Health-Related Quality of Life (HRQoL) of Residents with Persistent Lower Respiratory Symptoms or Asthma Following a Sulphur Stockpile Fire Incident
Abstract
:1. Introduction
2. Materials and Methods
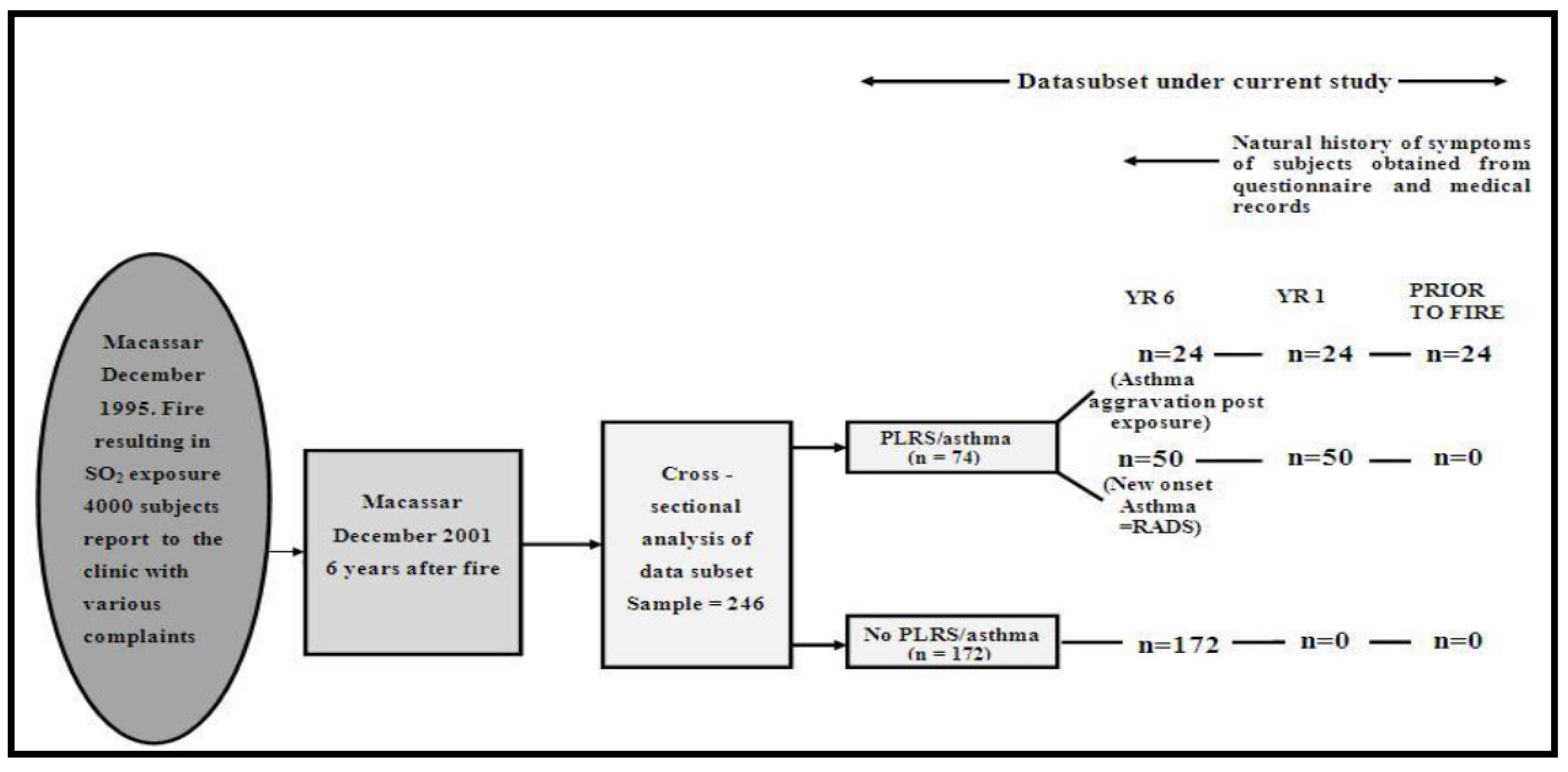
2.1. Recruitment and Study Sample
2.2. Questionnaires
2.3. Definition of PLRS or Asthma
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baatjies, R.; Adams, S.; Cairncross, E.; Omar, F.; Jeebhay, M.F. Factors associated with persistent lower respiratory symptoms or asthma among residents exposed to a sulphur stockpile fire incident. Int. J. Environ. Res. Public Health 2019, 16, 438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, R.; Huang, W.; Wong, C.M.; Wang, Z.; Thach, T.Q.; Chen, B.; Kan, H.; CAPES Collaborative Group. Short-term exposure to sulfur dioxide and daily mortality in 17 Chinese cities: The China air pollution and health effects study (CAPES). Environ. Res. 2012, 118, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.M.; Kuschner, W.G.; Gokhale, J.; Shofer, S. Outdoor air pollution: Nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am. J. Med. Sci. 2007, 333, 249–256. [Google Scholar] [CrossRef]
- Piirilä, P.L.; Nordman, H.; Korhonen, O.S.; Winblad, I. A thirteen-year follow-up of respiratory effects of acute exposure to sulfur dioxide. Scand. J. Work. Environ. Health 1996, 22, 191–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, E.; Knutsson, A.; Hagberg, S.; Nilsson, T.; Karlsson, B.; Alfredsson, L.; Torén, K. Incidence of asthma among workers exposed to sulphur dioxide and other irritant gases. Eur. Respir. J. 2006, 27, 720–725. [Google Scholar] [CrossRef] [PubMed]
- Zock, J.P.; Rodríguez-Trigo, G.; Rodríguez-Rodríguez, E.; Espinosa, A.; Pozo-Rodríguez, F.; Gómez, F.; Fuster, C.; Castaño-Vinyals, G.; Antó, J.M.; Barberà, J.A. Persistent respiratory symptoms in clean-up workers 5 years after the Prestige oil spill. Occup. Environ. Med. 2012, 69, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Antao, V.C.; Pallos, L.L.; Graham, S.L.; Shim, Y.K.; Sapp, J.H.; Lewis, B.; Bullard, S.; Alper, H.E.; Cone, J.E.; Farfel, M.R.; et al. 9/11 Residential Exposures: The impact of world trade center dust on respiratory outcomes of lower Manhattan residents. Int. J. Environ. Res. Public Health 2019, 16, 798. [Google Scholar] [CrossRef] [Green Version]
- Friedman, S.M.; Farfel, M.R.; Maslow, C.B.; Cone, J.E.; Brackbill, R.M.; Stellman, S.D. Comorbid persistent lower respiratory symptoms and posttraumatic stress disorder 5–6 years post-9/11 in responders enrolled in the World Trade Center Health Registry. Am. J. Ind. Med. 2013, 56, 1251–1261. [Google Scholar] [CrossRef] [Green Version]
- Friedman, S.M.; Farfel, M.R.; Maslow, C.; Jordan, H.T.; Li, J.; Alper, H.; Cone, J.E.; Stellman, S.D.; Brackbill, R.M. Risk factors for and consequences of persistent lower respiratory symptoms among World Trade Center Health Registrants 10 years after the disaster. Occup. Environ. Med. 2016, 73, 676–684. [Google Scholar] [CrossRef] [Green Version]
- Jordan, H.T.; Friedman, S.M.; Reibman, J.; Goldring, R.M.; Archie, S.A.M.; Ortega, F.; Alper, H.; Shao, Y.; Maslow, C.B.; Cone, J.E.; et al. Risk factors for persistence of lower respiratory symptoms among community members exposed to the 2001 World Trade Center terrorist attacks. Occup. Environ. Med. 2017, 74, 449–455. [Google Scholar] [CrossRef]
- Yip, J.; Zeig-Owens, R.; Hall, C.B.; Webber, M.P.; Olivieri, B.; Schwartz, T.; Kelly, K.J.; Prezant, D.J. Health conditions as mediators of the association between World Trade Center exposure and health-related quality of life in firefighters and EMS workers. J. Occup. Environ. Med. 2016, 58, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Şakar, A.; Yorgancıoğlu, A.; Aydemir, Ö.; Sepit, L.; Çelik, P. Effect of severity of asthma on quality of life. Tuberk Toraks 2007, 55, 135–140. [Google Scholar] [PubMed]
- Bousquet, J.; Knani, J.; Dhivert, H.; Richard, A.L.A.I.N.; Chicoye, A.N.N.I.E.; Ware, J.E., Jr.; Michel, F.B. Quality of life in asthma. I. Internal consistency and validity of the SF-36 questionnaire. Am. J. Respir. Crit. Care Med. 1994, 149, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Ried, L.D.; Nau, D.P.; Grainger-Rousseau, T.J. Evaluation of patient’s Health-Related Quality of Life using a modified and shortened version of the Living with Asthma Questionnaire (ms-LWAQ) and the medical outcomes study, Short-Form 36 (SF-36). Qual. Life Res. 1999, 8, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Muraki, M.; Ichihashi, H.; Haraguchi, R.; Iwanaga, T.; Kubo, H.; Tohda, Y. Comparison of the Asthma Health Questionnaire-33-Japan and the short-form 36-item health survey for measuring quality of life in Japanese patients with asthma. Allergol. Int. 2008, 57, 339–346. [Google Scholar] [CrossRef] [Green Version]
- Brackbill, R.M.; Hadler, J.L.; Di Grande, L.; Ekenga, C.C.; Farfel, M.R.; Friedman, S.; Perlman, S.E.; Stellman, S.D.; Walker, D.J.; Wu, D.; et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. Jama 2009, 302, 502–516. [Google Scholar] [CrossRef] [Green Version]
- Corporation, R. 36-Item Short Form Survey (SF-36) Scoring Instructions. 2021. Available online: https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/scoring.html (accessed on 19 August 2021).
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Jeebhay, M.F.; Ngajilo, D.; le Moual, N. Risk factors for nonwork-related adult-onset asthma and occupational asthma: A comparative review. Curr. Opin. Allergy Clin. Immunol. 2014, 14, 84–94. [Google Scholar] [CrossRef]
- Soong, W.; Chipps, B.E.; O’Quinn, S.; Trevor, J.; Carr, W.W.; Belton, L.; Trudo, F.; Ambrose, C.S. Health-Related Quality of Life and Productivity Among US Patients with Severe Asthma. J. Asthma Allergy 2021, 14, 713. [Google Scholar] [CrossRef]
- Song, H.J.; Blake, K.V.; Wilson, D.L.; Winterstein, A.G.; Park, H. Health-related quality of life and health utilities of mild, moderate, and severe asthma: Evidence from the medical expenditure panel survey. J. Asthma Allergy 2021, 14, 929. [Google Scholar] [CrossRef]
- Stucky, B.D.; Sherbourne, C.D.; Edelen, M.O.; Eberhart, N.K. Understanding asthma-specific quality of life: Moving beyond asthma symptoms and severity. Eur. Respir. J. 2015, 46, 680–687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osman, L.M.; Calder, C.; Robertson, R.; Friend, J.A.; Legge, J.S.; Graham Douglas, J. Symptoms, quality of life, and health service contact among young adults with mild asthma. Am. J. Respir. Crit. Care Med. 2000, 161, 498–503. [Google Scholar] [CrossRef] [PubMed]
- de Albornoz, S.C.; Chen, G. Relationship between health-related quality of life and subjective wellbeing in asthma. J. Psychosom. Res. 2021, 142, 110356. [Google Scholar] [CrossRef] [PubMed]
- Leynaert, B.; Neukirch, C.; Liard, R.; Bousquet, J.; Neukirch, F. Quality of life in allergic rhinitis and asthma: A population-based study of young adults. Am. J. Respir. Crit. Care Med. 2000, 162, 1391–1396. [Google Scholar] [CrossRef] [PubMed]
- Kalpaklĩoğlu, A.F.; Baççıoğlu, A. Evaluation of quality of life: Impact of allergic rhinitis on asthma. J. Investig. Allergol. Clin. Immunol. 2008, 18, 168–173. [Google Scholar]
- Wijnhoven, H.A.; Kriegsman, D.M.; Snoek, F.J.; Hesselink, A.E.; De Haan, M. Gender differences in health-related quality of life among asthma patients. J. Asthma 2003, 40, 189–199. [Google Scholar] [CrossRef]
- Belloch, A.; Perpiñá, M.; Martínez-Moragón, E.; de Diego, A.; Martínez-Francés, M. Gender differences in health-related quality of life among patients with asthma. J. Asthma 2003, 40, 945–953. [Google Scholar] [CrossRef]
- Colombo, D.; Zagni, E.; Ferri, F.; Canonica, G.W. Gender differences in asthma perception and its impact on quality of life: A post hoc analysis of the PROXIMA (Patient Reported Outcomes and Xolair® In the Management of Asthma) study. Allergy Asthma Clin. Immunol. 2019, 15, 1–10. [Google Scholar] [CrossRef]
- Chhabra, S.K.; Chhabra, P. Gender differences in perception of dyspnea, assessment of control, and quality of life in asthma. J. Asthma 2011, 48, 609–615. [Google Scholar] [CrossRef]
- Larsson, U.; Taft, C.; Karlsson, J.; Sullivan, M. Gender and age differences in the relative burden of rhinitis and asthma on health-related quality of life—A Swedish population study. Respir. Med. 2007, 101, 1291–1298. [Google Scholar] [CrossRef] [Green Version]
- Tovt-Korshynska, M.I.; Dew, M.A.; Chopey, I.V.; Spivak, M.Y.; Lemko, I.S. Gender differences in psychological distress in adults with asthma. J. Psychosom. Res. 2001, 51, 629–637. [Google Scholar] [CrossRef]
| Demographic Characteristics | Total N (%) | PLRS or (n = 246) Symptoms after the Fire (n = 74) N (%) | No PLRS or Symptoms after the Fire (n = 172) N (%) | p-Value |
|---|---|---|---|---|
| * Age (years) Mean ± SD | 42 ± 12.8 | 42 ± 11.8 | 41 ± 13.2 | 0.494 |
| Gender | ||||
| Female | 162 (65.8) | 52 (70.3) | 110 (63.9) | |
| Male | 84 (34.2) | 22 (29.7) | 62 (36.1) | 0.338 |
| Smoking status | ||||
| Never | 101 (41.1) | 30 (40.5) | 71 (41.2) | |
| Previous | 81 (32.9) | 29 (39.1) | 52 (30.2) | |
| Current | 64 (26.0) | 15 (20.2) | 49 (28.4) | 0.271 |
| Previous Pulmonary Tuberculosis | 29 (11.8) | 13 (17.5) | 16 (19.3) | 0.065 |
| Current treatment for asthma | 45 (18.3) | 45 (60.8) | 0 (0) | <0.001 |
| Other chronic diseases | ||||
| Hypertension | 61 (24.8) | 17 (22.9) | 44 (25.5) | 0.664 |
| Cardiac disease | 19 (7.72) | 8 (10.8) | 11 (6.3) | 0.234 |
| Diabetes | 22 (8.94) | 10 (13.5) | 12 (6.9) | 0.099 |
| Arthritis | 25 (10.2) | 3 (4.0) | 22 (12.7) | 0.038 |
| Depression | 23 (9.3) | 8 (10.8) | 15 (8.7) | 0.606 |
| Anxiety | 29 (11.8) | 10 (13.5) | 19 (11.0) | 0.582 |
| Physical Functioning Score | Role—Physical Score | Bodily Pain Score | General Health Score | |||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | |
| PLRS/Asthma | 24 ± 25.1 | 15 (0–35) | 33 ± 45.9 | 0 (0–100) | 67 ± 30.8 | 78 (33–100) | 24 ± 17.8 | 19 (13–32) |
| No PLRS/Asthma | 39 ± 28.5 | 35 (18–35) | 48 ± 48.7 | 0 (0–100) | 67 ± 31.0 | 78 (33–100) | 37 ± 25.9 | 32 (13–56) |
| p-value * | <0.001 | 0.024 | 0.797 | <0.001 | ||||
| Vitality Score | Social Functioning Score | Role—Emotional Score | Mental Health Score | |||||
| Mean (SD) | Median (IQR) | Mean (SD) | Media (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | |
| PLRS/Asthma | 50 ± 20.1 | 50 (35–65) | 57 ± 28.8 | 55 (33–80) | 46 ± 49.2 | 0 (0–100) | 62 ± 26.9 | 60 (36–88) |
| No PLRS/Asthma | 52 ± 20.6 | 50 (40–65) | 62 ± 28.2 | 68 (43–80) | 51 ± 49.1 | 63 (0–100) | 63 ± 24.9 | 60 (44–84) |
| p-value * | 0.685 | 0.239 | 0.535 | 0.883 | ||||
| β-Coefficient (95% Confidence Interval) | ||||
|---|---|---|---|---|
| PF | RP | BP | GH | |
| Constant | 89.18 (77.12, 101.25) *** | 85.35 (62.58, 108.11) *** | 91.08 (76, 105.57) *** | 44.59 (39.27, 49.90) *** |
| Age (years) | −0.78 (−1.02, −0.55) *** | −0.70 (−1.169, −0.27) ** | −0.45 (−0.74, −0.16) ** | - |
| Female | −19.09 (−25.30, −12.89) *** | - | - | −9.98 (−16.16, −3.80) ** |
| Smoking | ||||
| - Previous | - | - | - | - |
| - Current | - | - | - | - |
| Previous Pulmonary TB | - | - | - | - |
| PLRS/asthma | −13.13 (−19.56, −6.71) *** | −13.09 (−25.86, −0.34) * | - | −12.94 (19.19, −6.49) *** |
| RUDS | - | - | - | - |
| Depression | - | −26.32 (−46.39, −6.26) ** | - | −10.10 (−21.01, −0.89) * |
| Anxiety | - | - | −21.50 (−33.06, −9.93) *** | - |
| Cardiac disease | −10.72 (−22.11,0.66) δ | - | - | - |
| Model R2 | 0.33 | 0.08 | 0.08 | 0.06 |
| β-Coefficient (95% Confidence Interval) | ||||
|---|---|---|---|---|
| V | SF | RE | MH | |
| Constant | 64.40 (54.78, 74.01) *** | 62.63 (59.00, 66.26) *** | 98.89 (74.58, 123.20) * | 77.42 (71.08, 83.77) *** |
| Age (years) | −0.23 (−0.42, −0.03) * | - | −0.75 (−1.22, −0.28) ** | - |
| Female | - | - | −14.39 (−27.09, −1.70) * | −9.57 (−15.77, −3.37) ** |
| Smoking | - | - | - | −4.84 (−8.49, −1.19) ** |
| - Previous | - | - | - | −6.82 (−13.61, −0.04) * |
| - Current | - | - | - | −9.80 (−17.05, −2.54) ** |
| Previous Pulmonary TB | - | - | - | - |
| PLRS/asthma | - | - | - | - |
| RUDS | - | - | - | - |
| Depression | −13.98 (−22.81, −5.15) ** | −25.24 (−37.11, −13.37) *** | −21.85 (−42.45, −1.25) * | −19.64 (−29.82, 9.26) *** |
| Anxiety | −7.38 (−15.35, 0.58) δ | - | - | −17.32 (−26.76, −7.88) *** |
| Cardiac disease | - | - | - | - |
| Model R2 | 0.08 | 0.06 | 0.09 | 0.2 |
| Decline in SF-36 Scores after 1 Year Odds Ratio (95% CI) | Decline in SF-36 Scores after 6 Years Odds Ratio (95% CI) | |||||
|---|---|---|---|---|---|---|
| Role—Physical | Bodily Pain | General Health | Role—Physical | Bodily Pain | General Health | |
| PLRS/asthma | 1.97 (1.09, 3.55) * | 1.24 (0.70, 2.21) | 7.07 (2.88, 17.35) *** | 1.59 (0.89, 2.84) | 1.05 (0.59, 1.84) | 3.50 (1.39. 8.79) ** |
| PLRS/asthma and RUDS | 1.82 (0.84, 4.15) | 0.95 (0.42, 2.13) | 7.04 (1.61, 30.7) ** | 1.65 (0.74, 3.79) | 0.84 (0.38, 1.84) | 8.58 (1.10, 65.02) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adams, S.; Rajani, M.; Baatjies, R.; Omar, F.; Jeebhay, M.F. Health-Related Quality of Life (HRQoL) of Residents with Persistent Lower Respiratory Symptoms or Asthma Following a Sulphur Stockpile Fire Incident. Int. J. Environ. Res. Public Health 2022, 19, 2915. https://doi.org/10.3390/ijerph19052915
Adams S, Rajani M, Baatjies R, Omar F, Jeebhay MF. Health-Related Quality of Life (HRQoL) of Residents with Persistent Lower Respiratory Symptoms or Asthma Following a Sulphur Stockpile Fire Incident. International Journal of Environmental Research and Public Health. 2022; 19(5):2915. https://doi.org/10.3390/ijerph19052915
Chicago/Turabian StyleAdams, Shahieda, Mayuri Rajani, Roslynn Baatjies, Faieza Omar, and Mohamed Fareed Jeebhay. 2022. "Health-Related Quality of Life (HRQoL) of Residents with Persistent Lower Respiratory Symptoms or Asthma Following a Sulphur Stockpile Fire Incident" International Journal of Environmental Research and Public Health 19, no. 5: 2915. https://doi.org/10.3390/ijerph19052915
APA StyleAdams, S., Rajani, M., Baatjies, R., Omar, F., & Jeebhay, M. F. (2022). Health-Related Quality of Life (HRQoL) of Residents with Persistent Lower Respiratory Symptoms or Asthma Following a Sulphur Stockpile Fire Incident. International Journal of Environmental Research and Public Health, 19(5), 2915. https://doi.org/10.3390/ijerph19052915






