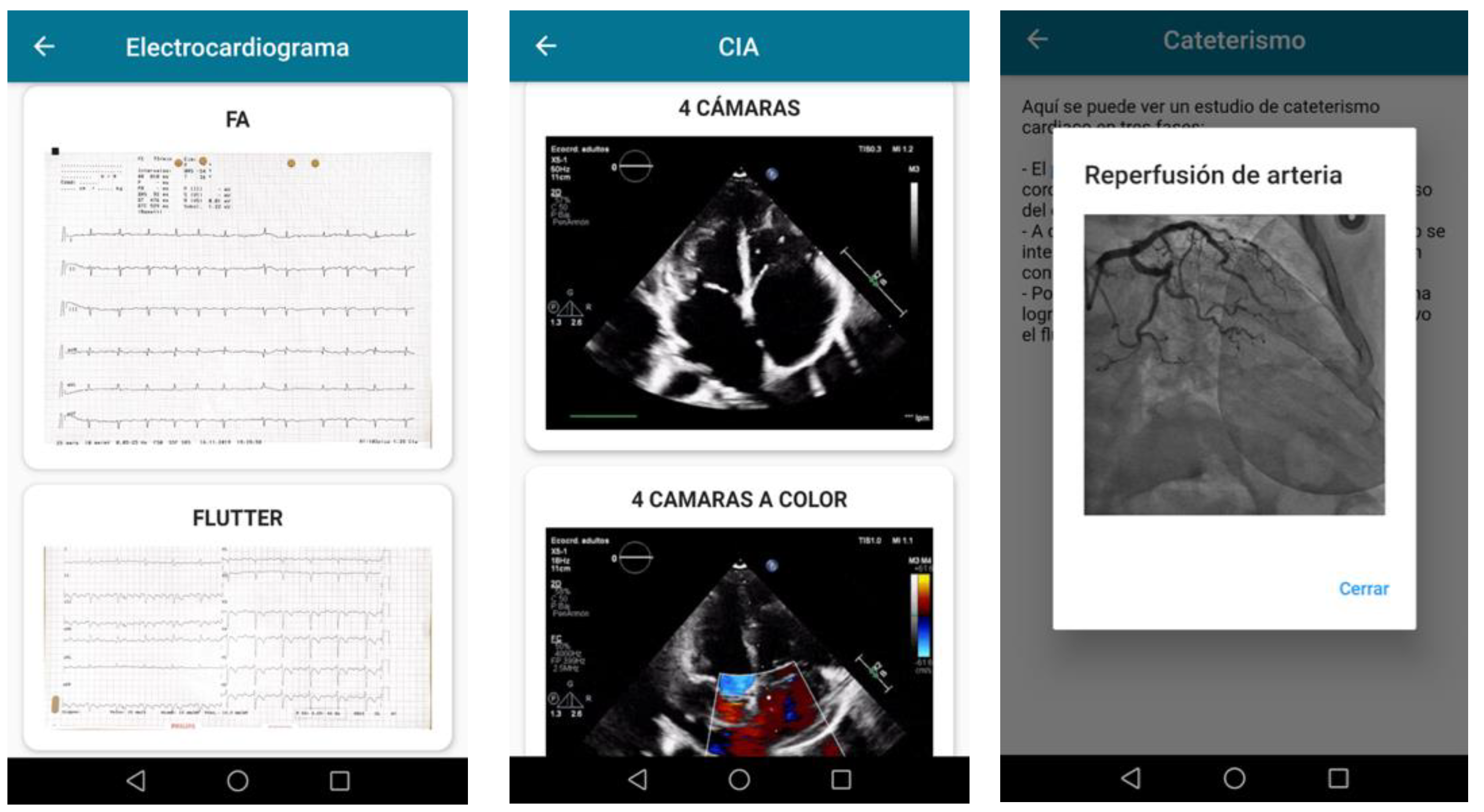
Appendix A. Description of the App
- Bookshelf. Presentations and resources connected to the lectures;
- Physical exploration module. Useful information and didactic resources, presented in several formats (images, texts, videos, sounds, links) aiming to contribute to the teaching of the systematic process of exploring a patient. The app included an interactive module of auscultation in which the students could be trained in this set of skills following two approaches: the first one allowed them to select what kind of sound they wanted to hear, and the second one consisted of a multiple-choice battery of questions based on presented sounds on the virtual patient’s thorax. More than 25 physiological and pathological sounds were included;
- Investigations. More than 30 resources and multi-format examples about electrocardiography, echocardiography, and catheterization studies were included;
- Test. More than 1300 true and false statements filtered by the different topics covered in the subject were included to be randomly combined according to the students’ preferences when loading a self-assessment test;
- Arena. Multi-participant and collaborative competition among the students. When registered, the students were assigned a team or “House”. In each of the 15 min programmed activities, the students answered multiple-choice questions to gain points for their “House”;
- Others. Access to the University’s online platform, previous results, help, and support;
Appendix B. Survey Used
- Rate your satisfaction with the methodology traditionally used for teaching the subject (e.g., the one used during the Hematology module).Totally unsatisfied Totally Satisfied
- Indicate your expected satisfaction with a methodology combining both the traditional resources and the new app as it has been used during the Cardiology module.Totally unsatisfied Totally Satisfied
- Up to what extent an app like this one could help you improve your auscultation skills and ability to identify heart sounds?Useless Really Useful
- Up to what extent an app like this one could help you improve your knowledge and other competencies included in the “General Pathology” subject?Useless Really Useful
- Rate your level of agreement with the following statement: “My digital competence is good and I can use new technologies with ease”.O Disagree. O Somewhat agree. O Strongly agree.
- Have you received enough information about the app and the ongoing project, and do you fully understand its aim?O Yes. O No.
- Rate your level of agreement with the following statements:
Disagree Somewhat Agree Strongly Agree “Being able to self-evaluate stimulates my learning” “This app would encourage interaction with peers while studying the subject” “This app would give the student more autonomy and flexibility in his learning” “This app would help to keep up to date with the subject” “This app would be useful to revise content from the subject that has been previously taught” “This app would be useful to learn new content from the subject”
References
- Flexner, A.; Updike, D.B.; Pritchett, H.S. Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching; Science and Health Publications, Inc.: New York, NY, USA, 1910. [Google Scholar]
- Dedeilia, A.; Sotiropoulos, M.; Hanrahan, J.G.; Janga, D.; Dedeilias, P.; Sideris, M. Medical and Surgical Education Challenges and Innovations in the COVID-19 Era: A Systematic Review. In Vivo 2020, 34 (Suppl. 3), 1603–1611. [Google Scholar] [CrossRef]
- Holmboe, E.S.; Call, S.; Ficalora, R.D. Milestones and Competency-Based Medical Education in Internal Medicine. JAMA Intern. Med. 2016, 176, 1601–1602. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, R.E.; Welcher, C.M.; Holmboe, E.S.; Kirk, L.M.; Norcini, J.J.; Simons, K.B.; Skochelak, S.E. Implementation of competency-based medical education: Are we addressing the concerns and challenges? Med. Educ. 2015, 49, 1086–1102. [Google Scholar] [CrossRef] [PubMed]
- Baheerathan, A.; Selvaskandan, H. Smartphones and medical education. Clin. Teach. 2014, 11, 485–486. [Google Scholar] [CrossRef]
- Kaul, V.; de Moraes, A.G.; Khateeb, D.; Greenstein, Y.; Winter, G.; Chae, J.; Stewart, N.H.; Qadir, N.; Dangayach, N.S. Medical Education During the COVID-19 Pandemic. Chest 2021, 159, 1949–1960. [Google Scholar] [CrossRef] [PubMed]
- Loda, T.; Löffler, T.; Erschens, R.; Zipfel, S.; Herrmann-Werner, A. Medical education in times of COVID-19: German students’ expectations—A cross-sectional study. PLoS ONE 2020, 15, e0241660. [Google Scholar] [CrossRef]
- Al Samaraee, A. The impact of the COVID-19 pandemic on medical education. Br. J. Hosp. Med. 2020, 81, 1–4. [Google Scholar] [CrossRef]
- Iancu, A.M.; Kemp, M.T.; Alam, H.B. Unmuting Medical Students’ Education: Utilizing Telemedicine During the COVID-19 Pandemic and Beyond. J. Med. Internet Res. 2020, 22, e19667. [Google Scholar] [CrossRef]
- Rose, S. Medical Student Education in the Time of COVID-19. JAMA 2020, 323, 2131–2132. [Google Scholar] [CrossRef]
- Sandhu, P.; de Wolf, M. The impact of COVID-19 on the undergraduate medical curriculum. Med. Educ. Online 2020, 25, 1764740. [Google Scholar] [CrossRef]
- Sharma, S.; Sharma, V. Medical Education During the COVID-19 Pandemics—Challenges Ahead. Indian Pediatr. 2020, 57, 772. [Google Scholar] [CrossRef] [PubMed]
- Hilburg, R.; Patel, N.; Ambruso, S.; Biewald, M.A.; Farouk, S.S. Medical Education during the Corona-virus Disease-2019 Pandemic: Learning from a Distance. Adv. Chronic Kidney Dis. 2020, 27, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Ruthberg, J.S.; Quereshy, H.A.; Ahmadmehrabi, S.; Trudeau, S.; Chaudry, E.; Hair, B.; Kominsky, A.; Otteson, T.D.; Bryson, P.C.; Mowry, S.E. A Multimodal Multi-institutional Solution to Remote Medical Student Education for Otolaryngology during COVID-19. Otolaryngol. Head Neck Surg. 2020, 163, 707–709. [Google Scholar] [CrossRef] [PubMed]
- Alsoufi, A.; Alsuyihili, A.; Msherghi, A.; Elhadi, A.; Atiyah, H.; Ashini, A.; Ashwieb, A.; Ghula, M.; Ben Hasan, H.; Abudabuos, S.; et al. Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS ONE 2020, 15, e0242905. [Google Scholar] [CrossRef] [PubMed]
- Almarzooq, Z.I.; Lopes, M.; Kochar, A. Virtual Learning During the COVID-19 Pandemic: A Disruptive Technology in Graduate Medical Education. J. Am. Coll. Cardiol. 2020, 75, 2635–2638. [Google Scholar] [CrossRef]
- Wynter, L.; Burgess, A.; Kalman, E.; Heron, J.E.; Bleasel, J. Medical students: What educational resources are they using? BMC Med. Educ. 2019, 19, 36. [Google Scholar] [CrossRef] [Green Version]
- Li, H.O.; Bailey, A.M.J. Medical Education Amid the COVID-19 Pandemic: New Perspectives for the Future. Acad Med. 2020, 95, e11–e12. [Google Scholar] [CrossRef]
- Mukhtar, K.; Javed, K.; Arooj, M.; Sethi, A. Advantages, Limitations and Recommendations for online learning during COVID-19 pandemic era. Pak. J. Med. Sci. 2020, 36, S27–S31. [Google Scholar] [CrossRef]
- Guze, P.A. Using Technology to Meet the Challenges of Medical Education. Trans. Am. Clin. Clim. Assoc. 2015, 126, 260–270. [Google Scholar]
- Issenberg, S.B.; McGaghie, W.; Petrusa, E.R.; Gordon, D.L.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef]
- Koohestani, H.R.; Arabshahi, S.K.S.; Fata, L.; Ahmadi, F. The educational effects of mobile learning on medical sciences students: A systematic review in experimental studies. J. Adv. Med. Educ. Prof. 2018, 6, 58–69. [Google Scholar] [PubMed]
- Guo, P.; Watts, K.; Wharrad, H. An integrative review of the impact of mobile technologies used by healthcare professionals to support education and practice. Nurs. Open 2015, 3, 66–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gentry, S.V.; Gauthier, A.; Ehrstrom, B.L.; Wortley, D.; Lilienthal, A.; Car, L.T.; Dauwels-Okutsu, S.; Nikolaou, C.K.; Zary, N.; Campbell, J.; et al. Serious Gaming and Gamification Education in Health Professions: Systematic Review. J. Med Internet Res. 2019, 21, e12994. [Google Scholar] [CrossRef] [Green Version]
- Valle, J.; Godby, T.; Paul, D.P.; Smith, H.; Coustasse, A. Use of Smartphones for Clinical and Medical Education. Health Care Manag. 2017, 36, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Desy, J.R.; Reed, D.A.; Wolanskyj, A.P. Milestones and Millennials: A Perfect Pairing—Competency-Based Medical Education and the Learning Preferences of Generation Y. Mayo Clin. Proc. 2017, 92, 243–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chase, T.J.G.; Julius, A.; Chandan, J.S.; Powell, E.; Hall, C.S.; Phillips, B.L.; Burnett, R.; Gill, D.; Fernando, B. Mobile learning in medicine: An evaluation of attitudes and behaviours of medical students. BMC Med Educ. 2018, 18, 152. [Google Scholar] [CrossRef] [Green Version]
- Matzavela, V.; Alepis, E. M-learning in the COVID-19 era: Physical vs digital class. Educ. Inf. Technol. 2021, 26, 7183–7203. [Google Scholar] [CrossRef]
- Torda, A.J.; Velan, G.; Perkovic, V. The impact of the COVID-19 pandemic on medical education. Med. J. Aust. 2020, 213, 334.e1. [Google Scholar] [CrossRef]
- Ding, A. Medical education-collateral damage of COVID-19? Postgrad. Med. J. 2021, 97, 404–405. [Google Scholar] [CrossRef]
- Adedoyin, O.B.; Soykan, E. Covid-19 pandemic and online learning: The challenges and opportunities. Interact. Learn. Environ. 2020, 2, 1–13. [Google Scholar] [CrossRef]
- Caverzagie, K.J.; Nousiainen, M.T.; Ferguson, P.C.; ten Cate, O.; Ross, S.; Harris, K.A.; Busari, J.; Dylan Bould, M.; Bouchard, J.; Iobst, W.F. Overarching challenges to the implementation of competency-based medical education. Med Teach. 2017, 39, 588–593. [Google Scholar] [CrossRef] [PubMed]
- Dunleavy, G.; Nikolaou, C.K.; Nifakos, S.; Atun, R.; Law, G.C.Y.; Tudor Car, L. Mobile Digital Education for Health Professions: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12937. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKinney, J.; Cook, D.A.; Wood, D.; Hatala, R. Simulation-Based Training for Cardiac Auscultation Skills: Systematic Review and Meta-Analysis. J. Gen. Intern. Med. 2012, 28, 283–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lall, P.; Rees, R.; Law, G.C.Y.; Dunleavy, G.; Cotič, Ž.; Car, J. Influences on the Implementation of Mobile Learning for Medical and Nursing Education: Qualitative Systematic Review by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12895. [Google Scholar] [CrossRef]
- Ellaway, R.; Masters, K. AMEE Guide 32: E-Learning in medical education Part 1: Learning, teaching and assessment. Med Teach. 2008, 30, 455–473. [Google Scholar] [CrossRef]
- Masters, K.; Ellaway, R.H.; Topps, D.; Archibald, D.; Hogue, R.J. Mobile technologies in medical education: AMEE Guide No. 105. Med. Teach. 2016, 38, 537–549. [Google Scholar] [CrossRef]
- Kononowicz, A.A.; Woodham, L.A.; Edelbring, S.; Stathakarou, N.; Davies, D.; Saxena, N.; Car, L.T.; Carlstedt-Duke, J.; Car, J.; Zary, N. Virtual Patient Simulations in Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e14676. [Google Scholar] [CrossRef]
- Akaike, M.; Fukutomi, M.; Nagamune, M.; Fujimoto, A.; Tsuji, A.; Ishida, K.; Iwata, T. Simulation-based medical education in clinical skills laboratory. J. Med. Investig. 2012, 59, 28–35. [Google Scholar] [CrossRef] [Green Version]
- Schneider, S.L.; Council, M.L. Distance learning in the era of COVID-19. Arch. Dermatol. Res. 2021, 313, 389–390. [Google Scholar] [CrossRef]
- Green, B.L.; Kennedy, I.; Hassanzadeh, H.; Sharma, S.; Frith, G.; Darling, J.C. A semi-quantitative and thematic analysis of medical student attitudes towards M-Learning. J. Eval. Clin. Pract. 2015, 21, 925–930. [Google Scholar] [CrossRef]
- Organización Médica Colegial de España (OMC). Estudio sobre Demografía Médica. In Revista del CGCOM; Organización Médica Colegial de España (OMC): Madrid, Spain, 2018. [Google Scholar]
- Singh, K.; Srivastav, S.; Bhardwaj, A.; Dixit, A.; Misra, S. Medical Education During the COVID-19 Pandemic: A Single Institution Experience. Indian Pediatr. 2020, 57, 678–679. [Google Scholar] [CrossRef]
- Rezende, A.B.; De Oliveira, A.G.; Vale, T.C.; Teixeira, L.A.; Lima, A.R.; Lucchetti, A.L.; Lucchetti, G.; Tibiriçá, S.H.; Ezequiel, O.S. Comparison of Team-Based Learning versus Traditional Lectures in Neuroanatomy: Medical Student Knowledge and Satisfaction. Anat. Sci. Educ. 2020, 13, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Alegría, D.A.; Boscardin, C.; Poncelet, A.; Mayfield, C.; Wamsley, M. Using tablets to support self-regulated learning in a longitudinal integrated clerk-ship. Med. Educ. Online 2014, 19, 23638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chatterjee, S.; Desai, S.; Manesh, R.; Sun, J.; Nundy, S.; Wright, S.M. Assessment of a Simulated Case-Based Measurement of Physician Diagnostic Performance. JAMA Netw. Open 2019, 2, e187006. [Google Scholar] [CrossRef] [PubMed]
- Tokuda, Y.; Matayoshi, T.; Nakama, Y.; Kurihara, M.; Suzuki, T.; Kitahara, Y.; Kitai, Y.; Nakamura, T.; Itokazu, D.; Miyazato, T. Cardiac auscultation skills among junior doctors: Effects of sound stimulation lesson. Int. J. Med. Educ. 2020, 11, 107–110. [Google Scholar] [CrossRef]
- Bradley, P. The history of simulation in medical education and possible future directions. Med. Educ. 2006, 40, 254–262. [Google Scholar] [CrossRef]
- Gordon, M.S.; Ewy, G.A.; DeLeon, A.C.; Waugh, R.A.; Felner, J.M.; Forker, A.D.; Gessner, I.H.; Mayer, J.W.; Patterson, D. “Harvey,” the cardiology patient simulator: Pilot studies on teaching effectiveness. Am. J. Cardiol. 1980, 45, 791–796. [Google Scholar] [CrossRef]
- Owen, H. Early Use of Simulation in Medical Education by the Society for Simulation in Healthcare. Simul Healthc. 2012, 7, 102–116. [Google Scholar] [CrossRef] [Green Version]
- Okuda, Y.; Bryson, E.O.; DeMaria, S.; Jacobson, L.; Quinones, J.; Shen, B.; Levine, A.I. The Utility of Simulation in Medical Education: What Is the Evidence? Mt. Sinai J. Med. A J. Transl. Pers. Med. 2009, 76, 330–343. [Google Scholar] [CrossRef]
- Nousiainen, M.T.; Caverzagie, K.J.; Ferguson, P.C.; Frank, J.R.; on behalf of the ICBME Collaborators. Implementing competency-based medical education: What changes in curricular structure and processes are needed? Med. Teach. 2017, 39, 594–598. [Google Scholar] [CrossRef]
- Pimmer, C.; Linxen, S.; Gröhbiel, U.; Jha, A.K.; Burg, G. Mobile learning in resource-constrained environments: A case study of medical education. Med. Teach. 2013, 35, 1157–1165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walsh, K. Mobile Learning in Medical Education: Review. Ethiop. J. Health Sci. 2015, 25, 363–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, B.S.; Rafique, J.; Vincent, T.R.; Fairclough, J.; Packer, M.H.; Vincent, R.; Haq, I. Mobile Medical Education (MoMEd)—How mobile information resources contribute to learning for undergraduate clinical students—A mixed methods study. BMC Med. Educ. 2012, 12, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chinelatto, L.A.; da Costa, T.R.; Medeiros, V.M.B.; Boog, G.H.P.; Hojaij, F.C.; Tempski, P.Z.; Martins, M.D.A. What You Gain and What You Lose in COVID-19: Perception of Medical Students on their Education. Clinics 2020, 75, e2133. [Google Scholar] [CrossRef]
- Kirk, L.E.; Mitchell, I. The impact of the COVID -19 pandemic on medical education. Med. J. Aust. 2020, 213. [Google Scholar] [CrossRef]
- Kho, A.; Henderson, L.E.; Dressler, D.D.; Kripalani, S. Use of handheld computers in medical education. J. Gen. Intern. Med. 2006, 21, 531–537. [Google Scholar] [CrossRef] [Green Version]
- Ruiz, J.G.; Mintzer, M.J.; Leipzig, R.M. The Impact of E-Learning in Medical Education. Acad. Med. 2006, 81, 207–212. [Google Scholar] [CrossRef]
- Atreya, A.; Acharya, J. Distant virtual medical education during COVID-19: Half a loaf of bread. Clin. Teach. 2020, 17, 418–419. [Google Scholar] [CrossRef]
- Sandars, J.; Patel, R. The challenge of online learning for medical education during the COVID-19 pandemic. Int. J. Med Educ. 2020, 11, 169–170. [Google Scholar] [CrossRef]

| Volunteers | ||
| Male, n (%) | 19 | (27.5) |
| Female, n (%) | 50 | (72.5) |
| Total, (sex ratio F/M) | 69 | (2.6) |
| Answered to the survey | ||
| Male, n (%) | 13 | (29.5) |
| Female, n (%) | 31 | (70.5) |
| Subtotal “n”, (% from volunteers) | 44 | (63.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prados-Carmona, A.; Fuentes-Jimenez, F.; Roman de los Reyes, R.; García-Rios, A.; Rioja-Bravo, J.; Herruzo-Gomez, E.; Perez-Martinez, P.; Lopez-Miranda, J.; Delgado-Lista, J. A Pilot Study on the Feasibility of Developing and Implementing a Mobile App for the Acquisition of Clinical Knowledge and Competencies by Medical Students Transitioning from Preclinical to Clinical Years. Int. J. Environ. Res. Public Health 2022, 19, 2777. https://doi.org/10.3390/ijerph19052777
Prados-Carmona A, Fuentes-Jimenez F, Roman de los Reyes R, García-Rios A, Rioja-Bravo J, Herruzo-Gomez E, Perez-Martinez P, Lopez-Miranda J, Delgado-Lista J. A Pilot Study on the Feasibility of Developing and Implementing a Mobile App for the Acquisition of Clinical Knowledge and Competencies by Medical Students Transitioning from Preclinical to Clinical Years. International Journal of Environmental Research and Public Health. 2022; 19(5):2777. https://doi.org/10.3390/ijerph19052777
Chicago/Turabian StylePrados-Carmona, Alvaro, Francisco Fuentes-Jimenez, Rafael Roman de los Reyes, Antonio García-Rios, Jesus Rioja-Bravo, Ezequiel Herruzo-Gomez, Pablo Perez-Martinez, Jose Lopez-Miranda, and Javier Delgado-Lista. 2022. "A Pilot Study on the Feasibility of Developing and Implementing a Mobile App for the Acquisition of Clinical Knowledge and Competencies by Medical Students Transitioning from Preclinical to Clinical Years" International Journal of Environmental Research and Public Health 19, no. 5: 2777. https://doi.org/10.3390/ijerph19052777
APA StylePrados-Carmona, A., Fuentes-Jimenez, F., Roman de los Reyes, R., García-Rios, A., Rioja-Bravo, J., Herruzo-Gomez, E., Perez-Martinez, P., Lopez-Miranda, J., & Delgado-Lista, J. (2022). A Pilot Study on the Feasibility of Developing and Implementing a Mobile App for the Acquisition of Clinical Knowledge and Competencies by Medical Students Transitioning from Preclinical to Clinical Years. International Journal of Environmental Research and Public Health, 19(5), 2777. https://doi.org/10.3390/ijerph19052777