Evaluating Completeness of Foodborne Outbreak Reporting in the United States, 1998–2019
Abstract
:1. Introduction
2. Methods
2.1. Data Source
2.2. Data Preparation
- 26 variables generated by CDC personnel to track the reporting of electronic records (e.g., data recorder ID, local report date, CDC report date, etc.);
- 12 variables providing reporter contact information and optional comments written during reporting (e.g., recall comments, agency title, reporting site, etc.);
- 9 variables providing clarification responses to specific questions asked only for specific outbreaks (e.g., clarification of supply chain stage of contamination, questions regarding antimicrobial resistance testing, etc.); and
- 17 variables unavailable for the entire study period duration (e.g., illness attack rate, percentage of illnesses by age group, food contaminant infecting exposed persons, age percentage, etc.).
2.3. Crude Completeness Estimation
2.4. Measuring Temporal Changes in Completeness
2.5. Temporal Trend Analyses
3. Results
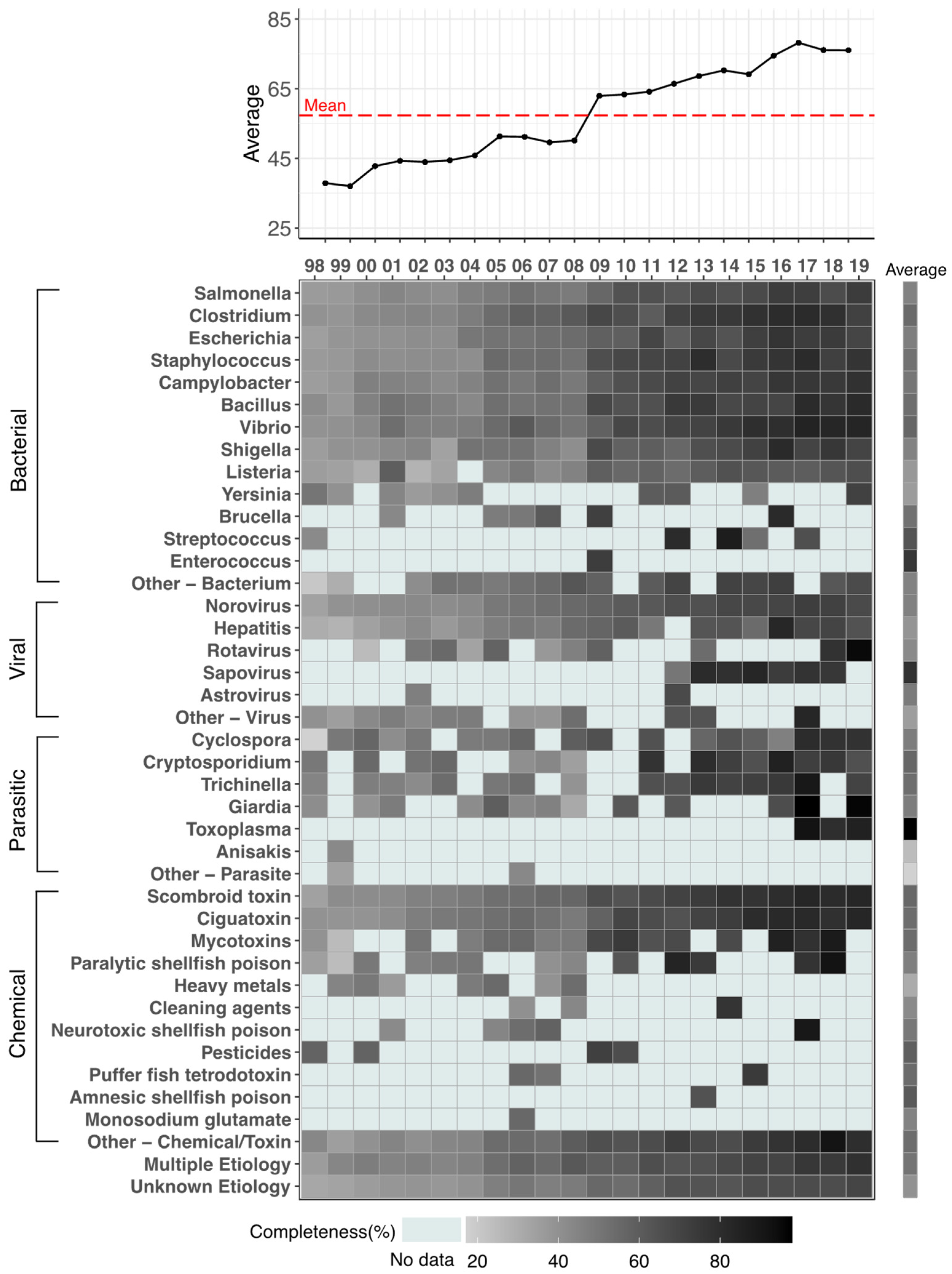
3.1. Outbreak Frequency and Completeness by Pathogen
3.2. Annual Completeness
3.3. Segemented and Seasonality Trend Analyses
4. Discussion
- Create a Standard Operating Procedure (SOP) to identify must-have variables, variables that are related to one another, and less-relevant variables. This SOP can assist in the streamlining of data cleaning procedures to identify true missingness, zero values, and information that is not applicable for an outbreak. Moreover, SOP can be used as a guideline to create NORS checkpoints to avoid missing information between related variables.
- Consider removing variables with consistently low completeness or conduct thorough investigation into the obstacles preventing adequate reporting these variables.
- Publicly report documentation explaining reasons for incomplete data; NORS has a rigorous data cleaning process that includes 30+ checkpoints for foodborne outbreaks. Outbreak data are reported as missing until all issues are solved [52]. Although incomplete outbreak reports cannot provide all information, these checkpoints and their completion may still be useful for researchers to study.
- In accordance with the Population Health Surveillance Theory, perform periodic system audits to evaluate data reporting procedure and data quality at the local level [53]. In addition, these periodic system audits can be used as an assessment to evaluate both workforce resource and laboratory testing capacities. For any local agency with low audit scores, the CDC can provide training materials, or relocate necessary recourses.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC). Foodborne Illnesses and Germs. Available online: http://www.cdc.gov/foodsafety/foodborne-germs.html (accessed on 30 November 2021).
- Tack, D.M. Preliminary Incidence and Trends of Infections with Pathogens Transmitted Commonly Through Food—Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2016–2019. Morb. Mortal. Wkly. Rep. 2020, 69, 509–514. [Google Scholar] [CrossRef] [PubMed]
- United States Food and Drug Association (FDA). Most Common Foodborne Illnesses; United States Department of Health and Human Services: Washington, DC, USA. Available online: https://www.fda.gov/files/food/published/Most-Common-Foodborne-Illnesses-%28PDF%29.pdf (accessed on 1 September 2021).
- United States Food and Drug Association (FDA). What You Need to Know About Foodborne Illnesses. United States Department of Health and Human Services. Available online: https://www.fda.gov/food/consumers/what-you-need-know-about-foodborne-illnesses (accessed on 1 September 2021).
- Centers for Disease Control and Prevention (CDC); Office of Public Health Scientific Services (OPHSS); Center for Surveillance, Epidemiology, and Laboratory Services (CSELS); Division of Health Informatics and Surveillance (DHIS). Surveillance Case Definitions for Current and Historical Conditions. National Notifiable Diseases Surveillance System (NNDSS). Available online: https://wwwn.cdc.gov/nndss/conditions/ (accessed on 1 September 2021).
- Centers for Disease Control and Prevention (CDC). Burden of Foodborne Illness: Findings. Available online: http://www.cdc.gov/foodborneburden/2011-foodborne-estimates.html (accessed on 1 August 2021).
- U.S. Department of Agriculture Economic Research Service (USDA ERS). Cost Estimates of Foodborne Illnesses. Available online: https://www.ers.usda.gov/data-products/cost-estimates-of-foodborne-illnesses/ (accessed on 1 August 2021).
- Hoffmann, S.; Batz, M.B.; Morris, J.G. Annual Cost of Illness and Quality-Adjusted Life Year Losses in the United States Due to 14 Foodborne Pathogens. J. Food Prot. 2012, 75, 1292–1302. [Google Scholar] [CrossRef] [PubMed]
- Rolka, H.; Walker, D.W.; English, R.; Katzoff, M.J.; Scogin, G.; Neuhaus, E. Analytical Challenges for Emerging Public Health Surveillance. Morb. Mortal. Wkly. Rep. 2012, 61, 35–40. [Google Scholar]
- George, J.; Häsler, B.; Mremi, I.; Sindato, C.; Mboera, L.; Rweyemamu, M.; Mlangwa, J. A Systematic Review on Integration Mechanisms in Human and Animal Health Surveillance Systems with a View to Addressing Global Health Security Threats. One Health Outlook 2020, 2, 11. [Google Scholar] [CrossRef]
- Gkogka, E.; Reij, M.W.; Havelaar, A.H.; Zwietering, M.H.; Gorris, L.G.M. Risk-based Estimate of Effect of Foodborne Diseases on Public Health, Greece. Emerg. Infect. Dis. 2011, 17, 9. [Google Scholar] [CrossRef] [Green Version]
- Lee, B. Foodborne Disease and the Need for Greater Foodborne Disease Surveillance in the Caribbean. Vet. Sci. 2017, 4, 40. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention (CDC). Outbreaks of Foodborne Illness. Available online: https://www.fda.gov/food/recalls-outbreaks-emergencies/outbreaks-foodborne-illness (accessed on 1 September 2021).
- Centers for Disease Control and Prevention (CDC). About National Outbreak Reporting System (NORS). Available online: http://www.cdc.gov/nors/about.html (accessed on 1 September 2021).
- Centers for Disease Control and Prevention (CDC). Other Systems Linked to National Outbreak Reporting System (NORS). Available online: http://www.cdc.gov/nors/other-systems.html (accessed on 1 September 2021).
- Centers for Disease Control and Prevention (CDC). NORSDirect—National Outbreak Reporting System (NORS). Available online: http://www.cdc.gov/nors/norsdirect.html (accessed on 1 September 2021).
- Menachemi, N.; Collum, T.H. Benefits and drawbacks of electronic health record systems. Risk Manag. Healthc. Policy 2011, 4, 47–55. [Google Scholar] [CrossRef] [Green Version]
- Arendt, S.; Rajagopal, L.; Strohbehn, C.; Stokes, N.; Meyer, J.; Mandernach, S. Reporting of Foodborne Illness by U.S. Consumers and Healthcare Professionals. Int. J. Environ. Res. 2013, 10, 3684–3714. [Google Scholar] [CrossRef] [Green Version]
- Institute of Medicine. Addressing Foodborne Threats to Health: Policies, Practices, and Global Coordination: Workshop Summary. In Investigating Foodborne Threats; Institute of Medicine (US) Forum on Microbial Threats, National Academies Press (US): Washington, DC, USA, 2006; pp. 70–91. ISBN 0-309-65457-2. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Diagnosis and Management of Foodborne Illnesses—A Primer for Physicians and Other Health Care Professionals. Morb. Mortal. Wkly. Rep. 2004, 53, 1–32. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Lesson 5: Public Health Surveillance, Appendix E. Limitation of Notifiable Disease Surveillance and Recommendations for Improvement. Principles of Epidemiology. Available online: http://www.cdc.gov/csels/dsepd/ss1978/lesson5/appendixe.html (accessed on 5 September 2021).
- Centers for Disease Control and Prevention (CDC). Investigating Outbreaks. Foodborne Outbreaks. Available online: http://www.cdc.gov/foodsafety/outbreaks/investigating-outbreaks/index.html (accessed on 5 September 2021).
- Costard, S.; Espejo, L.; Groenendaal, H.; Zagmutt, F.J. Outbreak-Related Disease Burden Associated with Consumption of Unpasteurized Cow’s Milk and Cheese, United States, 2009–2014. Emerg. Infect. Dis. 2017, 23, 957–964. [Google Scholar] [CrossRef]
- Hall, A.J.; Wikswo, M.E.; Manikonda, K.; Roberts, V.A.; Yoder, J.S.; Gould, L.H. Acute Gastroenteritis Surveillance through the National Outbreak Reporting System, United States. Emerg. Infect. Dis. 2013, 19, 1305–1309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steele, M.K.; Wikswo, M.E.; Hall, A.J.; Koelle, K.; Handel, A.; Levy, K.; Waller, L.A.; Lopman, B.A. Characterizing Norovirus Transmission from Outbreak Data, United States. Emerg. Infect. Dis. 2020, 26, 1818–1825. [Google Scholar] [CrossRef] [PubMed]
- Lawpoolsri, S.; Kaewkungwal, J.; Khamsiriwatchara, A.; Sovann, L.; Sreng, B.; Phommasack, B.; Kitthiphong, V.; Lwin Nyein, S.; Win Myint, N.; Dang Vung, N.; et al. Data Quality and Timeliness of Outbreak Reporting System among Countries in Greater Mekong Subregion: Challenges for International Data Sharing. PLoS Negl. Trop. Dis. 2018, 12, e0006425. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, K.; Gasparrini, A.; Hajat, S.; Smeeth, L.; Armstrong, B. Time Series Regression Studies in Environmental Epidemiology. Int. J. Epidemiol. 2013, 42, 1187–1195. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). National Outbreak Reporting System (NORS) Dashboard. Available online: https://wwwn-cdc-gov.ezproxy.library.tufts.edu/norsdashboard/ (accessed on 4 March 2021).
- Mor, S.M.; DeMaria, A., Jr.; Naumova, E.N. Hospitalization Records as a Tool for Evaluating Performance of Food- and Water-Borne Disease Surveillance Systems: A Massachusetts Case Study. PLoS ONE 2014, 9, e93744. [Google Scholar] [CrossRef]
- Gould, L.H.; Mungai, E.A.; Johnson, S.D.; Richardson, L.C.; Williams, I.T.; Griffin, P.M.; Cole, D.J.; Hall, A.J. Surveillance for Foodborne Disease Outbreaks—United States, 2009–2010. Morb. Mortal. Wkly. Rep. 2013, 62, 41–47. [Google Scholar]
- Izzo, M.; Kirkland, P.; Mohler, V.; Perkins, N.; Gunn, A.; House, J. Prevalence of Major Enteric Pathogens in Australian Dairy Calves with Diarrhea. Aust. Vet. J. 2011, 89, 167–173. [Google Scholar] [CrossRef]
- Dong, H.T.; Nguyen, V.V.; Le, H.D.; Sangsuriya, P.; Jitrakorn, S.; Saksmerprome, V.; Senapin, S.; Rodkhum, C. Naturally Concurrent Infections of Bacterial and Viral Pathogens in Disease Outbreaks in Cultured Nile Tilapia (Oreochromis niloticus) Farms. Aquaculture 2015, 448, 427–435. [Google Scholar] [CrossRef]
- Simpson, R.B.; Zhou, B.; Naumova, E.N. Seasonal synchronization of foodborne outbreaks in the United States, 1996–2017. Sci. Rep. 2020, 10, 17500. [Google Scholar] [CrossRef]
- Wenger, J.B.; Naumova, E.N. Seasonal Synchronization of Influenza in the United States Older Adult Population. PLoS ONE 2010, 5, e10187. [Google Scholar] [CrossRef]
- Lofgren, E.T.; Wenger, J.B.; Fefferman, N.H.; Bina, D.; Gradus, S.; Bhattacharyya, S.; Naumov, Y.N.; Gorski, J.; Naumova, E.N. Disproportional Effects in Populations of Concern for Pandemic Influenza: Insights from Seasonal Epidemics in Wisconsin, 1967–2004. Influenza Other Respir. Viruses 2010, 4, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Chui, K.K.H.; Jagai, J.S.; Griffiths, J.K.; Naumova, E.N. Hospitalization of the Elderly in the United States for Nonspecific Gastrointestinal Diseases: A Search for Etiological Clues. Am. J. Public Health 2011, 101, 2082–2086. [Google Scholar] [CrossRef] [PubMed]
- Jagai, J.S.; Sarkar, R.; Castronovo, D.; Kattula, D.; McEntee, J.; Ward, H.; Kang, G.; Naumova, E.N. Seasonality of Rotavirus in South Asia: A Meta-Analysis Approach Assessing Associations with Temperature, Precipitation, and Vegetation Index. PLoS ONE 2012, 7, e38168. [Google Scholar] [CrossRef]
- Jagai, J.S.; Castronovo, D.A.; Monchak, J.; Naumova, E.N. Seasonality of Cryptosporidiosis: A Meta-Analysis Approach. Environ. Res. 2009, 109, 465–478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naumova, E.N.; Jagai, J.S.; Matyas, B.; DeMaria, A.; MacNeill, I.B.; Griffiths, J.K. Seasonality in Six Enterically Transmitted Diseases and Ambient Temperature. Epidemiol. Infect. 2007, 135, 281–292. [Google Scholar] [CrossRef]
- Alarcon Falconi, T.M.; Estrella, B.; Sempértegui, F.; Naumova, E.N. Effects of Data Aggregation on Time Series Analysis of Seasonal Infections. Int. J. Environ. Res. Public Health 2020, 17, 5887. [Google Scholar] [CrossRef]
- Nygren, B.L.; Schilling, K.A.; Blanton, E.M.; Silk, B.J.; Cole, D.J.; Mintz, E.D. Foodborne Outbreaks of Shigellosis in the USA, 1998–2008. Epidemiol. Infect. 2013, 141, 233–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Middaugh, J.P.; Hammond, R.M.; Eisenstein, L.; Lazensky, R. Using the Electronic Foodborne Outbreak Reporting System (EFORS) to Improve Foodborne Outbreak Surveillance, Investigations, and Program Evaluation. J. Environ. Health 2010, 73, 8–11. [Google Scholar]
- David, S.D.; Katz, R.L. Navigating the Legal Framework for State Foodborne Illness Surveillance and Outbreak Response: Observations and Challenges. J. Law Med. Ethics 2013, 41 (Suppl. 1), 28–32. [Google Scholar] [CrossRef]
- Painter, J.A.; Hoekstra, R.M.; Ayers, T.; Tauxe, R.V.; Braden, C.R.; Angulo, F.J.; Griffin, P.M. Attribution of Foodborne Illnesses, Hospitalizations, and Deaths to Food Commodities by Using Outbreak Data, United States, 1998–2008. Emerg. Infect Dis. 2013, 19, 407–415. [Google Scholar] [CrossRef]
- O’Neil, E.A.; Naumova, E.N. Defining Outbreak: Breaking Out of Confusion. J. Public Health Policy 2007, 28, 442–455. [Google Scholar] [CrossRef]
- Dewey-Mattia, D.; Kisselburgh, H.; Manikonda, K.; Silver, R.; Subramhanya, S.; Sundararaman, P.; Whitham, H.; Crowe, S. Surveillance for Foodborne Disease Outbreaks, United States, 2017 Annual Report. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3647642/ (accessed on 1 December 2021).
- Jones, T.F.; Yackley, J. Foodborne Disease Outbreaks in the United States: A Historical Overview. Foodborne Pathog. Dis. 2018, 15, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Lynch, M.; Painter, J.; Woodruff, R.; Braden, C. Surveillance for Foodborne-Disease Outbreaks—United States, 1998—2002. Morb. Mortal. Wkly. Rep. 2006, 55, 1–42. [Google Scholar]
- Biggerstaff, G. Improving Response to Foodborne Disease Outbreaks in the United States: Findings of the Foodborne Disease Centers for Outbreak Response Enhancement (FoodCORE), 2010–2012. J. Public Health Manag. Pract. 2015, 21, E18–E26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebel, E.D.; Williams, M.S.; Cole, D.; Travis, C.C.; Klontz, K.C.; Golden, N.J.; Hoekstra, R.M. Comparing Characteristics of Sporadic and Outbreak-Associated Foodborne Illnesses, United States, 2004–2011. Emerg. Infect. Dis. 2016, 22, 1193–1200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scharff, R.L.; Besser, J.; Sharp, D.J.; Jones, T.F.; Peter, G.-S.; Hedberg, C.W. An Economic Evaluation of PulseNet. Am. J. Prev. Med. 2016, 50, 66–73. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention (CDC). National Outbreak Reporting System (NORS) Training Materials. Available online: http://www.cdc.gov/nors/training/index.html (accessed on 1 December 2021).
- El Allaki, F.; Bigras-Poulin, M.; Michel, P.; Ravel, A. A Population Health Surveillance Theory. Epidemiol. Health 2012, 34, e2012007. [Google Scholar] [CrossRef]


| Contaminant Name | Number of Outbreaks | Crude Completeness | Completeness Category | |||||
|---|---|---|---|---|---|---|---|---|
| per Outbreak | per Variable | 1 | 2 | 3 | 4 | 5 | ||
| All Outbreaks | 22,792 | 59.45 | 53.65 | 98.45 | 81.00 | 52.48 | 29.01 | 14.46 |
| Multiple Etiologies | 779 | 64.54 | 60.19 | 98.61 | 87.72 | 60.09 | 34.91 | 25.56 |
| Unknown Etiologies | 7401 | 51.22 | 46.06 | 96.42 | 75.19 | 40.60 | 18.46 | 7.60 |
| Bacterial Pathogens | ||||||||
| Salmonella | 2872 | 58.94 | 53.90 | 97.16 | 77.20 | 52.12 | 27.08 | 22.41 |
| Clostridium | 944 | 62.37 | 56.90 | 98.83 | 85.91 | 59.62 | 32.99 | 13.91 |
| Escherichia | 649 | 58.69 | 56.18 | 97.69 | 75.28 | 51.29 | 30.69 | 32.07 |
| Staphylococcus | 625 | 56.02 | 49.69 | 98.84 | 78.39 | 48.04 | 21.57 | 9.29 |
| Campylobacter | 510 | 62.93 | 58.76 | 98.25 | 83.53 | 60.44 | 39.52 | 18.61 |
| Bacillus | 376 | 59.69 | 53.95 | 98.30 | 82.50 | 55.27 | 31.13 | 9.84 |
| Vibrio | 220 | 67.38 | 66.18 | 98.09 | 84.57 | 64.32 | 44.25 | 27.67 |
| Shigella | 195 | 53.61 | 48.23 | 97.08 | 74.77 | 46.32 | 18.78 | 7.92 |
| Listeria | 95 | 57.63 | 52.45 | 97.49 | 68.12 | 44.18 | 34.81 | 17.79 |
| Yersinia | 17 | 50.83 | 49.33 | 97.15 | 69.75 | 38.69 | 17.23 | 10.11 |
| Brucella | 6 | 61.39 | 59.13 | 99.07 | 78.57 | 63.96 | 32.14 | 6.25 |
| Streptococcus | 5 | 65.87 | 65.90 | 100.00 | 79.05 | 69.25 | 45.71 | 23.75 |
| Enterococcus | 1 | 74.42 | 73.03 | 100.00 | 100.00 | 85.00 | 57.14 | 6.25 |
| Other—Bacterium | 138 | 57.87 | 54.66 | 98.00 | 88.34 | 51.53 | 27.83 | 10.55 |
| Subtotal | 6653 | 59.55 | 54.59 | 97.81 | 79.40 | 53.59 | 29.31 | 19.54 |
| Viral Pathogens | ||||||||
| Norovirus | 6416 | 60.36 | 54.54 | 98.52 | 85.03 | 56.77 | 25.19 | 13.90 |
| Hepatitis | 103 | 47.08 | 44.13 | 96.55 | 62.23 | 34.07 | 19.73 | 8.00 |
| Rotavirus | 15 | 55.54 | 52.22 | 97.01 | 76.83 | 48.11 | 23.67 | 13.33 |
| Sapovirus | 15 | 73.41 | 66.79 | 96.30 | 91.75 | 67.84 | 33.33 | 42.75 |
| Astrovirus | 2 | 58.43 | 57.02 | 100.00 | 88.10 | 51.25 | 17.86 | 9.38 |
| Other—Virus | 102 | 45.59 | 38.64 | 97.26 | 67.65 | 29.86 | 2.84 | 0.88 |
| Subtotal | 6653 | 59.95 | 54.11 | 98.46 | 84.41 | 56.01 | 24.77 | 13.68 |
| Parasitic Pathogens | ||||||||
| Cyclospora | 112 | 70.58 | 72.49 | 98.54 | 85.63 | 67.79 | 62.10 | 46.95 |
| Cryptosporidium | 32 | 61.59 | 60.36 | 96.30 | 78.13 | 59.90 | 32.59 | 21.48 |
| Trichinella | 23 | 62.58 | 61.01 | 97.54 | 84.89 | 55.04 | 41.30 | 13.32 |
| Giardia | 22 | 53.63 | 48.42 | 98.94 | 71.65 | 45.70 | 13.86 | 10.43 |
| Toxoplasma | 3 | 85.37 | 85.86 | 100.00 | 100.00 | 88.75 | 76.19 | 56.25 |
| Anisakis | 1 | 44.57 | 43.07 | 100.00 | 57.14 | 36.67 | 7.14 | 0.00 |
| Other—Parasite | 2 | 41.96 | 38.86 | 100.00 | 52.38 | 27.92 | 0.00 | 0.00 |
| Subtotal | 195 | 66.05 | 64.10 | 98.15 | 82.47 | 61.69 | 43.00 | 33.32 |
| Chemicals and Toxins | ||||||||
| Scombroid toxin/ Histamine | 505 | 58.51 | 55.08 | 98.31 | 83.88 | 48.66 | 29.48 | 12.13 |
| Ciguatoxin | 349 | 61.97 | 59.12 | 98.74 | 84.84 | 49.61 | 41.98 | 13.39 |
| Mycotoxins | 35 | 62.78 | 57.25 | 98.24 | 88.03 | 58.27 | 26.57 | 10.59 |
| Paralytic shellfish poison | 17 | 56.43 | 54.45 | 94.77 | 80.95 | 44.94 | 25.63 | 11.40 |
| Heavy metals | 9 | 51.10 | 44.35 | 100.00 | 79.37 | 35.94 | 4.44 | 0.00 |
| Cleaning agents | 8 | 57.72 | 55.35 | 100.00 | 70.24 | 54.43 | 33.93 | 5.47 |
| Neurotoxic shellfish poison | 7 | 57.44 | 54.86 | 100.00 | 82.31 | 46.99 | 17.35 | 10.71 |
| Pesticides | 4 | 64.24 | 63.20 | 100.00 | 95.24 | 70.00 | 28.57 | 1.56 |
| Puffer fish tetrodotoxin | 3 | 62.65 | 60.54 | 99.79 | 92.06 | 57.92 | 33.33 | 2.08 |
| Amnesic shellfish poison | 1 | 66.57 | 64.33 | 100.00 | 95.24 | 51.25 | 57.14 | 6.25 |
| Monosodium glutamate (MSG) | 1 | 57.36 | 55.43 | 100.00 | 95.24 | 56.67 | 0.00 | 0.00 |
| Other—Chemical/Toxin | 172 | 56.37 | 50.73 | 98.65 | 83.19 | 47.95 | 23.76 | 7.83 |
| Subtotal | 1111 | 59.34 | 53.09 | 98.49 | 84.10 | 48.81 | 30.38 | 11.26 |
| Yearly % Change (eFORS) | Monthly Outbreaks Jan’09 | Yearly % Change (NORS) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | Estimate | LCI | UCI | Estimate | LCI | UCI | Estimate | LCI | UCI |
| All pathogens | −0.048 ** | −0.060 | −0.036 | 75.25 | 71.27 | 79.45 | −0.0024 | −0.012 | 0.012 |
| Norovirus | 0.048 ** | 0.024 | 0.060 | 30.01 | 26.47 | 34.01 | −0.036 ** | −0.06 | −0.012 |
| Salmonella | −0.012 | −0.036 | 0.000 | 9.96 | 8.82 | 11.24 | 0.012 | 0.000 | 0.036 |
| Clostridium | −0.048 ** | −0.072 | −0.024 | 3.18 | 2.76 | 3.64 | −0.0036 | −0.024 | 0.024 |
| Unknown Etiology | −0.096 ** | −0.108 | −0.084 | 21.92 | 20.36 | 23.61 | −0.036 ** | −0.048 | −0.024 |
| Multiple Etiology † | −0.048 ** | −0.072 | −0.012 | 2.47 | 2.07 | 2.95 | 0.072 ** | 0.036 | 0.096 |
| Category | Estimated % Completeness at the Point of System Changing | Estimated Effect Associated with Outbreak Counts | Estimated % Completeness Change in eFORS Time | Estimated % Completeness Change in NORS Time | ||||
|---|---|---|---|---|---|---|---|---|
| Estimate | Std. Error | Estimate | Std. Error | Estimate | Std.Error | Estimate | Std. Error | |
| All Pathogens | ||||||||
| 1 | 97.943 ** | 0.161 | −0.017 * | 0.005 | −0.002 | 0.002 | 0.001 | 0.002 |
| 2 | 87.826 ** | 0.489 | −0.080 ** | 0.016 | 0.160 ** | 0.006 | 0.036 ** | 0.006 |
| 3 | 67.491 ** | 0.531 | −0.228 ** | 0.017 | 0.304 ** | 0.007 | 0.078 ** | 0.007 |
| 4 | 26.317 ** | 0.781 | −0.142 ** | 0.026 | 0.197 ** | 0.01 | 0.328 ** | 0.01 |
| 5 | 5.459 ** | 0.499 | −0.038 | 0.016 | 0.031 ** | 0.006 | 0.396 ** | 0.006 |
| Norovirus | ||||||||
| 1 | 97.913 ** | 0.276 | 0.033 ** | 0.007 | 0.005 | 0.003 | −0.009 ** | 0.003 |
| 2 | 87.420 ** | 1.13 | 0.052 | 0.029 | 0.155 ** | 0.011 | 0.025 * | 0.011 |
| 3 | 67.965 ** | 1.098 | −0.058 * | 0.028 | 0.339 ** | 0.011 | 0.072 ** | 0.011 |
| 4 | 22.537 ** | 1.9 | 0.039 | 0.049 | 0.219 ** | 0.019 | 0.273 ** | 0.019 |
| 5 | 3.493 * | 1.114 | 0.028 | 0.029 | 0.034 * | 0.011 | 0.383 ** | 0.011 |
| Salmonella | ||||||||
| 1 | 97.946 ** | 0.388 | −0.035 | 0.027 | 0.003 | 0.004 | −0.007 | 0.004 |
| 2 | 80.611 ** | 1.229 | −0.014 | 0.084 | 0.138 ** | 0.013 | 0.045 ** | 0.013 |
| 3 | 61.927 ** | 1.263 | −0.139 | 0.086 | 0.254 ** | 0.014 | 0.068 ** | 0.014 |
| 4 | 21.740 ** | 1.609 | −0.188 | 0.11 | 0.150 ** | 0.017 | 0.331 ** | 0.018 |
| 5 | 9.286 ** | 1.253 | −0.071 | 0.086 | 0.021 | 0.014 | 0.432 ** | 0.014 |
| Clostridium | ||||||||
| 1 | 97.777 ** | 0.537 | 0.231 * | 0.111 | 0.002 | 0.006 | 0.001 | 0.006 |
| 2 | 95.423 ** | 1.413 | −0.245 | 0.292 | 0.190 ** | 0.017 | −0.011 | 0.016 |
| 3 | 73.487 ** | 1.536 | 0.057 | 0.317 | 0.347 ** | 0.018 | 0.066 ** | 0.017 |
| 4 | 31.267 ** | 2.325 | −0.584 | 0.48 | 0.212 ** | 0.027 | 0.417 ** | 0.026 |
| 5 | 0.335 | 1.465 | 0.479 | 0.303 | 0.028 | 0.017 | 0.445 ** | 0.016 |
| Unknown Etiology | ||||||||
| 1 | 96.679 ** | 0.45 | −0.092 ** | 0.017 | −0.048 ** | 0.006 | 0.029 ** | 0.005 |
| 2 | 85.505 ** | 0.919 | −0.088 * | 0.034 | 0.160 ** | 0.013 | 0.068 ** | 0.009 |
| 3 | 55.788 ** | 1.119 | 0.076 | 0.042 | 0.368 ** | 0.016 | 0.085 ** | 0.011 |
| 4 | 18.537 ** | 1.82 | 0.12 | 0.068 | 0.225 ** | 0.026 | 0.249 ** | 0.018 |
| 5 | 3.826 ** | 0.914 | 0.044 | 0.034 | 0.060 ** | 0.013 | 0.297 ** | 0.009 |
| Multiple Etiology | ||||||||
| 1 | 97.870 ** | 0.501 | 0.270 * | 0.101 | 0.002 | 0.007 | −0.012 | 0.006 |
| 2 | 88.028 ** | 1.940 | 1.189 * | 0.391 | 0.138 ** | 0.026 | −0.041 | 0.025 |
| 3 | 71.680 ** | 1.775 | −0.580 | 0.358 | 0.335 ** | 0.024 | 0.049 * | 0.023 |
| 4 | 22.670 ** | 2.225 | −0.776 | 0.448 | 0.168 ** | 0.030 | 0.380 ** | 0.028 |
| 5 | 1.809 | 1.459 | 0.222 | 0.294 | 0.022 | 0.020 | 0.496 ** | 0.019 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Simpson, R.B.; Sallade, L.E.; Sanchez, E.; Monahan, K.M.; Naumova, E.N. Evaluating Completeness of Foodborne Outbreak Reporting in the United States, 1998–2019. Int. J. Environ. Res. Public Health 2022, 19, 2898. https://doi.org/10.3390/ijerph19052898
Zhang Y, Simpson RB, Sallade LE, Sanchez E, Monahan KM, Naumova EN. Evaluating Completeness of Foodborne Outbreak Reporting in the United States, 1998–2019. International Journal of Environmental Research and Public Health. 2022; 19(5):2898. https://doi.org/10.3390/ijerph19052898
Chicago/Turabian StyleZhang, Yutong, Ryan B. Simpson, Lauren E. Sallade, Emily Sanchez, Kyle M. Monahan, and Elena N. Naumova. 2022. "Evaluating Completeness of Foodborne Outbreak Reporting in the United States, 1998–2019" International Journal of Environmental Research and Public Health 19, no. 5: 2898. https://doi.org/10.3390/ijerph19052898
APA StyleZhang, Y., Simpson, R. B., Sallade, L. E., Sanchez, E., Monahan, K. M., & Naumova, E. N. (2022). Evaluating Completeness of Foodborne Outbreak Reporting in the United States, 1998–2019. International Journal of Environmental Research and Public Health, 19(5), 2898. https://doi.org/10.3390/ijerph19052898






