Association of Breastfeeding Duration with 12-Month Postpartum Blood Lipids in a Predominately Lower-Income Hispanic Pregnancy Cohort in Los Angeles
Abstract
:1. Introduction
2. Method
2.1. Study Population
2.2. Measurement of Breastfeeding
2.3. Measurement of Blood Lipids
2.4. Covariates
2.5. Statistical Analysis
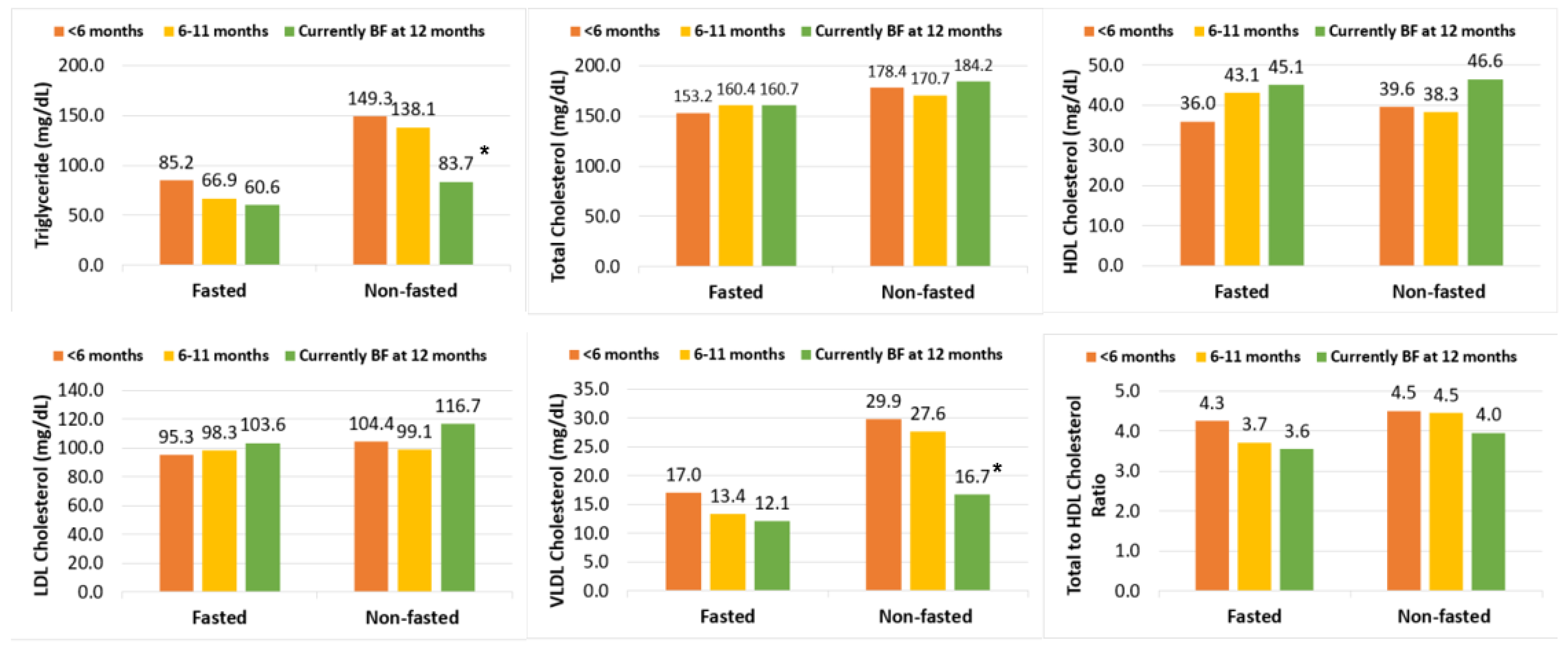
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kochanek, K.D.; Xu, J.; Arias, E. Mortality in the United States, 2019; National Center for Health Statistics: Hyattsville, MD, USA, 2020.
- Carroll, M.D.; Fryar, C.D.; Kit, B.K. Total and High-density Lipoprotein Cholesterol in Adults: United States, 2011–2014. NCHS Data Brief 2015, 226, 1–8. [Google Scholar]
- Kwiterovich, P.O. The antiatherogenic role of high-density lipoprotein cholesterol. Am. J. Cardiol. 1998, 82, 13–21. [Google Scholar] [CrossRef]
- Tunstall-Pedoe, H. Myth and paradox of coronary risk and the menopause. Lancet 1998, 351, 1425–1427. [Google Scholar] [CrossRef]
- Montelongo, A.; Lasuncion, M.A.; Pallardo, L.F.; Herrera, E. Longitudinal study of plasma lipoproteins and hormones during pregnancy in normal and diabetic women. Diabetes 1992, 41, 1651–1659. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, F.G. Normal reference ranges for laboratory values in pregnancy. UpToDate 2014. Available online: https://www.uptodate.com/contents/normal-reference-ranges-for-laboratory-values-in-pregnancy (accessed on 30 October 2021).
- Stuebe, A.M.; Rich-Edwards, J.W. The Reset Hypothesis: Lactation and Maternal Metabolism. Am. J. Perinatol. 2008, 26, 081–088. [Google Scholar] [CrossRef] [Green Version]
- Gunderson, E.P.; Jacobs, D.R.; Chiang, V.; Lewis, C.E.; Feng, J.; Quesenberry, C.P.; Sidney, S. Duration of Lactation and Incidence of the Metabolic Syndrome in Women of Reproductive Age According to Gestational Diabetes Mellitus Status: A 20-Year Prospective Study in CARDIA (Coronary Artery Risk Development in Young Adults). Diabetes 2009, 59, 495–504. [Google Scholar] [CrossRef] [Green Version]
- Jäger, S.; Jacobs, S.; Kröger, J.; Fritsche, A.E.; Schienkiewitz, A.; Rubin, D.; Boeing, H.; Schulze, M.B. Breast-feeding and maternal risk of type 2 diabetes: A prospective study and meta-analysis. Diabetologia 2014, 57, 1355–1365. [Google Scholar] [CrossRef] [Green Version]
- Peters, S.A.; van der Schouw, Y.T.; Wood, A.M.; Sweeting, M.J.; Moons, K.G.M.; Weiderpass, E.; Arriola, L.; Benetou, V.; Boeing, H.; Fabrice, B.; et al. Parity, breastfeeding and risk of coronary heart disease: A pan-European case-cohort study. Eur. J. Prev. Cardiol. 2016, 23, 1755–1765. [Google Scholar] [CrossRef]
- Peters, S.A.E.; Yang, L.; Guo, Y.; Chen, Y.; Bian, Z.; Du, J.; Yang, J.; Li, S.; Li, L.; Woodward, M.; et al. Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300 000 Chinese Women. J. Am. Heart Assoc. 2017, 6, e006081. [Google Scholar] [CrossRef] [Green Version]
- Stuebe, A.M.; Michels, K.B.; Willett, W.C.; Manson, J.E.; Rexrode, K.; Rich-Edwards, J.W. Duration of lactation and incidence of myocardial infarction in middle to late adulthood. Am. J. Obstet. Gynecol. 2009, 200, 138.e1–138.e8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ram, K.T.; Bobby, P.; Hailpern, S.M.; Lo, J.C.; Schocken, M.; Skurnick, J.; Santoro, N. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife—SWAN, the study of women’s health across the nation. Am. J. Obstet. Gynecol. 2008, 198, 268.e1–268.e6. [Google Scholar] [CrossRef] [Green Version]
- Yu, J.; Pudwell, J.; Dayan, N.; Smith, G.N. Postpartum Breastfeeding and Cardiovascular Risk Assessment in Women following Pregnancy Complications. J. Women Health 2020, 29, 627–635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knopp, R.H.; Bergelin, R.O.; Wahl, P.W.; Walden, C.E. Effects of pregnancy, postpartum lactation, and oral contraceptive use on the lipoprotein cholesterol/triglyceride ratio. Metabolism 1985, 34, 893–899. [Google Scholar] [CrossRef]
- Kjos, S.L.; Henry, O.; Lee, R.M.; Buchanan, T.A.; Mishell, D.R. The effect of lactation on glucose and lipid metabolism in women with recent gestational diabetes. Obstet. Gynecol. 1993, 82, 451–455. [Google Scholar]
- Shub, A.; Miranda, M.; Georgiou, H.; McCarthy, E.A.; Lappas, M. The effect of breastfeeding on postpartum glucose tolerance and lipid profiles in women with gestational diabetes mellitus. Int. Breastfeed. J. 2019, 14, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Butte, N.F.; Hopkinson, J.M. Body Composition Changes during Lactation Are Highly Variable among Women. J. Nutr. 1998, 128, 381S–385S. [Google Scholar] [CrossRef] [Green Version]
- Lubold, A.M. Historical-qualitative analysis of breastfeeding trends in three OECD countries. Int. Breastfeed. J. 2019, 14, 1–12. [Google Scholar] [CrossRef]
- Eidelman, A.I.; Schanler, R.J.; Johnston, M.; Landers, S.; Noble, L.; Szucs, K.; Viehmann, L. Breastfeeding and the Use of Human Milk. Pediatrics 2012, 129, e827–e841. [Google Scholar] [CrossRef] [Green Version]
- Beauregard, J.L.; Hamner, H.C.; Chen, J.; Avila-Rodriguez, W.; Elam-Evans, L.D.; Perrine, C.G. Racial Disparities in Breastfeeding Initiation and Duration Among U.S. Infants Born in 2015. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 745–748. [Google Scholar] [CrossRef]
- Chiang, K.V.; Li, R.; Anstey, E.H.; Perrine, C.G. Racial and Ethnic Disparities in Breastfeeding Initiation─ United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Bastain, T.M.; Chavez, T.; Habre, R.; Girguis, M.S.; Grubbs, B.; Toledo-Corral, C.; Amadeus, M.; Farzan, S.F.; Al-Marayati, L.; Lerner, D.; et al. Study Design, Protocol and Profile of the Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) Pregnancy Cohort: A Prospective Cohort Study in Predominantly Low-Income Hispanic Women in Urban Los Angeles. BMC Pregnancy Childbirth 2019, 19, 189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Saki, A.; Eshraghian, M.R.; Tabesh, H. Patterns of Daily Duration and Frequency of Breastfeeding among Exclusively Breastfed Infants in Shiraz, Iran, a 6-month Follow-up Study Using Bayesian Generalized Linear Mixed Models. Glob. J. Health Sci. 2012, 5, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S.; Pearl, J.; Robins, J.M. Causal Diagrams for Epidemiologic Research. Epidemiology 1999, 10, 37–48. [Google Scholar] [CrossRef]
- Allen, J.; Hector, D. Benefits of breastfeeding. N. S. W. Public Health Bull. 2005, 16, 42–46. [Google Scholar]
- Schwarz, E.B.; Nothnagle, M. The maternal health benefits of breastfeeding. Am. Fam. Physician 2015, 91, 603–604. [Google Scholar]
- Kramer, M.S.; Kakuma, R. Optimal duration of exclusive breastfeeding. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2012. [Google Scholar] [CrossRef]
- Kelly, Y.J.; Watt, R.G.; Nazroo, J.Y. Racial/Ethnic Differences in Breastfeeding Initiation and Continuation in the United Kingdom and Comparison With Findings in the United States. Pediatrics 2006, 118, e1428–e1435. [Google Scholar] [CrossRef] [Green Version]
- Kallio, M.J.; Siimes, M.A.; Perheentupa, J.; Salmenperä, L.; Miettinen, T.A. Serum cholesterol and lipoprotein concentrations in mothers during and after prolonged exclusive lactation. Metabolism 1992, 41, 1327–1330. [Google Scholar] [CrossRef]
- Guzmán-Mercado, E.; Vásquez-Garibay, E.M.; Ramírez, C.A.S.; Muñoz-Esparza, N.C.; Larrosa-Haro, A.; Arreola, P.L.M. Full Breastfeeding Modifies Anthropometric and Body Composition Indicators in Nursing Mothers. Breastfeed. Med. 2021, 16, 264–271. [Google Scholar] [CrossRef]
- Basu, D.; Goldberg, I.J. Regulation of lipoprotein lipase-mediated lipolysis of triglycerides. Curr. Opin. Lipidol. 2020, 31, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Flint, D.J.; Binart, N.; Kopchick, J.; Kelly, P. Effects of growth hormone and prolactin on adipose tissue development and function. Pituitary 2003, 6, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Tulenko, T.; Sumner, A.E. The physiology of lipoproteins. J. Nucl. Cardiol. 2002, 9, 638–649. [Google Scholar] [CrossRef] [PubMed]
- Natland, S.T.; Nilsen, T.I.L.; Midthjell, K.; Andersen, L.F.; Forsmo, S. Lactation and cardiovascular risk factors in mothers in a population-based study: The HUNT-study. Int. Breastfeed. J. 2012, 7, 8. [Google Scholar] [CrossRef] [Green Version]
- Velle-Forbord, V.; Skråstad, R.B.; Salvesen, Ø.; Kramer, M.S.; Morken, N.H.; Vanky, E. Breastfeeding and long-term maternal metabolic health in the HUNT Study: A longitudinal population-based cohort study. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 526–534. [Google Scholar] [CrossRef]
- Gunderson, E.P.; Lewis, C.E.; Wei, G.S.; Whitmer, R.A.; Quesenberry, C.P.; Sidney, S. Lactation and Changes in Maternal Metabolic Risk Factors. Obstet. Gynecol. 2007, 109, 729–738. [Google Scholar] [CrossRef] [Green Version]
- Choi, S.R.; Kim, Y.M.; Cho, M.S.; Kim, S.H.; Shim, Y.S. Association Between Duration of Breast Feeding and Metabolic Syndrome: The Korean National Health and Nutrition Examination Surveys. J. Women Health 2017, 26, 361–367. [Google Scholar] [CrossRef]
- Stuebe, A.M.; Kleinman, K.; Gillman, M.W.; Rifas-Shiman, S.L.; Gunderson, E.P.; Rich-Edwards, J. Duration of lactation and maternal metabolism at 3 years postpartum. J. Women Health 2010, 19, 941–950. [Google Scholar] [CrossRef]
- Sidhu, D.; Naugler, C. Fasting time and lipid levels in a community-based population: A cross-sectional study. Arch. Intern. Med. 2012, 172, 1707–1710. [Google Scholar] [CrossRef] [Green Version]
- Driver, S.L.; Martin, S.S.; Gluckman, T.J.; Clary, J.M.; Blumenthal, R.S.; Stone, N.J. Fasting or Nonfasting Lipid Measurements: It Depends on the Question. J. Am. Coll. Cardiol. 2016, 67, 1227–1234. [Google Scholar] [CrossRef]
| Characteristics | Overall (n = 79) | <6 Months (n = 28) | ≥6–11 Months (n = 24) | ≥12 Months (n = 27) | F/χ2 | p |
|---|---|---|---|---|---|---|
| Maternal age | 29.62 (5.80) | 30.19 (5.56) | 28.25 (5.18) | 30.48 (6.64) | 1.16 | 0.32 |
| Pre-Pregnancy BMI | 27.45 (4.99) | 28.58 (6.23) | 27.30 (3.29) | 26.30 (4.85) | 1.38 | 0.26 |
| GA at enrollment | 14.27 (6.54) | 15.09 (6.95) | 12.98 (5.80) | 14.56 (6.77) | 0.71 | 0.49 |
| Maternal race * | 6.63 | 0.36 | ||||
| White | 73 (92.41) | 25 (89.29) | 24 (100.00) | 24 (92.31) | ||
| Asian | 2 (2.53) | 2 (7.14) | 0 (0.00) | 0 (0.00) | ||
| Black or African American | 1 (1.27) | 0 (0.00) | 0 (0.00) | 1 (3.85) | ||
| More than one race | 2 (2.53) | 1 (3.57) | 0 (0.00) | 1 (3.85) | ||
| Maternal country origin | 9.46 | 0.15 | ||||
| Latin America | 35 (44.30) | 10 (35.71) | 16 (66.67) | 9 (33.33) | ||
| USA | 37 (46.84) | 16 (57.14) | 7 (29.17) | 14 (51.85) | ||
| Asia/Unknown | 7 (8.86) | 2 (7.14) | 1 (4.17) | 4 (14.81) | ||
| Maternal ethnicity | 1.32 | 0.73 | ||||
| Non-Hispanic | 15 (18.99) | 7 (25.00) | 3 (12.50) | 5 (18.52) | ||
| Hispanic | 64 (81.01) | 21 (75.00) | 21 (87.50) | 22 (81.48) | ||
| Maternal marital status | 4.52 | 0.61 | ||||
| Married | 23 (29.11) | 12 (42.86) | 6 (25.00) | 5 (18.52) | ||
| Cohabiting | 36 (45.57) | 10 (35.71) | 12 (50.00) | 14 (51.85) | ||
| Separated/Unknown | 20 (25.32) | 6 (21.43) | 6 (25.00) | 8 (29.63) | ||
| Annual household income | 6.02 | 0.11 | ||||
| ≥$30,000 | 27 (34.18) | 12 (42.86) | 6 (25.00) | 9 (33.33) | ||
| <$30,000 | 52 (65.82) | 16 (57.14) | 18 (75.00) | 18 (66.67) | ||
| Maternal education | 0.93 | 0.82 | ||||
| Some college or above | 45 (56.96) | 14 (50.00) | 15 (62.50) | 16 (59.26) | ||
| High school or lower | 34 (43.04) | 14 (50.00) | 9 (37.50) | 11 (40.74) | ||
| Pre-Pregnancy BMI categories | 12.89 | 0.05 | ||||
| Normal/Underweight | 27 (34.18) | 10 (35.71) | 8 (33.33) | 9 (33.33) | ||
| Overweight | 30 (37.97) | 7 (25.00) | 11 (45.83) | 12 (44.44) | ||
| Obese | 22 (27.85) | 11 (39.29) | 5 (20.83) | 6 (22.22) | ||
| Birth order | 0.98 | 0.81 | ||||
| First | 43 (54.43) | 14 (50.00) | 15 (62.50) | 14 (51.85) | ||
| Second or later | 36 (45.57) | 14 (50.00) | 9 (37.50) | 13 (48.15) | ||
| Fasting blood | 5.66 | 0.13 | ||||
| Did not fast > 8 h | 41 (51.90) | 14 (50.00) | 14 (58.33) | 13 (48.15) | ||
| Fasted > 8 h | 38 (48.10) | 14 (50.00) | 10 (41.67) | 14 (51.85) | ||
| Lipid levels | ||||||
| Triglyceride | 118.17 (66.98) | 131.09 (58.32) | 134.42 (81.35) | 90.33 (53.34) | 3.82 | 0.03 |
| Total Cholesterol | 168.39 (29.63) | 165.40 (22.80) | 169.93 (34.37) | 170.12 (32.15) | 0.22 | 0.81 |
| HDL Cholesterol | 40.19 (11.93) | 36.94 (11.89) | 40.24 (10.20) | 43.52 (12.84) | 2.16 | 0.12 |
| LDL Cholesterol | 104.56 (24.61) | 102.25 (19.47) | 102.81 (30.54) | 108.53 (23.96) | 0.53 | 0.59 |
| VLDL Cholesterol | 23.63 (13.40) | 26.22 (11.66) | 26.88 (16.27) | 18.07 (10.67) | 3.82 | 0.03 |
| Total to HDL Cholesterol Ratio | 4.52 (1.45) | 4.94 (1.77) | 4.44 (1.29) | 4.15 (1.13) | 2.12 | 0.13 |
| Pregnancy-related complications | ||||||
| Glucose intolerant/GDM/T2DM | 4.22 | 0.24 | ||||
| No | 59 (74.68) | 19 (67.86) | 17 (70.83) | 23 (85.19) | ||
| Yes | 20 (25.32) | 9 (32.14) | 7 (29.17) | 4 (14.81) | ||
| Hypertensive disorder of pregnancy/pre-eclampsia | 1.26 | 0.74 | ||||
| No | 65 (82.28) | 24 (85.71) | 18 (75.00) | 23 (85.19) | ||
| Yes | 14 (17.72) | 4 (14.29) | 6 (25.00) | 4 (14.81) | ||
| Asthma | 2.42 | 0.49 | ||||
| No | 69 (87.34) | 26 (92.86) | 21 (87.50) | 22 (81.48) | ||
| Yes | 10 (12.66) | 2 (7.14) | 3 (12.50) | 5 (18.52) | ||
| Depression | 0.77 | 0.86 | ||||
| No | 75 (94.94) | 27 (96.43) | 23 (95.83) | 25 (92.59) | ||
| Yes | 4 (5.06) | 1 (3.57) | 1 (4.17) | 2 (7.41) | ||
| Breastfeeding Duration | Model 1 | Model 2 | Model 3 | Model 4 | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (95% CI) | p † | Mean (95% CI) | p † | Mean (95% CI) | p † | Mean (95% CI) | p † | |
| Triglyceride (mg/dL) | ||||||||
| 12 months | 80.45 (66.20, 97.77) | 0.01 | 80.86 (66.96, 97.66) | <0.01 | 79.30 (64.20, 97.96) | 0.01 | 81.56 (66.13, 100.59) | 0.01 |
| 6–11 months | 112.58 (91.55, 138.45) | 0.69 | 110.01 (89.98, 134.50) | 0.56 | 99.11 (76.33, 128.69) | 0.35 | 101.35 (78.33, 131.14) | 0.37 |
| <6 months | 119.11 (98.36, 144.25) | Ref. | 119.11 (98.97, 143.35) | Ref. | 113.94 (91.23, 142.30) | Ref. | 115.46 (93.06, 143.25) | Ref. |
| P for trend | <0.01 | <0.01 | 0.01 | 0.01 | ||||
| Total Cholesterol (mg/dL) | ||||||||
| ≥12 months | 167.36 (156.78, 178.65) | 0.66 | 167.61 (157.27, 178.64) | 0.62 | 170.57 (158.55, 183.49) | 0.57 | 172.96 (160.94, 185.88) | 0.42 |
| ≥6–12 months | 166.84 (155.68, 178.80) | 0.71 | 165.70 (154.83, 177.33) | 0.82 | 166.00 (151.67, 181.67) | 1.00 | 167.99 (153.76, 183.54) | 0.87 |
| <6 months | 163.96 (153.78, 174.82) | Ref. | 163.96 (154.02, 174.55) | Ref. | 165.97 (153.70, 179.22) | Ref. | 166.59 (154.69, 179.40) | Ref. |
| P for trend | 0.65 | 0.62 | 0.56 | 0.41 | ||||
| HDL Cholesterol (mg/dL) | ||||||||
| ≥12 months | 41.74 (37.27, 46.74) | 0.03 | 41.75 (37.25, 46.78) | 0.03 | 45.17 (40.47, 50.43) | 0.02 | 45.02 (40.30, 50.30) | 0.02 |
| ≥6–12 months | 39.07 (34.65, 44.05) | 0.20 | 39.03 (34.57, 44.06) | 0.21 | 41.44 (36.18, 47.48) | 0.26 | 41.51 (36.23, 47.57) | 0.21 |
| <6 months | 35.11 (31.42, 39.24) | Ref. | 35.11 (31.40, 39.27) | Ref. | 37.98 (33.83, 42.64) | Ref. | 37.67 (33.62, 42.22) | Ref. |
| P for trend | 0.03 | 0.03 | 0.02 | 0.02 | ||||
| LDL Cholesterol (mg/dL) | ||||||||
| ≥12 months | 105.96 (96.97, 115.79) | 0.40 | 106.09 (97.11, 115.90) | 0.39 | 105.81 (95.31, 117.46) | 0.43 | 107.78 (97.23, 119.48) | 0.32 |
| ≥6–12 months | 98.88 (90.00, 108.63) | 0.80 | 98.34 (89.50, 108.05) | 0.73 | 98.07 (86.20, 111.58) | 0.76 | 99.55 (87.71, 112.98) | 0.86 |
| <6 months | 100.54 (92.15, 109.69) | Ref. | 100.54 (92.18, 109.66) | Ref. | 100.27 (89.84, 111.91) | Ref. | 100.85 (90.71, 112.12) | Ref. |
| P for trend | 0.41 | 0.40 | 0.42 | 0.31 | ||||
| VLDL Cholesterol (mg/dL) | ||||||||
| ≥12 months | 16.09 (13.24, 19.56) | 0.01 | 16.17 (13.39, 19.53) | <0.01 | 15.86 (12.84, 19.59) | 0.01 | 16.31 (13.23, 20.12) | 0.01 |
| ≥6–12 months | 22.52 (18.31, 27.69) | 0.69 | 22.00 (18.00, 26.90) | 0.56 | 19.82 (15.27, 25.74) | 0.35 | 20.27 (15.66, 26.23) | 0.37 |
| <6 months | 23.82 (19.67, 28.85) | Ref. | 23.82 (19.79, 28.67) | Ref. | 22.79 (18.25, 28.46) | Ref. | 23.09 (18.61, 28.65) | Ref. |
| P for trend | <0.01 | <0.01 | 0.01 | 0.01 | ||||
| Total to HDL Cholesterol Ratio | ||||||||
| ≥12 months | 4.01 (3.58, 4.49) | 0.06 | 4.02 (3.58, 4.50) | 0.06 | 3.78 (3.35, 4.26) | 0.06 | 3.84 (3.43, 4.30) | 0.06 |
| ≥6–12 months | 4.27 (3.78, 4.82) | 0.28 | 4.25 (3.76, 4.79) | 0.25 | 4.01 (3.45, 4.65) | 0.30 | 4.05 (3.52, 4.65) | 0.26 |
| <6 months | 4.67 (4.18, 5.22) | Ref. | 4.67 (4.18, 5.22) | Ref. | 4.37 (3.85, 4.96) | Ref. | 4.42 (3.94, 4.97) | Ref. |
| P for trend | 0.06 | 0.06 | 0.06 | 0.06 | ||||
| Natural Log-Transformed Lipids | Model 1 | Model 2 | Model 3 | Model 4 | ||||
|---|---|---|---|---|---|---|---|---|
| Beta (95% CI) | p | Beta (95% CI) | p | Beta (95% CI) | p | Beta (95% CI) | p | |
| Triglyceride | −0.04 (−0.07, −0.01) | <0.01 | −0.04 (−0.07, −0.01) | <0.01 | −0.04 (−0.06, −0.01) | <0.01 | −0.03 (−0.06, −0.01) | 0.01 |
| Total Cholesterol | 0.00 (−0.01, 0.01) | 0.46 | 0.00 (−0.01, 0.01) | 0.45 | 0.00 (−0.01, 0.01) | 0.47 | 0.00 (0.00, 0.01) | 0.29 |
| HDL Cholesterol | 0.02 (0.01, 0.04) | <0.01 | 0.02 (0.01, 0.04) | <0.01 | 0.02 (0.01, 0.04) | <0.01 | 0.02 (0.01, 0.03) | <0.01 |
| LDL Cholesterol | 0.01 (−0.01, 0.02) | 0.36 | 0.01 (−0.01, 0.02) | 0.36 | 0.01 (−0.01, 0.02) | 0.42 | 0.01 (−0.01, 0.02) | 0.25 |
| VLDL Cholesterol | −0.04 (−0.07, −0.01) | <0.01 | −0.04 (−0.07, −0.01) | <0.01 | −0.04 (−0.06, −0.01) | <0.01 | −0.03 (−0.06, −0.01) | 0.01 |
| Total to HDL Cholesterol Ratio | −0.02 (−0.03, 0.00) | 0.02 | −0.02 (−0.03, 0.00) | 0.02 | −0.02 (−0.03, 0.00) | 0.02 | −0.02 (−0.03, 0.00) | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niu, Z.; Naya, C.H.; Reynaga, L.; Toledo-Corral, C.M.; Johnson, M.; Yang, T.; Grubbs, B.; Lurvey, N.; Lerner, D.; Dunton, G.F.; et al. Association of Breastfeeding Duration with 12-Month Postpartum Blood Lipids in a Predominately Lower-Income Hispanic Pregnancy Cohort in Los Angeles. Int. J. Environ. Res. Public Health 2022, 19, 3008. https://doi.org/10.3390/ijerph19053008
Niu Z, Naya CH, Reynaga L, Toledo-Corral CM, Johnson M, Yang T, Grubbs B, Lurvey N, Lerner D, Dunton GF, et al. Association of Breastfeeding Duration with 12-Month Postpartum Blood Lipids in a Predominately Lower-Income Hispanic Pregnancy Cohort in Los Angeles. International Journal of Environmental Research and Public Health. 2022; 19(5):3008. https://doi.org/10.3390/ijerph19053008
Chicago/Turabian StyleNiu, Zhongzheng, Christine H. Naya, Lorena Reynaga, Claudia M. Toledo-Corral, Mark Johnson, Tingyu Yang, Brendan Grubbs, Nathana Lurvey, Deborah Lerner, Genevieve F. Dunton, and et al. 2022. "Association of Breastfeeding Duration with 12-Month Postpartum Blood Lipids in a Predominately Lower-Income Hispanic Pregnancy Cohort in Los Angeles" International Journal of Environmental Research and Public Health 19, no. 5: 3008. https://doi.org/10.3390/ijerph19053008
APA StyleNiu, Z., Naya, C. H., Reynaga, L., Toledo-Corral, C. M., Johnson, M., Yang, T., Grubbs, B., Lurvey, N., Lerner, D., Dunton, G. F., Habre, R., Breton, C. V., Bastain, T. M., & Farzan, S. F. (2022). Association of Breastfeeding Duration with 12-Month Postpartum Blood Lipids in a Predominately Lower-Income Hispanic Pregnancy Cohort in Los Angeles. International Journal of Environmental Research and Public Health, 19(5), 3008. https://doi.org/10.3390/ijerph19053008







