Exploring the Peer Effect of Physicians’ and Patients’ Participation Behavior: Evidence from Online Health Communities
Abstract
:1. Introduction
1.1. Background
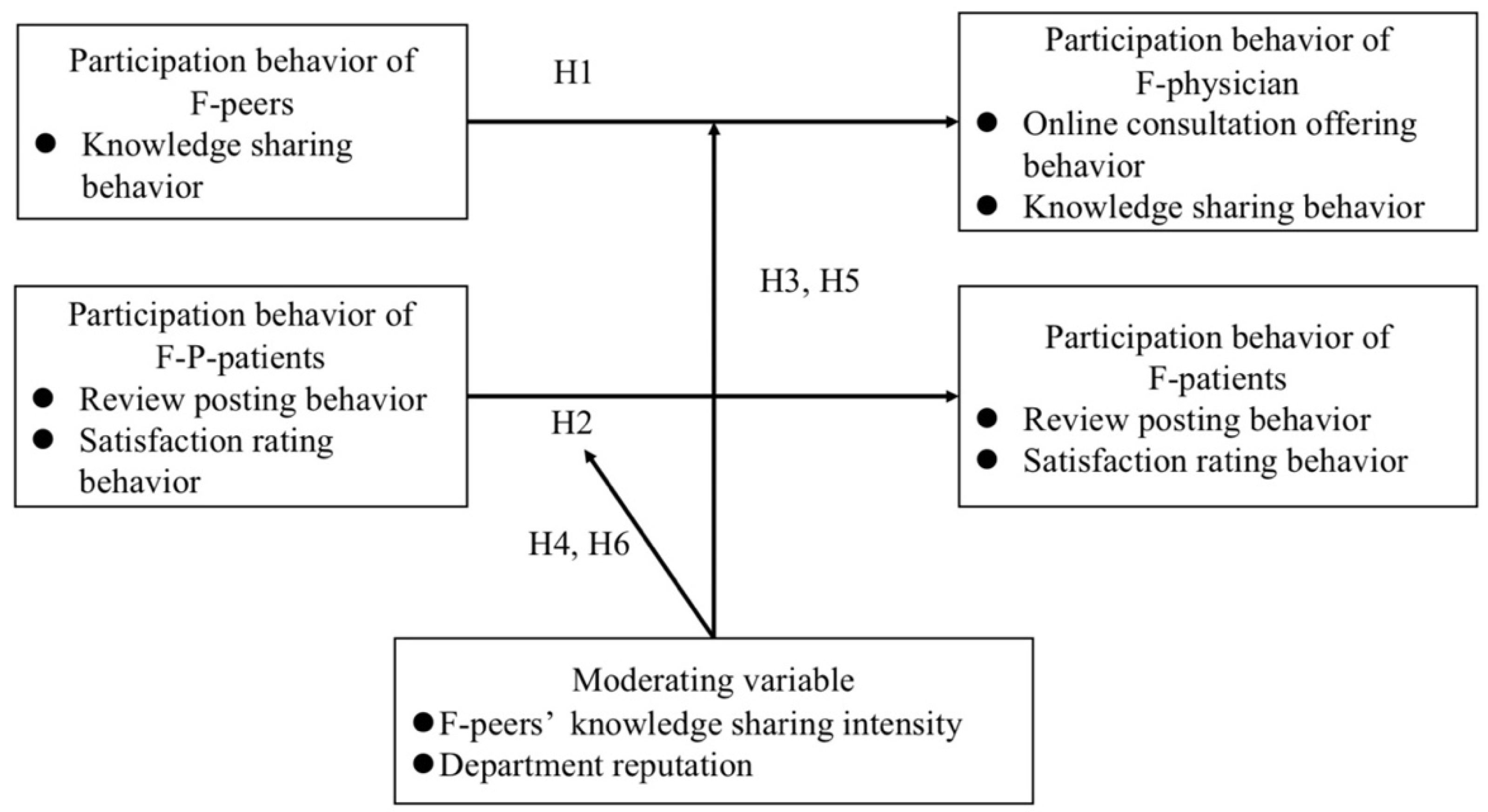
- RQ1: How does the participation behavior of F-peers affect the F-physician’s participation behavior?
- RQ2: How does the participation behavior of F-P-patients affect F-patients’ participation behavior?
- RQ3: How does the intensity of F-peers’ knowledge sharing behavior and the department reputation moderate the relationship between peers’ participation behavior and the participation behavior of the F-physician and F-patients?
1.2. Related Work
1.2.1. Physician Participation Behavior
1.2.2. Physician Participation Behavior
1.2.3. Peer Effect
1.3. Research Model and Hypotheses
1.3.1. Main Effect Analysis
1.3.2. Moderating Effect Analysis
2. Materials and Methods
2.1. Research Design
2.2. Data and Variables
2.3. Empirical Model
3. Results
3.1. Effect on the F-Physician and F-Patients
3.2. Moderation Effect on the F-Physician and F-Patients
3.3. Robust Test
4. Discussion
5. Conclusions
5.1. Research Contributions
5.2. Practical Implications
5.3. Limitations and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eysenbach, G. Medicine 2.0: Social networking, collaboration, participation, apomediation, and openness. J. Med. Internet Res. 2008, 10, e22. [Google Scholar] [CrossRef]
- Roettl, J.; Bidmon, S.; Terlutter, R. What predicts patients’ willingness to undergo online treatment and pay for online treatment? Results from a web-based survey to investigate the changing patient-physician relationship. J. Med. Internet Res. 2016, 18, e32. [Google Scholar] [CrossRef]
- Lin, M.; Hung, S.W.; Chen, C.J. Fostering the determinants of knowledge sharing in professional virtual communities. Comput. Hum. Behav. 2009, 25, 929–939. [Google Scholar] [CrossRef]
- Wu, H.; Lu, N. How your colleagues’ reputation impact your patients’ odds of posting experiences: Evidence from an online health community. Electron. Commer. Res. Appl. 2016, 16, 7–17. [Google Scholar] [CrossRef]
- Zhou, J.; Fan, T. Understanding the factors influencing patient E-health literacy in online health communities (OHCs): A social cognitive theory perspective. Int. J. Environ. Res. Public Health 2019, 16, 2455. [Google Scholar] [CrossRef] [Green Version]
- Yan, L.; Tan, Y. Feeling blue? Go online: An empirical study of social support among patients. Inf. Syst. Res. 2014, 25, 690–709. [Google Scholar] [CrossRef]
- Li, Y.; Yan, X. How could peers in online health community help improve health behavior. Int. J. Environ. Res. Public Health 2020, 17, 2995. [Google Scholar] [CrossRef]
- Koh, J.; Kim, Y.G.; Butler, B.; Bock, G.W. Encouraging participation in virtual communities. Commun. ACM 2007, 50, 68–73. [Google Scholar] [CrossRef]
- Chen, J.; Lan, Y.-C.; Chang, Y.-W.; Chang, P.-Y. Exploring doctors’ willingness to provide online counseling services: The roles of motivations and costs. Int. J. Environ. Res. Public Health 2020, 17, 110. [Google Scholar] [CrossRef] [Green Version]
- Wasko, M.M.; Faraj, S. Why should I share? Examining social capital and knowledge contribution in electronic networks of practice. MIS Q. 2005, 29, 35–57. [Google Scholar] [CrossRef]
- Shen, W.Q.; Hu, Y.J.; Ulmer, J.R. Competing for attention: An empirical study of online reviewers’ strategic behavior. MIS Q. 2015, 39, 683–696. [Google Scholar] [CrossRef]
- Goes, P.B.; Guo, C.; Lin, M. Do incentive hierarchies induce user effort? Evidence from an online knowledge exchange. Inf. Syst. Res. 2016, 27, 497–516. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Feng, Z. Group size and incentives to contribute: A natural experiment at Chinese wikipedia. Am. Econ. Rev. 2011, 101, 1601–1615. [Google Scholar] [CrossRef] [Green Version]
- Qiu, L.; Kumar, S. Understanding voluntary knowledge provision and content contribution through a social-media-based prediction market: A field experiment. Inf. Syst. Res. 2017, 28, 529–546. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, X.; Lee, P.K.C. Improving the effectiveness of online healthcare platforms: An empirical study with multi-period patient-doctor consultation data. Int. J. Prod. Econ. 2019, 207, 70–80. [Google Scholar] [CrossRef]
- Fei, L.; Li, Y.; Ju, X. Exploring patients’ consultation behaviors in the online health community: The role of disease risk. Telemed. e-Health 2018, 25, 213–220. [Google Scholar] [CrossRef]
- Jing, D.; Jin, Y.; Liu, J. The impact of monetary incentives on physician prosocial behavior in online medical consulting platforms: Evidence from China. J. Med. Internet Res. 2019, 21, e14685. [Google Scholar] [CrossRef]
- Sun, Y.; Dong, X.; Mcintyre, S. Motivation of user-generated content: Social connectedness moderates the effects of monetary rewards. Mark. Sci. 2017, 36, 329–337. [Google Scholar] [CrossRef]
- Meng, F.; Guo, X.; Peng, Z.; Lai, K.H.; Zhao, X. Investigating the adoption of mobile health services by elderly users: Trust transfer model and survey study. JMIR mHealth uHealth 2019, 7, e12269. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.; Zhang, X. Investigating the effect of paid and free feedback about physicians’ telemedicine services on patients’ and physicians’ behaviors: Panel data analysis. J. Med. Internet Res. 2019, 21, e12156. [Google Scholar] [CrossRef]
- Guo, S.S.; Guo, X.T.; Fang, Y.L.; Doug, V. How Doctors Gain Social and Economic Returns in Online Health-Care Communities: A Professional Capital Perspective. J. Manag. Inf. Syst. 2017, 34, 487–519. [Google Scholar] [CrossRef]
- Wang, J.N.; Chiu, Y.L.; Yu, H.; Hsu, Y.T. Understanding a nonlinear causal relationship between rewards and physicians’ contributions in online health care communities: Longitudinal study. J. Med. Internet Res. 2017, 19, e427. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Wang, T.; Chen, Y.; Zhang, H. Knowledge sharing in online health communities: A social exchange theory perspective. Inf. Manag. 2016, 53, 643–653. [Google Scholar] [CrossRef]
- Xz, A.; Feng, G.B.; Tx, C.; Yl, D. What motivates physicians to share free health information on online health platforms? Inf. Processing Manag. 2020, 57, 77–86. [Google Scholar] [CrossRef]
- Rupert, D.J.; Moultrie, R.R.; Read, J.G.; Amoozegar, J.B.; Bornkessel, A.S.; O’Donoghue, A.; Sullivan, H.W. Perceived healthcare provider reactions to patient and caregiver use of online health communities. Patient Educ. Couns. 2014, 96, 320–326. [Google Scholar] [CrossRef]
- Zhang, K.; Cheung, C.; Lee, M. Examining the moderating effect of inconsistent reviews and its gender differences on consumers’ online shopping decision. Int. J. Inf. Manag. 2014, 34, 89–98. [Google Scholar] [CrossRef]
- Verhoef, L.M.; Belt, T.; Engelen, L.J.; Schoonhoven, L.; Kool, R.B. Social media and rating sites as tools to understanding quality of care: A scoping review. J. Med. Internet Res. 2014, 16, e56. [Google Scholar] [CrossRef]
- Manstead, A.; Hewstone, M.; Fiske, S.T.; Hogg, M.A.; Reis, H.T.; Semin, G.R. The Blackwell Encyclopedia of Social Psychology; Blackwell Publishers: Hoboken, NJ, USA, 1995; ISBN 0631181466. [Google Scholar]
- Salvy, S.J.; Haye, K.; Bowker, J.C.; Hermans, R. Influence of peers and friends on children’s and adolescents’ eating and activity behaviors. Physiol. Behav. 2012, 106, 369–378. [Google Scholar] [CrossRef] [Green Version]
- Bapna, R.; Umyarov, A. Do your online friends make you pay? A randomized field experiment on peer influence in online social networks. Manag. Sci. 2015, 61, 1902–1920. [Google Scholar] [CrossRef] [Green Version]
- Uetake, K.; Yang, N. Inspiration from the ‘Biggest Loser’: Social Interactions in a Weight Loss Program. Mark. Sci. 2020, 39, 487–499. [Google Scholar] [CrossRef]
- Narayan, V.; Rao, V.R. How peer influence affects attribute preferences: A bayesian updating mechanism. Mark. Sci. 2011, 30, 368–384. [Google Scholar] [CrossRef]
- Feldman, J.M.; Lynch, J.G. Self-generated validity and other effects of measurement on belief, attitude, intention, and behavior. J. Appl. Psychol. 1988, 73, 421–435. [Google Scholar] [CrossRef]
- Roehm, M.L.; Tybout, A.M. When will a brand scandal spill over, and how should competitors respond? J. Mark. Res. 2006, 49, 312–318. [Google Scholar] [CrossRef]
- Festinger, L.A. A theory of social comparison processes. Hum. Relat. 1954, 7, 117–140. [Google Scholar] [CrossRef]
- Ambrose, S.C.; Matthews, L.M.; Rutherford, B.N. Cross-functional teams and social identity theory: A study of sales and operations planning (S&OP). J. Bus. Res. 2018, 92, 270–278. [Google Scholar] [CrossRef]
- Li, X.; Hitt, L.M. Self-selection and information role of online product reviews. Oper. Res. 2009, 19, 456–474. [Google Scholar] [CrossRef] [Green Version]
- Moe, W.W.; Trusov, M. The value of social dynamics in online product ratings forums. J. Mark. Res. 2011, 48, 444–456. [Google Scholar] [CrossRef]
- Tan, T.F.; Netessine, S. When you work with a superman, Will you also fly? An empirical study of the impact of coworkers on performance. Manag. Sci. 2019, 65, 3495–3517. [Google Scholar] [CrossRef]
- Spence, M. Job market signaling. Q. J. Econ. 1973, 87, 355–374. [Google Scholar] [CrossRef]
- Stiglitz, J.E. The theory the of “screening” education, and the distribution of income. Am. Econ. Rev. 1975, 65, 283–300. [Google Scholar]
- Gao, G.G.; Mccullough, J.S.; Agarwal, R.; Jha, A.K. A changing landscape of physician quality reporting: Analysis of patients’ online ratings of their physicians over a 5-year period. J. Med. Internet Res. 2012, 14, e38. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Li, H.; Shan, S. Understanding the health behavior decision-making process with situational theory of problem solving in online health communities: The effects of health beliefs, message source credibility, and communication behaviors on health behavioral intention. Int. J. Environ. Res. Public Health 2021, 18, 4488. [Google Scholar] [CrossRef] [PubMed]
- Yong, L. Word of mouth for movies: Its dynamics and impact on box office revenue. J. Mark. 2006, 70, 74–89. [Google Scholar] [CrossRef]
- Mayzlin, D. Promotional chat on the Internet. Mark. Sci. 2006, 25, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Wang, M.-Y.; Zhang, P.-Z.; Zhou, C.-Y.; Lai, N.-Y. Effect of emotion, expectation, and privacy on purchase intention in WeChat health product consumption: The mediating role of trust. Int. J. Environ. Res. Public Health 2019, 16, 3861. [Google Scholar] [CrossRef] [Green Version]
- Kumar, N.; Qiu, L.; Kumar, S. Exit, voice, and response on digital platforms. Inf. Syst. Res. 2018, 29, 849–870. [Google Scholar] [CrossRef]
- Dranove, D.; Mazzeo, G. Differentiation and Competition in HMO Markets. J. Ind. Econ. 2003, 51, 433–454. [Google Scholar] [CrossRef]
- Le, W.; Chang, P.-Y.; Chang, Y.-W.; Chen, J. Why do patients move from online health platforms to hospitals? The perspectives of fairness theory and brand extension theory. Int. J. Environ. Res. Public Health 2019, 16, 3755. [Google Scholar] [CrossRef] [Green Version]
- Hajli, M.N.; Sims, J.; Featherman, M.; Love, P. Credibility of information in online communities. J. Strateg. Mark. 2015, 23, 238–253. [Google Scholar] [CrossRef]
- Lu, N.; Hong, W. Exploring the impact of word-of-mouth about physicians’ service quality on patient choice based on online health communities. BMC Med. Inform. Decis. Mak. 2016, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]

| Variable | Definition | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Dependent Variable | |||||
| Consultit | Number of online consultations for a physician i in month t. | 8.163 | 32.851 | 0 | 4236 |
| Art_Nmit | Number of scientific articles published for a physician i in month t. | 0.183 | 2.307 | 0 | 217 |
| Com_Allit | Total number of reviews for a physician i in month t. | 1.21 | 4.681 | 0 | 135 |
| S_Allit | Average satisfaction of reviews for a physician i in month t. | 1.353 | 1.667 | 0 | 4 |
| Independent Variable | |||||
| Pr_Artit−1 | Binary variable equals to 1 if peer of a physician i published articles in month t−1; otherwise it equals 0. | 0.245 | 0.43 | 0 | 1 |
| P_Allit−1 | Average number of services reviews for peer of a physician i in month t−1. | 0.733 | 1.728 | 0 | 78 |
| P_Qit−1 | Average satisfaction of services reviews for peer of a physician i in month t−1. | 0.796 | 0.787 | 0 | 4 |
| Control Variable | |||||
| Self_Artit−1 | Binary variable equals to 1 if a physician i published articles in month t−1; otherwise it equals 0. | 0.047 | 0.211 | 0 | 1 |
| Comtit−1 | Total number of online services reviews for a physician i in month t−1. | 16.515 | 70.583 | 0 | 1543 |
| Cmt_Qit−1 | Average satisfaction of online services reviews for a physician i in month t−1. | 0.376 | 0.478 | 0 | 1 |
| Voteit−1 | Total number of offline services reviews for a physician i in month t−1. | 28.851 | 77.357 | 0 | 1400 |
| Vote_Qit−1 | Average satisfaction of offline services evaluations for a physician i in month t−1. | 0.976 | 1.386 | 0 | 3 |
| Hypothesis 1a | Hypothesis 1b | |||
|---|---|---|---|---|
| Variable | M1 | M2 | M1 | M2 |
| Self_Artit−1 | 0.363 *** | 0.361 *** | ||
| (22.56) | (22.46) | |||
| p < 0.001 | p < 0.001 | |||
| Comtit−1 | −0.002 *** | −0.002 *** | −0.006 *** | −0.006 *** |
| (−3.66) | (−3.62) | (−3.77) | (−3.73) | |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | |
| Cmt_Qit−1 | 0.058 *** | 0.058 *** | 0.073 | 0.072 |
| (4.42) | (4.40) | (1.58) | (1.56) | |
| p < 0.001 | p < 0.001 | p = 0.114 | p = 0.119 | |
| Voteit−1 | 0.001 *** | 0.002 *** | 0.004 ** | 0.004 ** |
| (2.63) | (2.67) | (2.04) | (2.07) | |
| p = 0.008 | p = 0.007 | p = 0.041 | p = 0.038 | |
| Vote_Qit−1 | 0.041 *** | 0.041 *** | 0.007 | 0.008 |
| (8.80) | (8.88) | (0.44) | (0.51) | |
| p < 0.001 | p < 0.001 | p = 0.660 | p = 0.610 | |
| Pr_Artit−1 | 0.039 *** | 0.120 *** | ||
| (4.26) | (3.74) | |||
| p < 0.001 | p < 0.001 | |||
| Constant | 0.943 *** | 0.932 *** | 0.134 *** | 0.101 *** |
| (68.63) | (66.77) | (2.77) | (2.05) | |
| p < 0.001 | p < 0.001 | p = 0.006 | p = 0.040 | |
| Observations | 39,564 | 39,564 | 39,564 | 39,564 |
| R-squared | 0.824 | 0.824 | 0.328 | 0.328 |
| Number of ID | 3297 | 3297 | 3297 | 3297 |
| Hypothesis 2a | Hypothesis 2b | |||
|---|---|---|---|---|
| Variable | M1 | M2 | M1 | M2 |
| Art_Nmit−1 | 0.018 *** | 0.018 *** | 0.002 | 0.002 |
| (3.48) | (3.44) | (1.16) | (1.19) | |
| p < 0.001 | p < 0.001 | p = 0.246 | p = 0.234 | |
| Consultit−1 | 0.014 *** | 0.014 *** | 0.0004 *** | 0.0004 ** |
| (31.21) | (31.09) | (2.66) | (2.46) | |
| p < 0.001 | p < 0.001 | p = 0.008 | p = 0.014 | |
| P_Allit−1 | 0.114 *** | 0.019 *** | ||
| (6.64) | (3.02) | |||
| p < 0.001 | p = 0.003 | |||
| P_Qit−1 | 0.159 *** | 0.190 *** | ||
| (3.91) | (13.03) | |||
| p < 0.001 | p < 0.001 | |||
| Constant | 1.046 *** | 0.901 *** | 0.685 *** | 0.594 *** |
| (29.95) | (22.38) | (54.65) | (41.18) | |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | |
| Observations | 39,564 | 39,564 | 39,564 | 39,564 |
| R-squared | 0.030 | 0.032 | 0.236 | 0.240 |
| Number of ID | 3297 | 3297 | 3297 | 3297 |
| Variable | Obs | Mean | Std. Dev. | Variance | Skew. | Kurt. |
|---|---|---|---|---|---|---|
| Art_Nmit | 39564 | 0.183 | 2.307 | 5.322 | 51.919 | 3867.941 |
| Consultit | 39564 | 8.163 | 32.851 | 1079.208 | 57.297 | 6964.579 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yin, Q.; Fan, H.; Wang, Y.; Guo, C.; Cui, X. Exploring the Peer Effect of Physicians’ and Patients’ Participation Behavior: Evidence from Online Health Communities. Int. J. Environ. Res. Public Health 2022, 19, 2780. https://doi.org/10.3390/ijerph19052780
Yin Q, Fan H, Wang Y, Guo C, Cui X. Exploring the Peer Effect of Physicians’ and Patients’ Participation Behavior: Evidence from Online Health Communities. International Journal of Environmental Research and Public Health. 2022; 19(5):2780. https://doi.org/10.3390/ijerph19052780
Chicago/Turabian StyleYin, Qiuju, Haoyue Fan, Yijie Wang, Chenxi Guo, and Xingzhi Cui. 2022. "Exploring the Peer Effect of Physicians’ and Patients’ Participation Behavior: Evidence from Online Health Communities" International Journal of Environmental Research and Public Health 19, no. 5: 2780. https://doi.org/10.3390/ijerph19052780
APA StyleYin, Q., Fan, H., Wang, Y., Guo, C., & Cui, X. (2022). Exploring the Peer Effect of Physicians’ and Patients’ Participation Behavior: Evidence from Online Health Communities. International Journal of Environmental Research and Public Health, 19(5), 2780. https://doi.org/10.3390/ijerph19052780







