Assessing Trade-Offs and Optimal Ranges of Density for Life Expectancy and 12 Causes of Mortality in Metro Vancouver, Canada, 1990–2016
Abstract
:1. Introduction
2. Materials and Methods
2.1. Overview
2.2. Study Design—Growth Management Plans in the 1990s
2.3. Data Sources and Preparation
2.4. Statistical Analysis
3. Results
3.1. Baseline Statistics
3.2. Difference-in-Differences (DID) Analyses
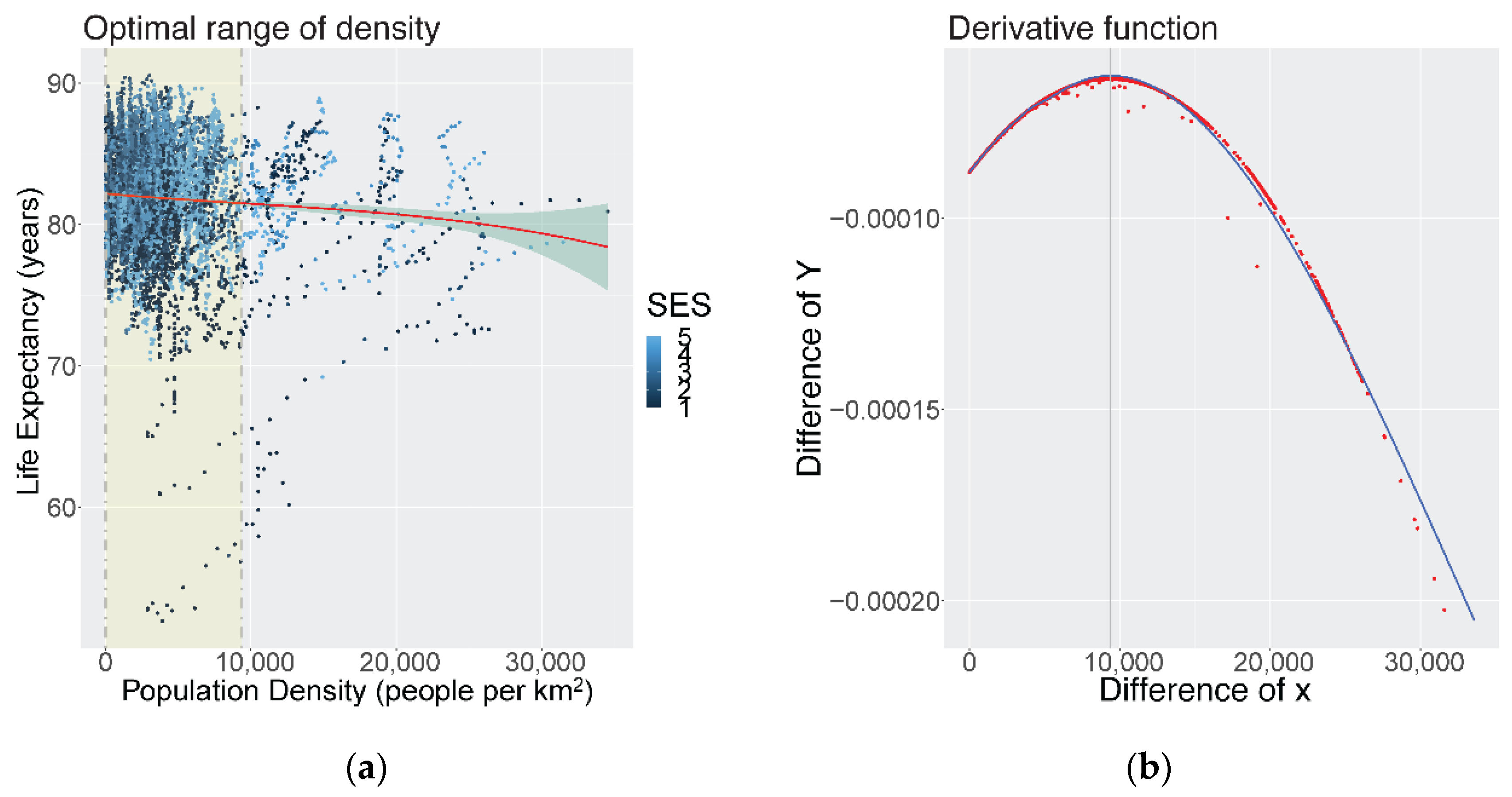
3.3. Shape of the Association for Life Expectancy
3.4. Shape of the Association for Cause-Specific Mortality Rates
4. Discussion
4.1. DID Model Results by SES
4.2. Optimal Ranges of Density for Multiple Mortality Outcomes
4.3. High-Density and Mortality from Respiratory Infections
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- DESA UN. 68% of the World Population Projected to Live in Urban Areas by 2050, Says UN; United Nations Department of Economic and Social Affairs: New York, NY, USA, 2018. [Google Scholar]
- Tomalty, R. Growth Management in the Vancouver Region. Local Environ. 2002, 7, 431–445. [Google Scholar] [CrossRef]
- The Ontario Professional Planners Institute. Exploring Growth Management Roles in Ontario: Learning from “Who Does What” Elsewhere; The Ontario Professional Planners Institute: Toronto, ON, Canada, 2001. [Google Scholar]
- Sarkar, C.; Webster, C. Healthy Cities of Tomorrow: The Case for Large Scale Built Environment–Health Studies. J. Hered. 2017, 94, 4–19. [Google Scholar] [CrossRef] [Green Version]
- Giles-Corti, B.; Vernez-Moudon, A.; Reis, R.; Turrell, G.; Dannenberg, A.L.; Badland, H.; Foster, S.; Lowe, M.; Sallis, J.F.; Stevenson, M.; et al. City planning and population health: A global challenge. Lancet 2016, 388, 2912–2924. [Google Scholar] [CrossRef]
- Forsyth, A. Congested cities vs. sprawl makes you fat: Unpacking the health effects of planning density. Town Plan. Rev. 2018, 89, 333–354. [Google Scholar]
- Boyko, C.T.; Cooper, R. Clarifying and re-conceptualising density. Prog. Plan. 2011, 76, 1–61. [Google Scholar] [CrossRef]
- Hummel, D. The effects of population and housing density in urban areas on income in the United States. Local Econ. J. Local Econ. Policy Unit 2020, 35, 27–47. [Google Scholar] [CrossRef]
- Landcom. Residential Density Guide; For Landcom Project Teams; Landcom: Parramatta, Australia, 2011. [Google Scholar]
- Roskamm, N. Taking Sides with a Man-Eating Shark: Jane Jacobs and the 1960s “Density Turn”. In Urban Planning. Contemporary Perspectives on Jane Jacobs: Reassessing the Impacts of an Urban Visionary Burlington, VT; Ashgate: Burlington, VT, USA, 2014; pp. 83–92. [Google Scholar]
- Rundle, A.; Roux, A.V.D.; Freeman, L.M.; Miller, D.; Neckerman, K.M.; Weiss, C.C. The Urban Built Environment and Obesity in New York City: A Multilevel Analysis. Am. J. Health Promot. 2007, 21, 326–334. [Google Scholar] [CrossRef]
- Badland, H.; Foster, S.; Bentley, R.; Higgs, C.; Roberts, R.; Pettit, C.; Giles-Corti, B. Examining associations between area-level spatial measures of housing with selected health and wellbeing behaviours and outcomes in an urban context. Health Place 2017, 43, 17–24. [Google Scholar] [CrossRef]
- Leal, C.; Chaix, B. The influence of geographic life environments on cardiometabolic risk factors: A systematic review, a methodological assessment and a research agenda. Obes. Rev. 2011, 12, 217–230. [Google Scholar] [CrossRef]
- Ewing, R.; Schieber, R.A.; Zegeer, C.V. Urban Sprawl as a Risk Factor in Motor Vehicle Occupant and Pedestrian Fatalities. Am. J. Public Health 2003, 93, 1541–1545. [Google Scholar] [CrossRef]
- Papas, M.A.; Alberg, A.J.; Ewing, R.; Helzlsouer, K.J.; Gary-Webb, T.L.; Klassen, A.C. The Built Environment and Obesity. Epidemiol. Rev. 2007, 29, 129–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sturm, R.; Cohen, D.A.; Street, M.; Monica, S. Suburban sprawl and physical and mental health. Public Health 2004, 118, 488–496. [Google Scholar] [CrossRef] [PubMed]
- Ross, N.A.; Tremblay, S.; Khan, S.; Crouse, D.; Tremblay, M.; Berthelot, J.-M. Body Mass Index in Urban Canada: Neighborhood and Metropolitan Area Effects. Am. J. Public Health 2007, 97, 500–508. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cerin, E.; Conway, T.L.; Adams, M.A.; Frank, L.D.; Pratt, M.; Salvo, D.; Schipperijn, J.; Smith, G.; Cain, K.L.; et al. Physical activity in relation to urban environments in 14 cities worldwide: A cross-sectional study. Lancet 2016, 387, 2207–2217. [Google Scholar] [CrossRef] [Green Version]
- Frank, L.D.; Andresen, M.; Schmid, T.L. Obesity relationships with community design, physical activity, and time spent in cars. Am. J. Prev. Med. 2004, 27, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Pouliou, T.; Elliott, S.J. Health & Place Individual and socio-environmental determinants of overweight and obesity in Urban Canada. Health Place 2010, 16, 389–398. [Google Scholar] [PubMed]
- Beenackers, M.A.; Groeniger, J.O.; Kamphuis, C.B.M.; Van Lenthe, F.J. Urban population density and mortality in a compact Dutch city: 23-year follow-up of the Dutch GLOBE study. Health Place 2018, 53, 79–85. [Google Scholar] [CrossRef]
- McCormack, G.R.; Shiell, A. In search of causality: A systematic review of the relationship between the built environment and physical activity among adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 125. [Google Scholar] [CrossRef] [Green Version]
- Hanlon, M.; Burstein, R.; Masters, S.H.; Zhang, R. Exploring the relationship between population density and maternal health coverage. BMC Health Serv. Res. 2012, 12, 416. [Google Scholar] [CrossRef] [Green Version]
- Xu, F.; Li, J.; Liang, Y.; Wang, Z.; Hong, X.; Ware, R.; Leslie, E.; Sugiyama, T.; Owen, N. Residential density and adolescent overweight in a rapidly urbanising region of mainland China. J. Epidemiol. Community Health 2009, 64, 1017–1021. [Google Scholar] [CrossRef]
- Lin, B.; Meyers, J.; Barnett, G. Understanding the potential loss and inequities of green space distribution with urban densification. Urban For. Urban Green. 2015, 14, 952–958. [Google Scholar] [CrossRef]
- Cramer, V.; Torgersen, S.; Kringlen, E. Quality of Life in a City: The Effect of Population Density. Soc. Indic. Res. 2004, 69, 103–116. [Google Scholar] [CrossRef]
- Colodro-Conde, L.; Couvy-Duchesne, B.; Whitfield, J.B.; Streit, F.; Gordon, S.; Kemper, K.E.; Yengo, L.; Zheng, Z.; Trzaskowski, M.; de Zeeuw, E.L.; et al. Association between population density and genetic risk for schizophrenia. JAMA Psychiatry 2018, 75, 901–910. [Google Scholar] [CrossRef] [Green Version]
- Vancouver, M. Metro Vancouver 2040: Shaping Our Future. Retrieved Novemb. 2011, 2, 2014. [Google Scholar]
- Statistics Canada. Focus on Geography Series, 2016 Census; Catalogue No. 98-404-X2016001; Statistics Canada: Ottawa, ON, Canada, 2017. [Google Scholar]
- Yu, J.; Dwyer-Lindgren, L.; Bennett, J.; Ezzati, M.; Gustafson, P.; Tran, M.; Brauer, M. A spatiotemporal analysis of inequalities in life expectancy and 20 causes of mortality in sub-neighbourhoods of Metro Vancouver, British Columbia, Canada, 1990—2016. Health Place 2021, 72, 102692. [Google Scholar] [CrossRef] [PubMed]
- Dwyer-lindgren, L.; Stubbs, R.W.; Bertozzi-villa, A.; Morozoff, C.; Callender, C.; Finegold, S.B.; Shirude, S.; Flaxman, A.D.; Laurent, A.; Kern, E.; et al. Vari-ation in life expectancy and mortality by cause among neighbourhoods in King County, WA, USA, 1990–2014: A census tract-level analysis for the Global Burden of Disease Study 2015. Lancet Public Health 2017, 2, e400-10. [Google Scholar] [CrossRef] [Green Version]
- Pampalon, R.; Hamel, D.; Gamache, P.; Philibert, M.D.; Raymond, G.; Simpson, A. An Area-Based Material and Social Deprivation Index for Public Health in Québec and Canada. Can. J. Public Health 2012, 103, S17–S22. [Google Scholar] [CrossRef]
- Allen, J.; Taylor, Z. A new tool for neighbourhood change research: The Canadian Longitudinal Census Tract Database, 1971–2016. Can. Geogr./Géographe Can. 2018, 62, 575–588. [Google Scholar] [CrossRef]
- Coogan, P.F.; White, L.F.; Adler, T.J.; Hathaway, K.M.; Palmer, J.R.; Rosenberg, L. Prospective Study of Urban Form and Physical Activity in the Black Women’s Health Study. Am. J. Epidemiol. 2009, 170, 1105–1117. [Google Scholar] [CrossRef] [Green Version]
- Udell, T.; Daley, M.; Johnson, B.; Tolley, R. Does Density Matter? The Role of Density in Creating Walkable Neighbourhoods; National Heart Foundation of Australia: Melbourne, Australia, 2014; Volume 1, pp. 1–35.
- Larson, N.I.; Story, M.T.; Nelson, M.C. Neighborhood Environments: Disparities in Access to Healthy Foods in the U.S. Am. J. Prev. Med. 2009, 36, 74–81.e10. [Google Scholar] [CrossRef]
- Seliske, L.M.; Pickett, W.; Boyce, W.F.; Janssen, I. Density and type of food retailers surrounding Canadian schools: Variations across socioeconomic status. Health Place 2009, 15, 903–907. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, J.R.; Horel, S.; Han, D.; Huber, J.C. Association between neighborhood need and spatial access to food stores and fast food restaurants in neighborhoods of colonias. Int. J. Health Geogr. 2009, 8, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, R.; Feng, Z.; Xue, D.; Liu, Y.; Wu, R. Exploring the links between population density, lifestyle, and being overweight: Secondary data analyses of middle-aged and older Chinese adults. Health Qual. Life Outcomes 2019, 17, 100. [Google Scholar] [CrossRef] [PubMed]
- Cusimano, M.; Marshall, S.; Rinner, C.; Jiang, D.; Chipman, M. Patterns of urban violent injury: A spatio-temporal analysis. PLoS ONE 2010, 5, e8669. [Google Scholar] [CrossRef] [Green Version]
- Wanyeki, I.; Olson, S.; Brassard, P.; Menzies, D.; Ross, N.; Behr, M.; Schwartzman, K. Dwellings, crowding, and tuberculosis in Montreal. Soc. Sci. Med. 2006, 63, 501–511. [Google Scholar] [CrossRef]
- Correia, A.W.; Pope, C.A., III; Dockery, D.W.; Wang, Y.; Ezzati, M.; Dominici, F. The effect of air pollution control on life expectancy in the United States: An analysis of 545 US counties for the period 2000 to 2007. Epidemiology 2013, 24, 23. [Google Scholar] [CrossRef] [Green Version]
- Greenhalgh, J. Consuming communities: The neighbourhood unit and the role of retail spaces on British housing estates, 1944–1958. Urban Hist. 2015, 43, 158–174. [Google Scholar] [CrossRef] [Green Version]
- Sarkar, C.; Webster, C.; Gallacher, J. Articles Association between adiposity outcomes and residential density: A full-data, cross-sectional analysis of 419 562 UK Biobank adult participants. Lancet Planet. Health 2017, 1, e277–e288. [Google Scholar] [CrossRef] [Green Version]
- Yin, C.; Sun, B. Does Compact Built Environment Help to Reduce Obesity? Influence of Population Density on Waist–Hip Ratio in Chinese Cities. Int. J. Environ. Res. Public Health 2020, 17, 7746. [Google Scholar] [CrossRef]
- Hamidi, S.; Ewing, R.; Tatalovich, Z.; Grace, J.B.; Berrigan, D. Associations between Urban Sprawl and Life Expectancy in the United States. Int. J. Environ. Res. Public Health 2018, 15, 861. [Google Scholar] [CrossRef] [Green Version]
- Meijer, M.; Kejs, A.M.; Stock, C.; Bloomfield, K.; Ejstrud, B.; Schlattmann, P. Population density, socio-economic environment and all-cause mortality: A multilevel survival analysis of 2.7 million indi-viduals in Denmark. Health Place 2012, 18, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Nakaya, T.; Honjo, K.; Hanibuchi, T.; Ikeda, A.; Iso, H.; Inoue, M.; Sawada, N.; Tsugane, S.; The Japan Public Health Center-Based Prospective Study Group. Associations of All-Cause Mortality with Census-Based Neighbourhood Deprivation and Population Density in Japan: A Multilevel Survival Analysis. PLoS ONE 2014, 9, e97802. [Google Scholar] [CrossRef] [PubMed]
- Chaix, B.; Rosvall, M.; Lynch, J.; Merlo, J. Disentangling contextual effects on cause-specific mortality in a longitudinal 23-year follow-up study: Impact of population density or socioeconomic environment? Int. J. Epidemiol. 2006, 35, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Lisonkova, S.; Liu, S.; Bartholomew, S.; Liston, R.M.; Joseph, K.S.; Maternal Health Study Group of the Canadian Perinatal Surveillance System. Temporal trends in maternal mortality in Canada II: Estimates based on hospitalization data. J. Obstet. Gynaecol. Can. 2011, 33, 1020–1030. [Google Scholar] [CrossRef]
- Nandram, B.; Sedransk, J.; Pickle, L.W. Bayesian Analysis and Mapping of Mortality Rates for Chronic Obstructive Pulmonary Disease. J. Am. Stat. Assoc. 2000, 95, 1110. [Google Scholar] [CrossRef]
- Webster, C. How high can we go? Urban density, infectious versus chronic disease, and the adaptive resilience of cities. Town Plan. Rev. 2021, 92, 123–130. [Google Scholar] [CrossRef]
- Hamidi, S.; Sabouri, S.; Ewing, R. Does Density Aggravate the COVID-19 Pandemic?: Early Findings and Lessons for Planners. J. Am. Plan. Assoc. 2020, 86, 495–509. [Google Scholar] [CrossRef]
- Carozzi, F. Urban Density and COVID-19; Centre for Economic Performance: London, UK, 2020. [Google Scholar]
- Hamidi, S.; Ewing, R.; Sabouri, S. Longitudinal analyses of the relationship between development density and the COVID-19 morbidity and mortality rates: Early evidence from 1165 metropolitan counties in the United States. Health Place 2020, 64, 102378. [Google Scholar] [CrossRef]
- Bhadra, A.; Mukherjee, A.; Sarkar, K. Impact of population density on COVID-19 infected and mortality rate in India. Model. Earth Syst. Environ. 2020, 7, 623–629. [Google Scholar] [CrossRef]
- Baser, O. Population density index and its use for distribution of COVID-19: A case study using Turkish data. Health Policy 2020, 125, 148–154. [Google Scholar] [CrossRef]
- Kadi, N.; Khelfaoui, M. Population density, a factor in the spread of COVID-19 in Algeria: Statistic study. Bull. Natl. Res. Cent. 2020, 44, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shannon, H.; Allen, C.; Dávila, D.; Fletcher-Wood, L.; Gupta, S.; Keck, K.; Lang, S.; Ludolph, R.; Kahangire, D. WHO Housing and Health Guidelines: Web Annex A: Report of the Systematic Review on the Effect of Household Crowding on Health; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Jenks, M.; Dempsey, N. Defining the neighbourhood: Challenges for empirical research. Town Plan. Rev. 2007, 78, 153–177. [Google Scholar] [CrossRef]
- Renalds, A.; Smith, T.H.; Hale, P.J. A Systematic Review of Built Environment and Health. Fam. Community Health 2010, 33, 68–78. [Google Scholar] [CrossRef]
- Ashenfelter, O. Estimating the Effect of Training Programs on Earnings. Rev. Econ. Stat. 1978, 60, 47. [Google Scholar] [CrossRef]
- Zhou, H.; Taber, C.; Arcona, S.; Li, Y. Difference-in-Differences Method in Comparative Effectiveness Research: Utility with Unbalanced Groups. Appl. Health Econ. Health Policy 2016, 14, 419–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wing, C.; Simon, K.; Bello-Gomez, R.A. Designing Difference in Difference Studies: Best Practices for Public Health Policy Research. Annu. Rev. Public Health 2018, 39, 453–469. [Google Scholar] [CrossRef] [Green Version]
- Hooper, M.W.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and Racial/Ethnic Disparities. JAMA J. Am. Med. Assoc. 2020, 323, 2466. [Google Scholar] [CrossRef]
- Hsu, A.T.; Lane, N.; Sinha, S.K.; Dunning, J.; Dhuper, M.; Kahiel, Z.; Sveistrup, H. Impact of COVID-19 on residents of Canada’s long-term care homes--ongoing challenges and policy response. Int. Long-Term Care Policy Netw. 2020, 17, 1–18. [Google Scholar]
- Fuss, J.; Globerman, S. Canada’s Aging Population and Long-Term Projections for Federal Finances; Fraser Institute: Vancouver, BC, Canada, 2020. [Google Scholar]




| No. of CTs | Median Area (km2) | Median Population Density (People per km2) | Median Life Expectancy (Years) | Median Material Deprivation Index Score | Median Social Deprivation Index Score | |
|---|---|---|---|---|---|---|
| Entire study region | 368 | 1.8 | 2463 | 79.8 | 1.03 | 1.02 |
| Model 1: All CTsb | 74 | 2.6 | 713 | 79.7 | 1.05 | 1.03 |
| P90 CTs | 37 | 3.1 | 387 | 79.6 | 1.05 | 1.05 |
| P10 CTs | 37 | 2.2 | 1915 | 79.8 | 1.05 | 1.02 |
| Model 2: Low SES (high MSDI) CT subsetb | 39 | 1.3 | 715 | 78.6 | 625.90 | 625.95 |
| P90 CTs | 19 | 1.4 | 515 | 79.0 | 763.67 | 763.66 |
| P10 CTs | 20 | 1.3 | 2974 | 78.4 | 331.27 | 331.19 |
| Model 3: High SES (low MSDI) CT subsetb | 33 | 2.2 | 2793 | 77.2 | 0.99 | 0.98 |
| P90 CTs | 17 | 3.2 | 1482 | 75.7 | 1.00 | 0.95 |
| P10 CTs | 16 | 1.6 | 5802 | 78.3 | 0.99 | 0.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, J.; Gustafson, P.; Tran, M.; Brauer, M. Assessing Trade-Offs and Optimal Ranges of Density for Life Expectancy and 12 Causes of Mortality in Metro Vancouver, Canada, 1990–2016. Int. J. Environ. Res. Public Health 2022, 19, 2900. https://doi.org/10.3390/ijerph19052900
Yu J, Gustafson P, Tran M, Brauer M. Assessing Trade-Offs and Optimal Ranges of Density for Life Expectancy and 12 Causes of Mortality in Metro Vancouver, Canada, 1990–2016. International Journal of Environmental Research and Public Health. 2022; 19(5):2900. https://doi.org/10.3390/ijerph19052900
Chicago/Turabian StyleYu, Jessica, Paul Gustafson, Martino Tran, and Michael Brauer. 2022. "Assessing Trade-Offs and Optimal Ranges of Density for Life Expectancy and 12 Causes of Mortality in Metro Vancouver, Canada, 1990–2016" International Journal of Environmental Research and Public Health 19, no. 5: 2900. https://doi.org/10.3390/ijerph19052900
APA StyleYu, J., Gustafson, P., Tran, M., & Brauer, M. (2022). Assessing Trade-Offs and Optimal Ranges of Density for Life Expectancy and 12 Causes of Mortality in Metro Vancouver, Canada, 1990–2016. International Journal of Environmental Research and Public Health, 19(5), 2900. https://doi.org/10.3390/ijerph19052900






