Cost–Benefit Evaluation of an Organizational-Level Intervention Program for Decreasing Sickness Absence among Public Sector Employees in Sweden
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Program Design
2.2. Estimating Intervention Effects on Sickness Absence
2.3. Identifying and Measuring Costs
2.4. Identifying and Measuring Benefits
2.5. Cost–Benefit and Sensitivity Analyses
3. Results
3.1. Net Benefits for the Program and the Two Approaches
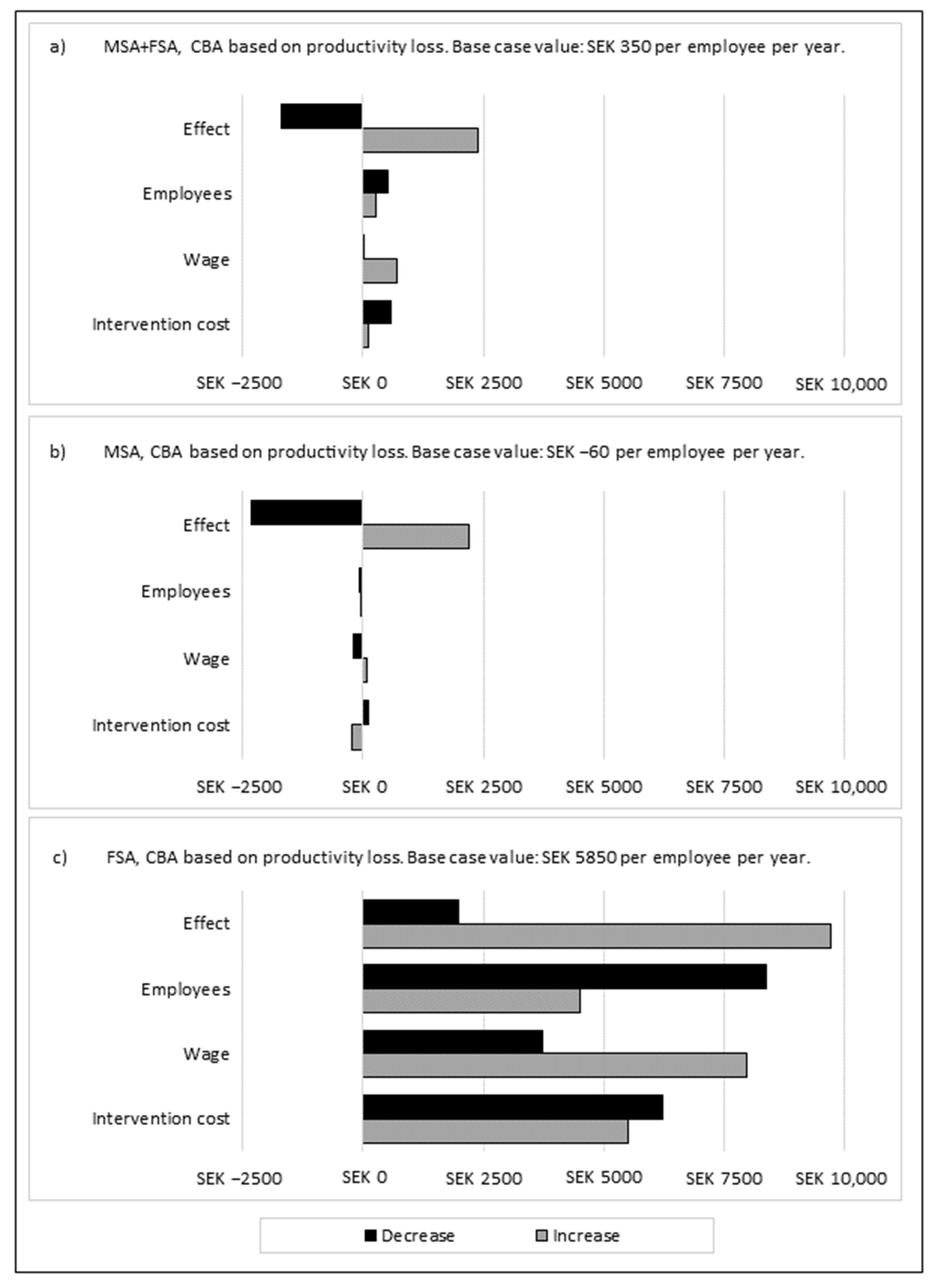
3.2. Sensitivity Analyses of the Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aronsson, G.; Theorell, T.; Grape, T.; Hammarström, A.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Träskman-Bendz, L.; Hall, C. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health 2017, 17, 264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Försäkringskassan. Sjukfrånvaro i psykiatriska diagnoser—En registerstudie av Sveriges arbetande befolkning i åldern 20–69 år. Försäkringskassan 2020, 2020, 8. [Google Scholar]
- Arbetsmiljöverket. Arbetsorsakade besvär. Arbetsmiljöverket 2018, 2018, 3. [Google Scholar]
- Waddell, G.; Burton, A.K. Is Work Good for Your Health and Well-Being? The Stationery Office: London, UK, 2006. [Google Scholar]
- Schultz, A.B.; Chen, C.-Y.; Edington, D.W. The cost and impact of health conditions on presenteeism to employers. Pharmacoeconomics 2009, 27, 365–378. [Google Scholar] [CrossRef]
- Hassard, J.; Teoh, K.; Cox, T.; Cosmar, M.; Gründler, R.; Flemming, D.; Cosemans, B.; Van den Broek, K. Calculating the Cost of Work-Related Stress and Psychosocial Risks; Publications Office of the European Union: Luxembourg, 2014. [Google Scholar]
- Sanandaji, N. Samhällsförlusten av Sjukskrivningar: 64 Miljarder Kronor; Livsförsäkringsbolaget Skandia: Stockholm, Sweden, 2019. [Google Scholar]
- Giga, S.I.; Noblet, A.J.; Faragher, B.; Cooper, C.L. The UK perspective: A review of research on organisational stress management interventions. Aust. Psychol. 2003, 38, 158–164. [Google Scholar] [CrossRef]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Bauer, G.; Davies, J.K.; Pelikan, J. The EUHPID Health Development Model for the classification of public health indicators. Health Promot. Int. 2006, 21, 153–159. [Google Scholar] [CrossRef] [Green Version]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Institute for Future Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Martin, A.; Karanika-Murray, M.; Biron, C.; Sanderson, K. The psychosocial work environment, employee mental health and organizational interventions: Improving research and practice by taking a multilevel approach. Stress Health 2016, 32, 201–215. [Google Scholar] [CrossRef]
- Nielsen, K.; Randall, R. Opening the black box: Presenting a model for evaluating organizational-level interventions. Eur. J. Work Organ. Psychol. 2013, 22, 601–617. [Google Scholar] [CrossRef]
- Cox, T.; Karanika, M.; Griffiths, A.; Houdmont, J. Evaluating organizational-level work stress interventions: Beyond traditional methods. Work Stress 2007, 21, 348–362. [Google Scholar] [CrossRef]
- Swedish Work Environment Authority. Organisational and Social Work Environment. 2015. Available online: http://www.av.se/en/work-environment-work-and-inspections/publications/foreskrifter/organisatorisk-och-social-arbetsmiljo-afs-20154-foreskrifter/ (accessed on 7 December 2021).
- Burgess, M.G.; Brough, P.; Biggs, A.; Hawkes, A.J. Why interventions fail: A systematic review of occupational health psychology interventions. Int. J. Stress Manag. 2020, 27, 195. [Google Scholar] [CrossRef]
- Van Dongen, J.; Proper, K.; Van Wier, M.; Van der Beek, A.; Bongers, P.; Van Mechelen, W.; Van Tulder, M. Systematic review on the financial return of worksite health promotion programmes aimed at improving nutrition and/or increasing physical activity. Obes. Rev. 2011, 12, 1031–1049. [Google Scholar] [CrossRef] [PubMed]
- Gaillard, A.; Sultan-Taïeb, H.; Sylvain, C.; Durand, M.-J. Economic evaluations of mental health interventions: A systematic review of interventions with work-focused components. Saf. Sci. 2020, 132, 104982. [Google Scholar] [CrossRef]
- Reenen, H.H.H.-V.; Proper, K.I.; van den Berg, M. Worksite mental health interventions: A systematic review of economic evaluations. Occup. Environ. Med. 2012, 69, 837–845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grimani, A.; Bergström, G.; Casallas, M.I.R.; Aboagye, E.; Jensen, I.; Lohela-Karlsson, M. Economic evaluation of occupational safety and health interventions from the employer perspective: A systematic review. J. Occup. Environ. Med. 2018, 60, 147. [Google Scholar] [CrossRef] [Green Version]
- Akerstrom, M.; Corin, L.; Severin, J.; Jonsdottir, I.H.; Björk, L. Can Working Conditions and Employees’ Mental Health Be Improved via Job Stress Interventions Designed and Implemented by Line Managers and Human Resources on an Operational Level? Int. J. Environ. Res. Public Health 2021, 18, 1916. [Google Scholar] [CrossRef]
- Severin, J.; Björk, L.; Corin, L.; Jonsdottir, I.H.; Akerstrom, M. Process Evaluation of an Operational-Level Job Stress Intervention Aimed at Decreasing Sickness Absence among Public Sector Employees in Sweden. Int. J. Environ. Res. Public Health 2021, 18, 1778. [Google Scholar] [CrossRef]
- Akerstrom, M.; Severin, J.; Imberg, H.; Jonsdottir, I.H.; Björk, L.; Corin, L. Methodological approach for measuring the effects of organisational-level interventions on employee withdrawal behaviour. Int. Arch. Occup. Environ. Health 2021, 94, 1671–1686. [Google Scholar] [CrossRef]
- Rae, D. How to Reduce Sickness Absences in Sweden: Lessons from International Experience. In OECD Economics Department Working Papers; OECD: Paris, France, 2005. [Google Scholar]
- Board Pharmaceutical Benefits. Läkemedelsförmånsnämndens allmänna råd och ekonomiska utvärderingar. Läkemedelsförmånsnämndens Allmänna Råd LFNAR 2003, 2, 1–4. [Google Scholar]
- Kompier, M.A.; Cooper, C.L.; Geurts, S.A. A multiple case study approach to work stress prevention in Europe. Eur. J. Work Organ. Psychol. 2000, 9, 371–400. [Google Scholar] [CrossRef]
- Dellve, L.; Skagert, K.; Eklöf, M. The impact of systematic occupational health and safety management for occupational disorders and long-term work attendance. Soc. Sci. Med. 2008, 67, 965–970. [Google Scholar] [CrossRef]
- Wikström, E.; Severin, J.; Jonsdottir, I.H.; Akerstrom, M. Process facilitators shifting between the support and expert roles in a complex work environment intervention in the Swedish healthcare sector. J. Health Organ. Manag. 2022, 36, 25–47. [Google Scholar] [CrossRef] [PubMed]
- Sultan-Taieb, H.; Parent-Lamarche, A.; Gaillard, A.; Stock, S.; Nicolakakis, N.; Hong, Q.N.; Vezina, M.; Coulibaly, Y.; Vezina, N.; Berthelette, D. Economic evaluations of ergonomic interventions preventing work-related musculoskeletal disorders: A systematic review of organizational-level interventions. BMC Public Health 2017, 17, 935. [Google Scholar] [CrossRef] [PubMed]
- Aronsson, G.; Gustafsson, K.; Dallner, M. Sick but yet at work. An empirical study of sickness presenteeism. J. Epidemiol. Commun. Health 2000, 54, 502–509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dellve, L.; Hadzibajramovic, E.; Ahlborg, G., Jr. Work attendance among healthcare workers: Prevalence, incentives, and long-term consequences for health and performance. J. Adv. Nurs. 2011, 67, 1918–1929. [Google Scholar] [CrossRef]
- Kankaanpää, E. Economic incentives as a policy tool to promote safety and health at work. Scand. J. Work Environ. Health 2010, 36, 319–324. [Google Scholar] [CrossRef] [Green Version]
- van Dongen, J.M.; Tompa, E.; Clune, L.; Sarnocinska-Hart, A.; Bongers, P.M.; van Tulder, M.W.; van der Beek, A.J.; van Wier, M.F. Bridging the gap between the economic evaluation literature and daily practice in occupational health: A qualitative study among decision-makers in the healthcare sector. Implement. Sci. 2013, 8, 57. [Google Scholar] [CrossRef] [Green Version]


| Total Net Benefit (MSEK) * | Net Benefit per Year (MSEK) | Cost–Benefit Ratio | Net Benefit per Employee per Year (SEK) | |
|---|---|---|---|---|
| CBA based on productivity loss † | ||||
| MSA + FSA | 4.796 | 1.693 | 1.45 | 350 |
| MSA | −0.523 | −0.184 | 0.90 | −60 |
| FSA | 27.213 | 9.605 | 5.83 | 5850 |
| CBA based on sick pay † | ||||
| MSA + FSA | −7.615 | −2.688 | 0.29 | −560 |
| MSA | −3.351 | −1.183 | 0.33 | −370 |
| FSA | −3.361 | −1.186 | 0.40 | −720 |
| MSA + FSA | MSA | FSA | |
|---|---|---|---|
| Costs collected through invoices | |||
| 2017 (MSEK) | 2.438 | 2.260 | 0.178 |
| 2018 (MSEK) | 5.124 | 2.683 | 2.441 |
| Costs for facilitator support | |||
| 2017 (MSEK) | 1.444 | 0 | 1.444 |
| 2018 (MSEK) | 1.532 | 0 | 1.532 |
| Total direct costs (MSEK) | 10.538 | 4.943 | 5.594 |
| Cost per employee (SEK) | 2200 | 1560 | 3410 |
| Estimated intervention effect * | |||
| Total sickness absence (percentage points) | −0.31 | −0.14 | −1.93 † |
| (95% CI) | (−0.88–0.25) | (−0.77–0.49) | (−2.99–−0.87) |
| Short-term sickness absence (percentage points) | −0.08 | −0.07 | −0.18 |
| (95% CI) | (−0.28–0.11) | (−0.29–0.15) | (−0.48–0.12) |
| MSA + FSA | Monetary Support Approach (MSA) | Monetary and Facilitator Support Approach (FSA) | |||||
|---|---|---|---|---|---|---|---|
| Intervention groups (workplaces) n = 79 | Reference groups (operational areas *) n = 79 | Intervention groups (workplaces) n = 71 | Reference groups (operational areas *) n = 71 | Intervention groups (workplaces) n = 8 | Reference groups (operational areas *) n = 8 | ||
| Employees per group (n) | Mean (range) | 61 (11–458) | 1090 (23–15,435) | 45 (11–191) | 1034 (23–15,435) | 205 (41–458) | 1587 (113–3179) |
| Total sickness absence per month, pre-intervention (%) † | Mean (range) | 8.5 (1.0–17.8) | 7.1 (1.2–12.7) | 8.2 (1.0–17.8) | 7.0 (1.2–12.7) | 11.3 (9.1–14.1) | 7.6 (6.1–9.8) |
| Short-term sickness absence (≤14 days) per month, pre-intervention (%) † | Mean (range) | 3.0 (0.4–5.4) | 2.5 (0.8–3.7) | 2.9 (0.4–5.4) | 2.5 (0.8–3.7) | 3.5 (2.5–4.8) | 2.6 (1.9–3.1) |
| Estimated effect on total sickness absence (percentage points) | β (variance) | −0.56 (0.067) | −0.25 (0.016) | −0.43 ‡ (0.083) | −0.29 ‡ (0.019) | −1.9 ‡ (0.247) | 0.03 ‡ (0.044) |
| Estimated effect on short-term sickness absence ≤ 14 days (percentage points) | β (variance) | −0.18 (0.008) | −0.1 (0.002) | −0.2 ‡ (0.009) | −0.13 ‡ (0.003) | −0.11 ‡ (0.02) | 0.07 ‡ (0.004) |

| MSA + FSA | Monetary Support Approach (MSA) | Monetary and Facilitator Support Approach (FSA) | |||||
|---|---|---|---|---|---|---|---|
| Intervention groups (workplaces) n = 79 | Reference groups (operational areas *) n = 79 | Intervention groups (workplaces) n = 71 | Reference groups (operational areas *) n = 71 | Intervention groups (workplaces) n = 8 | Reference groups (operational areas *) n = 8 | ||
| Employees per group (n) | Mean (range) | 61 (11–458) | 1090 (23–15,435) | 45 (11–191) | 1034 (23–15,435) | 205 (41–458) | 1587 (113–3179) |
| Total sickness absence per month, pre-intervention (%) † | Mean (range) | 8.5 (1.0–17.8) | 7.1 (1.2–12.7) | 8.2 (1.0–17.8) | 7.0 (1.2–12.7) | 11.3 (9.1–14.1) | 7.6 (6.1–9.8) |
| Short-term sickness absence (≤14 days) per month, pre-intervention (%) † | Mean (range) | 3.0 (0.4–5.4) | 2.5 (0.8–3.7) | 2.9 (0.4–5.4) | 2.5 (0.8–3.7) | 3.5 (2.5–4.8) | 2.6 (1.9–3.1) |
| Estimated effect on total sickness absence (percentage points) | β (variance) | −0.56 (0.067) | −0.25 (0.016) | −0.43 ‡ (0.083) | −0.29 ‡ (0.019) | −1.9 ‡ (0.247) | 0.03 ‡ (0.044) |
| Estimated effect on short-term sickness absence ≤ 14 days (percentage points) | β (variance) | −0.18 (0.008) | −0.1 (0.002) | −0.2 ‡ (0.009) | −0.13 ‡ (0.003) | −0.11 ‡ (0.02) | 0.07 ‡ (0.004) |
| MSA + FSA | MSA | FSA | |
|---|---|---|---|
| Costs collected through invoices | |||
| 2017 (MSEK) | 2.438 | 2.260 | 0.178 |
| 2018 (MSEK) | 5.124 | 2.683 | 2.441 |
| Costs for facilitator support | |||
| 2017 (MSEK) | 1.444 | 0 | 1.444 |
| 2018 (MSEK) | 1.532 | 0 | 1.532 |
| Total direct costs (MSEK) | 10.538 | 4.943 | 5.594 |
| Cost per employee (SEK) | 2200 | 1560 | 3410 |
| Estimated intervention effect * | |||
| Total sickness absence (percentage points) | −0.31 | −0.14 | −1.93 † |
| (95% CI) | (−0.88–0.25) | (−0.77–0.49) | (−2.99–−0.87) |
| Short-term sickness absence (percentage points) | −0.08 | −0.07 | −0.18 |
| (95% CI) | (−0.28–0.11) | (−0.29–0.15) | (−0.48–0.12) |
| Total Net Benefit (MSEK) * | Net Benefit per Year (MSEK) | Cost–Benefit Ratio | Net Benefit per Employee per Year (SEK) | |
|---|---|---|---|---|
| CBA based on productivity loss † | ||||
| MSA + FSA | 4.796 | 1.693 | 1.45 | 350 |
| - MSA | −0.523 | −0.184 | 0.90 | −60 |
| - FSA | 27.213 | 9.605 | 5.83 | 5850 |
| CBA based on sick pay † | ||||
| MSA + FSA | −7.615 | −2.688 | 0.29 | −560 |
| - MSA | −3.351 | −1.183 | 0.33 | −370 |
| - FSA | −3.361 | −1.186 | 0.40 | −720 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Severin, J.; Svensson, M.; Akerstrom, M. Cost–Benefit Evaluation of an Organizational-Level Intervention Program for Decreasing Sickness Absence among Public Sector Employees in Sweden. Int. J. Environ. Res. Public Health 2022, 19, 2998. https://doi.org/10.3390/ijerph19052998
Severin J, Svensson M, Akerstrom M. Cost–Benefit Evaluation of an Organizational-Level Intervention Program for Decreasing Sickness Absence among Public Sector Employees in Sweden. International Journal of Environmental Research and Public Health. 2022; 19(5):2998. https://doi.org/10.3390/ijerph19052998
Chicago/Turabian StyleSeverin, Jonathan, Mikael Svensson, and Magnus Akerstrom. 2022. "Cost–Benefit Evaluation of an Organizational-Level Intervention Program for Decreasing Sickness Absence among Public Sector Employees in Sweden" International Journal of Environmental Research and Public Health 19, no. 5: 2998. https://doi.org/10.3390/ijerph19052998







